The Moderating Effect of Contact with Children on the Relationship between Adverse Childhood Experiences and Depression in Adulthood among a Chinese Adult Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.2. Variables
2.2.1. Dependent Variable
2.2.2. Independent and Control Variables
2.2.3. Moderating Variable
2.3. Statistical Analysis
3. Results
3.1. Differences in Depression among People with Different Characteristics
3.2. The Effects of ACDs on Depression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
Appendix A
References
- Beck, A.T. Depression: Clinical, Experimental and Theoretical Aspects; Hoeber: New York, NY, USA, 1967. [Google Scholar]
- Abbott, M.; Slack, K.S. Exploring the relationship between childhood adversity and adult depression: A risk versus strengths-oriented approach. Child Abus. Negl. 2021, 120, 105207. [Google Scholar] [CrossRef] [PubMed]
- Masiano, S.P.; Yu, X.; Tembo, T.; Wetzel, E.; Mphande, M.; Khama, I.; Kim, M.H. The relationship between adverse childhood experiences and common mental disorders among pregnant women living with HIV in Malawi. J. Affect. Disord. 2022, 312, 159–168. [Google Scholar] [CrossRef]
- Chen, H.; Fan, Q.; Nicholas, S.; Maitland, E. The long arm of childhood: The prolonged influence of adverse childhood experiences on depression during middle and old age in China. J. Health Psychol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Kendler, K.S.; Gardner, C.O.; Prescott, C.A. Toward a comprehensive developmental model for major depression in men. Am. J. Psychiatry 2006, 163, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Maercker, A.; Michael, T.; Fehm, L.; Becker, E.S.; Margraf, J. Age of traumatisation as a predictor of post-traumatic stress disorder or major depression in young women. Br. J. Psychiatry 2004, 184, 482–487. [Google Scholar] [CrossRef]
- Widom, C.S.; DuMont, K.; Czaja, S.J. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch. Gen. Psychiatry 2007, 64, 49–56. [Google Scholar] [CrossRef]
- Werner, E.E. What can We Learn about Resilience from Large-scale Longitudinal Studies? In Handbook of Resilience in Children; Springer: Boston, MA, USA, 2013; pp. 87–102. [Google Scholar]
- Chapman, D.P.; Whitfield, C.L.; Felitti, V.J.; Dube, S.R.; Edwards, V.J.; Anda, R.F. Adverse childhood experiences and the risk of depressive disorders in adulthood. J. Affect. Disord. 2004, 82, 217–225. [Google Scholar] [CrossRef]
- De Venter, M.; Demyttenaere, K.; Bruffaerts, R. The relationship between adverse childhood experiences and mental health in adulthood: A systematic literature review. Tijdschr. Voor Psychiatr. 2013, 55, 259–268. [Google Scholar]
- Li, M.; D’Arcy, C.; Meng, X. Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: Systematic review, meta-analysis, and proportional attributable fractions. Psychol. Med. 2016, 46, 717–730. [Google Scholar] [CrossRef]
- Lindert, J.; von Ehrenstein, O.S.; Grashow, R.; Gal, G.; Braehler, E.; Weisskopf, M.G. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: Systematic review and meta-analysis. Int. J. Public Health 2014, 59, 359–372. [Google Scholar] [CrossRef]
- Sahle, B.W.; Reavley, N.J.; Li, W.; Morgan, A.J.; Yap, M.B.H.; Reupert, A.; Jorm, A.F. The association between adverse childhood experiences and common mental disorders and suicidality: An umbrella review of systematic reviews and meta-analyses. Eur. Child Adolesc. Psychiatry 2021. [Google Scholar] [CrossRef] [PubMed]
- Mancini, C.; Van Ameringen, M.; MacMillan, H. Relationship of childhood sexual and physical abuse to anxiety disorders. J. Nerv. Ment. Dis. 1995, 183, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Alloy, L.B.; Abramson, L.Y.; Francis, E.L. Do negative cognitive styles confer vulnerability to depression? Curr. Dir. Psychol. Sci. 1999, 8, 128–132. [Google Scholar] [CrossRef]
- Heim, C.; Newport, D.J.; Mletzko, T.; Miller, A.H.; Nemeroff, C.B. The link between childhood trauma and depression: Insights from HPA axis studies in humans. Psychoneuroendocrinology 2008, 33, 693–710. [Google Scholar] [CrossRef] [PubMed]
- Sachs-Ericsson, N.; Joiner, T.E.; Cougle, J.R.; Stanley, I.H.; Sheffler, J.L. Combat exposure in early adulthood interacts with recent stressors to predict PTSD in aging male veterans. Gerontologist 2016, 56, 82–91. [Google Scholar] [CrossRef]
- Sachs-Ericsson, N.; Verona, E.; Joiner, T.; Preacher, K.J. Parental verbal abuse and the mediating role of self-criticism in adult internalizing disorders. J. Affect. Disord. 2006, 93, 71–78. [Google Scholar] [CrossRef]
- Jiang, W.; Ji, M.; Chi, X.; Sun, X. Relationship between adverse childhood experiences and mental health in Chinese adolescents: Differences among girls and boys. Children 2022, 9, 689. [Google Scholar] [CrossRef]
- LeMasters, K.; Bates, L.M.; Chung, E.O.; Gallis, J.A.; Hagaman, A.; Scherer, E.; Maselko, J. Adverse childhood experiences and depression among women in rural Pakistan. BMC Public Health 2021, 21, 400. [Google Scholar] [CrossRef]
- Cavanaugh, C.; Nelson, T. A national study of the influence of adverse childhood experiences on depression among Black adults in the United States. J. Affect. Disord. 2022, 311, 523–529. [Google Scholar] [CrossRef]
- Wang, D.; Jiang, Q.; Yang, Z.; Choi, J.K. The longitudinal influences of adverse childhood experiences and positive childhood experiences at family, school, and neighborhood on adolescent depression and anxiety. J. Affect. Disord. 2021, 292, 542–551. [Google Scholar] [CrossRef]
- McKeen, H.; Hook, M.; Podduturi, P.; Beitzell, E.; Jones, A.; Liss, M. Mindfulness as a mediator and moderator in the relationship between adverse childhood experiences and depression. Curr. Psychol. 2021, 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Lee, H.; Park, A. Patterns of adverse childhood experiences and depressive symptoms: Self-esteem as a mediating mechanism. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Poole, J.C.; Dobson, K.S.; Pusch, D. Childhood adversity and adult depression: The protective role of psychological resilience. Child Abus. Negl. 2017, 64, 89–100. [Google Scholar] [CrossRef]
- Kelifa, M.O.; Yang, Y.; Herbert, C.; He, Q.; Wang, P. Psychological resilience and current stressful events as potential mediators between adverse childhood experiences and depression among college students in Eritrea. Child Abus. Negl. 2020, 106, 104480. [Google Scholar] [CrossRef] [PubMed]
- Cloitre, M.; Khan, C.; Mackintosh, M.A.; Garvert, D.W.; Henn-Haase, C.M.; Falvey, E.C.; Saito, J. Emotion regulation mediates the relationship between ACES and physical and mental health. Psychol. Trauma Theory Res. Pract. Policy 2019, 11, 82. [Google Scholar] [CrossRef] [PubMed]
- Bravo, L.G.; Nagy, G.A.; Stafford, A.M.; McCabe, B.E.; Gonzalez-Guarda, R.M. Adverse childhood experiences and depressive symptoms among young adult Hispanic immigrants: Moderating and mediating effects of distinct facets of acculturation stress. Issues Ment. Health Nurs. 2022, 43, 209–219. [Google Scholar] [CrossRef]
- National Bureau of Statistics of China. 2021 Migrant Workers Monitoring Survey Report in2021. 2022. Available online: http://www.stats.gov.cn/xxgk/sjfb/zxfb2020/202204/t20220429_1830139.html (accessed on 21 May 2022).
- Romanowski, M.H. Meeting the unique needs of the children of migrant farm workers. Clear. House A J. Educ. Strateg. Issues Ideas 2003, 77, 27–33. [Google Scholar] [CrossRef]
- Chan, A. Paying the Price for Economic Development: The Children of Migrant Workers in China; China Labour Bulletin: Hongkong, China, 2009. [Google Scholar]
- Ministry of Civil Affairs of China. Statistical Communique of the People’s Republic of China on the Development of Civil Affairs in 1987. 1988. Available online: http://www.mca.gov.cn/article/sj/tjgb/200801/200801150094339.shtml (accessed on 21 May 2022).
- Ministry of Civil Affairs of China. Statistical Communique of the People’s Republic of China on the Development of Civil Affairs in 2020. 2021. Available online: http://images3.mca.gov.cn/www2017/file/202109/1631265147970.pdf (accessed on 21 May 2022).
- Wong, F.K.D.; Chang, Y.L.; He, X.S. Correlates of psychological wellbeing of children of migrant workers in Shanghai, China. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 815–824. [Google Scholar] [CrossRef]
- Dennis, C.H.; Clohessy, D.S.; Stone, A.L.; Darnall, B.D.; Wilson, A.C. Adverse childhood experiences in mothers with chronic pain and intergenerational impact on children. J. Pain 2019, 20, 1209–1217. [Google Scholar] [CrossRef]
- Narayan, A.J.; Lieberman, A.F.; Masten, A.S. Intergenerational transmission and prevention of adverse childhood experiences (ACEs). Clin. Psychol. Rev. 2021, 85, 101997. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Dube, S.R.; Felitti, V.J.; Dong, M.; Giles, W.H.; Anda, R.F. The impact of adverse childhood experiences on health problems: Evidence from four birth cohorts dating back to 1900. Prev. Med. 2003, 37, 268–277. [Google Scholar] [CrossRef]
- Chang, X.; Jiang, X.; Mkandarwire, T.; Shen, M.; Seedat, S. Associations between adverse childhood experiences and health outcomes in adults aged 18–59 years. PLoS ONE 2019, 14, e0211850. [Google Scholar] [CrossRef]
- Von Cheong, E.; Sinnott, C.; Dahly, D.; Kearney, P.M. Adverse childhood experiences (ACEs) and later-life depression: Perceived social support as a potential protective factor. BMJ Open 2017, 7, e013228. [Google Scholar] [CrossRef] [PubMed]
- Waite, R.; Shewokis, P.A. Childhood Trauma and Adult Self-Reported Depression. ABNF J. 2012, 23, 8–14. [Google Scholar]
- Racine, N.; Devereaux, C.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Adverse childhood experiences and maternal anxiety and depression: A meta-analysis. BMC Psychiatry 2021, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Zhao, Y. The Relationship between Adverse Family Experiences during Childhood and Self-rated Health Outcome in Adulthood. Social Work in Public Health 2022, 37, 342–355. [Google Scholar] [CrossRef] [PubMed]
- Asmundson, G.G.; Afifi, T.O. Adverse Childhood Experiences: Using Evidence to Advance Research, Practice, Policy, and Prevention; Academic Press: Cambridge, MA, USA, 2019. [Google Scholar]
- Rosenbaum, S. ACEs and child health policy: The enduring case for EPSDT. Acad. Pediatrics 2017, 17, S34–S35. [Google Scholar] [CrossRef][Green Version]
- Srivastav, A.; Spencer, M.; Thrasher, J.F.; Strompolis, M.; Crouch, E.; Davis, R.E. Addressing health and well-being through state policy: Understanding barriers and opportunities for policy-making to prevent adverse childhood experiences (ACEs) in South Carolina. Am. J. Health Promot. 2020, 34, 189–197. [Google Scholar] [CrossRef]
| Variables | Frequency | Percent (%) | |
|---|---|---|---|
| Sex | Male | 5501 | 47.57 |
| Female | 6063 | 52.43 | |
| Ethnic | Minority ethnic groups | 913 | 7.90 |
| Han ethnic groups | 10,651 | 92.10 | |
| Hukou type | Rural | 10,709 | 92.61 |
| Urban | 855 | 7.39 | |
| Education level | Elementary and below | 6672 | 57.70 |
| Middle school | 3257 | 28.16 | |
| High school | 1312 | 11.35 | |
| College or above | 323 | 2.79 | |
| Religious belief | No religion | 10,453 | 90.39 |
| Religious affiliation | 1111 | 9.61 | |
| Political status | Non-party member | 10,402 | 89.95 |
| Party member | 1162 | 10.05 | |
| Categories | Depression Scores | ||
|---|---|---|---|
| (x ± s) | Test | ||
| Sex # | Male | 16.604 ± 5.823 | −16.504 *** |
| Female | 18.521 ± 6.593 | ||
| Hukou type # | Rural | 17.750 ± 6.360 | 8.520 *** |
| Urban | 15.844 ± 5.368 | ||
| Education level + | Elementary and below | 18.593 ± 6.632 | 148.77 *** |
| Middle school | 16.667 ± 5.733 | ||
| High school | 15.675 ± 5.259 | ||
| College or above | 14.628 ± 4.583 | ||
| Ethnic # | Minority ethnic groups | 17.717 ± 6.150 | 0.542 † |
| Han ethnic groups | 17.599 ± 6.325 | ||
| Religious belief # | No religion | 17.644 ± 6.313 | −1.832 |
| Religious affiliation | 17.279 ± 6.286 | ||
| Political status # | Non-party member | 17.633 ± 6.324 | −1.222 |
| Party member | 17.394 ± 6.197 | ||
| Male | Female | All | |||||
|---|---|---|---|---|---|---|---|
| (x ± s) | t-Test | (x ± s) | t-Test | (x ± s) | t-Test | ||
| Physical abuse | Yes | 17.230 ± 6.122 | −5.883 *** | 19.656 ± 6.763 | −7.516 *** | 18.266 ± 6.514 | −7.188 *** |
| No | 16.265 ± 5.626 | 18.168 ± 6.500 | 17.339 ± 6.206 | ||||
| Emotional neglect | Yes | 17.088 ± 6.057 | −3.171 ** | 19.044 ± 6.793 | −3.393 *** | 18.164 ± 6.543 | −5.032 *** |
| No | 16.476 ± 5.753 | 18.363 ± 6.524 | 17.452 ± 6.236 | ||||
| Parental divorce | Yes | 16.130 ± 5.268 | 0.390 | 20.531 ± 7.255 | −1.729 † | 18.691 ± 6.806 | −1.275 |
| No | 16.606 ± 5.825 | 18.510 ± 6.588 | 17.604 ± 6.309 | ||||
| Parental death | Yes | 17.581 ± 6.449 | −4.373 *** | 19.415 ± 7.036 | −3.542 *** | 18.506 ± 6.810 | −5.239 *** |
| No | 16.483 ± 5.730 | 18.420 ± 6.534 | 17.504 ± 6.242 | ||||
| Sibling death | Yes | 17.338 ± 6.162 | −5.025 *** | 19.279 ± 6.930 | −4.835 *** | 18.360 ± 6.647 | −6.892 *** |
| No | 16.393 ± 5.705 | 18.301 ± 6.476 | 17.392 ± 6.194 | ||||
| Parental drug abuse | Yes | 17.714 ± 7.376 | −0.876 | 21.700 ± 9.129 | −1.526 | 19.000 ± 8.053 | −1.229 |
| No | 16.599 ± 5.816 | 18.516 ± 6.588 | 17.605 ± 6.306 | ||||
| Parental alcoholism | Yes | 17.373 ± 6.348 | −3.051 ** | 18.734 ± 6.495 | −0.683 | 18.002 ± 6.449 | −1.950 † |
| No | 16.529 ± 5.765 | 18.505 ± 6.600 | 17.576 ± 6.299 | ||||
| Parental crime | Yes | 20.304 ± 6.574 | −3.057 ** | 19.000 ± 6.656 | −0.272 | 19.811 ± 6.544 | −2.126 * |
| No | 16.588 ± 5.815 | 18.520 ± 6.593 | 17.602 ± 6.310 | ||||
| Parental illness/disability | Yes | 18.233 ± 6.693 | −10.413 *** | 20.356 ± 6.987 | −11.271 *** | 19.376 ± 6.933 | −15.397 *** |
| No | 16.201 ± 5.514 | 18.035 ± 6.398 | 17.156 ± 6.060 | ||||
| Parental depression | Yes | 18.808 ± 6.647 | −14.486 *** | 21.238 ± 5.910 | −17.427 *** | 20.125 ± 7.074 | −22.737 *** |
| No | 16.038 ± 5.451 | 17.757 ± 6.191 | 16.931 ± 5.910 | ||||
| Experience of starvation | Yes | 17.061 ± 5.999 | −9.069 *** | 19.329 ± 6.818 | −12.778 *** | 18.192 ± 6.520 | −14.235 *** |
| No | 15.512 ± 5.222 | 17.110 ± 5.923 | 16.433 ± 5.691 | ||||
| Experience of violence | Yes | 18.401 ± 6.316 | −6.661 *** | 20.568 ± 7.158 | −7.842 *** | 19.643 ± 6.891 | −10.705 *** |
| No | 16.453 ± 5.755 | 18.308 ± 6.495 | 17.417 ± 6.220 | ||||
| Being bullied by a schoolmate | Yes | 18.497 ± 6.721 | −9.906 *** | 20.067 ± 7.014 | −6.626 *** | 19.239 ± 6.903 | −10.708 *** |
| No | 16.290 ± 5.600 | 18.319 ± 6.509 | 17.369 ± 6.184 | ||||
| Urban Hukou | Rural Hukou | ||||
|---|---|---|---|---|---|
| (x ± s) | t-Test | (x ± s) | t-Test | ||
| Physical abuse | Yes | 16.618 ± 5.533 | −2.851 ** | 18.408 ± 6.573 | −6.849 *** |
| No | 15.493 ± 5.259 | 17.482 ± 6.251 | |||
| Emotional neglect | Yes | 16.521 ± 5.917 | −2.127 * | 18.313 ± 6.578 | −4.850 *** |
| No | 15.620 ± 5.159 | 17.592 ± 6.289 | |||
| Parental divorce | Yes | 17.750 ± 9.287 | −0.711 | 18.765 ± 6.692 | −1.143 |
| No | 15.835 ± 5.351 | 17.745 ± 6.358 | |||
| Parental death | Yes | 15.625 ± 5.127 | 0.362 | 18.687 ± 6.864 | −5.278 *** |
| No | 15.864 ± 5.393 | 17.638 ± 6.288 | |||
| Sibling death | Yes | 16.339 ± 5.691 | −1.362 | 18.506 ± 6.688 | −6.654 *** |
| No | 15.718 ± 5.280 | 17.529 ± 6.244 | |||
| Parental drug abuse | Yes | 18.250 ± 5.560 | −0.898 | 19.111 ± 8.436 | −1.114 |
| No | 15.833 ± 5.368 | 17.632 ± 6.276 | |||
| Parental alcoholism | Yes | 17.000 ± 5.952 | −1.747 † | 18.075 ± 6.481 | −1.545 |
| No | 15.756 ± 5.315 | 17.722 ± 6.349 | |||
| Parental crime | Yes | 18.000 ± 5.627 | −1.067 | 20.233 ± 6.755 | −2.142 * |
| No | 15.827 ± 5.366 | 17.743 ± 6.357 | |||
| Parental illness/disability | Yes | 16.612 ± 6.233 | −1.698 † | 19.525 ± 6.938 | −15.006 *** |
| No | 15.718 ± 5.206 | 17.280 ± 6.113 | |||
| Parental depression | Yes | 17.469 ± 6.410 | −3.475 *** | 20.253 ± 7.080 | −22.023 *** |
| No | 15.597 ± 5.152 | 17.050 ± 5.958 | |||
| Experience of starvation | Yes | 16.442 ± 5.870 | −3.087 ** | 18.289 ± 6.540 | −13.004 *** |
| No | 15.312 ± 4.822 | 16.582 ± 5.781 | |||
| Experience of violence | Yes | 18.446 ± 5.707 | −3.781 *** | 19.714 ± 6.952 | −9.974 *** |
| No | 15.662 ± 5.300 | 17.560 ± 6.268 | |||
| Be bullied by schoolmate | Yes | 15.630 ± 5.206 | −3.118 ** | 19.384 ± 6.934 | −10.266 *** |
| No | 17.358 ± 6.221 | 17.508 ± 6.235 | |||
| Variables | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Sex (Ref. = Male) | 1.674 *** | 1.841 *** | 1.827 *** |
| (0.123) | (0.120) | (0.120) | |
| Ethnic (Ref. = Minority groups) | −0.215 | −0.578 | −0.592 |
| (0.215) | (0.222) | (0.222) | |
| Hukou type (Ref. = Rural Hukou) | −0.898 *** | −0.255 * | −0.273 ** |
| (0.228) | (0.208) | (0.208) | |
| Age | 0.038 *** | 0.033 *** | 0.029 *** |
| (0.006) | (0.006) | (0.006) | |
| Religious belief (Ref. = No religion) | −0.391 * | −0.452 * | −0.460 * |
| (0.197) | (0.190) | (0.190) | |
| Political status (Ref. = Non-party member) | −0.766 *** | −0.757 *** | −0.726 *** |
| (0.198) | (0.91) | (0.191) | |
| Education level (Ref. = Elementary and below) | |||
| Middle school | −1.317 *** | −0.965 *** | −0.944 *** |
| (0.140) | (0.137) | (0.137) | |
| High school | −2.133 *** | −1.701 *** | −1.664 *** |
| (0.196) | (0.190) | (0.191) | |
| College or above | −2.832 *** | −2.474 *** | −2.423 *** |
| (0.366) | (0.356) | (0.356) | |
| Physical abuse (Ref. = No) | 0.565 *** | 0.386 | |
| (0.127) | (0.352) | ||
| Emotional neglect (Ref. = No) | 0.430 *** | 0.224 | |
| (0.134) | (0.369) | ||
| Parental divorce (Ref. = No) | 0.051 | 3.125 † | |
| (0.804) | (1.826) | ||
| Parental death (Ref. = No) | −0.023 | 0.847 † | |
| (0.184) | (0.495) | ||
| Sibling death (Ref. = No) | 0.406 ** | −0.091 | |
| (0.134) | (0.371) | ||
| Parental drug abuse (Ref. = No) | 0.505 | 4.493 * | |
| (1.077) | (2.153) | ||
| Parental alcoholism (Ref. = No) | 0.128 | 0.607 | |
| (0.207) | (0.573) | ||
| Parental crime (Ref. = No) | 0.591 | −0.682 | |
| (0.985) | (2.845) | ||
| Parental illness/disability (Ref. = No) | 1.237 *** | 1.497 *** | |
| (0.141) | (0.394) | ||
| Parental depression (Ref. = No) | 2.168 *** | 2.615 *** | |
| (0.134) | (0.394) | ||
| Experience of starvation (Ref. = No) | 0.958 *** | 1.622 *** | |
| (0.123) | (0.333) | ||
| Experience of violence (Ref. = No) | 0.991 *** | 1.368 ** | |
| (0.204) | (0.549) | ||
| Be bullied by schoolmate (Ref. = No) | 1.230 *** | 1.542 *** | |
| (0.170) | (0.477) | ||
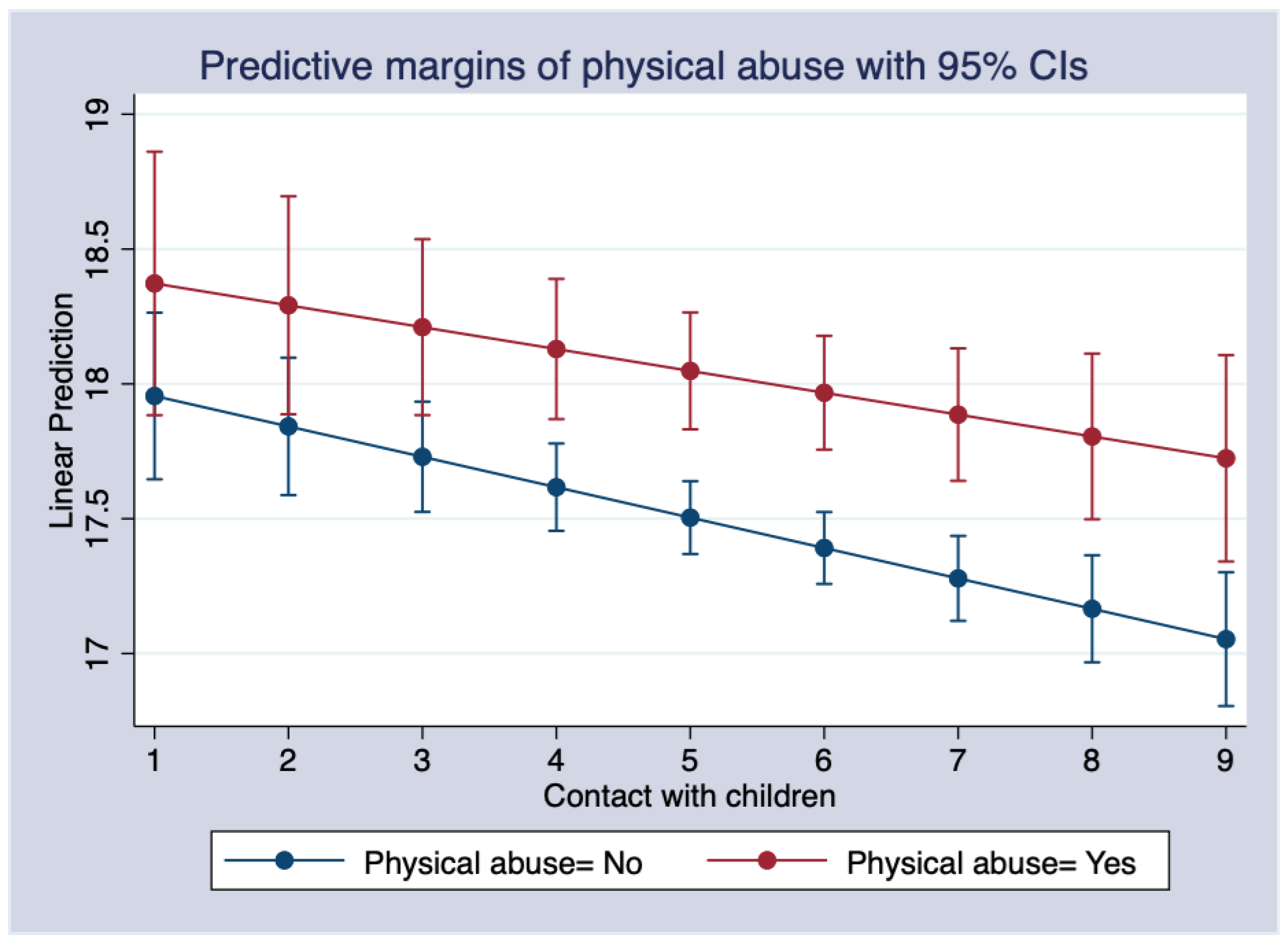
| Physical abuse × Contact with children | −1.862 ** | ||
| (0.709) | |||
| Emotional neglect × Contact with children | −0.035 | ||
| (0.062) | |||
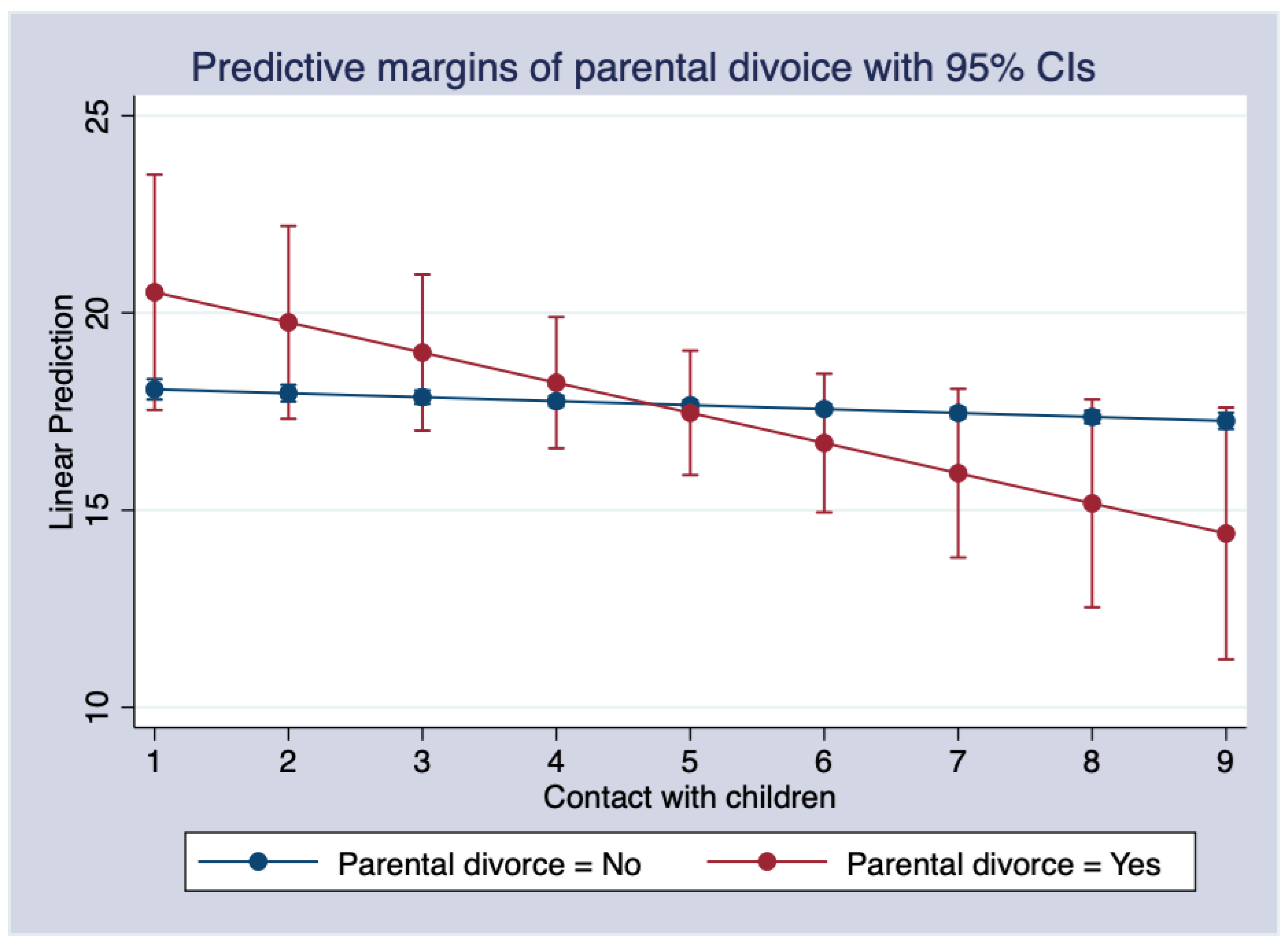
| Parental divorce × Contact with children | 0.664 † | ||
| (0.340) | |||
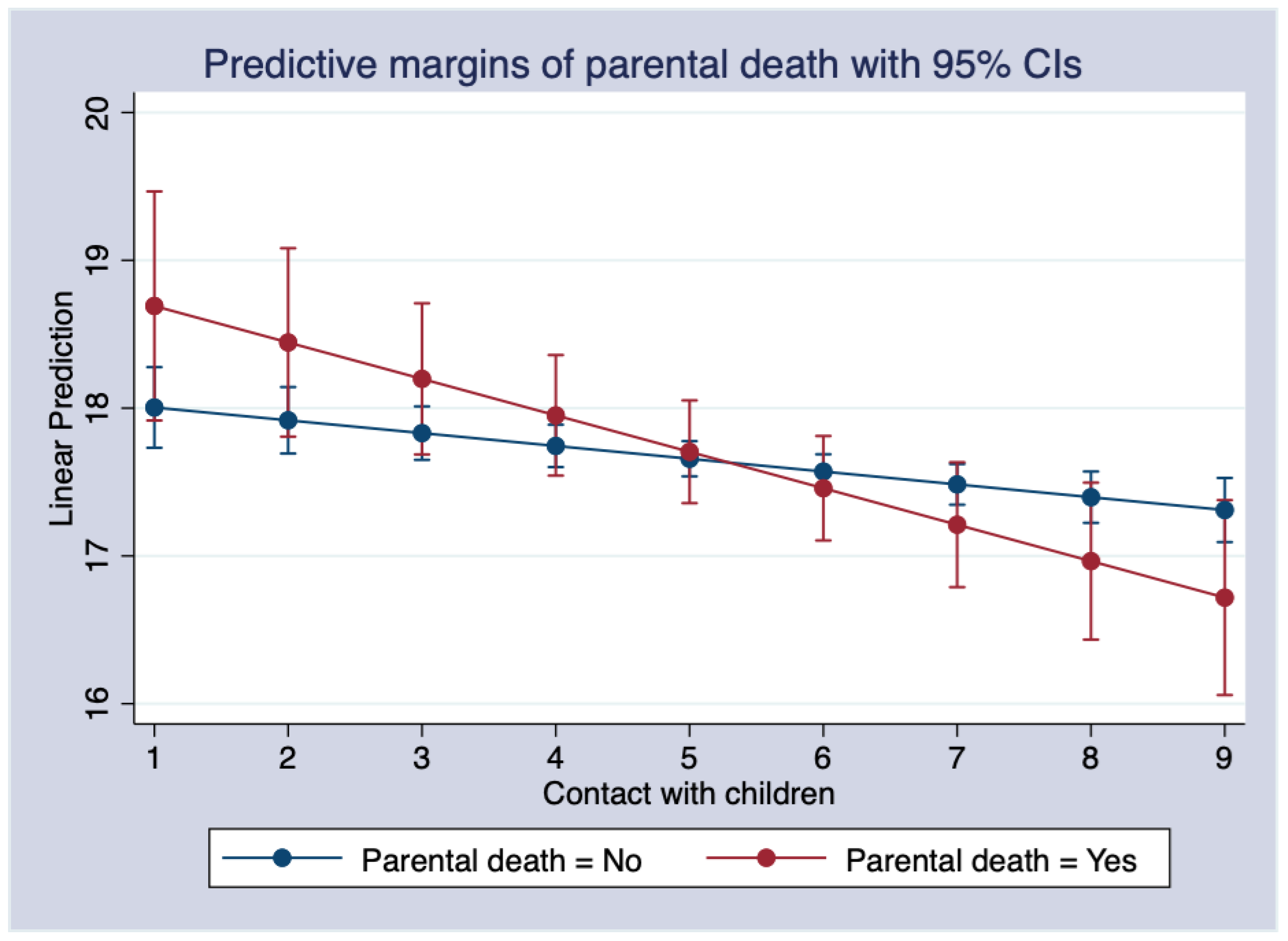
| Parental death × Contact with children | 0.160 † | ||
| (0.084) | |||
| Sibling death × Contact with children | −0.089 | ||
| (0.062) | |||
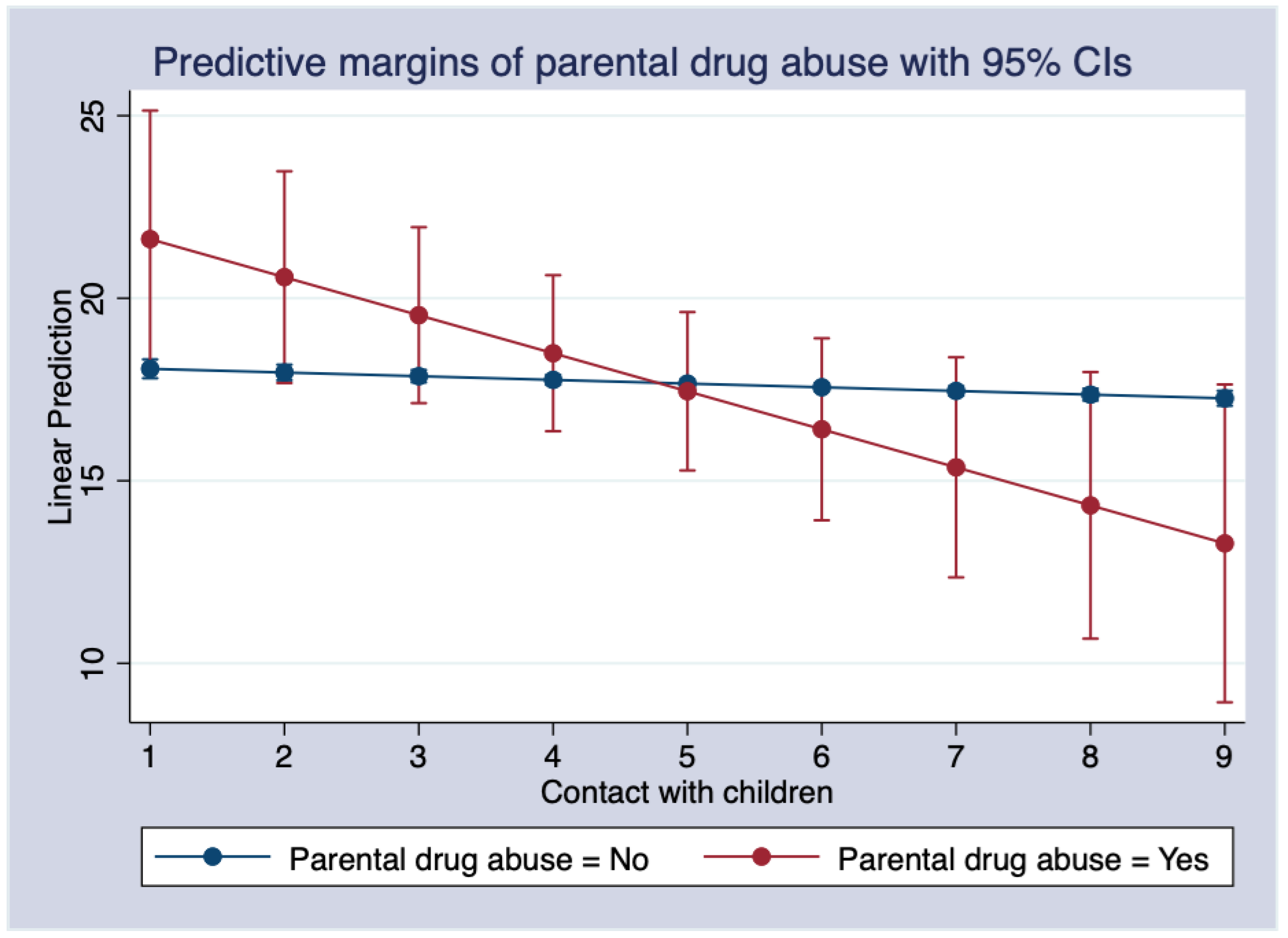
| Parental drug abuse × Contact with children | 0.941 * | ||
| (0.423) | |||
| Parental alcoholism × Contact with children | 0.089 | ||
| (0.096) | |||
| Parental crime × Contact with children | −0.227 | ||
| (0.454) | |||
| Parental illness/disability × Contact with children | 0.045 | ||
| (0.065) | |||
| Parental depression × Contact with children | 0.081 | ||
| (0.065) | |||
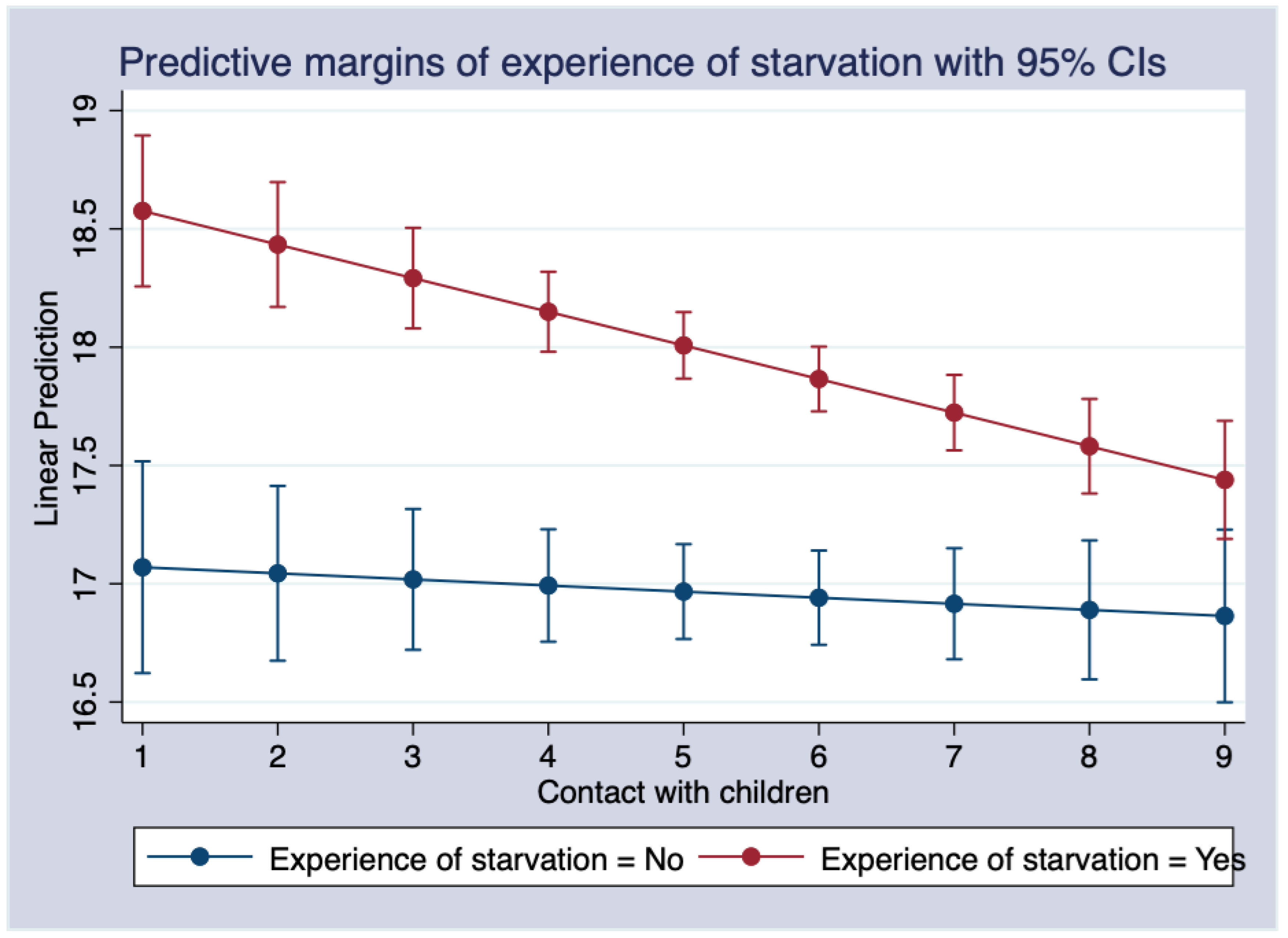
| Experience of starvation × Contact with children | 0.116 * | ||
| (0.055) | |||
| Experience of violence × Contact with children | 0.065 | ||
| (0.092) | |||
| Being bullied by schoolmate × Contact with children | 0.057 | ||
| (0.079) | |||
| Constant | 15.604 *** | 13.746 *** | 13.908 *** |
| (0.443) | (0.439) | (0.537) | |
| R2 | 0.055 | 0.116 | 0.120 |
| F-value | 74.45 *** | 68.89 *** | 43.45 *** |
| Df | 9 | 22 | 36 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Y.; Wang, D.; Du, F. The Moderating Effect of Contact with Children on the Relationship between Adverse Childhood Experiences and Depression in Adulthood among a Chinese Adult Population. Int. J. Environ. Res. Public Health 2022, 19, 8901. https://doi.org/10.3390/ijerph19158901
Zhao Y, Wang D, Du F. The Moderating Effect of Contact with Children on the Relationship between Adverse Childhood Experiences and Depression in Adulthood among a Chinese Adult Population. International Journal of Environmental Research and Public Health. 2022; 19(15):8901. https://doi.org/10.3390/ijerph19158901
Chicago/Turabian StyleZhao, Yufeng, Dianxi Wang, and Feilun Du. 2022. "The Moderating Effect of Contact with Children on the Relationship between Adverse Childhood Experiences and Depression in Adulthood among a Chinese Adult Population" International Journal of Environmental Research and Public Health 19, no. 15: 8901. https://doi.org/10.3390/ijerph19158901
APA StyleZhao, Y., Wang, D., & Du, F. (2022). The Moderating Effect of Contact with Children on the Relationship between Adverse Childhood Experiences and Depression in Adulthood among a Chinese Adult Population. International Journal of Environmental Research and Public Health, 19(15), 8901. https://doi.org/10.3390/ijerph19158901





