Abstract
The great challenge to global public health caused by the coronavirus pandemic has lasted for two years in Korea. However, Korean young adults seem less compliant with preventive health behaviors than older adults. This study aims to explore the relationship between risk perception variables of optimistic bias, hypochondriasis, and mass psychology, and preventive health behavior in relation to the coronavirus pandemic through a cross-sectional online survey. The participants are 91 Korean young adults aged 19–30. The results show that mass psychology has a positive relationship with preventive health behavior, whereas optimistic bias and hypochondriasis do not. In detail, people with high or middle levels of mass psychology displayed higher preventive health behavior compared with those who had low levels of mass psychology, and the highest compliance was for wearing a mask, followed by COVID-19 vaccination, whereas the lowest compliance was for influenza vaccination. These findings could be explained by the Korean culture of strong collectivism and the characteristics of COVID-19, which evoked extreme fear globally. The results of this study can be useful for policy establishment in the ongoing prevention of COVID-19 and suggest that mass psychology should be used effectively in planning preventive communication campaigns.
1. Introduction
COVID-19 and influenza (flu), the illnesses causing the pandemic, are both contagious respiratory illnesses. The coronavirus pandemic has been an especially great challenge for global public health in the last two years. The World Health Organization (WHO) estimates that 1 billion people worldwide are infected with influenza annually. As of 3 August 2022, the WHO reported 577,018,226 cases and 6,401,046 deaths globally from COVID-19 [1]. In South Korea, the first confirmed case appeared in February 2020, after the first cases appeared in China in late 2019, and the Korea Disease Control and Prevention Agency (KDCA) reported 20,052,305 cases and 25,110 deaths as of 3 August 2022 [2].
To remain safe during this public health crisis, individuals must take preventive measures. Accordingly, mass media report news related to COVID-19 to guide the public and promote preventive measures, including vaccination campaigns, every day. However, young adults seem less compliant with preventive behaviors than older adults, as COVID-19 is known to be more fatal to older adults. Based on a precedent study [3], being younger was associated with a lower chance of adopting the preventive rules during the H1N1 influenza pandemic. Young adulthood is an important period for establishing health behavior patterns in life.
Health behavior theories suggest that perceived risk is a key determinant of engagement in preventive behaviors. Perceived severity, a kind of risk perception, was a factor related to preventive behaviors during the COVID-19 pandemic [4]. When people encounter health information, they mostly either experience general fear or concerns about relevant health crises in their imagination or think they may have a health crisis, which is called personalized risk perception. Risk perception is an individual’s level of perceived risk in a message and is one of the main concepts supporting health behavior change in a person who receives a health promotion message [5]. Optimistic bias is the lack of the idea that a health crisis would happen to oneself, which means that there is no personalizing risk perception [6,7]. This bias occurs in the process of perceiving risk through a social comparison process, rather than being a simple belief [8]. Optimistic bias may decrease anxiety and provide psychological benefits for emotional well-being [8,9,10], but it has a negative relationship with preventive health behavior. A recent study on COVID-19-related health behavior showed that people with a high level of optimistic bias had a low-risk perception of contracting COVID-19, which negatively influenced their responses to health crises, information-seeking intentions, and behavior [9]. In addition, optimistic bias has a negative relationship with the adoption of protective behavior [10].
In contrast to optimistic bias, some people are excessively worried about health, which may cause a cognitive bias to develop health anxiety, which is called hypochondria or hypochondriasis [11]. Hypochondria is characterized by extensive worries about health [12] and lies on a continuous spectrum from clinical hypochondriasis to simple health anxiety [13]. The Diagnostic and Statistical Manual of Mental Disorders-V (DSM-V) is applied to hypochondria, which is classified as a somatic symptom disorder or an illness anxiety disorder [14]. However, hypochondriasis is viewed as a cognitive and perceptual impairment in psychology [15]. Lee [16] suggests that the illness attitude scale (IAS) is a suitable instrument for measuring hypochondriasis and includes four subscales: disease phobia and beliefs; impaired adaptation due to disease; safety pursuit behavior; and thanatophobia. Safety pursuit behavior, which is a factor in hypochondriasis, is related to preventive health behavior.
Another interesting factor influencing preventive health behavior is mass psychology, which is one’s perception based on the number of people exposed to the same risk as an individual. In a study of risk perception, Yamaguchi [17] reported that an individual’s perceived risk decreases as the number of people exposed to the same risk increases. This means that people feel secure when many people experience the same risk, which is called the group diffusion effect [18,19]. According to Rubin et al., who studied behavioral change during the swine flu outbreak [20], this is called public perception. In a recent study conducted during the COVID-19 pandemic, subjective norms related to parents was a significant factor associated with preventive behaviors among Korean young adults [21]. These studies indicate that one’s perception of the norm of the group they belong to, that is, mass psychology, is related to preventive health behavior.
Within the context of the COVID-19 pandemic, it is crucial to understand psychological factors, such as risk perceptions of preventive behaviors, to manage infection. Therefore, this study aims to explore the relationship between risk perception variables of optimistic bias, hypochondriasis, and mass psychology, and preventive health behavior in relation to the coronavirus pandemic in young adults.
2. Materials and Methods
2.1. Study Design
This cross-sectional descriptive study via an online survey examined the relationship between optimistic bias, hypochondriasis, mass psychology, and preventive health behavior for COVID-19 or influenza in young adults.
2.2. Participants and Enrollment
The study participants were recruited through an online posting on K university’s website from the 31 May to the 6 June 2022. Inclusion criteria were as follows: young adults aged 19–30 years who agreed to participate in the study after understanding the study purpose, and undergraduate or graduate students in K university. Exclusion criteria were those who were hospitalized or immobile with severe diseases. The sample size was calculated using the G power 3.1.9.2 program. With a level of significance (α) of 0.05, a medium effect size of 0.3, and a power of 0.80, the required sample size was 82. A total of 91 participants participated in the study.
2.3. Measurement
Four instruments were used in this study; optimistic bias (4 questions); hypochondriasis (27 questions); mass psychology (3 questions); and preventive health behaviors (6 questions). Questions on general characteristics of the study subject included gender, age, experience of COVID-19, experience of illness, history of hospitalization, religion, present illness, and cell phone number.
2.3.1. Optimistic Bias
Optimistic bias can be measured using two risk determinants: comparative risk and absolute risk. Comparative risk was assessed using the question ’compared with the average person of your age and sex, are you more, equally, or less likely to experience X?’. Absolute risk was assessed using two questions: ‘what is the possibility of a health crisis X you will have? (X1)’ and ‘what is the possibility of the health crisis X in those who are the same age and sex as you? (X2)’. If the difference between X2 and X1 (X2–X1) is positive, it is interpreted as an optimistic bias. This means that the person has an optimistic bias when giving a more favorable rating than other people.
Clarke et al. [22] support the use of absolute risk to reduce comparative consciousness and noticeable bias as a more conservative measure than using comparative risk. Accordingly, this study used absolute risk as the determinant of optimistic bias. In this study, optimistic bias for susceptibility was measured by asking a set of two questions: ‘what is the possibility of health crisis X (COVID-19 or influenza) you will have?’ and ‘what is the average possibility of health crisis X in those of the same age and sex as you?’ Optimistic bias for severity was measured by asking a set of two questions: ‘what is the chance you die of the health crisis X?’ and ‘what is the average chance to die of health crisis X in those of the same age and sex as you?’. The score for each question ranged from 1 point (very low) to 4 points (very high). It was interpreted that optimistic bias existed when the difference between the average score of other people and the average score of the subject (X2 − X1) was positive. In addition, optimistic bias was considered greater when the sum of the two differences was larger. In this study, Cronbach’s α was 0.72.
2.3.2. Hypochondriasis
The Illness Attitude Scale (IAS) was developed by Kellner [23] to measure hypochondriasis. This scale comprises a total of 27 question items with 9 categories, including worry about illness, concerns about pain, health habits, hypochondriacal beliefs, thanatophobia, disease phobia, bodily preoccupations, treatment experience, and effects of symptoms. Lee [24] translated and validated the scale to measure hypochondriac fear, beliefs, and attitudes. Lee [16] conducted a factor analysis of the scale and categorized it into 4 subscales: disease phobia and beliefs; impaired adaptation due to disease; safety pursuit behavior; and thanatophobia. Each subscale score ranged from 0 (strongly disagree) to 4 (strongly agree), with a higher score indicating a greater tendency for hypochondriasis. Lee [13] suggests that IAS is a suitable instrument for measuring hypochondriasis. Cronbach’s α was 0.86 in the study by Lee [16] and 0.91 in this study.
2.3.3. Mass Psychology
Mass psychology was assessed by measuring one’s perception of other people’s handwashing, mask-wearing, and vaccinating. Each item score ranged from 0 (strongly disagree) to 4 (strongly agree), with a higher score indicating greater mass psychology, that is, one perceives a larger group of people performing preventive health behavior. Cronbach’s α was 0.75 in a study by Lee [19], and 0.78 in this study.
2.3.4. Preventive Health Behavior
Preventive health behavior was assessed by measuring compliance with 6 preventive health behaviors related to influenza and COVID-19, including handwashing, wearing a mask, social distancing, COVID-19 vaccination, influenza vaccination, and proper fluid intake, including humidification. This instrument was made based on the preventive measures for COVID-19 suggested by the WHO, which include 6 items. All items were evaluated for content validity by 3 nursing professors on a scale of 1 to 4 points. The content validity index (CVI) for all 6 items was 3 points or higher. Exploratory factor analysis conducted for construct validity revealed that all 6 items had communality of 0.5 or higher, with a KMO (Kaiser–Meyer–Olkin) of 0.704, Bartlett χ2 of 124.072, df of 15, and p of 0.000, which showed the appropriateness of the instrument. Each item score ranged from 0 (strongly disagree) to 4 (strongly agree), with higher scores indicating more preventive health behaviors. In this study, Cronbach’s α was 0.74.
2.4. Data Collection and Ethical Consideration
This study was approved by the institutional review board of K University before data were collected to protect the study participants, who were recruited through the posting on the K University online site and were asked to complete the survey online. The study participants voluntarily signed the informed consent form online after reviewing the instructions on the consent for the study subject and then proceeded with the survey. They were informed that the completion of the survey would take 10 min and were given the lead researcher’s contact information (cell phone and email address) for further questions in the instructions. Participants’ responses, including personal information, were collected in the secured folder of the lead researcher’s computer drive to protect participants’ sensitive information. Each participant in the study received a KRW 5000.00 (approximately USD 5.00) Starbucks gift card via their cell phone as gratitude for their contribution, and then all personal information of the participants was removed.
2.5. Statistical Analysis
Data were analyzed using the IBM SPSS software (version 26.0; IBM Corp., Armonk, NY, USA). Descriptive statistics were used to analyze the general characteristics of the study participants. Normality was tested using Kolmogorov–Smirnov and Shapiro–Wilk.
The differences in optimistic bias, hypochondriasis, mass psychology, and preventive health behavior based on participants’ characteristics (gender, age, experience of COVID-19, experience of illness, history of hospitalization, and present illness) were analyzed using Mann–Whitney, a non-parametric test for a non-normal distribution of variables: optimistic bias, hypochondriasis, mass psychology, and preventive health behavior. The differences in preventive health behavior among the three groups (lower than 25%, 25–75%, and higher than 75%), based on the level of optimistic bias, hypochondriasis, and mass psychology, were analyzed using the Kruskal–Wallis test, a non-parametric test. The correlation between optimistic bias, hypochondriasis, mass psychology, and preventive health behavior was analyzed using Spearman’s rho, a non-parametric test.
3. Results
3.1. General Characteristics
The study participants’ characteristics were age, gender, experience of COVID-19, experience of illness (including COVID-19), present illness, and history of hospital administration. There were 91 participants, with 38 males (41.8%) and 53 females (58.2%), and the average age was 25.40 years, with 27 participants younger than 25 years (30%) and 63 participants older than 26 years (70%). All participants were divided into two groups, younger than 25 years and older than 26 years, since the mean value (25.40) is located between 25 and 26 years. COVID-19 was contracted by 54.9% of the participants, illness, including COVID-19, was experienced by 73.6% of the participants, prior hospitalization was experienced by 57.1% of the participants, and the present illness was experienced by 11% of the participants. The variables of preventive health behavior, optimistic bias, hypochondria, and mass psychology showed a non-normal distribution (Table 1).

Table 1.
Characteristics of participants (N = 91).
Table 2 shows compliance with six preventive health behaviors in young adults. The highest compliance was observed in wearing a mask, followed by the COVID-19 vaccination, whereas the lowest compliance was with influenza vaccination.

Table 2.
Descriptive statistics of preventive health behavior (N = 91).
3.2. Difference between Optimistic Bias, Hypochondriasis, and Mass Psychology Associated with Participants’ Characteristics
The Mann–Whitney test showed differences in the main variables (optimistic bias, hypochondriasis, mass psychology, and preventive health behavior) based on the general characteristics of the participants. People without present or previous illness showed significantly higher optimistic bias scores than those with illness. In addition, individuals with COVID-19 or other illnesses showed significantly higher hypochondriasis scores than those without illnesses. Those aged 26 years or older had significantly higher mass psychology scores than those aged 25 years or younger. However, preventive health behaviors were not associated with the general characteristics of the participants (Table 3).

Table 3.
Difference of main variables by participant characteristics (N = 91).
3.3. Relationship between Preventive Health Behavior, Optimistic Bias, Hypochondria, and Mass Psychology
Correlations between the main variables (preventive health behavior, optimistic bias, hypochondria, and mass psychology) show that there was only a significant relationship between preventive health behavior and mass psychology (Table 4). This means that participants with a high level of mass psychology showed a high level of preventive health behavior (Figure 1).

Table 4.
Correlations of main variables (N = 91).
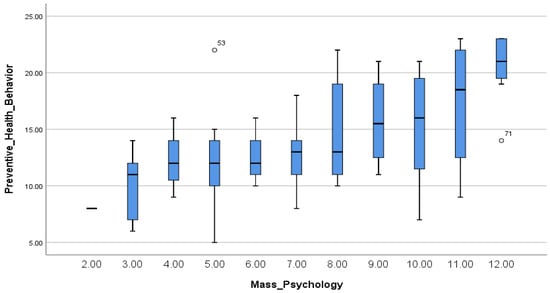
Figure 1.
Spearman’s correlations between preventive health behavior and mass psychology.
3.4. Preventive Health Behavior by Optimistic Bias, Hypochondria, and Mass Psychology
Differences in preventive health behavior based on optimistic bias, hypochondria, and mass psychology were analyzed using the Kruskal–Wallis test. Preventive health behaviors did not show differences based on the level of optimistic bias or hypochondria. However, the results differed according to the level of mass psychology. Post hoc tests revealed that the groups with high (top 25%) and middle (25–75%) levels of mass psychology showed a higher score for preventive health behavior than the group with a low level (bottom 25%) of mass psychology (Table 5).

Table 5.
Preventive health behavior by optimistic bias, hypochondria, mass psychology.
4. Discussion
This study aims to explore the relationship between preventive behaviors, optimistic bias, hypochondria, and mass psychology within the context of the coronavirus pandemic among Korean young adults. Risk perception in Korean young adults showed that individuals without past illness, including COVID-19, had a lower optimistic bias and higher hypochondriasis than those without it. These findings are similar to the study results on optimistic bias about cervical cancer in Korean female college students, stating that optimistic bias diminished as the individual’s involvement in cervical cancer was enhanced [25]. Trobst et al. [26] reported that related experience is positively associated with risk perception. Weinstein [6] stated that people who had not experienced illness or health problems were likely to be optimistic about perceiving health and safety risks, whereas those with past illness or health problems tended to be hypochondriac, characterized by worrying about general health.
Interestingly, our study identified that mass psychology was related to preventive health behavior regarding influenza and COVID-19 but not optimistic bias or hypochondriasis. Mass psychology showed a positive relationship with preventive health behavior, and people with high or middle levels of mass psychology had higher preventive health behavior than those with low levels of mass psychology. These findings are similar to the study result by Park et al., who reported that subjective norms related to parents were a significant factor influencing Korean young adults’ preventive behavior, but perceived susceptibility and severity were not [21].
This may be interpreted in two ways. The first explanation is Korean culture. Korea has a higher tendency for collectivism [27]. Koreans’ strong collectivism helps to solve problems and does not allow an individual’s behavior to cause a conflict or crisis in others or a group of people [28], and an individual is likely to behave like most people in a group. Accordingly, it is interpreted that a person tends to follow other people’s behaviors when the individual recognizes that many people engage in preventive health behaviors around them.
Park and Kim [27] identified Koreans’ cultural self-orientation using a meta-analysis of 41 national studies and reported that Koreans were more likely to be collectivist than individualist as they aged. Our study showed a higher score for mass psychology, especially in those aged 26 years or older compared to those at aged 25 years or younger, which was in accordance with previous studies. In addition, unlike in Western countries, mask-wearing was mostly complied with among all six preventive health behaviors, which can also be explained due to this aspect of Korean culture.
The second explanation is the characteristics of COVID-19. It is probably one of the reasons why optimistic bias or hypochondriasis were not associated with preventive health behavior for influenza and COVID-19 in Korean young adults. The COVID-19 pandemic has evoked extreme fear globally, and societal prevention guidelines would have more influence on preventive health behavior than the person’s risk perception. Although previous studies supported the relationship between risk perception variables, such as optimistic bias or hypochondriasis, and preventive health behavior [9,10,29,30,31], there are other studies showing no relationship [32,33]. Therefore, further studies on risk perception and preventive health behavior need to be conducted, and more studies are necessary to identify the factors that predict preventive health behavior for influenza or COVID-19. The limitations of this study include the failure to conduct a regression analysis to identify factors predicting preventive health behavior due to the non-normal distribution of major variables, despite the sample size of 91 participants.
5. Conclusions
This study concludes that preventive health behaviors for COVID-19 and influenza are associated with mass psychology, that is, the perceived group size in Korean young adults. This may result from Koreans’ strong collectivism and the global phobia that COVID-19 caused. The findings of the study provide useful implications for establishing policies to prevent COVID-19, which are still in progress, and suggest that mass psychology should be effectively applied in planning health communication campaigns for public safety.
Author Contributions
Conceptualization, D.-S.L.; data curation, H.-J.K. and J.-I.K.; formal analysis, D.-S.L.; investigation, S.-O.C.; methodology, D.-S.L.; software, S.-O.C.; writing, Y.S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the research grant of Kangwon National University in 2018.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Kangwon National University (IRB No: KWNUIRB-2022-05-007-001 and 28 May 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the subjects to publish this paper.
Data Availability Statement
The datasets used and/or analyzed in this study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- WHO. Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/?mapFilter=cases (accessed on 1 August 2022).
- KDCA. Coronavirus (COVID-19), Republic of Korea. Available online: http://ncov.mohw.go.kr/en/ (accessed on 1 August 2022).
- Bish, A.; Michie, S. Demographic and Attitudinal Determinants of Protective Behaviors during Pandemic: A review. Br. J. Health Psychol. 2010, 15, 797–824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.; Kim, S. Analysis of the Impact of Health Beliefs and Resource Factors on Preventive Behaviors against the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 8666. [Google Scholar] [CrossRef]
- Kim, J.H.; Yoon, Y.M. An Experimental Study on the Factors Affecting Persuasiveness of Health Messages in AIDS Campaign. Public Relat. 2010, 14, 83–123. [Google Scholar] [CrossRef]
- Weinstein, N.D. Why It Won’t Happen to Me: Perceptions of Risk Factors and Susceptibility. Health Psychol. 1984, 2, 11–20. [Google Scholar] [CrossRef]
- Fragkaki, I.; Maciejewski, D.F.; Weijman, E.L.; Feltes, J.; Cima, M. Human Responses to Covid-19: The Role of Optimism Bias, Perceived Severity, and Anxiety. Personal. Individ. Differ. 2021, 176, 110781. [Google Scholar] [CrossRef]
- Sharot, T. The Optimism bias. Curr. Biol. 2011, 21, R941–R945. [Google Scholar] [CrossRef] [Green Version]
- Park, T.; Ju, I.; Ohs, J.E.; Hinsley, A. Optimistic Bias and Preventive Behavioral Engagement in the Context of COVID-19. Res. Soc. Adm. Pharm. 2021, 17, 1859–1866. [Google Scholar] [CrossRef]
- McColl, K.; Debin, M.; Souty, C.; Guerrisi, C.; Turbelin, C.; Falchi, A.; Bonmarin, I.; Paolotti, D.; Obi, C.; Duggan, J.; et al. Are People Optimistically Biased About the Risk of COVID-19 Infection? Lessons from the First Wave of the Pandemic in Europe. Int. J. Environ. Res. Public Health 2021, 19, 436. [Google Scholar] [CrossRef]
- Warwick, H.M.; Salkovskis, P.M. Hypochondriasis. Behav. Res. Ther. 1990, 28, 105–117. [Google Scholar] [CrossRef]
- Olatunji, B.O.; Deacon, B.J.; Abramowitz, J.S. Is Hypochondriasis an Anxiety Disorder? Br. J. Psychiatry 2009, 194, 481–482. [Google Scholar] [CrossRef]
- Lee, I.H. A Relationship of Personality and Hypochondriacal Illness Attitudes. Korean J. Health Psychol. 2009, 14, 293–311. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Kim, J.H.; Cho, Y.R. Roles of Cognitive Vulnerability and Emotion Dysregulation in Hypochondriacal and Social Anxiety Symptoms Among Undergraduates. Cogn. Behav. Ther. 2015, 15, 113–136. [Google Scholar]
- Lee, I.H. Factor Structure of the Illness Attitudes Scale (IAS) in a Korean College Sample. Korean J. Health Psychol. 2004, 9, 203–218. [Google Scholar]
- Yamaguchi, S. Biased Risk Perceptions Among Japanese: Illusion of Interdependence among Risk Companions. Asian J. Soc. Psychol. 1998, 1, 117–131. [Google Scholar] [CrossRef]
- Ho, A.S.Y.; Leung, K. Group Size Effects on Risk Perception: A Test of Several Hypotheses. Asian J. Soc. Psychol. 1998, 1, 133–145. [Google Scholar] [CrossRef]
- Lee, D.S. A Structural Model Development of Health Insensitivity in Korean Adult. Korean J. Adult Nurs. 2004, 16, 355–365. [Google Scholar]
- Rubin, G.J.; Amlot, R.; Page, L.; Wessely, S. Public Perception, Anxiety, and Behavior Change in Relation to the Swine Flu Outbreak: Cross Sectional Telephone Survey. BMJ 2009, 339, b2651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.; Kim, B.; Kim, K.A. Preventive Behavioral Insights for Emerging Adults: A Survey during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 2569. [Google Scholar] [CrossRef]
- Clarke, V.A.; Lovegrove, H.; Williams, A.; Machperson, M. Unrealistic Optimism and Health Belief Model. J. Behav. Med. 2000, 23, 367–376. [Google Scholar] [CrossRef]
- Kellner, R. Hypochondriasis and Somatization. JAMA 1987, 258, 2718–2722. [Google Scholar] [CrossRef]
- Lee, J.S. The Catastrophizing Tendency of Individuals with High Health Anxiety. Master’s Thesis, Seoul National University, Seoul, Korea, 2004. [Google Scholar]
- Cho, S.Y. A Study on the Relationship Between Cervical Cancer Preventive Behavioral Intentions and Optimistic Bias among Korean Female College Students. Korean J. Commun. Stud. 2018, 26, 101–124. [Google Scholar] [CrossRef]
- Trobst, K.K.; Wiggins, J.S.; Costa, P.T.; Herbst, J.H.; McCrae, R.R.; Masters, H.L. Personality Psychology and Problem Behaviors: HIV Risk and the Five-Factor Model. J. Pers. 2000, 68, 1233–1252. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Kim, S. A Meta-Analytic Review of Koreans’ Cultural Self-Orientation: Focusing on Collectivism and Individualism. Locality Glob. 2018, 42, 5–37. [Google Scholar] [CrossRef]
- Kim, C.D. The Coping Process of Koreans as Compared to White Americans: The Influence of Culture. Korea J. Youth Couns. 1994, 2, 96–113. [Google Scholar]
- Baek, S.Y. A Study on Factors Affecting National Cancer Prevention Practices Health Behavior of Nursing Students. J. Digit. Converg. 2020, 18, 29–37. [Google Scholar] [CrossRef]
- Adachi, M.; Murakami, M.; Yoneoka, D.; Kawashima, T.; Hashizume, M.; Sakamoto, H.; Eguchi, A.; Ghaznavi, C.; Gilmour, S.; Kaneko, S.; et al. Factors Associated with the Risk Perception of COVID-19 Infection and Severe Illness: A Cross-Sectional Study in Japan. SSM Popul. Health 2021, 18, 101–105. [Google Scholar] [CrossRef]
- Son, H.J.; Lee, K.E. The Influence of Health Concern, Health Anxiety, and Communication with Healthcare Providers on Health Information Seeking Behavior on the Internet. J. Health Info. Stat. 2019, 44, 73–82. [Google Scholar] [CrossRef]
- Kim, D.J. Factors Affecting Preventive Behavior for COVID-19 in the Prolonged Pandemic: Focusing on HBM, RISP, Optimistic Bias, and Emotion. Locality Commun. 2022, 26, 5–35. [Google Scholar] [CrossRef]
- Kwon, M.S.; Choi, Y. Factors Affecting Preventive Behavior related to Tuberculosis among University Students in Korea: Focused on Knowledge, Attitude and Optimistic Bias related to Tuberculosis. J. Korean Acad. Fundam. Nurs. 2020, 27, 236–245. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).