Endoscopic Endonasal Repair of Congenital Choanal Atresia: Predictive Factors of Surgical Stability and Healing Outcomes
Abstract
:1. Introduction
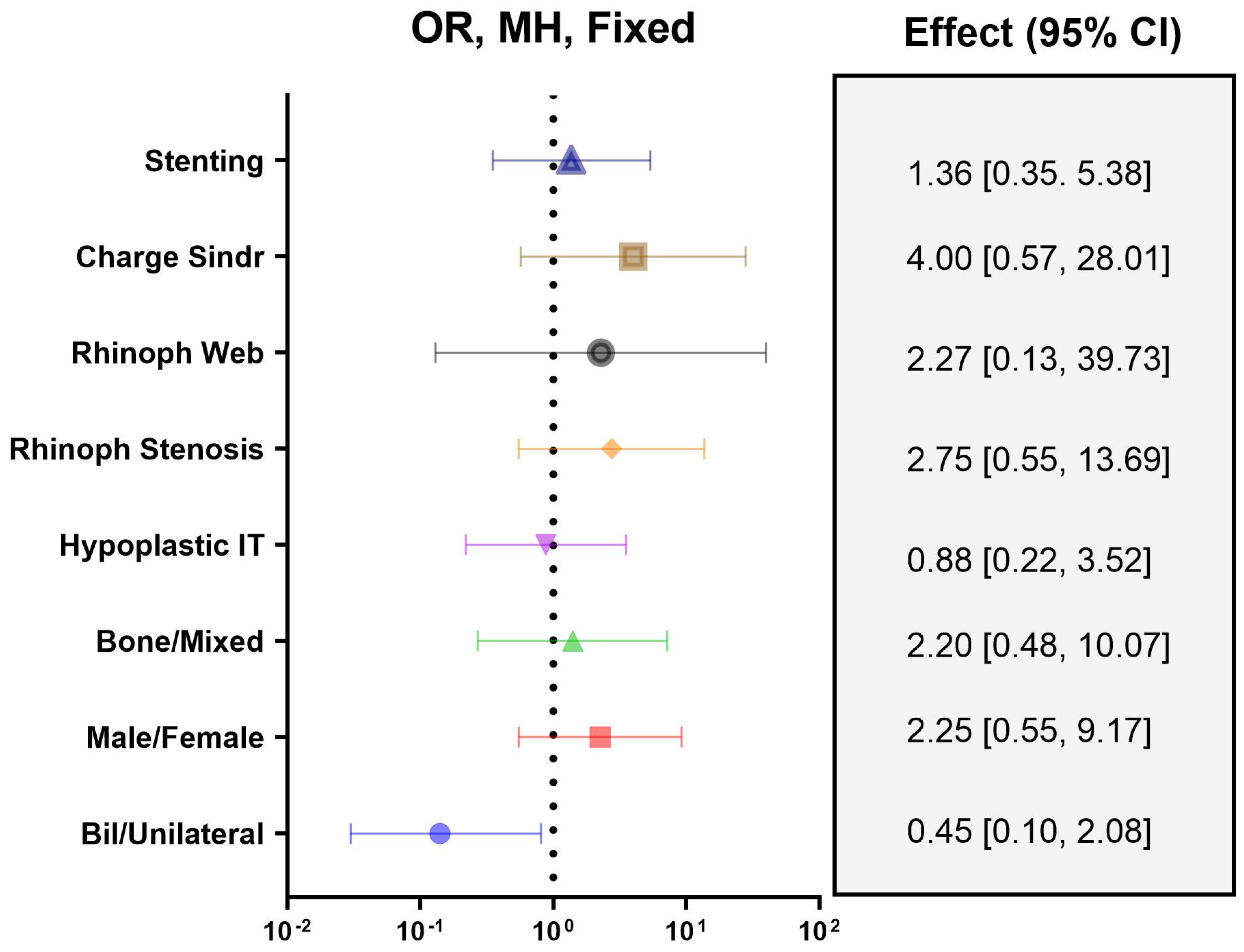
2. Materials and Methods
2.1. Surgical Technique and Postoperative Management
2.2. Nasal Stenting
2.3. Follow-Up and Postoperative Outcomes
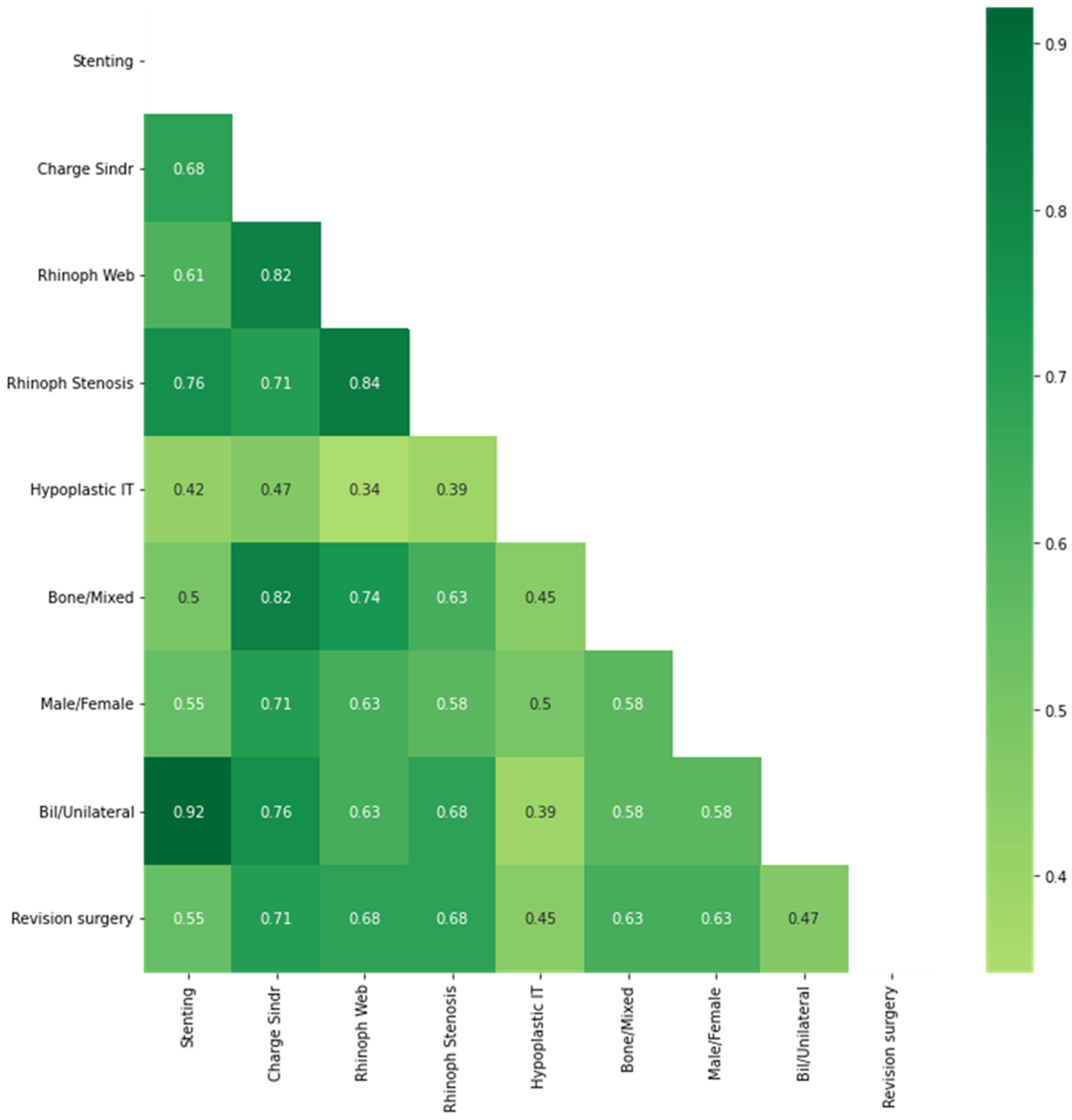
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pasquini, E.; Sciarretta, V.; Saggese, D.; Cantaroni, C.; Macrì, G.; Farneti, G. Endoscopic treatment of congenital choanal atresia. Int. J. Pediatr. Otorhinolaryngol. 2003, 67, 271–276. [Google Scholar] [CrossRef]
- Oh, M.S.; Kadom, N.; Abramowicz, S.; Todd, N.W., Jr. Pediatric unilateral isolated choanal atresia is not associated with mandibular condyle hypoplasia. Am. J. Otolaryngol. 2021, 42, 102824. [Google Scholar] [CrossRef]
- Brihaye, P.; Delpierre, I.; De Villé, A.; Johansson, A.-B.; Biarent, D.; Mansbach, A.-L. Comprehensive management of congenital choanal atresia. Int. J. Pediatr. Otorhinolaryngol. 2017, 98, 9–18. [Google Scholar] [CrossRef]
- Harris, J.; Robert, E.; Källén, B. Epidemiology of Choanal Atresia with Special Reference to the CHARGE Association. Pediatrics 1997, 99, 363–367. [Google Scholar] [CrossRef]
- Case, A.P.; Mitchell, L.E. Prevalence and patterns of choanal atresia and choanal stenosis among pregnancies in Texas, 1999-2004. Am. J. Med Genet. Part A 2011, 155, 786–791. [Google Scholar] [CrossRef]
- Ramsden, J.D.; Campisi, P.; Forte, V. Choanal Atresia and Choanal Stenosis. Otolaryngol. Clin. N. Am. 2009, 42, 339–352. [Google Scholar] [CrossRef]
- Kurosaka, H. Choanal atresia and stenosis: Development and diseases of the nasal cavity. Wiley Interdiscip. Rev. Dev. Biol. 2019, 8, e336. [Google Scholar] [CrossRef] [Green Version]
- Georgiopoulos, C.; Postler, M.; Rombaux, P.; Gudziol, V.; Abolmaali, N.; Hummel, T. Unilateral Choanal Atresia: Indications of Long-Term Olfactory Deficits and Volumetric Brain Changes Postsurgically. ORL J. Otorhinolaryngol. Relat. Spec. 2022, 84, 89–92. [Google Scholar] [CrossRef]
- Bajin, M.D.; Önay, Ö.; Günaydın, R.O.; Ünal, F.; Yücel, T.; Akyol, U.; Aydın, C. Endonasal choanal atresia repair; evaluating the surgical results of 58 cases. Turk. J. Pediatr. 2021, 63, 136–140. [Google Scholar] [CrossRef]
- Stankiewicz, J.A. The Endoscopic Repair of Choanal Atresia. Otolaryngol. Neck Surg. 1990, 103, 931–937. [Google Scholar] [CrossRef]
- Teissier, N.; Kaguelidou, F.; Couloigner, V.; François, M.; Abbeele, T.V.D. Predictive Factors for Success After Transnasal Endoscopic Treatment of Choanal Atresia. Arch. Otolaryngol. Head Neck Surg. 2008, 134, 57–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gundle, L.; Ojha, S.; Hendry, J.; Rosen, H. Stenting versus stentless repair for bilateral choanal atresia: A systematic review of the literature. Int. J. Pediatr. Otorhinolaryngol. 2021, 151, 110926. [Google Scholar] [CrossRef]
- Cedin, A.C.; Fujita, R.; Laércio, M.C.O. Endoscopic transeptal surgery for choanal atresia with a stentless folded-over-flap technique. Otolaryngol. Neck Surg. 2006, 135, 693–698. [Google Scholar] [CrossRef] [PubMed]
- Saraniti, C.; Santangelo, M.; Salvago, P. Surgical treatment of choanal atresia with transnasal endoscopic approach with stentless single side-hinged flap technique: 5 year retrospective analysis. Braz. J. Otorhinolaryngol. 2017, 83, 183–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strychowsky, J.E.; Kawai, K.; Moritz, E.; Rahbar, R.; Adil, E.A. To stent or not to stent? A meta-analysis of endonasal congenital bilateral choanal atresia repair. Laryngoscope 2016, 126, 218–227. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, O.E.; Pownell, P.; Manning, S.C. Choanal atresia: A new anatomic classification and clinical management applications. Laryngoscope 1996, 106 Pt 1, 97–101. [Google Scholar] [CrossRef]
- Debillon, T.; Zupan, V.; Ravault, N.; Magny, J.-F.; Dehan, M. Development and initial validation of the EDIN scale, a new tool for assessing prolonged pain in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 2001, 85, F36–F41. [Google Scholar] [CrossRef]
- Rosenfeld, R.M.; Shin, J.J.; Schwartz, S.R.; Coggins, R.; Gagnon, L.; Hackell, J.; Hoelting, D.; Hunter, L.L.; Kummer, A.W.; Payne, S.; et al. Clinical Practice Guideline: Otitis Media with Effusion (Update). Otolaryngol. Neck Surg. 2016, 154 (Suppl. S1), S1–S41. [Google Scholar] [CrossRef]
- Keller, J.L.; Kacker, A. Choanal atresia, CHARGE association, and congenital nasal stenosis. Otolaryngol. Clin. N. Am. 2000, 33, 1343–1351. [Google Scholar] [CrossRef]
- Yaniv, E.; Hadar, T.; Shvero, J.; Stern, Y.; Raveh, E. Endoscopic transnasal repair of choanal atresia. Int. J. Pediatr. Otorhinolaryngol. 2007, 71, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, H.; Cuestas, G.; Passali, D. A 20-year experience in microsurgical treatment of choanal atresia. Acta Otorrinolaringol. Esp. 2014, 65, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Devambez, M.; Delattre, A.; Fayoux, P. Congenital Nasal Pyriform Aperture Stenosis: Diagnosis and Management. Cleft Palate Craniofacial J. 2009, 46, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Velegrakis, S.; Mantsopoulos, K.; Iro, H.; Zenk, J. Long-term outcomes of endonasal surgery for choanal atresia: 28 years experience in an academic medical centre. Eur. Arch. Otorhinolaryngol. 2013, 270, 113–116. [Google Scholar] [CrossRef] [PubMed]
- El-Ahl, M.A.S.; El-Anwar, M.W. Stentless endoscopic transnasal repair of bilateral choanal atresia starting with resection of vomer. Int. J. Pediatr. Otorhinolaryngol. 2012, 76, 1002–1006. [Google Scholar] [CrossRef] [PubMed]
- Corrales, C.E.; Koltai, P.J. Choanal atresia: Current concepts and controversies. Curr. Opin. Otolaryngol. Head Neck Surg. 2009, 17, 466–470. [Google Scholar] [CrossRef]
- Carter, J.M.; Lawlor, C.; Guarisco, J.L. The efficacy of mitomycin and stenting in choanal atresia repair: A 20 year experience. Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 307–311. [Google Scholar] [CrossRef]
- Osguthorpe, J.D.; Singleton, G.T.; Adkins, W.Y. The Surgical Approach to Bilateral Choanal Atresia: Analysis of 14 Cases. Arch. Otolaryngol. Head Neck Surg. 1982, 108, 366–369. [Google Scholar] [CrossRef]
- Josephson, G.D.; Vickery, C.L.; Giles, W.C.; Gross, C.W. Transnasal Endoscopic Repair of Congenital Choanal Atresia: Long-term Results. Arch. Otolaryngol. Head Neck Surg. 1998, 124, 537–540. [Google Scholar] [CrossRef]
- Cumberworth, V.L.; Djazaeri, B.; Mackay, I.S. Endoscopic fenestration of choanal atresia. J. Laryngol. Otol. 1995, 109, 31–35. [Google Scholar] [CrossRef]
- Durmaz, A.; Tosun, F.; Yldrm, N.; Sahan, M.; Kvrakdal, C.; Gerek, M. Transnasal Endoscopic Repair of Choanal Atresia: Results of 13 Cases and Meta-Analysis. J. Craniofacial Surg. 2008, 19, 1270–1274. [Google Scholar] [CrossRef] [PubMed]
- Deutsch, E.; Kaufman, M.; Eilon, A. Transnasal endoscopic management of choanal atresia. Int. J. Pediatr. Otorhinolaryngol. 1997, 40, 19–26. [Google Scholar] [CrossRef]
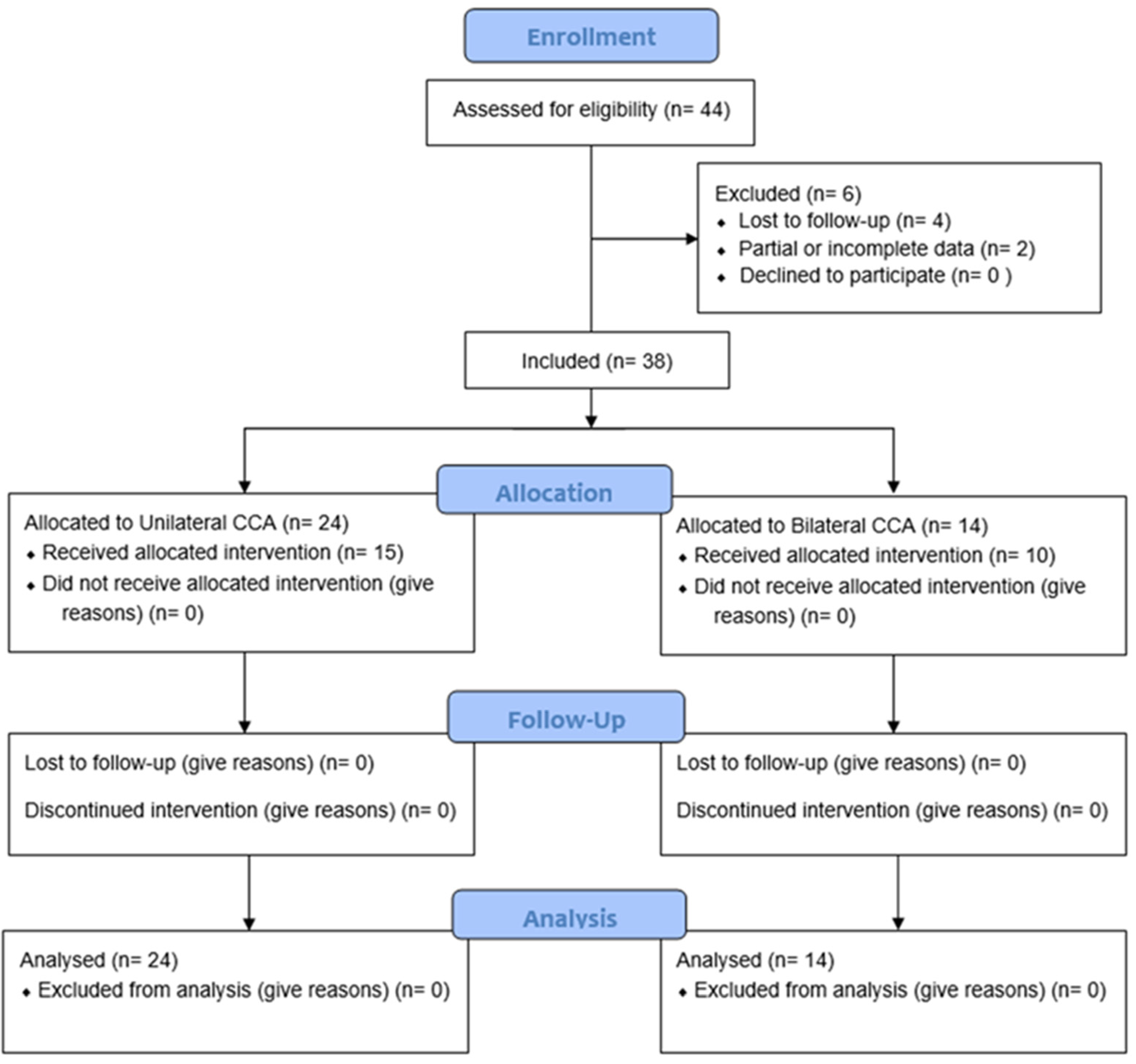
| Features | Total | Bilateral | Unilateral | p-Value |
|---|---|---|---|---|
| Total number of cases | 38 (100%) | 14 (36.84%) | 24 (63.16%) | |
| Gender | 14 M (40%)/24 F (60%) | 6 M (40%)/8 F (60%) | 8 M (40%)/16 F (60%) | - |
| Type of atresia | 8 B (12%)/30 BM (88%) | 3 B (10%)/11 BM (90%) | 5 B (13%)/19 BM (87%) | 0.50 |
| Age (days) | 7.9 ± 1.3 days | 105.5 ± 51.33 days | <0.001 | |
| Associated loco regional birth defects | 33 (100%) | 14 (40%) | 19 (60%) | 0.1 |
| Hypoplastic concha inferior | 23 (76%) | 7 (20%) | 16 (56%) | <0.001 |
| Rhinopharyngeal stenosis | 8 (20%) | 5 (16%) | 3 (4%) | 0.01 |
| Rhinopharyngeal web | 2 (4%) | 2 (4%) | - | - |
| Syndromic cases (Charge) | 5 (12%) | 5 (12%) | - | - |
| Revision surgery | 12 (8%) | 3 (4%) | 9 (4%) | - |
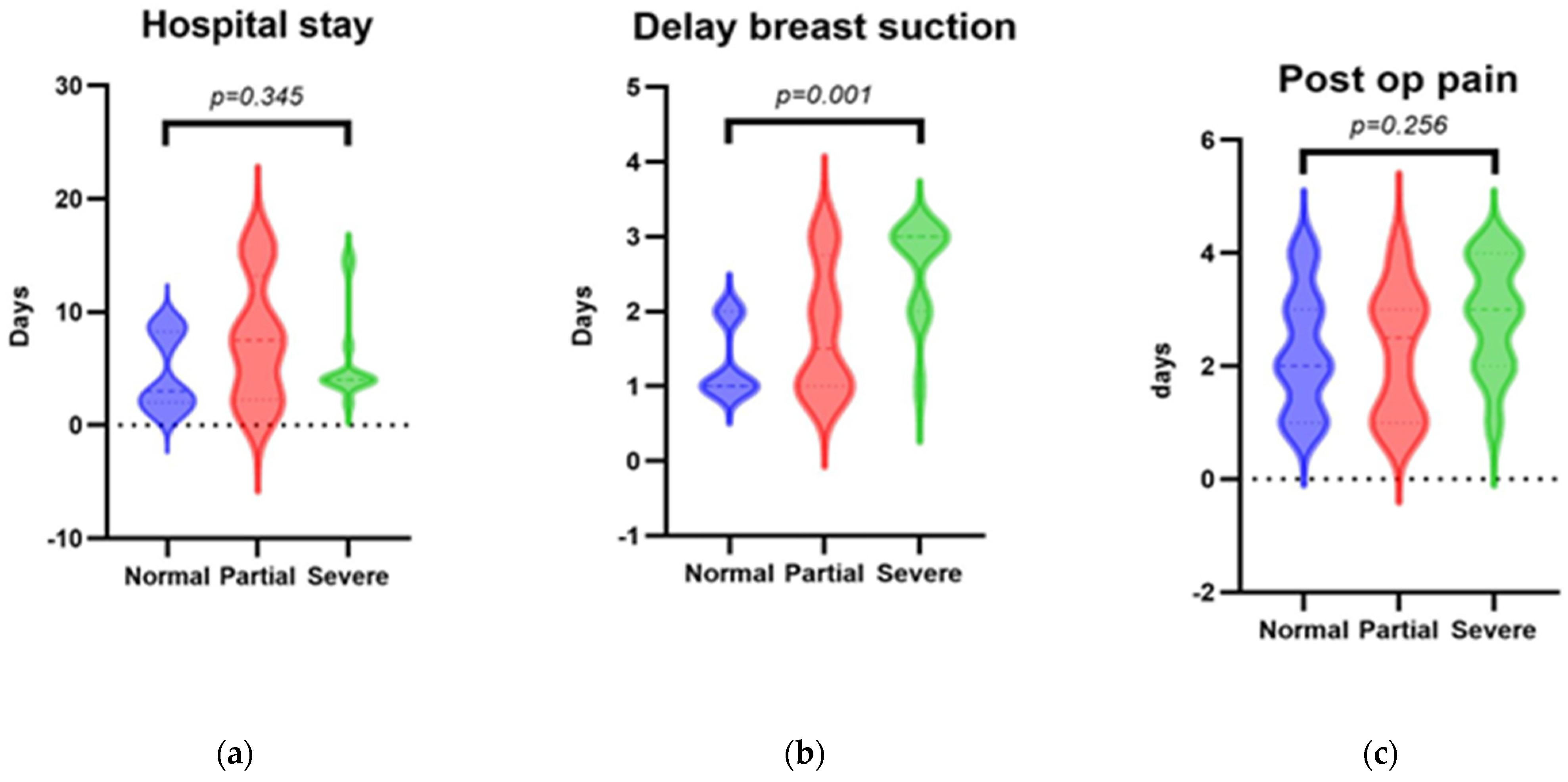
| Delay for starting Breast-suction (days) | 1.2 ± 0.49 | 1.55± 0.66 | 1 | 0.003 |
| Duration of Pain (days) | 2.2 ± 1.05 | 2.9 ± 1.13 | 1.73 ± 0.67 | 0.003 |
| Hospital stays (days) | 5.52 ± 4.09 | 9.8 ± 2.92 | 2.66 ± 1.39 | <0.001 |
| Healing postoperative | ||||
| Normal | 18 (68%) | 7 (24%) | 11 (44%) | 0.804 |
| limited scar-partial restenosis (<50%) | 8 (20%) | 4 (12%) | 4 (8%) | 0.385 |
| severe restenosis (>50%) | 12 (8%) | 3 (4%) | 9 (4%) | 0.303 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferlito, S.; Maniaci, A.; Dragonetti, A.G.; Cocuzza, S.; Lechien, J.R.; Calvo-Henríquez, C.; Maza-Solano, J.; Locatello, L.G.; Caruso, S.; Nocera, F.; et al. Endoscopic Endonasal Repair of Congenital Choanal Atresia: Predictive Factors of Surgical Stability and Healing Outcomes. Int. J. Environ. Res. Public Health 2022, 19, 9084. https://doi.org/10.3390/ijerph19159084
Ferlito S, Maniaci A, Dragonetti AG, Cocuzza S, Lechien JR, Calvo-Henríquez C, Maza-Solano J, Locatello LG, Caruso S, Nocera F, et al. Endoscopic Endonasal Repair of Congenital Choanal Atresia: Predictive Factors of Surgical Stability and Healing Outcomes. International Journal of Environmental Research and Public Health. 2022; 19(15):9084. https://doi.org/10.3390/ijerph19159084
Chicago/Turabian StyleFerlito, Salvatore, Antonino Maniaci, Alberto Giulio Dragonetti, Salvatore Cocuzza, Jerome Rene Lechien, Christian Calvo-Henríquez, Juan Maza-Solano, Luca Giovanni Locatello, Sebastiano Caruso, Francesco Nocera, and et al. 2022. "Endoscopic Endonasal Repair of Congenital Choanal Atresia: Predictive Factors of Surgical Stability and Healing Outcomes" International Journal of Environmental Research and Public Health 19, no. 15: 9084. https://doi.org/10.3390/ijerph19159084
APA StyleFerlito, S., Maniaci, A., Dragonetti, A. G., Cocuzza, S., Lechien, J. R., Calvo-Henríquez, C., Maza-Solano, J., Locatello, L. G., Caruso, S., Nocera, F., Achena, A., Mevio, N., Mantini, G., Ormellese, G., Placentino, A., & La Mantia, I. (2022). Endoscopic Endonasal Repair of Congenital Choanal Atresia: Predictive Factors of Surgical Stability and Healing Outcomes. International Journal of Environmental Research and Public Health, 19(15), 9084. https://doi.org/10.3390/ijerph19159084













