Does the Contractile Capability of Pelvic Floor Muscles Improve with Knowledge Acquisition and Verbal Instructions in Healthy Women? A Systematic Review
Abstract
:1. Introduction
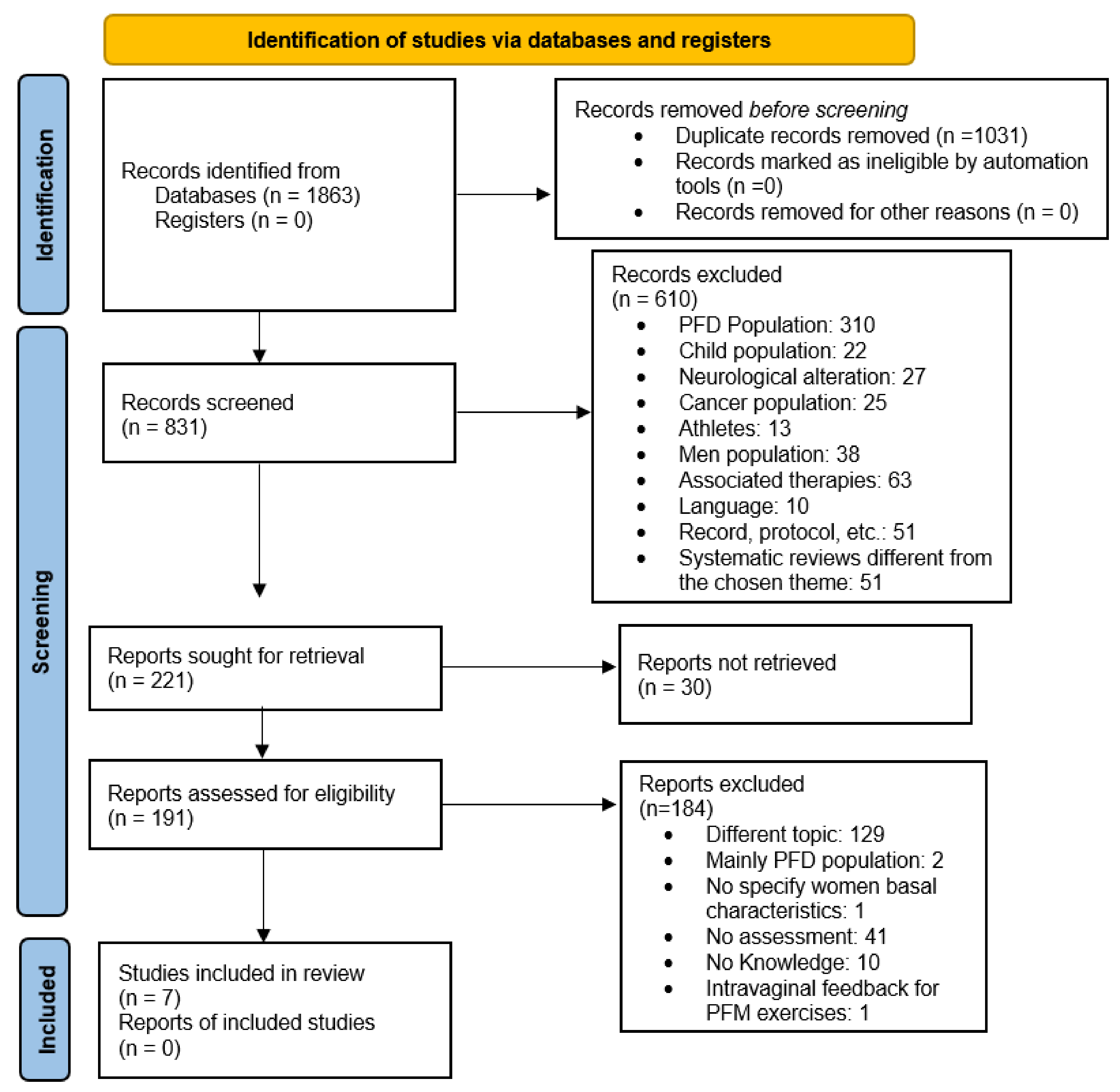
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Selection Criteria
2.4. Selection and Data Collection Processes
2.5. Quality and Risk of Bias Assessments
3. Results
3.1. Methodological and Scientific Quality and Risk of Bias
3.2. Participants
3.3. Physiotherapy Intervention
3.3.1. Health Education Programmes
3.3.2. PFM Strengthening Programme
3.3.3. Verbal Instructions to Achieve PFM Contraction
3.3.4. Intervention in the Control Group
3.4. Outcomes
3.4.1. Contraction Ability and Strength of the PFM
3.4.2. Urinary Incontinence
3.4.3. Knowledge about the Pelvic Floor
3.4.4. Other Outcomes
3.5. Effectiveness of Interventions and Adverse Effects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rocca Rossetti, S. Functional anatomy of pelvic floor. Arch. Ital. Urol. Androl. Organo Uff. Soc. Ital. Ecogr. Urol. Nefrol. 2016, 88, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Castro-Pardiñas, M.A.; Torres-Lacomba, M.; Navarro-Brazález, B. Muscle function of the pelvic floor in healthy, puerperal women with pelvic floor dysfunction. Actas Urol. Esp. 2017, 41, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Calleja-Agius, J.; Brincat, M.P. The urogenital system and the menopause. Climacteric: J. Int. Menopause Soc. 2015, 18 (Suppl. 1), 18–22. [Google Scholar] [CrossRef]
- Milsom, I.; Gyhagen, M. The prevalence of urinary incontinence. Climacteric: J. Int. Menopause Soc. 2019, 22, 217–222. [Google Scholar] [CrossRef] [Green Version]
- Sideris, M.; McCaughey, T.; Hanrahan, J.G.; Arroyo-Manzano, D.; Zamora, J.; Jha, S.; Knowles, C.H.; Thakar, R.; Chaliha, C.; Thangaratinam, S. Risk of obstetric anal sphincter injuries (OASIS) and anal incontinence: A meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 303–312. [Google Scholar] [CrossRef]
- Mou, T.; Warner, K.; Brown, O.; Yeh, C.; Beestrum, M.; Kenton, K.; Emi Bretschneider, C. Prevalence of pelvic organ prolapse among US racial populations: A systematic review and meta-analysis of population-based screening studies. Neurourol. Urodyn. 2021, 40, 1098–1106. [Google Scholar] [CrossRef]
- Fante, J.F.; Silva, T.D.; Mateus-Vasconcelos, E.C.L.; Ferreira, C.H.J.; Brito, L.G.O. Do Women have Adequate Knowledge about Pelvic Floor Dysfunctions? A Systematic Review. Rev. Bras. Ginecol. Obstet. 2019, 41, 508–519. [Google Scholar] [PubMed]
- Karaaslan, Y.; Karadag, M.; Toprak Celenay, S. Pelvic floor dysfunction symptoms and knowledge level in obese women. Women Health 2022, 62, 293–301. [Google Scholar] [CrossRef]
- McKay, E.R.; Lundsberg, L.S.; Miller, D.T.; Draper, A.; Chao, J.; Yeh, J.; Rangi, S.; Torres, P.; Stoltzman, M.; Guess, M.K. Knowledge of Pelvic Floor Disorders in Obstetrics. Female Pelvic Med. Reconstr. Surg. 2019, 25, 419–425. [Google Scholar] [CrossRef]
- Fitz, F.F.; Paladini, L.M.; Ferreira, L.A.; Gimenez, M.M.; Bortolini, M.A.T.; Castro, R.A. Ability to contract the pelvic floor muscles and association with muscle function in incontinent women. Int. Urogynecology J. 2020, 31, 2337–2344. [Google Scholar] [CrossRef]
- Bø, K.; Mørkved, S.; Aschehoug, A. Pelvic floor and exercise science. In Evidence-Based Physical Therapy for the Pelvic Floor; Bø, K., Berghmans, B., Mørkved, S., Van Kampen, M., Eds.; Churchill Livingstone: London, UK, 2015; pp. 111–130. [Google Scholar]
- Li, C.; Gong, Y.; Wang, B. The efficacy of pelvic floor muscle training for pelvic organ prolapse: A systematic review and meta-analysis. Int. Urogynecology J. 2016, 27, 981–992. [Google Scholar] [CrossRef] [PubMed]
- Wiegersma, M.; Panman, C.M.; Kollen, B.J.; Berger, M.Y.; Lisman-Van Leeuwen, Y.; Dekker, J.H. Effect of pelvic floor muscle training compared with watchful waiting in older women with symptomatic mild pelvic organ prolapse: Randomised controlled trial in primary care. BMJ 2014, 349, g7378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Mørkved, S.; Bø, K.; Schei, B.; Salvesen, K.A. Pelvic floor muscle training during pregnancy to prevent urinary incontinence: A single-blind randomized controlled trial. Obstet. Gynecol. 2003, 101, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Sampselle, C.M.; Messer, K.L.; Seng, J.S.; Raghunathan, T.E.; Hines, S.H.; Diokno, A.C. Learning outcomes of a group behavioral modification program to prevent urinary incontinence. Int. Urogynecology J. Pelvic Floor Dysfunct. 2005, 16, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Talasz, H.; Kalchschmid, E.; Kofler, M.; Lechleitner, M. Effects of multidimensional pelvic floor muscle training in healthy young women. Arch. Gynecol. Obstet. 2012, 285, 709–715. [Google Scholar] [CrossRef]
- Aliaga-Martínez, F.; Prats-Ribera, E.; Alsina-Hipólito, M.; Allepuz-Palau, A. Impacto en la función de los músculos del suelo pélvico de un programa de entrenamiento específico incluido en el control habitual del embarazo y el posparto: Ensayo clínico controlado no aleatorizado. Matronas Profesión 2013, 14, 36–44. [Google Scholar]
- Henderson, J.W.; Wang, S.; Egger, M.J.; Masters, M.; Nygaard, I. Can women correctly contract their pelvic floor muscles without formal instruction? Female Pelvic Med. Reconstr. Surg. 2013, 19, 8–12. [Google Scholar] [CrossRef] [Green Version]
- Vermandel, A.; De Wachter, S.; Beyltjens, T.; D’Hondt, D.; Jacquemyn, Y.; Wyndaele, J.J. Pelvic floor awareness and the positive effect of verbal instructions in 958 women early postdelivery. Int. Urogynecology J. 2015, 26, 223–228. [Google Scholar] [CrossRef]
- Uechi, N.; Fernandes, A.; Bø, K.; de Freitas, L.M.; de la Ossa, A.M.P.; Bueno, S.M.; Ferreira, C.H.J. Do women have an accurate perception of their pelvic floor muscle contraction? A cross-sectional study. Neurourol. Urodyn. 2020, 39, 361–366. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manterola, C.; Asenjo-Lobos, C.; Otzen, T. Jerarquización de la evidencia: Niveles de evidencia y grados de recomendación de uso actual. Rev. Chil. De Infectología 2014, 31, 705–718. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Berujon, E.; Blanchard, V.; Fauvet, R.; Nyangoh-Timoh, K.; Pizzoferrato, A.C. Benefits of group pelvic floor education sessions: Satisfaction and improvement of women’s knowledge. Prog. Urol. J. L’association Fr. D’urologie La Soc. Fr. D’urologie 2021, 31, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- Charrié, M.; Billecocq, S. Knowledge of pelvic floor disorders in peripartum women: A systematic review. Prog. Urol. J. L’association Fr. D’urologie La Soc. Fr. D’urologie 2021, 31, 204–214. [Google Scholar] [CrossRef] [PubMed]
- Goodridge, S.D.; Chisholm, L.P.; Heft, J.; Hartigan, S.; Kaufman, M.; Dmochowski, R.R.; Stewart, T.; Reynolds, W.S. Association of Knowledge and Presence of Pelvic Floor Disorders and Participation in Pelvic Floor Exercises: A Cross-sectional Study. Female Pelvic Med. Reconstr. Surg. 2021, 27, 310–314. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, B.; Arranz-Martín, B.; Navarro-Brazález, B.; Vergara-Pérez, F.; Bailón-Cerezo, J.; Torres-Lacomba, M. How Do We Assess Patient Skills in a Competence-Based Program? Assessment of Patient Competences Using the Spanish Version of the Prolapse and Incontinence Knowledge Questionnaire and Real Practical Cases in Women with Pelvic Floor Disorders. Int. J. Environ. Res. Public Health 2021, 18, 2377. [Google Scholar] [PubMed]
- Kandadai, P.; O’Dell, K.; Saini, J. Correct performance of pelvic muscle exercises in women reporting prior knowledge. Female Pelvic Med. Reconstr. Surg. 2015, 21, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Ben Ami, N.; Dar, G. What is the most effective verbal instruction for correctly contracting the pelvic floor muscles? Neurourol. Urodyn. 2018, 37, 2904–2910. [Google Scholar] [CrossRef] [PubMed]
- Crotty, K.; Bartram, C.I.; Pitkin, J.; Cairns, M.C.; Taylor, P.C.; Dorey, G.; Chatoor, D. Investigation of optimal cues to instruction for pelvic floor muscle contraction: A pilot study using 2D ultrasound imaging in pre-menopausal, nulliparous, continent women. Neurourol. Urodyn. 2011, 30, 1620–1626. [Google Scholar] [CrossRef]
- Navarro-Brazález, B.; Vergara-Pérez, F.; Prieto-Gómez, V.; Sánchez-Sánchez, B.; Yuste-Sánchez, M.J.; Torres-Lacomba, M. What Influences Women to Adhere to Pelvic Floor Exercises after Physiotherapy Treatment? A Qualitative Study for Individualized Pelvic Health Care. J. Pers. Med. 2021, 11, 1368. [Google Scholar] [PubMed]
- Torres-Lacomba, M.; Navarro-Brazález, B.; Yuste-Sánchez, M.J.; Sánchez-Sánchez, B.; Prieto-Gómez, V.; Vergara-Pérez, F. Women’s Experiences with Compliance with Pelvic Floor Home Exercise Therapy and Lifestyle Changes for Pelvic Organ Prolapse Symptoms: A Qualitative Study. J. Pers. Med. 2022, 12, 498. [Google Scholar]
- De Andrade, R.L.; Bø, K.; Antonio, F.I.; Driusso, P.; Mateus-Vasconcelos, E.C.L.; Ramos, S.; Julio, M.P.; Ferreira, C.H.J. An education program about pelvic floor muscles improved women’s knowledge but not pelvic floor muscle function, urinary incontinence or sexual function: A randomised trial. J. Physiother. 2018, 64, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Neels, H.; Tjalma, W.A.A.; Wyndaele, J.-J.; De Wachter, S.; Wyndaele, M.; Vermandel, A. Knowledge of the pelvic floor in menopausal women and in peripartum women. J. Phys. Ther. Sci. 2016, 28, 3020–3029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neels, H.; Wyndaele, J.J.; Tjalma, W.A.; De Wachter, S.; Wyndaele, M.; Vermandel, A. Knowledge of the pelvic floor in nulliparous women. J. Phys. Ther. Sci. 2016, 28, 1524–1533. [Google Scholar] [CrossRef] [Green Version]
- Roa, L.; Kent, S.; Yaskina, M.; Schulz, J.; Poirier, A. Knowledge of pelvic floor disorders amongst immigrant women in Canada. Int. Urogynecology J. 2021, 32, 3077–3084. [Google Scholar] [CrossRef]
- Tennfjord, M.K.; Engh, M.E.; Bø, K. The Influence of Early Exercise Postpartum on Pelvic Floor Muscle Function and Prevalence of Pelvic Floor Dysfunction 12 Months Postpartum. Phys. Ther. 2020, 100, 1681–1689. [Google Scholar] [CrossRef]
- Dumoulin, C.; Pazzoto Cacciari, L.; Mercier, J. Keeping the pelvic floor healthy. Climacteric J. Int. Menopause Soc. 2019, 22, 257–262. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 2019, 366, 14898. [Google Scholar] [CrossRef] [Green Version]
- Brennen, R.; Frawley, H.C.; Martin, J.; Haines, T.P. Group-based pelvic floor muscle training for all women during pregnancy is more cost-effective than postnatal training for women with urinary incontinence: Cost-effectiveness analysis of a systematic review. J. Physiother. 2021, 67, 105–114. [Google Scholar] [CrossRef]
- Wang, X.; Xu, X.; Luo, J.; Chen, Z.; Feng, S. Effect of app-based audio guidance pelvic floor muscle training on treatment of stress urinary incontinence in primiparas: A randomized controlled trial. Int. J. Nurs. Stud. 2020, 104, 103527. [Google Scholar] [CrossRef] [PubMed]
- Bernard, S.; McLean, L.; Boucher, S.; Hébert, L.J.; Plante, M.; Grégoire, J.; Sebastianelli, A.; Renaud, M.C.; Froment, M.A.; Moffet, H. An in-home rehabilitation program for the treatment of urinary incontinence symptoms in endometrial cancer survivors: A single-case experimental design study. Int. Urogynecol. J. 2021, 32, 2947–2957. [Google Scholar] [CrossRef] [PubMed]
| Author/s | Year | Journal | Journal Impact Factor (JCR) | City, Country | Study Design | Methodological Quality PEDro/10 and NOS /10 | Evidence Grading (SIGN) |
|---|---|---|---|---|---|---|---|
| Mørkved, S. et al. [15] | 2003 | Obstetrics & Gynecology | 4.965 | Trondheim, Norway | Randomised clinical trial | 9/10 | 1+ |
| Sampselle, C.M. et al. [16] | 2005 | International Urogynecology Journal | 2.094 | Michigan, United States | Randomised clinical trial | 5/10 | 1− |
| Talasz, H. et al. [17] | 2012 | Archives of Gynecology and Obstetrics | 2.493 | Innsbruck, Austria | Interventional, non-randomised, cross-sectional study | 6/10 | 2+ |
| Aliaga-Martínez, F. et al. [18] | 2013 | Matronas Profesión | 0.123 (SJR) | Catalonia, Spain | Controlled non- randomised clinical trial | 5/10 | 1− |
| Henderson, J.W. et al. [19] | 2013 | Female Pelvic Medicine and Reconstructive Surgery | 1.237 | Salt Lake City, Utah, United States | Observational cross-sectional study | 8/10 | 2+ |
| Vermandel, A. et al. [20] | 2015 | International Urogynecology Journal | 2.094 | Antwerp, Belgium | Observational cross-sectional study | 7/10 | 2+ |
| Uechi, N. et al. [21] | 2019 | Neurourology and Urodynamics | 2.354 | Brazil | Observational cross-sectional study | 8/10 | 2+ |
| Author/s | Participants | Intervention | Variables | Results |
|---|---|---|---|---|
| Mørkved, S. et al. [15] | N = 289 IG = 143 CG = 146 Reported incontinence during baseline examination: IG= 47 (32%) CG= 47 (31%) | Both groups were taught about PF anatomy and how to contract the PF with intra-vaginal guide. IG: Face-to-face treatment with a physiotherapist in groups of 10–15 women, one weekly session, 60 min, 12 weeks. MVCs of 6–8 min were requested, followed by 3–4 fast MVC. They were performed in lying, sitting, kneeling, and standing positions. At home, they must perform 8–12 MVC twice a day in the position of their choice. CG: customary information. | Main variable: Onset of UI (self-reported) Secondary variables: UI episodes (voiding diary), PFM contraction ability (digital palpation and observation), PFM strength (manometer). | UI: lower prevalence of UI in the IG that reached statistical significance at 36 weeks (32% versus 48%) and 3 months (20% versus 32%) postpartum. Incontinence episodes: fewer UI episodes in the IG that reached statistical significance at 36 weeks and 3 months. PFM strength: statistically significant difference in the IG at 36 weeks (39.9 cmH2O versus 34.4 cmH2O) and 3 months (29.5 cmH2O versus 25.6 cmH2O) postpartum. Adverse effects were not reported in the IG. |
| Sampselle, C.M. et al. [16] | N = 318 IG = 141 CG = 177 Reported 0–5 leak episodes during the last year: 318 (100%) | IG: 2 h educational group session (5–25 women) using slides and flyers about PF anatomy and physiology, UI types, and their impacts on quality of life, daily fluid intake requirement and voiding habits, how to locate and strengthen PFMs, and strategies for the incorporation of habits and exercises during DLA. Practise session of PFMT using an audio tape (3 weeks, 50 exercises each day). 10 min individual explanation to women who were not able to correctly contract PFM. CG: No intervention. | Main variable: UI (MESA questionnaire); PFM contraction ability (vaginal exam). Secondary variables: Knowledge (multiple-choice exam, self-produced); Voiding frequency (3-day voiding diary). Questionnaires for PFMT adherence and voiding habits at 3, 6, 9, and 12 months (self-reported). | UI: statistically significant difference in the IG, where 37% of women presented UI episodes versus 28% in the CG. PFM contraction ability: statistically significant differences in the pressure and displacement variables in the IG (68% correct contraction, 29% after instruction, and 3% failed). Knowledge: 90% of correct hits about voiding habits and 86% about PFMT in the IG. Voiding frequency: lower voiding frequency in the IG that reached statistical significance. Adherence: statistically significant difference in PFMT in the IG (82%, 2–3 times per week at 3 months; 68% at 12 months) and voiding habits (66% performed the recommended interval at 3 months). |
| Aliaga-Martínez, F. et al. [18] | N = 110 IG = 55 CG = 55 UI perception at baseline examination (ICIQ-SF = 0): IG = 42 (76.4%) CG = 39 (70.9%) | IG: One individual session and group sessions about anatomy, PFM function, and healthy habits at 28 and 30 weeks during pregnancy, 2 h, once a week. PFM exercises, two series per day, 8–12 contractions of 6–8 min and 3–4 fast contractions in different positions. Integration of knack manoeuvre. Eight group sessions during postpartum about protection, nursing, and PFM exercises. CG: customary information. | Main variables: PFM MVC (MOS); PFM strength and endurance (manometry); UI perception (ICIQ-SF). | PFM MVC: statistically significant difference in MOS. A higher percentage of women in the IG obtained a score ≥ 3 (58.2% versus 36.4%). PFM strength and endurance: statistically significant differences in manometry in the IG in maximum values (41.3 cmH2O versus 31.6 cmH2O), on average (28.4 cmH2O versus 21.5 cmH2O), and in contraction duration (11.6 s versus 9.4 s). UI perception: no statistically significant inter-group differences (92.7% without UI perception in the IG versus 81.8% in the CG). |
| Author/s | Participants | Intervention | Variables | Results |
|---|---|---|---|---|
| Talasz, H. et al. [17] | N = 40 Healthy young nulliparous women = 40 (100%) FPFQ dysfunction score (maximum 40): Mean = 10 (SD 7) | Single group: One group session lasting 60 min: theoretical instruction about PF anatomy and PFM function, verbal feedback with hands-on instruction about PFM exercises with co-contraction of anterolateral abdominal muscles during forced expiration and coughing. PFM exercises consisted of ten sub-maximal contractions for 10s followed by 10 fast contractions, at least 10 times per week, 3 days/week. | Main variable: PFM contraction ability (MOS); ability to contract PFM during coughing. Secondary variables: FPFQ | MOS increased post-intervention from 3.3 ± 1.7 to 4.2 ± 1.0; 72.5% performed cough-related PFM contractions; 100% reported that the acquired knowledge was helpful, and 94.6% referred the gained information to their acquaintances. |
| Henderson, J.W. et al. [19] | N = 779 Baseline characteristics: POP = 166 (21.3%) SUI = 133 (17.1%) POP and SUI = 35 (4.5%) No POP/SUI = 445 (57.1%) | Only group: Assessment of POP presence using POP-Q and PFM contraction capacity by intravaginal exam. In women performing incorrect PFM contraction, researchers repeated the assessment of the PFM contraction after additional verbal instruction. | Main variable: PFM contraction capacity (Brink scale) Secondary variables: SUI presence (Incontinence Severity Index); POP presence (POP-Q) | PFM contraction capacity: statistically significant difference in the group of women who presented POP and SUI, with higher proportion of women capable of contracting PFM (68.6% versus 31.4%). No statistically significant difference in groups of women with POP (86.6% versus 14.6%), with SUI (83.5% versus 16.5%), and without POP, SUI, or any of them (85.8% versus 14.2%). On a second attempt to contract PFM, 78% of 120 women who received information corrected their execution. Statistically significant difference in the group of women without POP or SUI compared to women with POP (85.7% versus 54.3%). |
| Vermandel, A. et al. [20] | N = 958; KEG = 500 NKEG = 458 Reported UI before pregnancy: KEG = 56 (11%) NKEG = 34 (7%) Reported UI during pregnancy: KEG = 222 (44%) NKEG = 161 (35%) | Information was collected about previous PF knowledge, its function, experience with PFM exercises, and if the participants were capable of performing a correct PFM contraction. Information was given to women that did not have former knowledge, who received personalised information and instructions on how to contract the PFMs using visual inspection. | Main variable: PFM contraction (visual observation) Secondary variables: PF knowledge (physiotherapist questions); PFM contraction awareness (physiotherapist questions) | Statistically significant difference in the performance of better PFM contraction in women with knowledge and previous experience. Comparison of women with former knowledge and experience versus others lacking knowledge or experience following physiotherapist instruction: 19.2% versus 24% improved from grade 0 to grade 1, 26.2% maintained the level versus 26.6%, and 54.6% versus 49.4% upgraded from grade 0 or 1 to grade 2, respectively. No woman worsened the performance after physiotherapist indications. |
| Uechi, N. et al. [21] | N = 82 Urinary incontinence self-report = 37 (45.1%) | Only group: First, verbal instructions about correct PFM contraction. Second, assessment of PFM contraction. Finally, analysis of women’s self-perceptions of their PFM contraction performances. | Main variable: PFM function (MOS) Secondary variables: Self-perception (correlation between participant and assessor physiotherapist MOS); UI symptoms and severity (ICIQ-UI-SF). | PFM function: 61% obtained a score ≥ 3 on the MOS. Self-perception: 33% reported correct self-perception of PFM contraction. The majority of women considered that they had a higher score compared to objective measurement. UI symptoms and severity: no relation was found with self-perception of PFM contraction. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Díaz-Álvarez, L.; Lorenzo-Gallego, L.; Romay-Barrero, H.; Prieto-Gómez, V.; Torres-Lacomba, M.; Navarro-Brazález, B. Does the Contractile Capability of Pelvic Floor Muscles Improve with Knowledge Acquisition and Verbal Instructions in Healthy Women? A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 9308. https://doi.org/10.3390/ijerph19159308
Díaz-Álvarez L, Lorenzo-Gallego L, Romay-Barrero H, Prieto-Gómez V, Torres-Lacomba M, Navarro-Brazález B. Does the Contractile Capability of Pelvic Floor Muscles Improve with Knowledge Acquisition and Verbal Instructions in Healthy Women? A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(15):9308. https://doi.org/10.3390/ijerph19159308
Chicago/Turabian StyleDíaz-Álvarez, Lara, Laura Lorenzo-Gallego, Helena Romay-Barrero, Virginia Prieto-Gómez, María Torres-Lacomba, and Beatriz Navarro-Brazález. 2022. "Does the Contractile Capability of Pelvic Floor Muscles Improve with Knowledge Acquisition and Verbal Instructions in Healthy Women? A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 15: 9308. https://doi.org/10.3390/ijerph19159308
APA StyleDíaz-Álvarez, L., Lorenzo-Gallego, L., Romay-Barrero, H., Prieto-Gómez, V., Torres-Lacomba, M., & Navarro-Brazález, B. (2022). Does the Contractile Capability of Pelvic Floor Muscles Improve with Knowledge Acquisition and Verbal Instructions in Healthy Women? A Systematic Review. International Journal of Environmental Research and Public Health, 19(15), 9308. https://doi.org/10.3390/ijerph19159308









