Psychometric Properties of the Hospital Anxiety and Depression Scale (HADS) in Previously Hospitalized COVID-19 Patients
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. COVID-19 and Post-COVID Data Collection
2.3. Hospital Anxiety and Depression Scale (HADS)
2.4. Statistical Analysis
3. Results
3.1. Participants
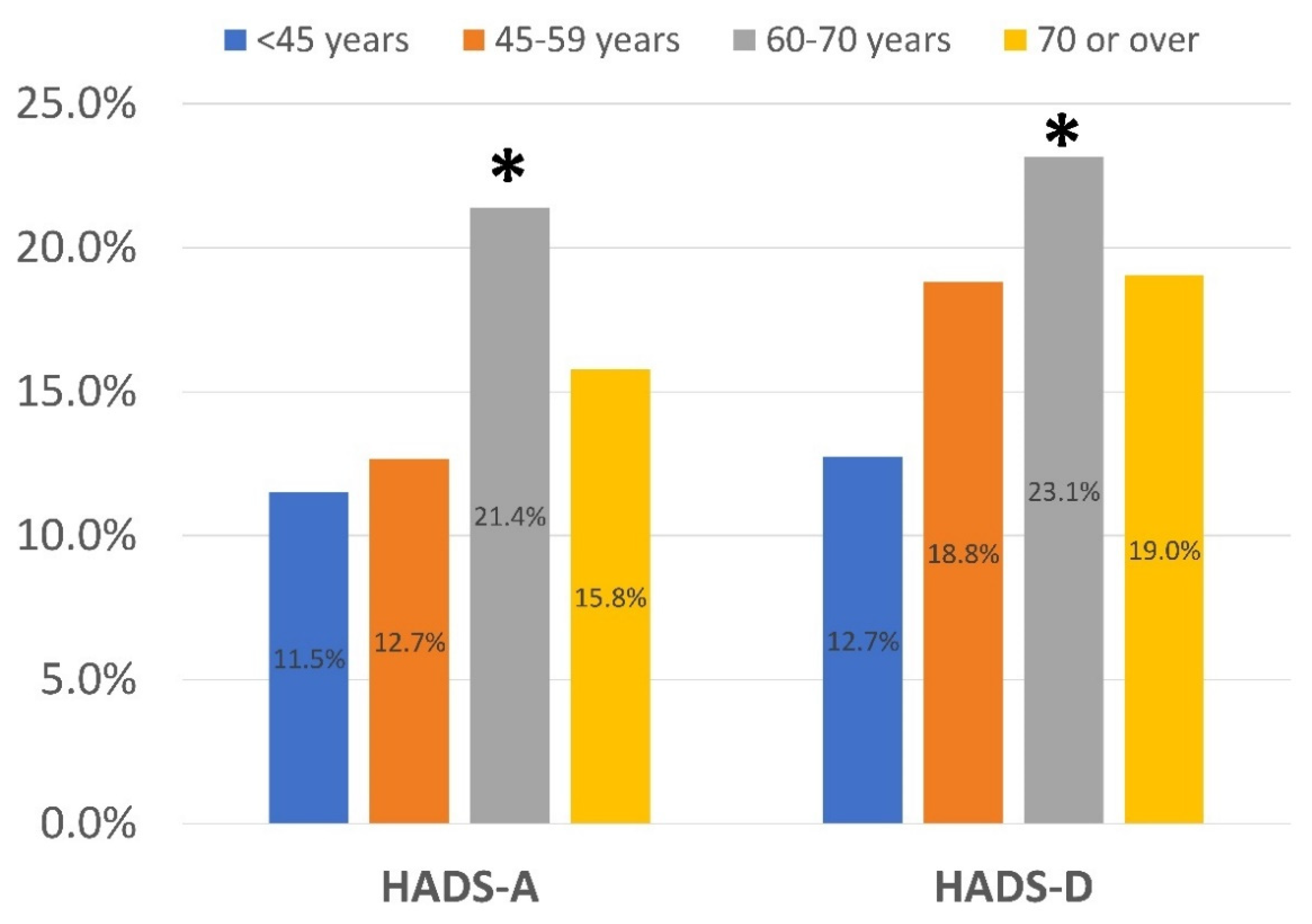
3.2. General Data
3.3. Reliability and Internal Consistency
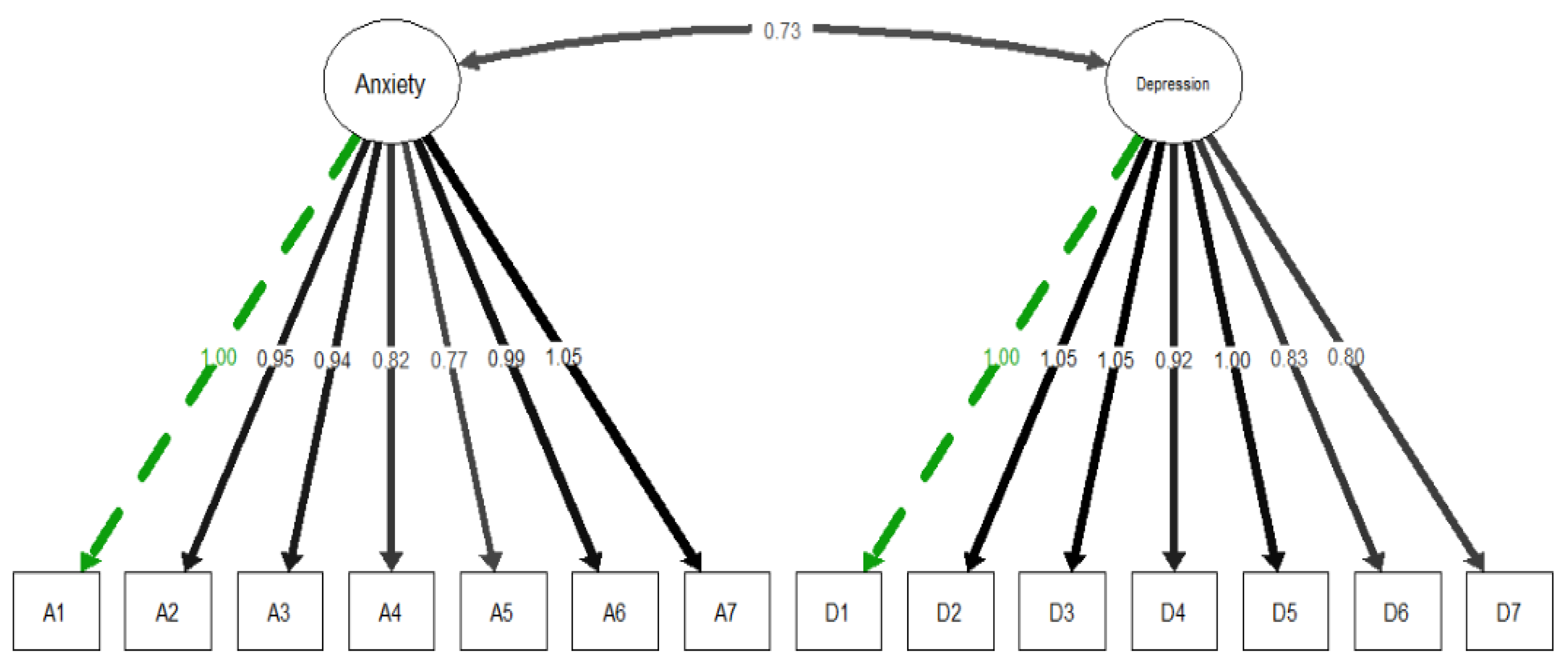
3.4. Construct Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zheng, K.I.; Feng, G.; Liu, W.Y.; Targher, G.; Byrne, C.D.; Zheng, M.H. Extrapulmonary complications of COVID-19: A multisystem disease? J. Med. Virol. 2021, 93, 323–335. [Google Scholar] [CrossRef] [PubMed]
- Hall, P.A.; Sheeran, P.; Fong, G.T.; Cheah, C.S.; Oremus, M.; Liu-Ambrose, T.; Sakib, M.N.; Butt, Z.A.; Ayaz, H.; Jandu, N.; et al. Biobehavioral Aspects of the COVID-19 Pandemic: A Review. Psychosom Med. 2021, 83, 309–321. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Pan, W.; Li, L.; Li, B.; Ren, Y.; Ma, X. Prevalence of depression, anxiety, and insomnia symptoms among patients with COVID-19: A meta-analysis of quality effects model. J. Psychosom. Res. 2021, 147, 110516. [Google Scholar] [CrossRef] [PubMed]
- Shanbehzadeh, S.; Tavahomi, M.; Zanjari, N.; Ebrahimi-Takamjani, I.; Amiri-Arimi, S. Physical and mental health complications post-COVID-19: Scoping review. Psychosomatics 2021, 147, 110525. [Google Scholar] [CrossRef]
- Bottemanne, H.; Gouraud, C.; Hulot, J.S.; Blanchard, A.; Ranque, B.; Lahlou-Laforêt, K.; Limosin, F.; Günther, S.; Lebeaux, D.; Lemogne, C. Do anxiety and depression predict persistent physical symptoms after a severe COVID-19 episode? A prospective study. Front. Psychiatry 2021, 12, 757685. [Google Scholar] [CrossRef]
- van den Besselaar, J.H.; Vroomen, J.L.M.; Buurman, B.M.; Hertogh, C.M.; Huisman, M.; Kok, A.A.; Hoogendijk, E.O. Symptoms of depression, anxiety, and perceived mastery in older adults before and during the COVID-19 pandemic: Results from the Longitudinal Aging Study Amsterdam. J. Psychosom. Res. 2021, 151, 110656. [Google Scholar] [CrossRef]
- Vincent, A.; Beck, K.; Becker, C.; Zumbrunn, S.; Ramin-Wright, M.; Urben, T.; Quinto, A.; Schaefert, R.; Meinlschmidt, G.; Gaab, J.; et al. Psychological burden in patients with COVID-19 and their relatives 90 days after hospitalization: A prospective observational cohort study. J. Psychosom. Res. 2021, 147, 110526. [Google Scholar] [CrossRef]
- Al Maqbali, M.; Al Sinani, M.; Al-Lenjawi, B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. J. Psychosom. Res. 2021, 141, 110343. [Google Scholar] [CrossRef]
- Klok, F.A.; Boon, G.J.; Barco, S.; Endres, M.; Geelhoed, J.M.; Knauss, S.; Rezek, S.A.; Spruit, M.A.; Vehreschild, J.; Siegerink, B. The Post-COVID-19 Functional Status (PCFS) scale: A tool to measure functional status over time after COVID-19. Eur. Respir. J. 2020, 56, 2001494. [Google Scholar] [CrossRef]
- Machado, F.V.C.; Meys, R.; Delbressine, J.M.; Vaes, A.W.; Goërtz, Y.M.J.; van Herck, M.; Houben-Wilke, S.; Boon, G.J.A.M.; Barco, S.; Burtin, C.; et al. Construct validity of the Post-COVID-19 Functional Status Scale in adult subjects with COVID-19. Health Qual. Life Outcomes 2021, 19, 40. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Djukanovic, I.; Carlsson, J.; Årestedt, K. Is the Hospital Anxiety and Depression Scale (HADS) a valid measure in a general population 65-80 years old? A psychometric evaluation study. Health Qual. Life Outcomes 2017, 15, 193. [Google Scholar] [CrossRef] [Green Version]
- Tasnim, R.; Sujan, S.H.; Islam, S.; Ritu, A.H.; Bin Siddique, A.; Toma, T.Y.; Nowshin, R.; Hasan, A.; Hossain, S.; Nahar, S.; et al. Prevalence and correlates of anxiety and depression in frontline healthcare workers treating people with COVID-19 in Bangladesh. BMC Psychiatry 2021, 21, 271. [Google Scholar] [CrossRef]
- Ato, M.; López, J.J.; Benavente, A. A classification system for research designs in psychology. Anal. Psicol. 2013, 29, 1038–1059. [Google Scholar]
- Fernández-de-las-Peñas, C.; Martín-Guerrero, J.; Navarro-Pardo, E.; Torres-Macho, J.; Canto-Diez, M.G.; Pellicer-Valero, O. Gastrointestinal symptoms at the acute COVID-19 phase are risk factors for developing gastrointestinal post-COVID symptoms: A multicenter study. Intern. Emerg. Med. 2022, 17, 583–586. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Pellicer-Valero, O.J.; Navarro-Pardo, E.; Rodríguez-Jiménez, J.; Martín-Guerrero, J.D.; Cigarán-Méndez, M. The number of symptoms at the acute COVID-19 phase is associated with anxiety and depressive long-term post-COVID symptoms: A multicenter study. J. Psychosom. Res. 2021, 150, 110625. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Martín-Guerrero, J.D.; Navarro-Pardo, E.; Fuensalida-Novo, S.; Palacios-Ceña, M.; Velasco-Arribas, M.; Pellicer-Valero, O.J. The presence of rheumatological conditions is not a risk factor of long-term post-COVID symptoms after SARS-CoV-2 infection: A multicenter study. Clin. Rheumatol. 2022, 41, 585–586. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Martín-Guerrero, J.D.; Pellicer-Valero, Ó.J.; Navarro-Pardo, E.; Gómez-Mayordomo, V.; Cuadrado, M.L.; Arias-Navalón, J.A.; Cigarán-Méndez, M.; Hernández-Barrera, V.; Arendt-Nielsen, L. Female sex is a risk factor associated with long-term post-COVID related-symptoms but not with COVID-19 symptoms: The LONG-COVID-EXP-CM Multicenter Study. J. Clin. Med. 2022, 11, 413. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Martín-Guerrero, J.D.; Cancela-Cilleruelo, I.; Moro-López-Menchero, P.; Rodríguez-Jiménez, J.; Pellicer-Valero, O.J. Post-COVID functional limitations on daily living activities are associated with symptoms experienced at the acute phase of SARS-CoV-2 infection and internal care unit admission: A multicenter study. Int. J. Infect. Dis. 2022, 117, 201–203. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Pellicer-Valero, O.J.; Navarro-Pardo, E.; Palacios-Ceña, D.; Florencio, L.L.; Guijarro, C.; Martín-Guerrero, J.D. Symptoms experienced at the acute phase of SARS-CoV-2 infection as risk factor of long-term post-COVID symptoms: The LONG-COVID-EXP-CM Multicenter Study. Int. J. Infect. Dis. 2022, 116, 241–244. [Google Scholar] [CrossRef]
- Hedman, E.; Ljótsson, B.; Blom, K.; El Alaoui, S.; Kraepelien, M.; Rück, C.; Andersson, G.; Svanborg, C.; Lindefors, N.; Kaldo, V. Telephone Versus Internet Administration of Self-Report Measures of Social Anxiety, Depressive Symptoms, and Insomnia: Psychometric Evaluation of a Method to Reduce the Impact of Missing Data. J. Med Internet Res. 2013, 15, e229. [Google Scholar] [CrossRef]
- Herrmann-Lingen, C.; Buss, U.; Snaith, R.P. Hospital Anxiety and Depression Scale–Deutsche Version (HADS-D); Verlag Hans Huber: Bern, Switzerland, 2011. [Google Scholar]
- Olssøn, I.; Mykletun, A.; Dahl, A.A. The Hospital Anxiety and Depression Rating Scale: A cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry 2005, 5, 46. [Google Scholar] [CrossRef] [Green Version]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J. Clin. Epidemiology 2010, 63, 737–745. [Google Scholar] [CrossRef] [Green Version]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Dunn, T.J.; Baguley, T.; Brunsden, V. From alpha to omega: A practical solution to the pervasive problem of internal consistency estimation. Br. J. Psychol. 2014, 105, 399–412. [Google Scholar] [CrossRef] [Green Version]
- Rosseel, Y. lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef] [Green Version]
- Epskamp, S. semPlot: Path Diagrams and Visual Analysis of Various SEM Packages; ver. 1.1.2; R Foundation: Vienna, Austria, 2019. [Google Scholar]
- Gates, K.M.; Molenaar, P.C. Group search algorithm recovers effective connectivity maps for individuals in homogeneous and heterogeneous samples. Neuroimage 2012, 63, 310–319. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Wu, Y.; Levis, B.; Sun, Y.; He, C.; Krishnan, A.; Neupane, D.; Bhandari, P.M.; Negeri, Z.; Benedetti, A.; Thombs, B.D. Accuracy of the Hospital Anxiety and Depression Scale Depression subscale (HADS-D) to screen for major depression: Systematic review and individual participant data meta-analysis. BMJ 2021, 373, n972. [Google Scholar] [CrossRef]
- Norton, S.; Cosco, T.; Doyle, F.; Done, J.; Sacker, A. The Hospital Anxiety and Depression Scale: A meta confirmatory factor analysis. J. Psychosom. Res. 2013, 74, 74–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LoMartire, R.; Äng, B.O.; Gerdle, B.; Vixner, L. Psychometric properties of Short Form-36 Health Survey, EuroQol 5-dimensions, and Hospital Anxiety and Depression Scale in patients with chronic pain. Pain. 2020, 161, 83–95. [Google Scholar] [CrossRef] [Green Version]
- Bai, F.; Tomasoni, D.; Falcinella, C.; Barbanotti, D.; Castoldi, R.; Mulè, G.; Augello, M.; Mondatore, D.; Allegrini, M.; Cona, A.; et al. Female gender is associated with long COVID syndrome: A prospective cohort study. Clin. Microbiol. Infect. 2021, 28, 611. [Google Scholar] [CrossRef] [PubMed]
- Zavlis, O.; Butter, S.; Bennett, K.; Hartman, T.K.; Hyland, P.; Mason, L.; McBride, O.; Murphy, J.; Gibson-Miller, J.; Levita, L.; et al. How does the COVID-19 pandemic impact on population mental health? A network analysis of COVID influences on depression, anxiety and traumatic stress in the UK population. Psychol. Med. 2021. [Google Scholar] [CrossRef]
- Chan, C.S.; Yang, C.T.; Xu, Y.; He, L.; Yip, P.S.F. Variability in the psychological impact of four waves of COVID-19: A time-series study of 60 000 text-based counseling sessions. Psychol. Med. 2022. [Google Scholar] [CrossRef]
- Gambin, M.; Oleksy, T.; Sękowski, M.; Wnuk, A.; Woźniak-Prus, M.; Kmita, G.; Holas, P.; Pisula, E.; Łojek, E.; Hansen, K.; et al. Pandemic trajectories of depressive and anxiety symptoms and their predictors: Five-wave study during the COVID-19 pandemic in Poland. Psychol. Med. 2021. [Google Scholar] [CrossRef]
- Saunders, R.; Buckman, J.E.J.; Fonagy, P.; Fancourt, D. Understanding different trajectories of mental health across the general population during the COVID-19 pandemic. Psychol. Med. 2021. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Martín-Guerrero, J.D.; Cancela-Cilleruelo, I.; Moro-López-Menchero, P.; Rodríguez-Jiménez, J.; Pellicer-Valero, O.J. Trajectory curves of post-COVID anxiety/depressive symptoms and sleep quality in previously hospitalized COVID-19 survivors: The LONG-COVID-EXP-CM multicenter study. Psychol. Med. 2022, 10, 1–2. [Google Scholar] [CrossRef]

| Age, mean (SD), years | 61 (16) |
| Gender, male/female (%) | 1054 (53.5%)/915 (46.5%) |
| Weight, mean (SD), kg. | 75 (15) |
| Height, mean (SD), cm. | 165 (16.5) |
| Medical co-morbidities | |
| Hypertension | 514 (26.1%) |
| Diabetes | 236 (12.0%) |
| Cardiovascular Disease | 234 (11.9%) |
| Asthma | 126 (6.4%) |
| Obesity | 88 (4.5%) |
| Chronic Obstructive Pulmonary Disease | 77 (3.9%) |
| Stroke | 38 (2.0%) |
| Rheumatological Disease | 31 (1.6%) |
| Other (Cancer, Kidney Disease) | 332 (16.9%) |
| Main Symptoms at hospital admission, n (%) | |
| Fever | 1469 (74.6%) |
| Dyspnea | 620 (31.5%) |
| Myalgia | 604 (30.7%) |
| Cough | 549 (27.9%) |
| Headache | 332 (16.9%) |
| Diarrhea | 210 (10.7%) |
| Anosmia | 167 (8.5%) |
| Ageusia | 145 (7.35%) |
| Throat Pain | 102 (5.2%) |
| Vomiting | 55 (2.8%) |
| Stay at the hospital, mean (SD), days | 11.3 (11.4) |
| Intensive Care Unit (ICU) admission | |
| Yes/No, n (%) | 130 (6.6%)/1839 (93.4%) |
| Persistent post-COVID symptoms, n (%) | |
| Fatigue | 1206 (61.3%) |
| Dyspnea at exertion | 1054 (53.5%) |
| Pain Symptoms | 887 (45.1%) |
| Loss hair | 470 (23.9%) |
| Dyspnea at rest | 459 (23.3%) |
| Memory loss | 341 (17.3%) |
| Skin Rashes | 236 (12.0%) |
| Brain fog | 189 (9.6%) |
| Concentration loss | 140 (7.1%) |
| Tachycardia-Palpitations | 140 (7.1%) |
| Gastrointestinal Disorders | 133 (6.75%) |
| Ocular/Vision Disorders | 116 (5.9%) |
| Anosmia | 80 (4.05%) |
| Ageusia | 53 (2.7%) |
| Throat Pain | 50 (2.5%) |
| Diarrhea | 49 (2.5%) |
| Voice problems | 35 (1.8%) |
| Item-Internal Consistency | Item-Discriminant Validity | Cronbach’s Alpha | Omega | Floor Effect | Ceiling Effect | |
|---|---|---|---|---|---|---|
| I feel tense or ‘wound up’ | 0.888 *** | 0.832 *** | 0.890 (HADS-A) | 0.911 (HADS-A) | 43.05% | 12.46% |
| I get a sort of frightened feeling as if something awful is about to happen | 0.845 *** | 0.768 *** | 52.97% | 11.62% | ||
| Worrying thoughts go through my mind | 0.857 *** | 0.788 *** | 43.40% | 11.45% | ||
| I can sit at ease and feel relaxed | 0.574 *** | 0.461 *** | 70.52% | 3.38% | ||
| I get a sort of frightened feeling like ‘butterflies’ in the stomach | 0.520 *** | 0.419 *** | 77.77% | 1.99% | ||
| I feel restless as I have to be on the move | 0.873 *** | 0.812 *** | 55.57% | 11.29% | ||
| I get sudden feelings of panic | 0.795 *** | 0.700 *** | 73.74% | 13.74% | ||
| I still enjoy the things I used to enjoy | 0.744 *** | 0.649 *** | 0.856 (HADS-D) | 0.821 (HADS-D) | 57.47% | 3.75% |
| I can laugh and see the funny side of things | 0.743 *** | 0.652 *** | 63.86% | 2.26% | ||
| I feel cheerful | 0.833 *** | 0.744 *** | 51.26% | 12.24% | ||
| I feel as if I am slowed down | 0.701 *** | 0.565 *** | 55.04% | 11.11% | ||
| I have lost interest in my appearance | 0.737 *** | 0.604 *** | 63.36% | 13.00% | ||
| I look forward with enjoyment to things | 0.738 *** | 0.621 *** | 54.50% | 8.03% | ||
| I can enjoy a good book or radio or TV program | 0.659 *** | 0.559 *** | 66.38% | 2.01% |
| LHS | RHS | Coef | SE | Pval | Type |
|---|---|---|---|---|---|
| Anxiety | A1 | 1.000 | Latent | ||
| Anxiety | A2 | 0.953 | 0.009 | <0.001 | Latent |
| Anxiety | A3 | 0.945 | 0.009 | <0.001 | Latent |
| Anxiety | A4 | 0.822 | 0.014 | <0.001 | Latent |
| Anxiety | A5 | 0.769 | 0.018 | <0.001 | Latent |
| Anxiety | A6 | 0.987 | 0.008 | <0.001 | Latent |
| Anxiety | A7 | 1.047 | 0.009 | <0.001 | Latent |
| Depression | D1 | 1.000 | Latent | ||
| Depression | D2 | 1.047 | 0.008 | <0.001 | Latent |
| Depression | D3 | 1.049 | 0.009 | <0.001 | Latent |
| Depression | D4 | 0.919 | 0.013 | <0.001 | Latent |
| Depression | D5 | 1.004 | 0.011 | <0.001 | Latent |
| Depression | D6 | 0.829 | 0.012 | <0.001 | Latent |
| Depression | D7 | 0.799 | 0.014 | <0.001 | Latent |
| A1 | A1 | 0.158 | vCov | ||
| A2 | A2 | 0.236 | vCov | ||
| A3 | A3 | 0.249 | vCov | ||
| A4 | A4 | 0.431 | vCov | ||
| A5 | A5 | 0.503 | vCov | ||
| A6 | A6 | 0.180 | vCov | ||
| A7 | A7 | 0.078 | vCov | ||
| D1 | D1 | 0.200 | vCov | ||
| D2 | D2 | 0.124 | vCov | ||
| D3 | D3 | 0.120 | vCov | ||
| D4 | D4 | 0.324 | vCov | ||
| D5 | D5 | 0.195 | vCov | ||
| D6 | D6 | 0.450 | vCov | ||
| D7 | D7 | 0.490 | vCov | ||
| Anxiety | Anxiety | 0.842 | 0.010 | <0.001 | vCov |
| Depression | Depression | 0.800 | 0.010 | <0.001 | vCov |
| Anxiety | Depression | 0.729 | 0.010 | <0.001 | vCov |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-de-las-Peñas, C.; Rodríguez-Jiménez, J.; Palacios-Ceña, M.; de-la-Llave-Rincón, A.I.; Fuensalida-Novo, S.; Florencio, L.L.; Ambite-Quesada, S.; Ortega-Santiago, R.; Arias-Buría, J.L.; Liew, B.X.W.; et al. Psychometric Properties of the Hospital Anxiety and Depression Scale (HADS) in Previously Hospitalized COVID-19 Patients. Int. J. Environ. Res. Public Health 2022, 19, 9273. https://doi.org/10.3390/ijerph19159273
Fernández-de-las-Peñas C, Rodríguez-Jiménez J, Palacios-Ceña M, de-la-Llave-Rincón AI, Fuensalida-Novo S, Florencio LL, Ambite-Quesada S, Ortega-Santiago R, Arias-Buría JL, Liew BXW, et al. Psychometric Properties of the Hospital Anxiety and Depression Scale (HADS) in Previously Hospitalized COVID-19 Patients. International Journal of Environmental Research and Public Health. 2022; 19(15):9273. https://doi.org/10.3390/ijerph19159273
Chicago/Turabian StyleFernández-de-las-Peñas, César, Jorge Rodríguez-Jiménez, María Palacios-Ceña, Ana I de-la-Llave-Rincón, Stella Fuensalida-Novo, Lidiane L. Florencio, Silvia Ambite-Quesada, Ricardo Ortega-Santiago, José L. Arias-Buría, Bernard X. W. Liew, and et al. 2022. "Psychometric Properties of the Hospital Anxiety and Depression Scale (HADS) in Previously Hospitalized COVID-19 Patients" International Journal of Environmental Research and Public Health 19, no. 15: 9273. https://doi.org/10.3390/ijerph19159273
APA StyleFernández-de-las-Peñas, C., Rodríguez-Jiménez, J., Palacios-Ceña, M., de-la-Llave-Rincón, A. I., Fuensalida-Novo, S., Florencio, L. L., Ambite-Quesada, S., Ortega-Santiago, R., Arias-Buría, J. L., Liew, B. X. W., Hernández-Barrera, V., & Cigarán-Méndez, M. (2022). Psychometric Properties of the Hospital Anxiety and Depression Scale (HADS) in Previously Hospitalized COVID-19 Patients. International Journal of Environmental Research and Public Health, 19(15), 9273. https://doi.org/10.3390/ijerph19159273








