Management of Chronic Musculoskeletal Disorders in the Workplace from the Perspective of Older Employees: A Mixed Methods Research Study
Abstract
1. Introduction
2. Materials and Methods
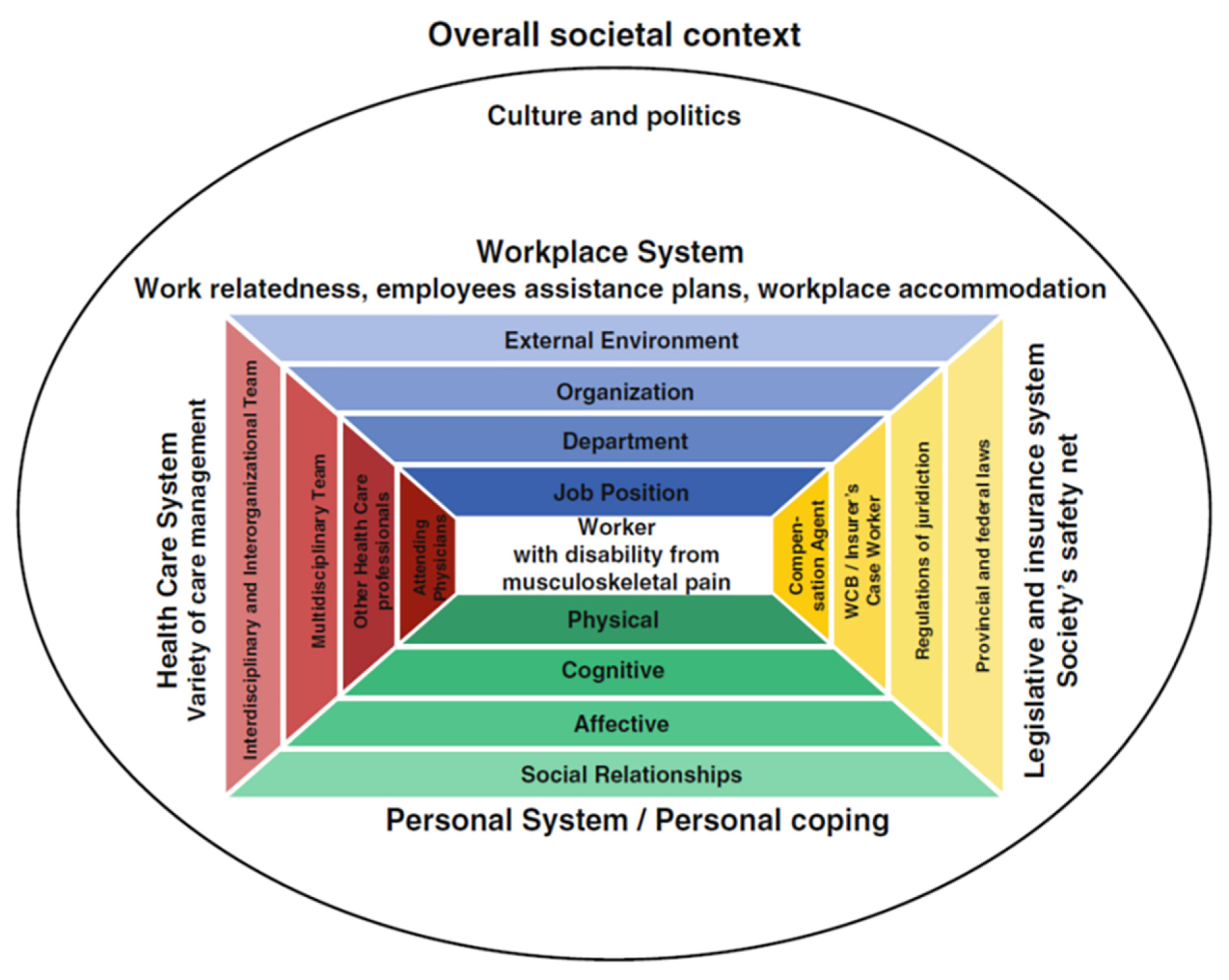
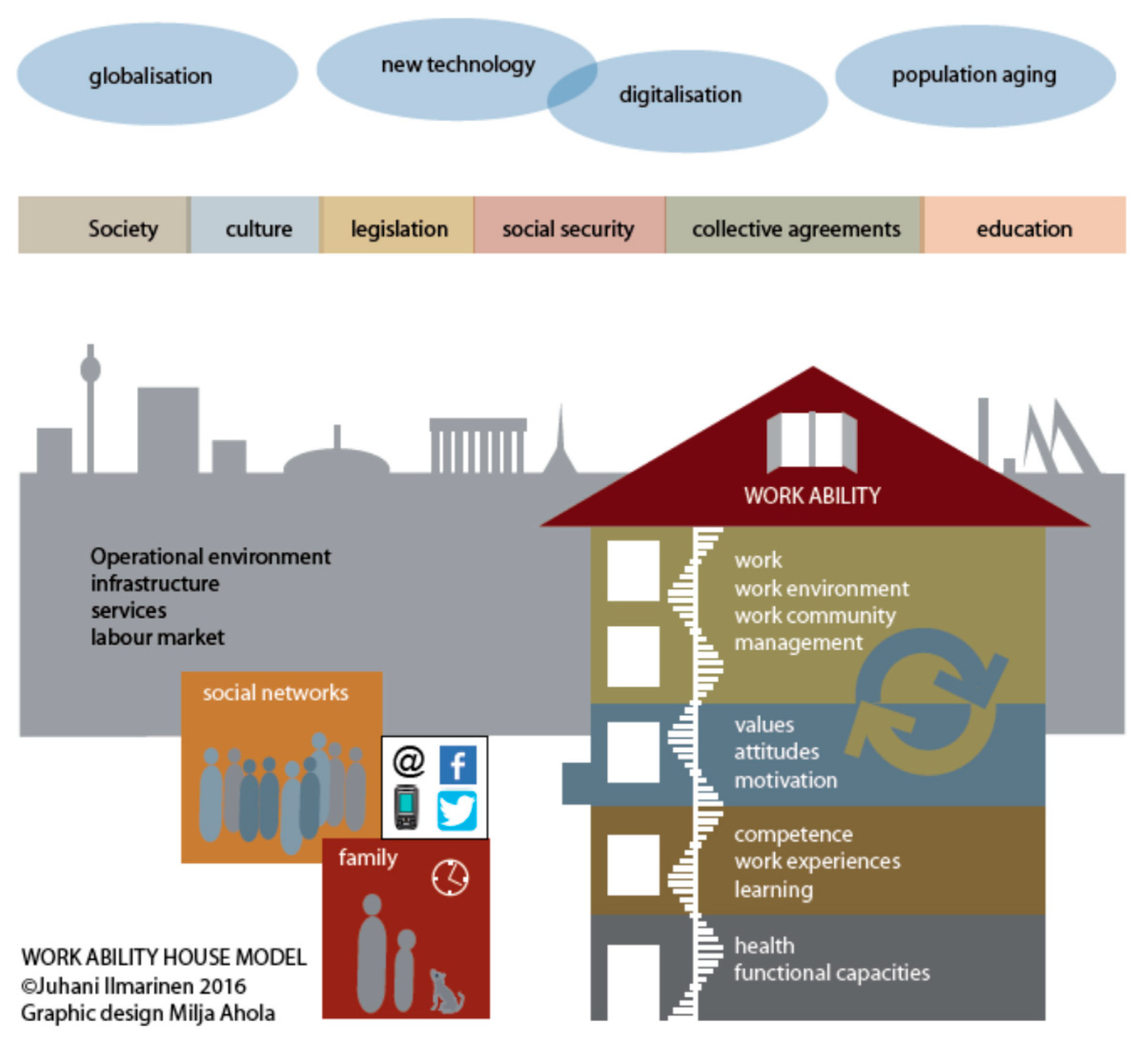
2.1. Using the Arena of Work Disability Prevention Model and the Work Ability House Model
2.2. Ethical Approval
2.3. Participants Selection
2.4. Sampling Strategy for MMR
2.4.1. Sampling Strategy in Qualitative Phase
2.4.2. Sampling Strategy in Quantitative Phase
2.5. Participant Recruitment
2.5.1. Qualitative Phase: Recruitment
2.5.2. Quantitative Phase: Recruitment
2.6. Qualitative Phase: Data Collection
2.7. Qualitative Phase: Data Analysis
2.8. Quantitative Phase: Data Collection
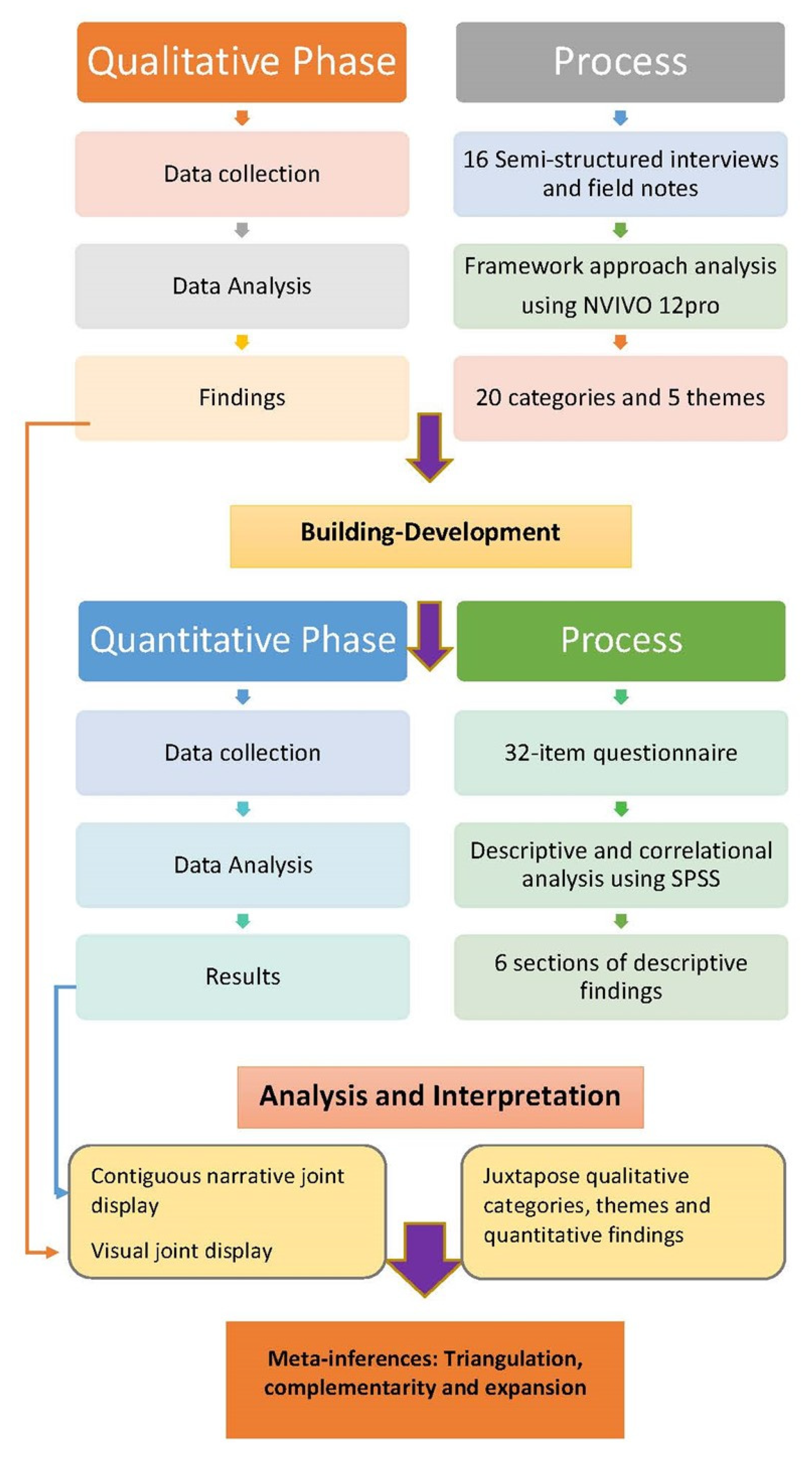
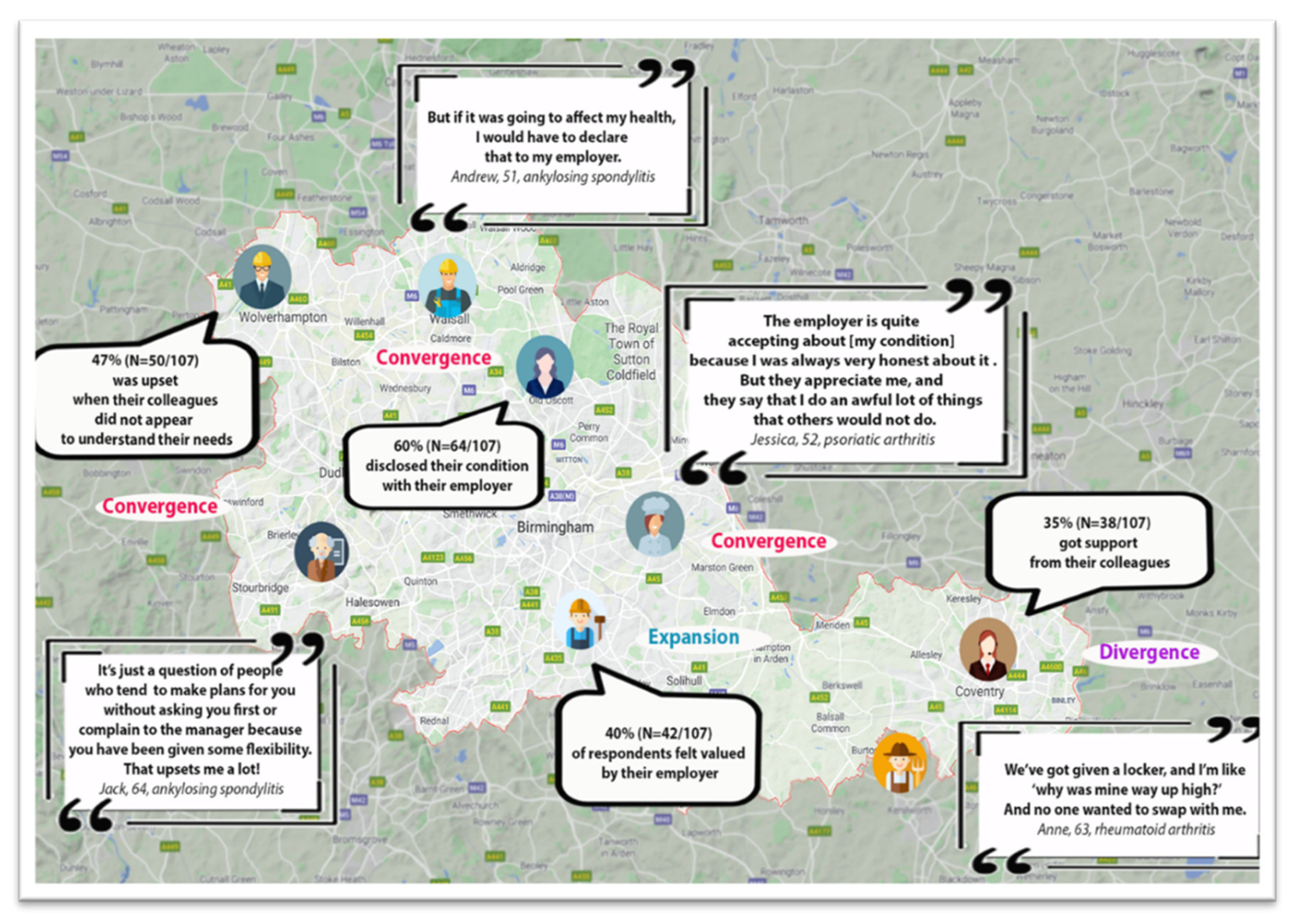
2.9. The Integration Process in an Exploratory Sequential MMR Study
3. Results
“A couple of steps I can manage, but if it is a lot of steps, it just takes me ages to get to them. But you know, sometimes I’m all right. I can do it.”
“So, it tells me, you know, come on you have got only done so many steps this hour, so get up and move.”
“My previous job offered me ‘Flexi-time’, which meant that If I couldn’t always be in at 8:00 [due to a bad night with arthritis], I could stay and work from home and attend the day later. That was really useful and beneficial.”
“My colleague had a hip operation, so you know… him being through his operation and me with my arthritis. So, we have an understanding, if you know what I mean.”
“My physiotherapist is very good. She listens, she understands, and I am happy with the treatment that I have had and the exercises of course.”
“We are all together in a big open plan office and they gave us those awful chairs. They were awful! I mean I literally couldn’t sit for longer than half an hour and I find I’m struggling.”
“I haven’t been asked anything and nobody sat down with me and said OK what is your condition, how bad is it, does it affect your work?”
“I just think people filter it out… people say to me now, ‘oh, you’ve hurt your leg’, because I’m in sandals and they can see that I’ve got a stocking and I’m thinking, no I’ve told you several times.”
“I think the managers are under a lot of pressure and I don’t think that they always have an awful lot of capacity to deal with people that can’t just fit into a standard box for them.”
“Yes, I would work with pain. Because it’s been a feature of my life that I’ve just got used to having, you know… So, for me, you know to have a day that is, ah, the back’s a bit sore means so what?”
“It’s fair to expect people to support you but you have to take responsibility for managing your own health and wellbeing before other people can help you do that.”
“People need to manage their conditions. It’s this animal instinct, where in the world of animals one is injured, one is a predator. The injured animal will always try to walk normally to convey to the predator that they’re not injured.”
“It worries me because it’s a progressive condition and it doesn’t matter what I do. I can stay as well as I can for as long as I can but there will come a point that it will become harder for me to stay mobile and I don’t know whether that’s going to be when I’m 62, 72. And how am I going to work?”
“And I don’t know what I will do if I cannot work, I’m hoping to make it till 60 and then I’ll review things. But I am still helping my daughter financially and I am also looking after my mum you see.”
“So, I will be taking what they call “phased retirement” which is the ideal thing for me. I could go down to 2 days; I can go down one more day before I actually fully retire.”
4. Discussion
4.1. Older Employees with CMSDs Face Uncertainty
4.2. Social Support for the Disclosure and Management of CMSDs
4.3. Presenteeism: Why Do Employees Come to Work When Unwell?
4.4. Presenteeism in Employees with Chronic Inflammatory Disorders (CIDs)
4.5. The Phenomenon of Leaveism
4.6. The Impact of State Pension Age Changes on Retirement
4.7. The Influence of Gender on the Transition to Retirement
4.8. Roles and Responsibilities of Employers in Supporting Employees
4.9. The Role of the Manager in Supporting Older Employees
4.10. The Role of Self-Management and Professional Health Services in Supporting Older Employees with CMSDs
4.11. Strengths and Limitations of the Study
- Discrepancies exist between how employers, managers and supervisors interpret and implement current employment policies and strategies to support older employees in managing CMSDs at work.
- The social context of the workplace and the positive attitudes and understanding of colleagues and managers significantly contribute to how older employees view their future work ability and how they manage CMSDs in the workplace.
- The involvement of relevant healthcare professionals can make an important contribution to supporting work adjustments, translating best evidence into practice and assisting managers and employers to build an inclusive work environment and individualised strategies for employees with CMSDs.
- Research related to OHS provision should be developed that encompasses the impact on work of musculoskeletal health and the co-existence of multiple chronic conditions, particularly in relation to the ageing workforce and subgroups such as women.
4.12. Recommendations for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- European Musculoskeletal Health Surveillance and Infomation Network, Executive Agency for Health and Consumers Musculoskeletal Health in Europe Report v5.0. Exec. Agency Health Consum. 2014, 1–13. Available online: http://www.eumusc.net/myUploadData/files/MusculoskeletalHealthinEuropeReportSummaryKEWIP.pdf (accessed on 18 October 2021).
- Parsons, S.; Symmons, D.P. The burden of musculoskeletal conditions. Medicine 2014, 42, 190–192. [Google Scholar] [CrossRef]
- Briggs, A.M.; Shiffman, J.; Shawar, Y.R.; Åkesson, K.; Ali, N.; Woolf, A.D. Global health policy in the 21st century: Challenges and opportunities to arrest the global disability burden from musculoskeletal health conditions. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101549. [Google Scholar] [CrossRef]
- Kyu, H.H.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study. Lancet 2018, 392, 1859–1922. [Google Scholar] [CrossRef]
- Schneider, E.; Irastorza, X. Work-Related Musculoskeletal Disorders in the EU—Facts and Figures. 2010. pp. 1–184. Available online: https://osha.europa.eu/en/tools-and-publications/publications/reports/TERO09009ENC (accessed on 18 October 2021).
- National Academies of Sciences and Medicine Engineering Musculoskeletal Disorders. In Selected Health Conditions and Likelihood of Improvement with Treatment; The National Academies Press: Washington, DC, USA, 2020; p. 318. Available online: https://www.ncbi.nlm.nih.gov/books/NBK559512/ (accessed on 9 May 2022).
- Schwarzkopf, S.R.; Ewert, T.; Dreinhöfer, K.E.; Cieza, A.; Stucki, G. Towards an ICF Core Set for chronic musculoskeletal conditions: Commonalities across ICF Core Sets for osteoarthritis, rheumatoid arthritis, osteoporosis, low back pain and chronic widespread pain. Clin. Rheumatol. 2008, 27, 1355–1361. [Google Scholar] [CrossRef]
- UK Government DPTAC Position Statement on Non-Visible Disabilities. 2020. Available online: https://www.gov.uk/government/publications/dptac-position-on-non-visible-disabilities/dptac-position-statement-on-non-visible-disabilities (accessed on 18 October 2021).
- EU-OSHA Priorities for Occupational Safety and Health Research in Europe: 2013–2020. 2013. pp. 1–107. Available online: https://osha.europa.eu/en/publications/priorities-occupational-safety-and-health-research-europe-2013-2020/view (accessed on 18 October 2020).
- Grant, D. Older women, work and the impact of discrimination. In Age Discrimination and Diversity: Multiple Discrimination from an Age Perspective; Sargeant, M., Ed.; Cambridge University Press: Cambridge, UK, 2011; pp. 41–64. [Google Scholar]
- Office for National Statistics (ONS) Female Employment Rate (Aged 16 to 64, Seasonally Adjusted). 2021. Available online: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/timeseries/lf25/lms (accessed on 18 October 2020).
- ONS World Population Ageing. United Nations, Dep. Econ. Soc. Aff. Popul. Div. 2015. p. 164. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Report.pdf (accessed on 15 October 2021).
- Health and Safety Executive (HSE) Work-Related Musculoskeletal Disorders Statistics in Great Britain. 2021. pp. 1–22. Available online: https://www.hse.gov.uk/statistics/causdis/msd.pdf (accessed on 2 July 2022).
- DWP. State Pension Age Review. 2017. pp. 1–38. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/630065/state-pension-age-review-final-report.pdf (accessed on 15 June 2019).
- Lewis, R.; Gómez Álvarez, C.B.; Rayman, M.; Lanham-New, S.; Woolf, A.; Mobasheri, A. Strategies for optimising musculoskeletal health in the 21st century. BMC Musculoskelet. Disord. 2019, 20, 164–179. [Google Scholar] [CrossRef]
- DHSC; DWP. Improving Health and Work: Changing Lives. 2008. pp. 1–107. Available online: https://www.gov.uk/government/publications/improving-health-and-work-changing-lives (accessed on 15 October 2021).
- Phillipson, C.; Smith, A. Extending Working Life: A Review of the Research Literature. DWP Res. Reports 299. 2005. pp. 1–299. Available online: https://www.iser.essex.ac.uk/research/publications/508056 (accessed on 15 February 2015).
- Versus Arthritis. The State of Musculoskeletal Health. 2019. Available online: https://www.versusarthritis.org/media/14594/state-of-musculoskeletal-health-2019.pdf (accessed on 10 May 2022).
- DWP. Your State Pension Explained. 2020. Available online: https://www.gov.uk/government/publications/your-new-state-pension-explained/your-state-pension-explained (accessed on 15 October 2021).
- Altmann, R. A New Vision for Older Workers: Retain, Retrain, Recruit. DWP Rep. 2015. pp. 1–64. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/411420/a-new-vision-for-older-workers.pdf (accessed on 15 October 2020).
- DWP; DHSC. Understanding Private Providers of Occupational Health Services. Res. Rep. no. 72. 2019. pp. 1–19. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/848173/understanding_-private-providers-of-occupational-health-services.pdf (accessed on 15 October 2020).
- National Institute for Health and Care Excellence (NICE) Workplace Health: Management Practices. Nice Guideline 13. NG13. 2015. p. 54. Available online: https://www.nice.org.uk/guidance/ng13/resources/workplace-health-management-practices-1837269751237 (accessed on 18 October 2021).
- NICE Workplace Health: Long-Term Sickness Absence and Capability to Work. [NG146]. 2019. Available online: https://www.nice.org.uk/guidance/ng146/chapter/Recommendations (accessed on 5 May 2022).
- Koma, B.S.; Bergh, A.-M.; Costa-Black, K.M. Barriers to and facilitators for implementing an office ergonomics programme in a South African research organisation. Appl. Ergon. 2019, 75, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Taylor, K.; Daniel, J. Musculoskeletal Disorders in the Workplace: The Role of HR and Line Managers. Pers. Today. 2015. Available online: http://www.personneltoday.com/hr/musculoskeletal-disorders-in-the-workplace-the-role-of-hr-and-line-managers/ (accessed on 18 October 2021).
- Coole, C.; Birks, E.; Watson, P.J.; Drummond, A. Communicating with employers: Experiences of occupational therapists treating people with musculoskeletal conditions. J. Occup. Rehabil. 2014, 24, 585–595. [Google Scholar] [CrossRef]
- Vornholt, K.; Villotti, P.; Muschalla, B.; Bauer, J.; Colella, A.; Zijlstra, F.; Ruitenbeek, G.V.; Uitdewilligen, S.; Corbière, M. Disability and employment—Overview and highlights. Eur. J. Work Organ. Psychol. 2018, 27, 40–55. [Google Scholar] [CrossRef]
- Costa-Black, K.M.; Feuerstein, M.; Loisel, P. Work Disability Models: Past and Present. In Handbook of Work Disability; Springer: New York, NY, USA, 2013; pp. 71–93. Available online: http://link.springer.com/10.1007/978-1-4614-6214-9_6 (accessed on 15 June 2022).
- Lederer, V.; Loisel, P.; Rivard, M.; Champagne, F. Exploring the Diversity of Conceptualizations of Work (Dis)ability: A Scoping Review of Published Definitions. J. Occup. Rehabil. 2014, 24, 242–267. [Google Scholar] [CrossRef]
- Andreas, L.S. A Tailored Learning Program for Prevention of Musculoskeletal Disorders. J. Ergon. 2015, 1–7. Available online: http://www.omicsgroup.org/journals/a-tailored-learning-program-for-prevention-of-musculoskeletal-disorders-2165-7556.S4-002.php?aid=26003 (accessed on 18 October 2021). [CrossRef]
- Franche, R.-L.; Cullen, K.; Clarke, J.; Irvin, E.; Sinclair, S.; Frank, J. Workplace-Based Return-to-Work Interventions: A Systematic Review of the Quantitative Literature. J. Occup. Rehabil. 2005, 15, 607–631. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.; Rees, S.; Underwood, M.; Froud, R. Obstacles to returning to work with chronic pain: In-depth interviews with people who are off work due to chronic pain and employers. BMC Musculoskelet. Disord. 2019, 20, 486. [Google Scholar] [CrossRef] [PubMed]
- Jezukaitis, P.; Kapur, D. Management of occupation-related musculoskeletal disorders. Best Pract. Res. Clin. Rheumatol. 2011, 25, 117–129. [Google Scholar] [CrossRef] [PubMed]
- Prall, J.; Ross, M. The management of work-related musculoskeletal injuries in an occupational health setting: The role of the physical therapist. J. Exerc. Rehabil. 2019, 15, 193–199. [Google Scholar] [CrossRef]
- van Eerd, D.; Munhall, C.; Irvin, E.; Rempel, D.; Brewer, S.; van Der Beek, A.; Dennerlein, J.; Tullar, J.; Skivington, K.; Pinion, C.; et al. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: An update of the evidence. Occup. Environ. Med. 2015, 73, 62–70. [Google Scholar] [CrossRef]
- Gay, C.; Chabaud, A.; Guilley, E.; Coudeyre, E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Ann. Phys. Rehabil. Med. 2016, 59, 174–183. [Google Scholar] [CrossRef]
- Du, S.; Yuan, C.; Xiao, X.; Chu, J.; Qiu, Y.; Qian, H. Self-management programs for chronic musculoskeletal pain conditions: A systematic review and meta-analysis. Patient Educ. Couns. 2011, 85, e299–e310. [Google Scholar] [CrossRef]
- Skamagki, G.; King, A.; Duncan, M.; Wåhlin, C. A systematic review on workplace interventions to manage chronic musculoskeletal conditions. Physiother. Res. Int. 2018, 23, 1–16. [Google Scholar] [CrossRef]
- Sundstrup, E.; Seeberg, K.G.V.; Bengtsen, E.; Andersen, L.L. A Systematic Review of Workplace Interventions to Rehabilitate Musculoskeletal Disorders Among Employees with Physical Demanding Work. J. Occup. Rehabil. 2020, 30, 588–612. [Google Scholar] [CrossRef]
- Tashakkori, A.; Johnson, R.B.; Teddlie, C. Foundations of Mixed Methods Research: Integrating Quantitative and Qualitative Approaches in the Social and Behavioral Sciences, 2nd ed.; Sage Publications Inc.: Thousand Oaks, CA, USA, 2021. [Google Scholar]
- Creswell, J.W.; Plano-Clark, V. Designing and Conducting Mixed Methods Research, 3rd ed.; Sage Publications Inc.: Thousand Oaks, CA, USA, 2017. [Google Scholar]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving integration in mixed methods designs—Principles and practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef]
- Creswell, J.; Plano-Clark, V.; Gutmann, M.; Hanson, W. Advanced Mixed Methods Research Designs. Handb. Mix. Methods Soc. Behav. Res. 2003, 209–240. Available online: http://www.sagepub.com/upm-data/19291_Chapter_7.pdf (accessed on 10 May 2020).
- Morgan, D.L. Pragmatism as a Paradigm for Social Research. Qual. Inq. 2014, 20, 1045–1053. [Google Scholar] [CrossRef]
- Official Labour Market Statistics Labour Market Profile. Nomis. 2019. Available online: https://www.nomisweb.co.uk/reports/lmp/gor/2013265925/report.aspx#tabrespop (accessed on 18 October 2021).
- van der Klink, J.J.; Bültmann, U.; Burdorf, A.; Schaufeli, W.B.; Zijlstra, F.R.; Abma, F.I.; Brouwer, S.; van der Wilt, G.J. Sustainable employability—Definition, conceptualization, and implications: A perspective based on the capability approach. Scand. J. Work. Environ. Health 2016, 42, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Tengland, P.-A. The Concept of Work Ability. J. Occup. Rehabil. 2011, 21, 275–285. [Google Scholar] [CrossRef]
- Loisel, P. Intervention for return to work-What is really effective? Scand. J. Work. Environ. Health 2005, 31, 245–247. [Google Scholar] [CrossRef][Green Version]
- Ilmarinen, J.; Ilmarinen, V. Work ability and aging. In Facing the Challenges of a Multi-Age Workforce: A Use-Inspired Approach; SIOP Organizational Frontiers Series; Routledge/Taylor & Francis Group: New York, NY, USA, 2015; pp. 134–156. [Google Scholar]
- Loisel, P.; Buchbinder, R.; Hazard, R.; Keller, R.; Scheel, I.; van Tulder, M.; Webster, B. Prevention of work disability due to musculoskeletal disorders: The challenge of implementing evidence. J. Occup. Rehabil. 2005, 15, 507–524. [Google Scholar] [CrossRef]
- Loisel, P.; Durand, M.J.; Berthelette, D.; Vézina, N.; Baril, R.; Gagnon, D.; Larivière, C.; Tremblay, C. Disability Prevention: New Paradigm for the Management of Occupational Back Pain. Dis. Manag. Health Outcomes 2001, 9, 351–360. [Google Scholar] [CrossRef]
- Ilmarinen, J.; von Bonsdorff, M. Work Ability. In The Encyclopedia of Adulthood and Aging; American Cancer Society: Atlanta, GA, USA, 2015; pp. 1–5. [Google Scholar]
- Nordenfelt, L. The Concept of Work Ability; PIE Peter Lang: Brussels, Belgium, 2008. [Google Scholar]
- Lavrakas, P.; Battaglia, M.P. Nonprobability Sampling. In Encyclopedia of Survey Research Methods; Sage Publications: Thousand Oaks, CA, USA, 2008; pp. 523–526. [Google Scholar]
- Bryman, A. Social Research Methods, 5th ed.; Oxford University Press: Oxford, UK, 2016. [Google Scholar]
- Carpenter, C.; Suto, M. Qualitative Research for Occupational and Physical Therapists: A Practical Guide; Wiley-Blackwell: Oxford, UK, 2008. [Google Scholar]
- Liamputtong, P. (Ed.) Research Methods in Health: Foundations for Evidence-Based Practice, 2nd ed.; Oxford University Press: Victoria, Australia, 2013. [Google Scholar]
- Johnson, B.; Christensen, L. Educational Research, 7th ed.; Sage Publications Inc.: Thousand Oaks, CA, USA, 2020. [Google Scholar]
- Carpenter, C. Phenomenology and rehabilitation research. In Research Methods in Health: Foundations for Evidence-Based Practice; Liamputtong, P., Ed.; Oxford University Press: Victoria, Australia, 2013; pp. 115–131. [Google Scholar]
- Smith, J.; Firth, J. Qualitative data analysis: The framework approach. Nurse Res. 2011, 8, 52–62. [Google Scholar] [CrossRef]
- Spencer, L.; Ritchie, J.; Lewis, J.; Dillon, L. Quality in Qualitative Evaluation: A framework for assessing research evidence. Soc. Res. 2003, 1–123. Available online: http://www.civilservice.gov.uk/wp-content/uploads/2011/09/Quality-in-qualitative-evaulation_tcm6-38739.pdf (accessed on 10 January 2020).
- Spencer, L.; Ritchie, J.; O’Connor, W.; Morrell, G.; Ormston, R. Analysis in practice. In Qualitative Research Practice: A Guide for Social Science Students and Researchers; Ritchie, J., Lewis, J., Carol, M.N., Ormston, R., Eds.; Sage Publications Ltd.: Thousand Oaks, CA, USA, 2014; pp. 295–346. [Google Scholar]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.T.; Walker-Bone, K.; Harris, E.C.; Linaker, C.; D’Angelo, S.; Sayer, A.A.; Gale, C.R.; Evandrou, M.; van Staa, T.; Cooper, C.; et al. Health and Employment after Fifty (HEAF): A new prospective cohort study. BMC Public Health 2015, 15, 1071. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.O. The Nordic Musculoskeletal Questionnaire. Occup. Med. 2007, 57, 300–301. [Google Scholar] [CrossRef]
- Ilmarinen, J. The Work Ability Index (WAI). Occup. Med. 2007, 57, 160. [Google Scholar] [CrossRef]
- 2016/679, R. (EU) Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/EC Da. 2016. Available online: https://www.legislation.gov.uk/eur/2016/679/contents# (accessed on 10 May 2021).
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; Sage Publications Inc.: London, UK, 2018. [Google Scholar]
- Plano-Clark, V.; Ivankova, N. Mixed Methods Research: A Guide to the Field; Sage Publications Inc.: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Teddlie, C.; Tashakkori, A. Handbook of Mixed Methods in Social and Behavioral Research; Sage Publications: Thousand Oaks, CA, USA, 2010. [Google Scholar]
- Fetters, M.D. The Mixed Methods Research Workbook Activities for Designing, Implementing, and Publishing Projects; Sage Publications, Inc.: Thousand Oaks, CA, USA, 2020. [Google Scholar]
- Moreton, B.J.; Tew, V.; das Nair, R.; Wheeler, M.; Walsh, D.A.; Lincoln, N.B. Pain phenotype in patients with knee osteoarthritis: Classification and measurement properties of pain and self-report Leeds assessment of neuropathic symptoms and signs scale in a cross-sectional study. Arthritis Care Res. 2015, 67, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Burston, J.J.; Valdes, A.M.; Woodhams, S.G.; Mapp, P.I.; Stocks, J.; Watson, D.J.G.; Gowler, P.R.W.; Xu, L.; Sagar, D.R.; Fernandes, G.; et al. The impact of anxiety on chronic musculoskeletal pain and the role of astrocyte activation. Pain 2019, 160, 658–669. [Google Scholar] [CrossRef]
- Smith, S.A.; Brunner, S.R. To reveal or conceal: Using communication privacy management theory to understand disclosures in the workplace. Manag. Commun. Q. 2017, 31, 429–446. [Google Scholar] [CrossRef]
- Kinman, G.; Wray, S. Presenteeism in academic employees—occupational and individual factors. Occup. Med. (Chic. Ill) 2018, 68, 46–50. [Google Scholar] [CrossRef]
- Miraglia, M.; Johns, G. Going to work ill: A meta-analysis of the correlates of presenteeism and a dual-path model. J. Occup. Health Psychol. 2016, 21, 261–283. [Google Scholar] [CrossRef]
- Garrow, V. Presenteeism: A Review of Current Thinking. Rep. 507. 2016. pp. 1–89. Available online: https://www.employment-studies.co.uk/resource/presenteeism-review-current-thinking (accessed on 18 October 2021).
- Carder, M.; McNamee, R.; Turner, S.; Hodgson, J.T.; Holland, F.; Agius, R.M. Time trends in the incidence of work-related mental ill-health and musculoskeletal disorders in the UK. Occup. Environ. Med. 2013, 70, 317–324. [Google Scholar] [CrossRef]
- Coole, C.; Drummond, A.; Watson, P.J.; Radford, K. What Concerns Workers with Low Back Pain? Findings of a Qualitative Study of Patients Referred for Rehabilitation. J. Occup. Rehabil. 2010, 20, 472–480. [Google Scholar] [CrossRef] [PubMed]
- Hutting, N.; Heerkens, Y.F.; Engels, J.A.; Staal, J.B.; Nijhuis-van der Sanden, M.W. Experiences of employees with arm, neck or shoulder complaints: A focus group study. BMC Musculoskelet. Disord. 2014, 15, 141–153. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wynne-Jones, G.; Buck, R.; Porteous, C.; Cooper, L.; Button, L.A.; Main, C.J.; Phillips, C.J. What happens to work if you’re unwell? Beliefs and attitudes of managers and employees with musculoskeletal pain in a public sector setting. J. Occup. Rehabil. 2011, 21, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Dietz, C.; Scheel, T. Leadership and Presenteeism among Scientific Staff: The Role of Accumulation of Work and Time Pressure. Front. Psychol. 2017, 8, 1885. [Google Scholar] [CrossRef]
- Duff, A.J.; Podolsky, M.; Biron, M.; Chan, C.C.A. The interactive effect of team and manager absence on employee absence: A multilevel field study. J. Occup. Organ. Psychol. 2015, 88, 61–79. [Google Scholar] [CrossRef]
- Ruhle, S.A.; Breitsohl, H.; Aboagye, E.; Baba, V.; Biron, C.; Correia Leal, C.; Dietz, C.; Ferreira, A.I.; Gerich, J.; Johns, G.; et al. “To work, or not to work, that is the question”—Recent trends and avenues for research on presenteeism. Eur. J. Work Organ. Psychol. 2020, 29, 344–363. [Google Scholar] [CrossRef]
- McGonagle, A.; Roebuck, A.; Diebel, H.; Aqwa, J.; Fragoso, Z.; Stoddart, S. Anticipated work discrimination scale: A chronic illness application. J. Manag. Psychol. 2016, 31, 61–78. [Google Scholar] [CrossRef]
- Silvaggi, F.; Eigenmann, M.; Scaratti, C.; Guastafierro, E.; Toppo, C.; Lindstrom, J.; Rantala, E.; Imaz-Iglesia, I.; Barnfield, A.; Maassen, A.; et al. Employment and Chronic Diseases: Suggested Actions for The Implementation of Inclusive Policies for The Participation of People with Chronic Diseases in the Labour Market. Int. J. Environ. Res. Public Health 2020, 17, 820. [Google Scholar] [CrossRef]
- Pager, D.; Shepherd, H. The Sociology of Discrimination: Racial Discrimination in Employment, Housing, Credit, and Consumer Markets. Annu. Rev. Sociol. 2008, 34, 181–209. [Google Scholar] [CrossRef]
- Strömberg, C.; Aboagye, E.; Hagberg, J.; Bergström, G.; Lohela-Karlsson, M. Estimating the Effect and Economic Impact of Absenteeism, Presenteeism, and Work Environment–Related Problems on Reductions in Productivity from a Managerial Perspective. Value Health 2017, 20, 1058–1064. [Google Scholar] [CrossRef]
- Jinnett, K.; Schwatka, N.; Tenney, L.; Brockbank, C.; Newman, L. Chronic Conditions, Workplace Safety, And Job Demands Contribute To Absenteeism And Job Performance. Health Aff. 2017, 36, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Higgins, A.; O’Halloran, P.; Porter, S. Management of long term sickness absence: A systematic realist review. J. Occup. Rehabil. 2012, 22, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Hammond, A.; Sutton, C.; Cotterill, S.; Woodbridge, S.; O’Brien, R.; Radford, K.; Forshaw, D.; Verstappen, S.; Jones, C.; Marsden, A.; et al. The effect on work presenteeism of job retention vocational rehabilitation compared to a written self-help work advice pack for employed people with inflammatory arthritis: Protocol for a multi-centre randomised controlled trial (the WORKWELL trial). BMC Musculoskelet. Disord. 2020, 21, 607–627. [Google Scholar] [CrossRef]
- Holland, P.; Collins, A.M. “Whenever I can I push myself to go to work”: A qualitative study of experiences of sickness presenteeism among workers with rheumatoid arthritis. Disabil. Rehabil. 2016, 40, 404–413. [Google Scholar] [CrossRef]
- Holland, P.; Collins, A.M. Supporting and retaining employees with rheumatoid arthritis: The importance of workplace social support. Int. J. Hum. Resour. Manag. 2020, 33, 539–560. [Google Scholar] [CrossRef]
- Hesketh, I.; Cooper, C.L.; Ivy, J. Leaveism and Work–Life Integration: The Thinning Blue Line? Polic. A J. Policy Pract. 2014, 9, 183–194. [Google Scholar] [CrossRef]
- Hesketh, I.; Cooper, C.L. Leaveism at work. Occup. Med. 2014, 64, 146–147. [Google Scholar] [CrossRef]
- Gerich, J. Leaveism and illness-related behaviour. Occup. Med. 2015, 65, 746–752. [Google Scholar] [CrossRef][Green Version]
- Brown, P.; Vickerstaff, S. Health subjectivities and labor market participation: Pessimism and older workers’ attitudes and narratives around retirement in the United Kingdom. Res. Aging 2011, 33, 529–550. [Google Scholar] [CrossRef]
- Andersen, L.L.; Jensen, P.H.; Sundstrup, E. Barriers and opportunities for prolonging working life across different occupational groups: The Senior Working Life study. Eur. J. Public Health 2020, 30, 241–246. [Google Scholar] [CrossRef]
- Schofield, D.J.; Shrestha, R.N.; Percival, R.; Callander, E.J.; Kelly, S.J.; Passey, M.E. Early retirement and the financial assets of individuals with back problems. Eur. Spine J. 2011, 20, 731–736. [Google Scholar] [CrossRef]
- EU-OSHA Safer and Healthier Work at Any Age: Review of Resources for Workplaces. 2016. pp. 1–55. Available online: https://osha.europa.eu/en/publications/safer-and-healthier-work-any-age-review-resources-workplaces/view (accessed on 22 April 2018).
- Sharma, N.; Chakrabarti, S.; Grover, S. Gender differences in caregiving among family—Caregivers of people with mental illnesses. World J. Psychiatry 2016, 6, 7–17. [Google Scholar] [CrossRef]
- Heise, L.; Greene, M.; Opper, N.; Stavropoulou, M.; Harper, C.; Nascimento, M.; Zewdie, D.; Darmstadt, G.L.; Greene, M.E.; Hawkes, S.; et al. Gender inequality and restrictive gender norms: Framing the challenges to health. Lancet 2019, 393, 2440–2454. [Google Scholar] [CrossRef]
- ONS Understanding the Gender Pay Gap in the UK. Understanding Gender pay gap UK. 2018. pp. 1–33. Available online: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/articles/understandingthegenderpaygapintheuk/2018-01-17 (accessed on 16 October 2021).
- Trades Union Congress Women over 50 in the Workplace. 2014. pp. 1–36. Available online: https://www.tuc.org.uk/research-analysis/reports/women-over-50-workplace-tuc-report (accessed on 18 October 2021).
- Pensions Policy Institute Understanding the Gender Pensions Gap. 2019. p. 54. Available online: www.pensionspolicyinstitute.org.uk (accessed on 18 October 2021).
- ONS Living Longer: Caring in Later Working Life. 2019. pp. 1–11. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/ageing/articles/livinglongerhowourpopulationischangingandwhyitmatters/2019-03-15 (accessed on 18 October 2021).
- DWP; DHSC. Employers’ Motivations and Practices: A Study of the Use of Occupational Health Services. DWP Res. Rep. no. 979. 2020. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/789894/employers-motivations-and-practices-a-study-of-the-use-of-occupational-health-services.pdf (accessed on 15 October 2020).
- Pescud, M.; Teal, R.; Shilton, T.; Slevin, T.; Ledger, M.; Waterworth, P.; Rosenberg, M. Employers’ views on the promotion of workplace health and wellbeing: A qualitative study. BMC Public Health 2015, 15, 642. [Google Scholar] [CrossRef]
- Business in the Community; Public Health England Musculoskeletal Health in the Workplace A Toolkit for Employers. 2019. p. 74. Available online: https://www.bitc.org.uk/wp-content/uploads/2019/10/bitc-wellbeing-toolkit-musculoskeletal-mar2017.pdf (accessed on 10 April 2020).
- Public Health England. Musculoskeletal Health: Applying All Our Health. 2019. Available online: https://www.gov.uk/government/publications/musculoskeletal-health-applying-all-our-health/musculoskeletal-health-applying-all-our-health (accessed on 7 April 2022).
- NICE Developing NICE Guidelines: The Manual. 2020. Available online: https://www.nice.org.uk/process/pmg20/chapter/the-validation-process-for-draft-guidelines-and-dealing-with-stakeholder-comments (accessed on 18 October 2021).
- Robertson, H. Improving Lives or a damp squib? TUC. 2017. Available online: https://www.tuc.org.uk/blogs/improving-lives-or-damp-squib (accessed on 10 May 2022).
- Flynn, M. Representing an Ageing Workforce: Challenges and Opportunities for Trade Unions. Trades Union Congr. 2014, 1–50. Available online: https://www.tuc.org.uk/research-analysis/reports/representing-ageing-workforce-challenges-and-opportunities-trade-unions (accessed on 18 October 2021).
- Kitson, A.L.; Rycroft-Malone, J.; Harvey, G.; McCormack, B.; Seers, K.; Titchen, A. Evaluating the successful implementation of evidence into practice using the PARiHS framework: Theoretical and practical challenges. Implement. Sci. 2008, 3, 1. [Google Scholar] [CrossRef] [PubMed]
- Jensen, I.B.; Björk Brämberg, E.; Wåhlin, C.; Björklund, C.; Hermansson, U.; Lohela Karlson, M.; Schäfer Elinder, L.; Munck af Rosenschöld, P.; Nevala, T.; Carter, N.; et al. Promoting Evidence-Based Practice for Improved Occupational Safety and Health at Workplaces in Sweden. Report on a Practice-Based Research Network Approach. Int. J. Environ. Res. Public Health 2020, 17, 5283–5298. [Google Scholar] [CrossRef]
- Steadman, K.; Wood, M.; Silvester, H. Health and Well-Being at Work: A Survey of Employees. Res. Rep. No 901. 2014. pp. 1–104. Available online: https://www.gov.uk/government/publications/health-and-wellbeing-at-work-survey-of-employees (accessed on 18 October 2021).
- Bartys, S.; Edmondson, A.; Burton, K. Work Conversations in Healthcare: How, Where, When and by Whom? Public Health Engl. 2019, 90. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832876/Work_Conversations_in_Healthcare_How_where_when_and_by_whom.pdf (accessed on 17 October 2021).
- Oakman, J.; Briggs, A.; Kinsman, N.; Bywaters, L. Working with Pain: What can Workplaces Do to Support Employees with Persistent Musculoskeletal Pain to Maintain Productive Employment. Arthritis Osteoporos. Victoria. Melbourne, Australia; 2015. pp. 1–36. Available online: https://www.msk.org.au/wp-content/uploads/2018/07/Working-with-pain.pdf (accessed on 18 October 2021).
- Hoosain, M.; de Klerk, S.; Burger, M. Workplace-Based Rehabilitation of Upper Limb Conditions: A Systematic Review. J. Occup. Rehabil. 2019, 29, 175–193. [Google Scholar] [CrossRef] [PubMed]
- Otterbring, T.; Pareigis, J.; Wästlund, E.; Makrygiannis, A.; Lindström, A. The relationship between office type and job satisfaction: Testing a multiple mediation model through ease of interaction and well-being. Scand. J. Work. Environ. Health 2018, 44, 330–334. [Google Scholar] [CrossRef] [PubMed]
- Bosma, A.R.; Boot, C.R.L.; Snippen, N.C.; Schaafsma, F.G.; Anema, J.R. Supporting employees with chronic conditions to stay at work: Perspectives of occupational health professionals and organizational representatives. BMC Public Health 2021, 21, 564–592. [Google Scholar] [CrossRef] [PubMed]
- Hutting, N.; Oswald, W.; Staal, J.B.; Engels, J.A.; Nouwens, E.; Nijhuis-van der Sanden, M.W.G.; Heerkens, Y.F. The contribution of physiotherapy to the employment of workers with a chronic musculoskeletal disorder: A focus group study. Eur. J. Physiother. 2017, 19, 51–53. [Google Scholar] [CrossRef]
- Hutting, N.; Boucaut, R.; Gross, D.P.; Heerkens, Y.F.; Johnston, V.; Skamagki, G.; Stigmar, K. Work-Focused Health Care: The Role of Physical Therapists. Phys. Ther. 2020, 100, 2231–2236. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, R.; Bjork, M.; Costa-Black, K.M.; Parker, M.; Pransky, G. Managing work participation for people with rheumatic and musculoskeletal diseases. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101517. [Google Scholar] [CrossRef]
- Wynne-Jones, G.; Artus, M.; Bishop, A.; Lawton, S.A.; Lewis, M.; Jowett, S.; Kigozi, J.; Main, C.; Sowden, G.; Wathall, S.; et al. Effectiveness and costs of a vocational advice service to improve work outcomes in patients with musculoskeletal pain in primary care: A cluster randomised trial. Pain 2018, 159, 128–138. [Google Scholar] [CrossRef] [PubMed]
- Hutting, N.; Johnston, V.; Staal, J.B.; Heerkens, Y.F. Promoting the Use of Self-management Strategies for People With Persistent Musculoskeletal Disorders: The Role of Physical Therapists. J. Orthop. Sport. Phys. Ther. 2019, 49, 212–215. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.; O’Sullivan, P. Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? Br. J. Sports Med. 2018, 52, 1543–1544. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.O.; Berkovic, D.; Erwin, J.; Copsey, S.M.; Davis, A.; Giagloglou, E.; Yazdani, A.; Hartvigsen, J.; Graveling, R.; Woolf, A. Musculoskeletal health in the workplace. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101558. [Google Scholar] [CrossRef]
- Johnston, V.; Shaw, W.S. Helping workers help themselves: Empowering physiotherapy clients to manage musculoskeletal problems at work. Phys. Ther. Rev. 2013, 18, 373–378. [Google Scholar] [CrossRef]
- Summers, K.; Bajorek, Z.; Bevan, S. Self-Management of Chronic Musculoskeletal Disorders and Employment. 2014. Available online: https://www.collegeofmedicine.org.uk/wp-content/uploads/2014/09/REPORT-Self-management-of-chronic-musculoskeletal-disorders-and-employment.-September-2014.pdf (accessed on 3 May 2020).
- Foster, N.; Anema, J.; Cherkin, D.; Chou, R.; Cohen, S.; Gross, D.; Ferreira, P.; Fritz, J.; Koes, B.; Peul, W.; et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef]
- O’Cathain, A.; Murphy, E.; Nicholl, J. Three techniques for integrating data in mixed methods studies. BMJ 2010, 341, 1147–1150. [Google Scholar] [CrossRef] [PubMed]
- Heyvaert, M.; Hannes, K.; Maes, B.; Onghena, P. Critical Appraisal of Mixed Methods Studies. J. Mix. Methods Res. 2013, 7, 302–327. [Google Scholar] [CrossRef]
- Halcomb, E.J. Appraising Mixed Methods Research. In Handbook of Research Methods in Health Social Sciences; Liamputtong, P., Ed.; Springer: Singapore, 2019; pp. 1051–1067. [Google Scholar]

| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Working-age adults (>50 years) | Specific pathological conditions (e.g., tumours, infections, fractures). Hypertension or cardiovascular diseases, symptomatic disc prolapses or severe cervical spine disorders, postoperative conditions in the neck and shoulder region, history of severe physical trauma and pregnancy. |
| All types of jobs | Applied for an early retirement |
| Reported chronic conditions (12 weeks or more) involving any area of the body | Acute musculoskeletal conditions |
| Public or private sector | Self-employed or part-time |
| Ability to understand and speak English | Not able to understand and speak English |
| Section 1: Demographics |
| Section 2: Employment status |
| Section 3: Impact of the chronic musculoskeletal condition |
| Section 4: Management pathways |
| Section 5: Barriers towards the management of your condition |
| Section 6: Future plans and retirement |
| Overarching Themes | Categories | Quantitative Findings | Qualitative Findings | Meta-Inferences and Interpretation | |
|---|---|---|---|---|---|
| Impact on wellness | Work performance | A total of 53% (N = 57/107) declared poor work ability, and 60% (N = 64/107) reported that the CMSD had interfered “quite a lot/extremely” with their ability to work effectively during the past six months. | I mean I ruined my hands working with no support for about 20 years. That is why I am worse now (Josh) I don’t know how much it really affects me now. I guess it affected me when I was having to go and have some physio a few times (before Christmas around 6 months ago). (Kathryn) | Convergence Expansion | Participants identified that work ability was affected at diverse levels. This was also confirmed by the quantitative responses. Both sets of findings demonstrated that work was affected in the past 6 months. Work ability was affected differently for the employees in the study. The condition fluctuates through the year due to the type of the CMSD, the use of medication, the job role they have and other factors affecting the intensity, e.g., stress, depression, comorbidities, flare-ups. |
| Participant Pseudonyms | Age | Employment | Interview Duration | Current CMSD |
|---|---|---|---|---|
| Claire | 58 | Academia | 70 min | Chronic pain |
| Debra | 54 | Mental health nurse practitioner | 45 min | Scoliosis and chronic back pain |
| Sarah | 52 | City council (administrator) | 58 min | Chronic hip pain |
| Nicky | 55 | Nurse practitioner | 50 min | Chronic back pain |
| Teresa | 57 | Academia | 45 min | Scoliosis and ankle pain |
| Anne | 63 | Customer service | 75 min | Rheumatoid arthritis |
| Andrew | 51 | Mechanical engineer | 52 min | Ankylosing spondylitis |
| Jessica | 52 | Human resources | 50 min | Psoriatic arthritis |
| Kathryn | 50 | Accountant | 40 min | Low back pain |
| John | 62 | Mechanical engineer | 40 min | Arthritis |
| Laura | 52 | Travel agent | 45 min | Chronic neck and shoulder pain |
| Maria | 60 | History teacher | 42 min | Chronic back pain |
| Sally | 51 | Prevent education officer | 79 min | Psoriatic arthritis |
| Annette | 51 | Laboratory technician | 40 min | Arthritis |
| Jack | 64 | Design engineer | 62 min | Ankylosing spondylitis |
| Josh | 55 | IT engineer | 55 min | Arthritis |
| Gender | Count (N) | Percentage (%) |
|---|---|---|
| Male | 44 | 41 |
| Female | 63 | 59 |
| Age group | ||
| 50–55 | 52 | 49 |
| 56–60 | 36 | 33 |
| 60–65 | 17 | 16 |
| >66 | 2 | 2 |
| Ethnicity | ||
| British | 97 | 90 |
| Other | 10 | 10 |
| Work Location | ||
| West Midlands | 81 | 76 |
| Other | 26 | 24 |
| Main Themes | Final Contributing Categories |
|---|---|
| Impact on wellness | Work performance |
| Physical issues | |
| Mental stressors | |
| Personal life | |
| Strategies and facilitators that support managing a CSMD | Taking a healthy approach |
| Strategies offered at work | |
| Supportive environment | |
| Managing the condition outside the workplace | |
| Perceived barriers related to management of a CMSD | Workstation design and environment |
| Bureaucracy and procedures | |
| Unsupportive colleagues | |
| Barriers with the management team | |
| Healthcare system | |
| Employees’ approach to living with a CMSD | Work ethic |
| Attitudes to management strategies | |
| Taking responsibility for self-management | |
| Disclosing the condition | |
| Emotions and beliefs about future employment and retirement | Fear of employment |
| Motivation to work longer | |
| Government changes and healthy retirement |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skamagki, G.; Carpenter, C.; King, A.; Wåhlin, C. Management of Chronic Musculoskeletal Disorders in the Workplace from the Perspective of Older Employees: A Mixed Methods Research Study. Int. J. Environ. Res. Public Health 2022, 19, 9348. https://doi.org/10.3390/ijerph19159348
Skamagki G, Carpenter C, King A, Wåhlin C. Management of Chronic Musculoskeletal Disorders in the Workplace from the Perspective of Older Employees: A Mixed Methods Research Study. International Journal of Environmental Research and Public Health. 2022; 19(15):9348. https://doi.org/10.3390/ijerph19159348
Chicago/Turabian StyleSkamagki, Glykeria, Christine Carpenter, Andrew King, and Charlotte Wåhlin. 2022. "Management of Chronic Musculoskeletal Disorders in the Workplace from the Perspective of Older Employees: A Mixed Methods Research Study" International Journal of Environmental Research and Public Health 19, no. 15: 9348. https://doi.org/10.3390/ijerph19159348
APA StyleSkamagki, G., Carpenter, C., King, A., & Wåhlin, C. (2022). Management of Chronic Musculoskeletal Disorders in the Workplace from the Perspective of Older Employees: A Mixed Methods Research Study. International Journal of Environmental Research and Public Health, 19(15), 9348. https://doi.org/10.3390/ijerph19159348







