Nature-Based Meditation, Rumination and Mental Wellbeing
Abstract
:1. Introduction
The Present Study
2. Materials and Methods
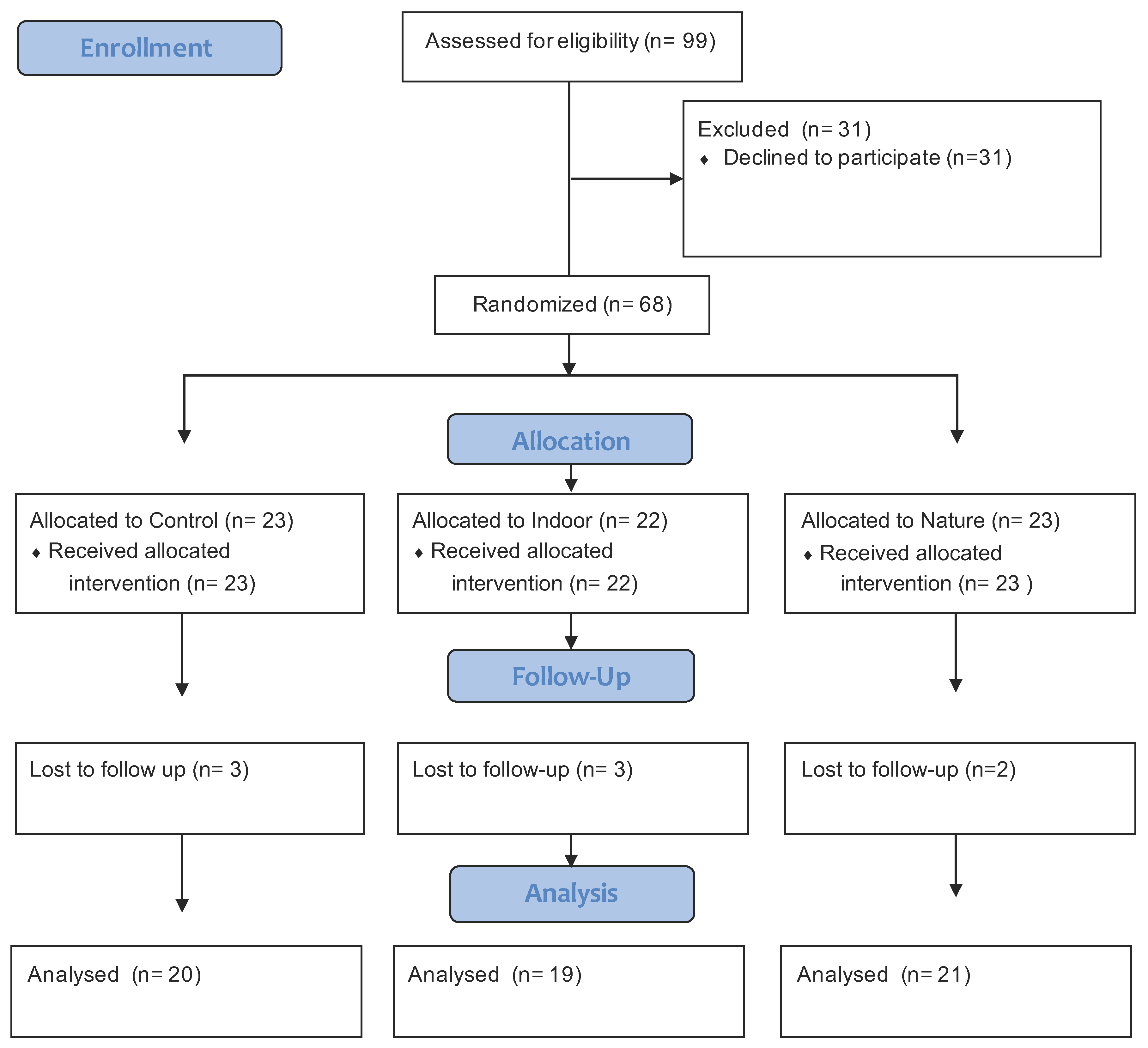
2.1. Sample Size
2.2. Hypotheses
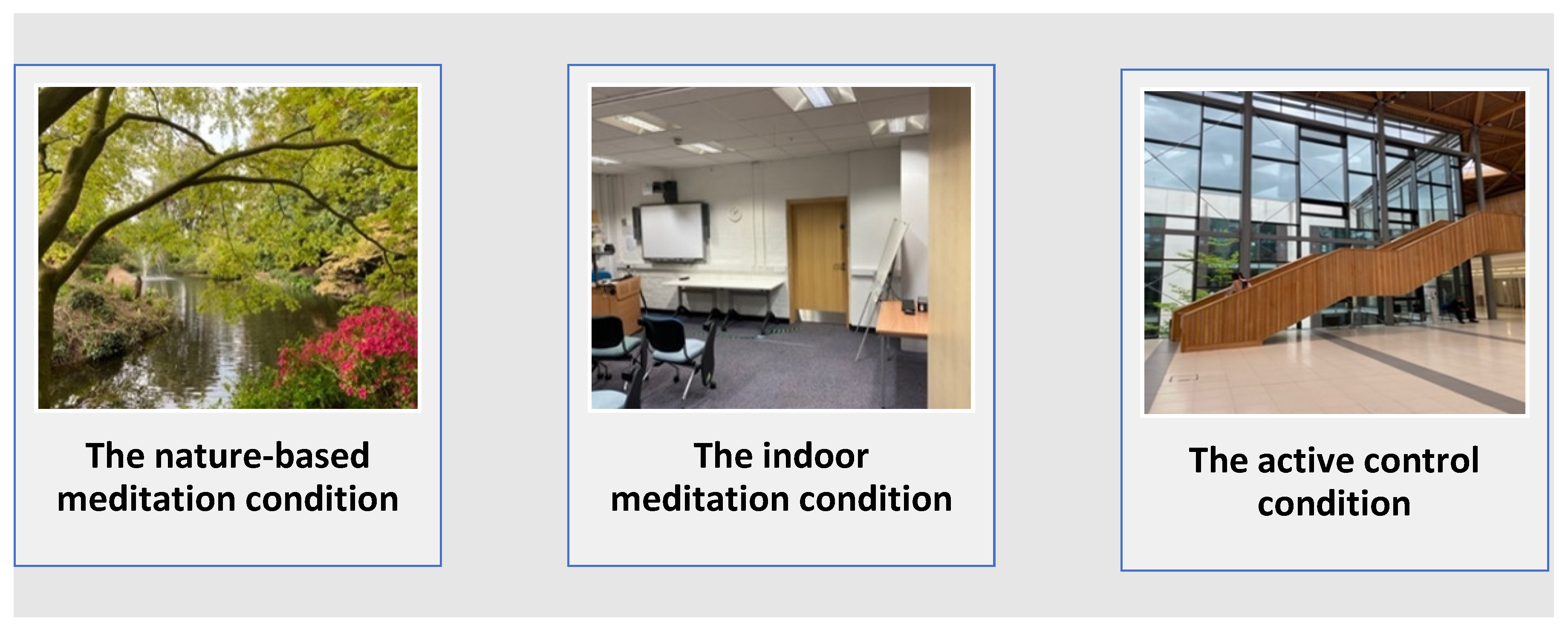
2.3. The Nature-Based Meditation Condition
2.4. The Indoor Meditation Condition
2.5. The Active Control Condition
2.6. Measures
2.6.1. Ruminative Response Styles (RRS)
2.6.2. Brief Rumination State Inventory (BSRI)
2.6.3. Patient Health Questionnaire (PHQ-8)
2.6.4. Short Warwickshire Edinburgh Mental Wellbeing Scale (SWEMWBS)
2.7. Statistical Analysis
2.8. Procedure
3. Results
3.1. Immediate Change in Rumination
3.2. Depression Symptoms and Mental Wellbeing
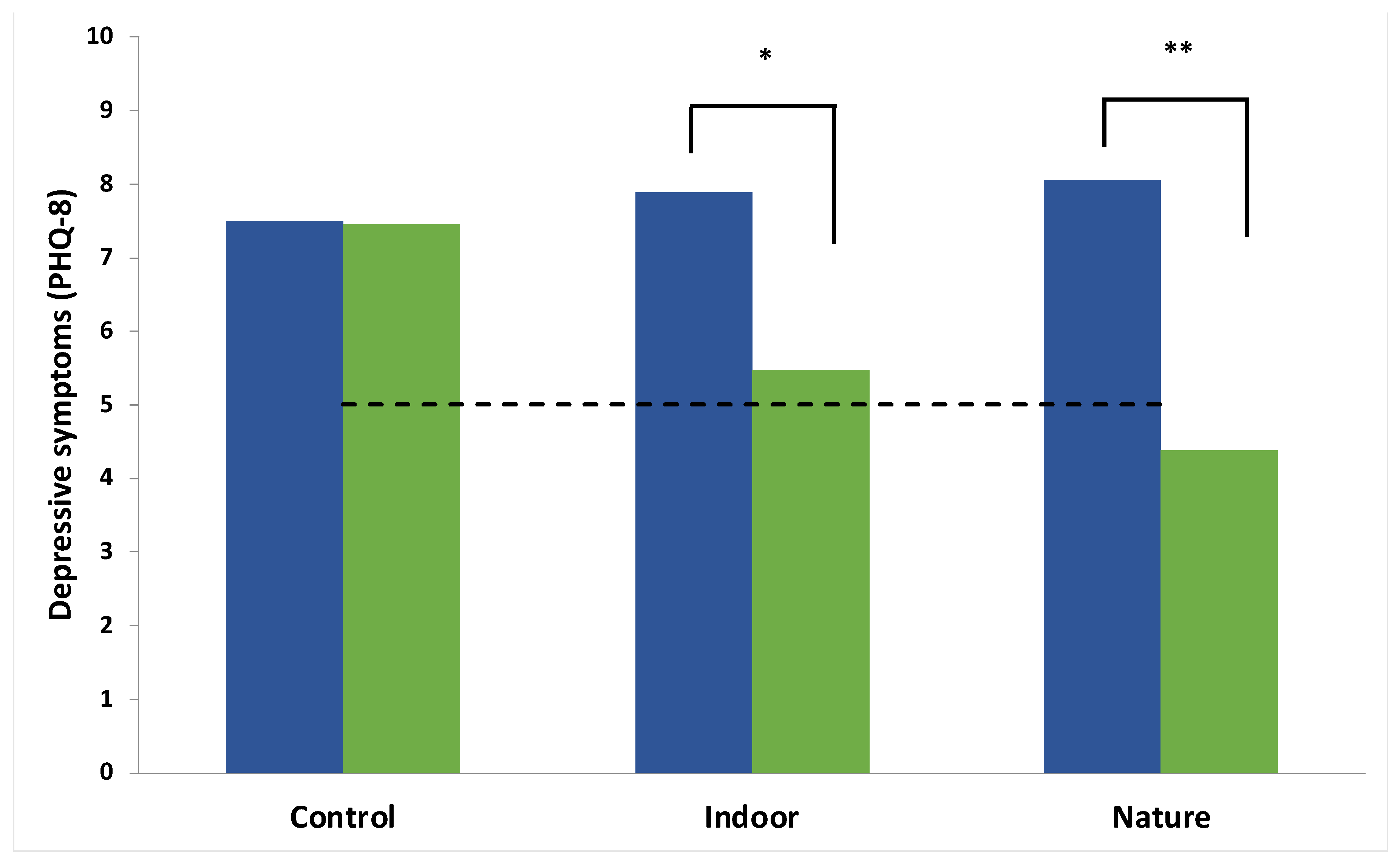
3.2.1. Depressive Symptoms
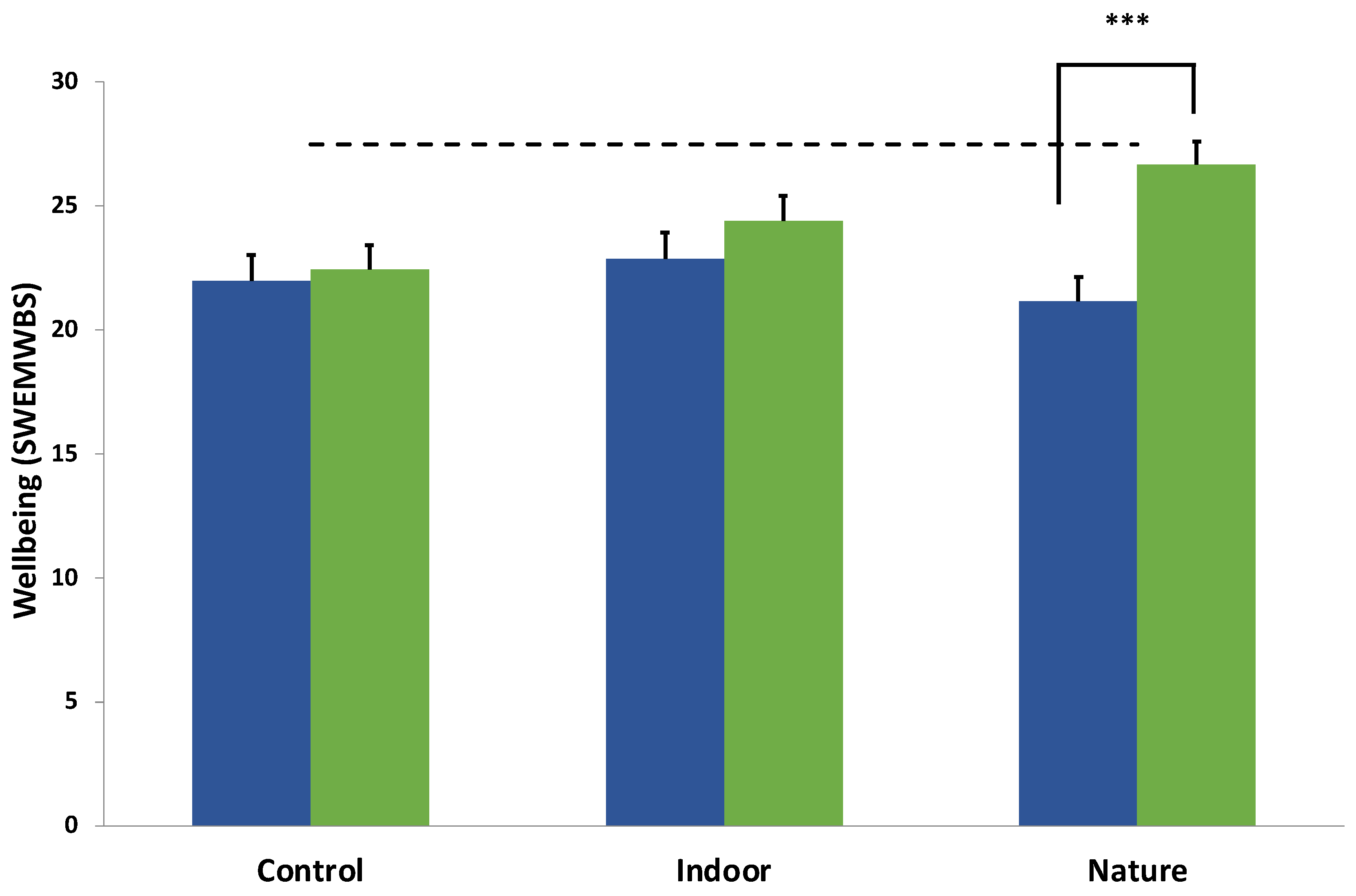
3.2.2. Wellbeing
3.3. Adherence to Meditation: A Dose–Response Analysis
4. Discussion
4.1. Clinical Implications
4.2. Strengths, Limitations & Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wittchen, H.U.; Jacobi, F.; Rehm, J.; Gustavsson, A.; Svensson, M.; Jönsson, B.; Olesen, J.; Allgulander, C.; Alonso, J.; Faravelli, C.; et al. The Size and Burden of Mental Disorders and Other Disorders of the Brain in Europe 2010. Eur. Neuropsychopharmacol. 2011, 21, 655–679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organisation. Depression and Other Common Mental Disorders: Global Health Estimates; WHO: Geneva, Switzerland, 2017.
- Owens, M.; Townsend, E.; Hall, E.; Bhatia, T.; Fitzgibbon, R.; Miller-Lakin, F. Mental Health and Wellbeing in Young People in the UK during Lockdown (COVID-19). Int. J. Environ. Res. Public Health 2022, 19, 1132. [Google Scholar] [CrossRef] [PubMed]
- Ford, T.; John, A.; Gunnell, D. Mental Health of Children and Young People during Pandemic. BMJ 2021, 372, n614. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of Mental Health Problems during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Mazidi, M.; Li, K.; Li, Y.; Chen, S.; Kirwan, R.; Zhou, H.; Yan, N.; Rahman, A.; Wang, W.; et al. Prevalence of Mental Health Problems among Children and Adolescents during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. J. Affect. Disord. 2021, 293, 78–89. [Google Scholar] [CrossRef]
- Jones, P.B. Adult Mental Health Disorders and Their Age at Onset. Br. J. Psychiatry 2013, 202, s5–s10. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef] [Green Version]
- Shorey, S.; Ng, E.D.; Wong, C.H.J. Global Prevalence of Depression and Elevated Depressive Symptoms among Adolescents: A Systematic Review and Meta-Analysis. Br. J. Clin. Psychol. 2021, 61, 287–305. [Google Scholar] [CrossRef]
- Werner-Seidler, A.; Spanos, S.; Calear, A.L.; Perry, Y.; Torok, M.; O’Dea, B.; Christensen, H.; Newby, J.M. School-Based Depression and Anxiety Prevention Programs: An Updated Systematic Review and Meta-Analysis. Clin. Psychol. Rev. 2021, 89, 102079. [Google Scholar] [CrossRef]
- Clayborne, Z.M.; Varin, M.; Colman, I. Systematic Review and Meta-Analysis: Adolescent Depression and Long-Term Psychosocial Outcomes. J. Am. Acad. Child Adolesc. Psychiatry 2019, 58, 72–79. [Google Scholar] [CrossRef] [Green Version]
- Fergusson, D.M.; Boden, J.M.; Horwood, L.J. Recurrence of Major Depression in Adolescence and Early Adulthood, and Later Mental Health, Educational and Economic Outcomes. Br. J. Psychiatry 2007, 191, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Hale, D.R.; Bevilacqua, L.; Viner, R.M. Adolescent Health and Adult Education and Employment: A Systematic Review. Pediatrics 2015, 136, 128–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alaie, I.; Philipson, A.; Ssegonja, R.; Copeland, W.E.; Ramklint, M.; Bohman, H.; Jonsson, U. Adolescent Depression and Adult Labor Market Marginalization: A Longitudinal Cohort Study. Eur. Child Adolesc. Psychiatry 2021, 1, 1–15. [Google Scholar] [CrossRef]
- Niles, A.N.; O’Donovan, A. Comparing Anxiety and Depression to Obesity and Smoking as Predictors of Major Medical Illnesses and Somatic Symptoms. Health Psychol. 2019, 38, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Chisholm, D.; Sweeny, K.; Sheehan, P.; Rasmussen, B.; Smit, F.; Cuijpers, P.; Saxena, S. Scaling-up Treatment of Depression and Anxiety: A Global Return on Investment Analysis. Lancet Psychiatry 2016, 3, 415–424. [Google Scholar] [CrossRef] [Green Version]
- O’Connell, M.E.; Boat, T.; Warner, K.E. Preventing Mental, Emotional, and Behavioral Disorders among Young People: Progress and Possibilities; The National Academies Press: Washington, DC, USA, 2009; ISBN 0309126746. [Google Scholar]
- Ebert, D.D.; Cuijpers, P. It Is Time to Invest in the Prevention of Depression. JAMA Netw. Open 2018, 1, e180335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Radez, J.; Reardon, T.; Creswell, C.; Lawrence, P.J.; Evdoka-Burton, G.; Waite, P. Why Do Children and Adolescents (Not) Seek and Access Professional Help for Their Mental Health Problems? A Systematic Review of Quantitative and Qualitative Studies. Eur. Child Adolesc. Psychiatry 2021, 30, 183–211. [Google Scholar] [CrossRef] [Green Version]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived Barriers and Facilitators to Mental Health Help-Seeking in Young People: A Systematic Review. BMC Psychiatry 2010, 10, 113. [Google Scholar] [CrossRef] [Green Version]
- Bruffaerts, R.; Mortier, P.; Auerbach, R.P.; Alonso, J.; Hermosillo De la Torre, A.E.; Cuijpers, P.; Demyttenaere, K.; Ebert, D.D.; Green, J.G.; Hasking, P.; et al. Lifetime and 12-Month Treatment for Mental Disorders and Suicidal Thoughts and Behaviors among First Year College Students. Int. J. Methods Psychiatr. Res. 2019, 28, e1764. [Google Scholar] [CrossRef] [Green Version]
- Andrews, G.; Szabo, M.; Burns, J. Preventing Major Depression in Young People. Br. J. Psychiatry 2002, 181, 460–462. [Google Scholar] [CrossRef] [Green Version]
- Cuijpers, P.; Christensen, H. Are Personalised Treatments of Adult Depression Finally within Reach? Epidemiol. Psychiatr. Sci. 2017, 26, 40–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herrman, H.; Kieling, C.; McGorry, P.; Horton, R.; Sargent, J.; Patel, V. Reducing the Global Burden of Depression: A Lancet–World Psychiatric Association Commission. Lancet 2019, 393, e42–e43. [Google Scholar] [CrossRef]
- Gunnell, D.; Kidger, J.; Elvidge, H. Adolescent Mental Health in Crisis. BMJ 2018, 361, k2608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NHS England. Implementing the Five Year Forward View for Mental Health; NHS England: London, UK, 2016.
- NHS England. Future in Mind: Promoting, Protecting and Improving Our Children and Young People’s Mental Health and Wellbeing; NHS England: London, UK, 2015.
- van Zoonen, K.; Buntrock, C.; Ebert, D.D.; Smit, F.; Reynolds, C.F.; Beekman, A.T.; Cuijpers, P. Preventing the Onset of Major Depressive Disorder: A Meta-Analytic Review of Psychological Interventions. Int. J. Epidemiol. 2014, 43, 318–329. [Google Scholar] [CrossRef]
- Havinga, P.J.; Maciejewski, D.F.; Hartman, C.A.; Hillegers, M.H.J.; Schoevers, R.A.; Penninx, B.W.J.H. Prevention Programmes for Children of Parents with a Mood/Anxiety Disorder: Systematic Review of Existing Programmes and Meta-Analysis of Their Efficacy. Br. J. Clin. Psychol. 2021, 60, 212–251. [Google Scholar] [CrossRef]
- Cuijpers, P.; Miguel, C.; Ciharova, M.; Aalten, P.; Batelaan, N.; Salemink, E.; Spinhoven, P.; Struijs, S.; de Wit, L.; Gentili, C.; et al. Prevention and Treatment of Mental Health and Psychosocial Problems in College Students: An Umbrella Review of Meta-Analyses. Clin. Psychol. Sci. Pract. 2021, 28, 229. [Google Scholar] [CrossRef]
- Bennett, S.D.; Cuijpers, P.; Ebert, D.D.; McKenzie Smith, M.; Coughtrey, A.E.; Heyman, I.; Manzotti, G.; Shafran, R. Practitioner Review: Unguided and Guided Self-Help Interventions for Common Mental Health Disorders in Children and Adolescents: A Systematic Review and Meta-Analysis. J. Child Psychol. Psychiatry 2019, 60, 828–847. [Google Scholar] [CrossRef]
- Firth, J.; Solmi, M.; Wootton, R.E.; Vancampfort, D.; Schuch, F.B.; Hoare, E.; Gilbody, S.; Torous, J.; Teasdale, S.B.; Jackson, S.E.; et al. A Meta-review of “Lifestyle Psychiatry”: The Role of Exercise, Smoking, Diet and Sleep in the Prevention and Treatment of Mental Disorders. World Psychiatry 2020, 19, 360–380. [Google Scholar] [CrossRef]
- Piotrowski, M.C.; Lunsford, J.; Gaynes, B.N. Lifestyle Psychiatry for Depression and Anxiety: Beyond Diet and Exercise. Lifestyle Med. 2021, 2, e21. [Google Scholar] [CrossRef]
- Bratman, G.N.; Anderson, C.B.; Berman, M.G.; Cochran, B.; de Vries, S.; Flanders, J.; Folke, C.; Frumkin, H.; Gross, J.J.; Hartig, T.; et al. Nature and Mental Health: An Ecosystem Service Perspective. Sci. Adv. 2019, 5, 903–927. [Google Scholar] [CrossRef] [Green Version]
- Frumkin, H.; Bratman, G.N.; Breslow, S.J.; Cochran, B.; Kahn, P.H.; Lawler, J.J.; Levin, P.S.; Tandon, P.S.; Varanasi, U.; Wolf, K.L.; et al. Nature Contact and Human Health: A Research Agenda. Environ. Health Perspect. 2017, 125, 075001. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Twohig-Bennett, C.; Jones, A. The Health Benefits of the Great Outdoors: A Systematic Review and Meta-Analysis of Greenspace Exposure and Health Outcomes. Environ. Res. 2018, 166, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Williams, T.; Barnwell, G.C.; Stein, D.J. A Systematic Review of Randomised Controlled Trials on the Effectiveness of Ecotherapy Interventions for Treating Mental Disorders. medRxiv 2020. [Google Scholar] [CrossRef]
- Cox, D.T.C.; Shanahan, D.F.; Hudson, H.L.; Fuller, R.A.; Anderson, K.; Hancock, S.; Gaston, K.J. Doses of Nearby Nature Simultaneously Associated with Multiple Health Benefits. Int. J. Environ. Res. Public Health 2017, 14, 172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yao, W.; Zhang, X.; Gong, Q. The Effect of Exposure to the Natural Environment on Stress Reduction: A Meta-Analysis. Urban For. Urban Green. 2021, 57, 126932. [Google Scholar] [CrossRef]
- Antonelli, M.; Donelli, D.; Carlone, L.; Maggini, V.; Firenzuoli, F.; Bedeschi, E. Effects of Forest Bathing (Shinrin-Yoku) on Individual Well-Being: An Umbrella Review. Int. J. Environ. Health Res. 2021, 32, 1842–1867. [Google Scholar] [CrossRef]
- Antonelli, M.; Barbieri, G.; Donelli, D. Effects of Forest Bathing (Shinrin-Yoku) on Levels of Cortisol as a Stress Biomarker: A Systematic Review and Meta-Analysis. Int. J. Biometeorol. 2019, 63, 1117–1134. [Google Scholar] [CrossRef]
- Kotera, Y.; Richardson, M.; Sheffield, D. Effects of Shinrin-Yoku (Forest Bathing) and Nature Therapy on Mental Health: A Systematic Review and Meta-Analysis. Int. J. Ment. Health Addict. 2022, 20, 337–361. [Google Scholar] [CrossRef]
- Hossain, M.; Sultana, A.; Ma, P.; Fan, Q.; Sharma, R.; Purohit, N.; Sharmin, D.F. Effects of Natural Environment on Mental Health: An Umbrella Review of Systematic Reviews and Meta-Analyses. PsyArXiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Rosa, C.D.; Larson, L.R.; Collado, S.; Profice, C.C. Forest Therapy Can Prevent and Treat Depression: Evidence from Meta-Analyses. Urban For. Urban Green. 2021, 57, 126943. [Google Scholar] [CrossRef]
- Stier-Jarmer, M.; Throner, V.; Kirschneck, M.; Immich, G.; Frisch, D.; Schuh, A. The Psychological and Physical Effects of Forests on Human Health: A Systematic Review of Systematic Reviews and Meta-Analyses. Int. J. Environ. Res. Public Health 2021, 18, 1770. [Google Scholar] [CrossRef] [PubMed]
- Owens, M.; Bunce, H.L.I. The Potential for Outdoor Nature-Based Interventions in the Treatment and Prevention of Depression. Front. Psychol. 2022, 13, 1–14. [Google Scholar] [CrossRef]
- Watkins, E.R. Constructive and Unconstructive Repetitive Thought. Psychol. Bull. 2008, 134, 163–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clancy, F.; Prestwich, A.; Caperon, L.; O’Connor, D.B. Perseverative Cognition and Health Behaviors: A Systematic Review and Meta-Analysis. Front. Hum. Neurosci. 2016, 10, 534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watkins, E.R.; Roberts, H. Reflecting on Rumination: Consequences, Causes, Mechanisms and Treatment of Rumination. Behav. Res. Ther. 2020, 127, 103573. [Google Scholar] [CrossRef]
- Joubert, A.E.; Moulds, M.L.; Werner-Seidler, A.; Sharrock, M.; Popovic, B.; Newby, J.M.; Amy Joubert, C.E. Understanding the Experience of Rumination and Worry: A Descriptive Qualitative Survey Study. Br. J. Clin. Psychol. 2022, 1–18. [Google Scholar] [CrossRef]
- Watkins, E.R.; Mullan, E.; Wingrove, J.; Rimes, K.; Steiner, H.; Bathurst, N.; Eastman, R.; Scott, J. Rumination-Focused Cognitive–Behavioural Therapy for Residual Depression: Phase II Randomised Controlled Trial. Br. J. Psychiatry 2011, 199, 317–322. [Google Scholar] [CrossRef]
- Topper, M.; Emmelkamp, P.; Watkins, E.; Ehring, T. Prevention of Anxiety Disorders and Depression by Targeting Excessive Worry and Rumination in Adolescents and Young Adults: A Randomized Controlled Trial. Behav. Res. Ther. 2017, 90, 123–136. [Google Scholar] [CrossRef]
- Umegaki, Y.; Nakagawa, A.; Watkins, E.; Mullan, E. A Rumination-Focused Cognitive-Behavioral Therapy Self-Help Program to Reduce Depressive Rumination in High-Ruminating Japanese Female University Students: A Case Series Study. Cogn. Behav. Pract. 2022, 29, 468–484. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Mindfulness-Based Interventions in Context: Past, Present, and Future. Clin. Psychol. Sci. Pract. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Khoury, B.; Lecomte, T.; Fortin, G.; Masse, M.; Therien, P.; Bouchard, V.; Chapleau, M.A.; Paquin, K.; Hofmann, S.G. Mindfulness-Based Therapy: A Comprehensive Meta-Analysis. Clin. Psychol. Rev. 2013, 33, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Kuyken, W.; Hayes, R.; Barrett, B.; Byng, R.; Dalgleish, T.; Kessler, D.; Lewis, G.; Watkins, E.; Brejcha, C.; Cardy, J.; et al. Effectiveness and Cost-Effectiveness of Mindfulness-Based Cognitive Therapy Compared with Maintenance Antidepressant Treatment in the Prevention of Depressive Relapse or Recurrence (PREVENT): A Randomised Controlled Trial. Lancet 2015, 386, 63–73. [Google Scholar] [CrossRef]
- Goldberg, S.B.; Tucker, R.P.; Greene, P.A.; Davidson, R.J.; Wampold, B.E.; Kearney, D.J.; Simpson, T.L. Mindfulness-Based Interventions for Psychiatric Disorders: A Systematic Review and Meta-Analysis. Clin. Psychol. Rev. 2018, 59, 52–60. [Google Scholar] [CrossRef] [PubMed]
- NICE Guidelines. 2018. Available online: https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-guidelines (accessed on 16 June 2022).
- Elices, M.; Pérez-Sola, V.; Pérez-Aranda, A.; Colom, F.; Polo, M.; Martín-López, L.M.; Gárriz, M. The Effectiveness of Mindfulness-Based Cognitive Therapy in Primary Care and the Role of Depression Severity and Treatment Attendance. Mindfulness 2022, 13, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Strauss, C.; Bond, R.; Cavanagh, K. How Do Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction Improve Mental Health and Wellbeing? A Systematic Review and Meta-Analysis of Mediation Studies. Clin. Psychol. Rev. 2015, 37, 1–12. [Google Scholar] [CrossRef]
- Winnebeck, E.; Fissler, M.; Gärtner, M.; Chadwick, P.; Barnhofer, T. Brief Training in Mindfulness Meditation Reduces Symptoms in Patients with a Chronic or Recurrent Lifetime History of Depression: A Randomized Controlled Study. Behav. Res. Ther. 2017, 99, 124–130. [Google Scholar] [CrossRef] [Green Version]
- Djernis, D.; Lerstrup, I.; Poulsen, D.; Stigsdotter, U.; Dahlgaard, J.; O’Toole, M. A Systematic Review and Meta-Analysis of Nature-Based Mindfulness: Effects of Moving Mindfulness Training into an Outdoor Natural Setting. Int. J. Environ. Res. Public Health 2019, 16, 3202. [Google Scholar] [CrossRef] [Green Version]
- Nisbet, E.K.; Zelenski, J.M.; Grandpierre, Z. Mindfulness in Nature Enhances Connectedness and Mood. Ecopsychology 2019, 11, 81–91. [Google Scholar] [CrossRef]
- Stigsdotter, U.K.; Corazon, S.S.; Sidenius, U.; Nyed, P.K.; Larsen, H.B.; Fjorback, L.O. Efficacy of Nature-Based Therapy for Individuals with Stress-Related Illnesses: Randomised Controlled Trial. Br. J. Psychiatry 2018, 213, 404–411. [Google Scholar] [CrossRef]
- McEwan, K.; Giles, D.; Clarke, F.J.; Kotera, Y.; Evans, G.; Terebenina, O.; Minou, L.; Teeling, C.; Basran, J.; Wood, W.; et al. A Pragmatic Controlled Trial of Forest Bathing Compared with Compassionate Mind Training in the UK: Impacts on Self-Reported Wellbeing and Heart Rate Variability. Sustainability 2021, 13, 1380. [Google Scholar] [CrossRef]
- Choe, E.Y.; Jorgensen, A.; Sheffield, D. Does a Natural Environment Enhance the Effectiveness of Mindfulness-Based Stress Reduction (MBSR)? Examining the Mental Health and Wellbeing, and Nature Connectedness Benefits. Landsc. Urban Plan. 2020, 202, 1–12. [Google Scholar] [CrossRef]
- Berman, M.G.; Kross, E.; Krpan, K.M.; Askren, M.K.; Burson, A.; Deldin, P.J.; Kaplan, S.; Sherdell, L.; Gotlib, I.H.; Jonides, J. Interacting with Nature Improves Cognition and Affect for Individuals with Depression. J. Affect. Disord. 2012, 140, 300–305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bratman, G.N.; Hamilton, J.P.; Hahn, K.S.; Daily, G.C.; Gross, J.J. Nature Experience Reduces Rumination and Subgenual Prefrontal Cortex Activation. Proc. Natl. Acad. Sci. USA 2015, 112, 8567–8572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, H.X.; Chen, X.; Shen, Y.Q.; Li, L.; Chen, N.X.; Zhu, Z.C.; Castellanos, F.X.; Yan, C.G. Rumination and the Default Mode Network: Meta-Analysis of Brain Imaging Studies and Implications for Depression. Neuroimage 2020, 206, 116287. [Google Scholar] [CrossRef]
- Bratman, G.N.; Young, G.; Mehta, A.; Lee Babineaux, I.; Daily, G.C.; Gross, J.J. Affective Benefits of Nature Contact: The Role of Rumination. Front. Psychol. 2021, 12, 643866. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, P. Introducing Compassion-Focused Therapy. Adv. Psychiatr. Treat. 2009, 15, 199–208. [Google Scholar] [CrossRef] [Green Version]
- Porges, S.W. The Polyvagal Perspective. Biol. Psychol. 2007, 74, 116–143. [Google Scholar] [CrossRef]
- Kosslyn, S.M.; Ganis, G.; Thompson, W.L. Neural Foundations of Imagery. Nat. Rev. Neurosci. 2001, 2, 635–642. [Google Scholar] [CrossRef]
- Holmes, E.A.; Mathews, A. Mental Imagery in Emotion and Emotional Disorders. Clin. Psychol. Rev. 2010, 30, 349–362. [Google Scholar] [CrossRef]
- Treynor, W.; Gonzalez, R.; Nolen-Hoeksema, S. Rumination Reconsidered: A Psychometric Analysis. Cogn. Ther. Res. 2003, 27, 247–259. [Google Scholar] [CrossRef]
- Roelofs, J.; Muris, P.; Huibers, M.; Peeters, F.; Arntz, A. On the Measurement of Rumination: A Psychometric Evaluation of the Ruminative Response Scale and the Rumination on Sadness Scale in Undergraduates. J. Behav. Ther. Exp. Psychiatry 2006, 37, 299–313. [Google Scholar] [CrossRef] [PubMed]
- Marchetti, I.; Mor, N.; Chiorri, C.; Koster, E.H.W. The Brief State Rumination Inventory (BSRI): Validation and Psychometric Evaluation. Cogn. Ther. Res. 2018, 42, 447–460. [Google Scholar] [CrossRef] [Green Version]
- Kroenke, K.; Strine, T.W.; Spitzer, R.L.; Williams, J.B.W.; Berry, J.T.; Mokdad, A.H. The PHQ-8 as a Measure of Current Depression in the General Population. J. Affect. Disord. 2009, 114, 163–173. [Google Scholar] [CrossRef]
- Wu, Y.; Levis, B.; Riehm, K.E.; Saadat, N.; Levis, A.W.; Azar, M.; Rice, D.B.; Boruff, J.; Cuijpers, P.; Gilbody, S.; et al. Equivalency of the Diagnostic Accuracy of the PHQ-8 and PHQ-9: A Systematic Review and Individual Participant Data Meta-Analysis. Psychol. Med. 2020, 50, 1368–1380. [Google Scholar] [CrossRef]
- Kroenke, K.; Wu, J.; Yu, Z.; Bair, M.J.; Kean, J.; Stump, T.; Monahan, P.O. The Patient Health Questionnaire Anxiety and Depression Scale (PHQ-ADS): Initial Validation in Three Clinical Trials. Psychosom. Med. 2016, 78, 716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levis, B.; Benedetti, A.; Thombs, B.D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for Screening to Detect Major Depression: Individual Participant Data Meta-Analysis. BMJ 2019, 365, 1476. [Google Scholar] [CrossRef] [Green Version]
- Clarke, A.; Friede, T.; Putz, R.; Ashdown, J.; Martin, S.; Blake, A.; Adi, Y.; Parkinson, J.; Flynn, P.; Platt, S.; et al. Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): Validated for Teenage School Students in England and Scotland. A Mixed Methods Assessment. BMC Public Health 2011, 11, 487. [Google Scholar] [CrossRef] [Green Version]
- Maheswaran, H.; Weich, S.; Powell, J.; Stewart-Brown, S. Evaluating the Responsiveness of the Warwick Edinburgh Mental Well-Being Scale (WEMWBS): Group and Individual Level Analysis. Health Qual. Life Outcomes 2012, 10, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Stewart-Brown, S.; Tennant, A.; Tennant, R.; Platt, S.; Parkinson, J.; Weich, S. Internal Construct Validity of the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): A Rasch Analysis Using Data from the Scottish Health Education Population Survey. Health Qual. Life Outcomes 2009, 7, 15. [Google Scholar] [CrossRef] [Green Version]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Dinburgh Mental Well-Being Scale (WEMWBS): Development and UK Validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef] [Green Version]
- Shah, N.; Cader, M.; Andrews, W.P.; Wijesekera, D.; Stewart-Brown, S.L. Responsiveness of the Short Warwick Edinburgh Mental Well-Being Scale (SWEMWBS): Evaluation a Clinical Sample. Health Qual. Life Outcomes 2018, 16, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng Fat, L.; Scholes, S.; Boniface, S.; Mindell, J.; Stewart-Brown, S. Evaluating and Establishing National Norms for Mental Wellbeing Using the Short Warwick–Edinburgh Mental Well-Being Scale (SWEMWBS): Findings from the Health Survey for England. Qual. Life Res. 2017, 26, 1129–1144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mbah, A.K.; Paothong, A. Shapiro–Francia Test Compared to Other Normality Test Using Expected p-Value. J. Stat. Comput. Simul. 2014, 85, 3002–3016. [Google Scholar] [CrossRef]
- Galante, J.; Dufour, G.; Vainre, M.; Wagner, A.P.; Stochl, J.; Benton, A.; Lathia, N.; Howarth, E.; Jones, P.B. A Mindfulness-Based Intervention to Increase Resilience to Stress in University Students (the Mindful Student Study): A Pragmatic Randomised Controlled Trial. Lancet Public Health 2018, 3, e72–e81. [Google Scholar] [CrossRef] [Green Version]
- Breedvelt, J.J.F.; Amanvermez, Y.; Harrer, M.; Karyotaki, E.; Gilbody, S.; Bockting, C.L.H.; Cuijpers, P.; Ebert, D.D. The Effects of Meditation, Yoga, and Mindfulness on Depression, Anxiety, and Stress in Tertiary Education Students: A Meta-Analysis. Front. Psychiatry 2019, 10, 193. [Google Scholar] [CrossRef]
- Schumer, M.C.; Lindsay, E.K.; David Creswell, J. Brief Mindfulness Training for Negative Affectivity: A Systematic Review and Meta-Analysis. J. Consult. Clin. Psychol. 2018, 86, 569–583. [Google Scholar] [CrossRef]
- Hilt, L.M.; Pollak, S.D. Getting out of Rumination: Comparison of Three Brief Interventions in a Sample of Youth. J. Abnorm. Child Psychol. 2012, 40, 1157–1165. [Google Scholar] [CrossRef]
- Frostadottir, A.D.; Dorjee, D. Effects of Mindfulness Based Cognitive Therapy (MBCT) and Compassion Focused Therapy (CFT) on Symptom Change, Mindfulness, Self-Compassion, and Rumination in Clients with Depression, Anxiety, and Stress. Front. Psychol. 2019, 10, 1099. [Google Scholar] [CrossRef]
- Chambers, R.; Lo, B.C.Y.; Allen, N.B. The Impact of Intensive Mindfulness Training on Attentional Control, Cognitive Style, and Affect. Cogn. Ther. Res. 2008, 32, 303–322. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Simons, R.F.; Losito, B.D.; Fiorito, E.; Miles, M.A.; Zelson, M. Stress Recovery during Exposure to Natural and Urban Environments. J. Environ. Psychol. 1991, 11, 201–230. [Google Scholar] [CrossRef]
- Robinson, M.S.; Alloy, L.B. Negative Cognitive Styles and Stress-Reactive Rumination Interact to Predict Depression: A Prospective Study. Cogn. Ther. Res. 2003, 27, 275–291. [Google Scholar] [CrossRef]
- Connolly, S.L.; Alloy, L.B. Rumination Interacts with Life Stress to Predict Depressive Symptoms: An Ecological Momentary Assessment Study. Behav. Res. Ther. 2017, 97, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Kross, E.; Davidson, M.; Weber, J.; Psychiatry, K.O.-B. Coping with Emotions Past: The Neural Bases of Regulating Affect Associated with Negative Autobiographical Memories. Biol. Psychiatry 2009, 65, 361–366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamilton, J.; Farmer, M.; Fogelman, P.; Gotlib, I. Depressive Rumination, the Default-Mode Network, and the Dark Matter of Clinical Neuroscience. Biol. Psychiatry 2015, 78, 224–230. [Google Scholar] [CrossRef] [Green Version]
- Owens, M.; Herbert, J.; Jones, P.B.; Sahakian, B.J.; Wilkinson, P.O.; Dunn, V.J.; Croudace, T.J.; Goodyer, I.M. Elevated Morning Cortisol Is a Stratified Populationlevel Biomarker for Major Depression in Boys Only with High Depressive Symptoms. Proc. Natl. Acad. Sci. USA 2014, 111, 3638–3643. [Google Scholar] [CrossRef] [Green Version]
- Jahn, A.L.; Fox, A.S.; Abercrombie, H.C.; Shelton, S.E.; Oakes, T.R.; Davidson, R.J.; Kalin, N.H. Subgenual Prefrontal Cortex Activity Predicts Individual Differences in Hypothalamic-Pituitary-Adrenal Activity Across Different Contexts. Biol. Psychiatry 2010, 67, 175–181. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, S. The Restorative Benefits of Nature: Toward an Integrative Framework. J. Environ. Psychol. 1995, 15, 169–182. [Google Scholar] [CrossRef]
- Kaplan, S.; Berman, M.G. Directed Attention as a Common Resource for Executive Functioning and Self-Regulation. Perspect Psychol. Sci. 2010, 5, 43–57. [Google Scholar] [CrossRef]
- Yaroslavsky, I.; Allard, E.S.; Sanchez-Lopez, A. Can’t Look Away: Attention Control Deficits Predict Rumination, Depression Symptoms and Depressive Affect in Daily Life. J. Affect. Disord. 2019, 245, 1061–1069. [Google Scholar] [CrossRef]
- Ohly, H.; White, M.P.; Wheeler, B.W.; Bethel, A.; Ukoumunne, O.C.; Nikolaou, V.; Garside, R. Attention Restoration Theory: A Systematic Review of the Attention Restoration Potential of Exposure to Natural Environments. J. Toxicol. Environ. Health Part B Crit. Rev. 2016, 19, 305–343. [Google Scholar] [CrossRef] [Green Version]
- Vanderlind, W.M.; Everaert, J.; Joormann, J. Positive Emotion in Daily Life: Emotion Regulation and Depression. Emotion 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Rohde, P.; Brière, F.N.; Stice, E. Major Depression Prevention Effects for a Cognitive-Behavioral Adolescent Indicated Prevention Group Intervention across Four Trials. Behav. Res. Ther. 2018, 100, 1–6. [Google Scholar] [CrossRef]
- Quach, D.; Gibler, R.C.; Jastrowski Mano, K.E. Does Home Practice Compliance Make a Difference in the Effectiveness of Mindfulness Interventions for Adolescents? Mindfulness 2017, 8, 495–504. [Google Scholar] [CrossRef]
- Manigault, A.W.; Slutsky, J.; Raye, J.; Creswell, J.D. Examining Practice Effects in a Randomized Controlled Trial: Daily Life Mindfulness Practice Predicts Stress Buffering Effects of Mindfulness Meditation Training. Mindfulness 2021, 12, 2487–2497. [Google Scholar] [CrossRef]
- Bowles, N.I.; Davies, J.N.; Van Dam, N.T. Dose-Response Relationship of Reported Lifetime Meditation Practice with Mental-Health and Wellbeing: A Cross Sectional Study. MindRxiv 2022. [Google Scholar] [CrossRef]
- Tifft, E.D.; Underwood, S.B.; Roberts, M.Z.; Forsyth, J.P. Using Meditation in a Control vs. Acceptance Context: A Preliminary Evaluation of Relations with Anxiety, Depression, and Indices of Well-Being. J. Clin. Psychol. 2022, 78, 1407–1421. [Google Scholar] [CrossRef]
- McDermut, W.; Miller, I.W.; Brown, R.A. The Efficacy of Group Psychotherapy for Depression: A Meta-Analysis and Review of the Empirical Research. Clin. Psychol. Sci. Pract. 2001, 8, 98–116. [Google Scholar] [CrossRef]
- Høglend, P.; Hagtvet, K. Change Mechanisms in Psychotherapy: Both Improved Insight and Improved Affective Awareness Are Necessary. J. Consult. Clin. Psychol. 2019, 87, 332–344. [Google Scholar] [CrossRef]
- Cheung, R.Y.M.; Ng, M.C.Y. Mindfulness and Symptoms of Depression and Anxiety: The Underlying Roles of Awareness, Acceptance, Impulse Control, and Emotion Regulation. Mindfulness 2019, 10, 1124–1135. [Google Scholar] [CrossRef]
- Roth, A.; Fonagy, P. What Works for Whom? A Critical Review of Psychotherapy Research; Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- Sweeney, A.; Filson, B.; Kennedy, A.; Collinson, L.; Gillard, S. A Paradigm Shift: Relationships in Trauma-Informed Mental Health Services. BJPsych. Adv. 2018, 24, 319–333. [Google Scholar] [CrossRef] [Green Version]
- Cooley, S.J.; Jones, C.R.; Kurtz, A.; Robertson, N. ‘Into the Wild’: A Meta-Synthesis of Talking Therapy in Natural Outdoor Spaces. Clin. Psychol. Rev. 2020, 77, 101841. [Google Scholar] [CrossRef] [PubMed]
- Ji, J.L.; Kavanagh, D.J.; Holmes, E.A.; Macleod, C.; di Simplicio, M. Mental Imagery in Psychiatry: Conceptual & Clinical Implications. CNS Spectr. 2019, 24, 114–126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, S.; Gur, R.M.; David, Z.; Currier, E. One-Session Mindfulness Meditation: A Randomized Controlled Study of Effects on Cognition and Mood. Mindfulness 2015, 6, 88–98. [Google Scholar] [CrossRef]

| Variable | Untransformed Distribution | Square Root Transformation |
|---|---|---|
| RRS T0 | W′ = 0.97, p = 0.14 | - |
| RRS T1 | W′ = 0.97, p = 0.12 | - |
| BSRI T0 | W′ = 0.98, p = 0.48 | - |
| BSRI T1 | W′ = 0.99, p = 0.58 | - |
| PHQ-8 T0 | W′ = 0.93, p < 0.001 | W′ = 0.99, p = 0.84 |
| PHQ-8 T2 | W′ = 0.93, p < 0.001 | W′ = 0.99, p = 0.68 |
| SWEMWBS T0 | W′ = 0.99, p = 0.93 | - |
| SWEMWBS T2 | W′ = 0.99, p = 0.66 | - |
| Outcome | T0 | Baseline Differences (p-Value *) | T1 | T2 | Simple Main Effects of Group ** |
|---|---|---|---|---|---|
| Mean (sd) | Mean (sd) | Mean (sd) | |||
| RRS | 0.25 | ||||
| Nature | 12.04 (3.90) | 12.04 (3.90) | 10.48 (2.94) | F(1,65) = 11.14, p = 0.001, η2 = 0.15 | |
| Indoor | 10.77 (3.29) | 10.77 (3.29) | 11.05 (3.20) | F(1,65) = 0.32, p = 0.57, η2 = 0.01 | |
| Control | 12.57 (3.90) | 12.57 (3.90) | 11.87 (3.20) | F(1,65) = 2.2, p = 0.14, η2 = 0.03 | |
| BSRI | 0.64 | ||||
| Nature | 357.65 (180.38) | 269.04 (146.61) | F(1,65) = 11.79, p = 0.001, η2 = 0.15 | ||
| Indoor | 325.45 (166.96) | 307.27 (155.35) | F(1,65) = 0.48, p = 0.49, η2 = 0.01 | ||
| Control | 374.78 (183.08) | 356.00 (205.49) | F(1,65) = 0.53, p = 0.47, η2 = 0.01 | ||
| PHQ-8 | 0.85 | ||||
| Nature | 8.05 (4.66) | 4.38 (4.48) | F(1,57) = 13.94, p < 0.001, η2 = 0.20 | ||
| Indoor | 7.89 (5.23) | 5.47 (2.55) | F(1,57) = 5.50, p = 0.02, η2 = 0.09 | ||
| Control | 7.50 (5.30) | 7.45 (5.54) | F(1,57) = 0.00, p = 0.96, η2 = 0.00 | ||
| SWEMWBS | 0.38 | ||||
| Nature | 21.14 (4.16) | 26.67 (5.03) | F(1,57) = 40.10, p < 0.001, η2 = 0.41 | ||
| Indoor | 22.89 (4.38) | 24.42 (3.52) | F(1,57) = 2.78, p = 0.10, η2 = 0.05 | ||
| Control | 22.00 (5.17) | 22.45 (4.14) | F(1,57) = 0.25, p = 0.62, η2 = 0.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Owens, M.; Bunce, H.L.I. Nature-Based Meditation, Rumination and Mental Wellbeing. Int. J. Environ. Res. Public Health 2022, 19, 9118. https://doi.org/10.3390/ijerph19159118
Owens M, Bunce HLI. Nature-Based Meditation, Rumination and Mental Wellbeing. International Journal of Environmental Research and Public Health. 2022; 19(15):9118. https://doi.org/10.3390/ijerph19159118
Chicago/Turabian StyleOwens, Matthew, and Hannah L. I. Bunce. 2022. "Nature-Based Meditation, Rumination and Mental Wellbeing" International Journal of Environmental Research and Public Health 19, no. 15: 9118. https://doi.org/10.3390/ijerph19159118
APA StyleOwens, M., & Bunce, H. L. I. (2022). Nature-Based Meditation, Rumination and Mental Wellbeing. International Journal of Environmental Research and Public Health, 19(15), 9118. https://doi.org/10.3390/ijerph19159118





