Eating Advice for People Who Wear Dentures: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Population, Context and Concept (PCC)
2.2. Types of Information
2.3. Search Strategy
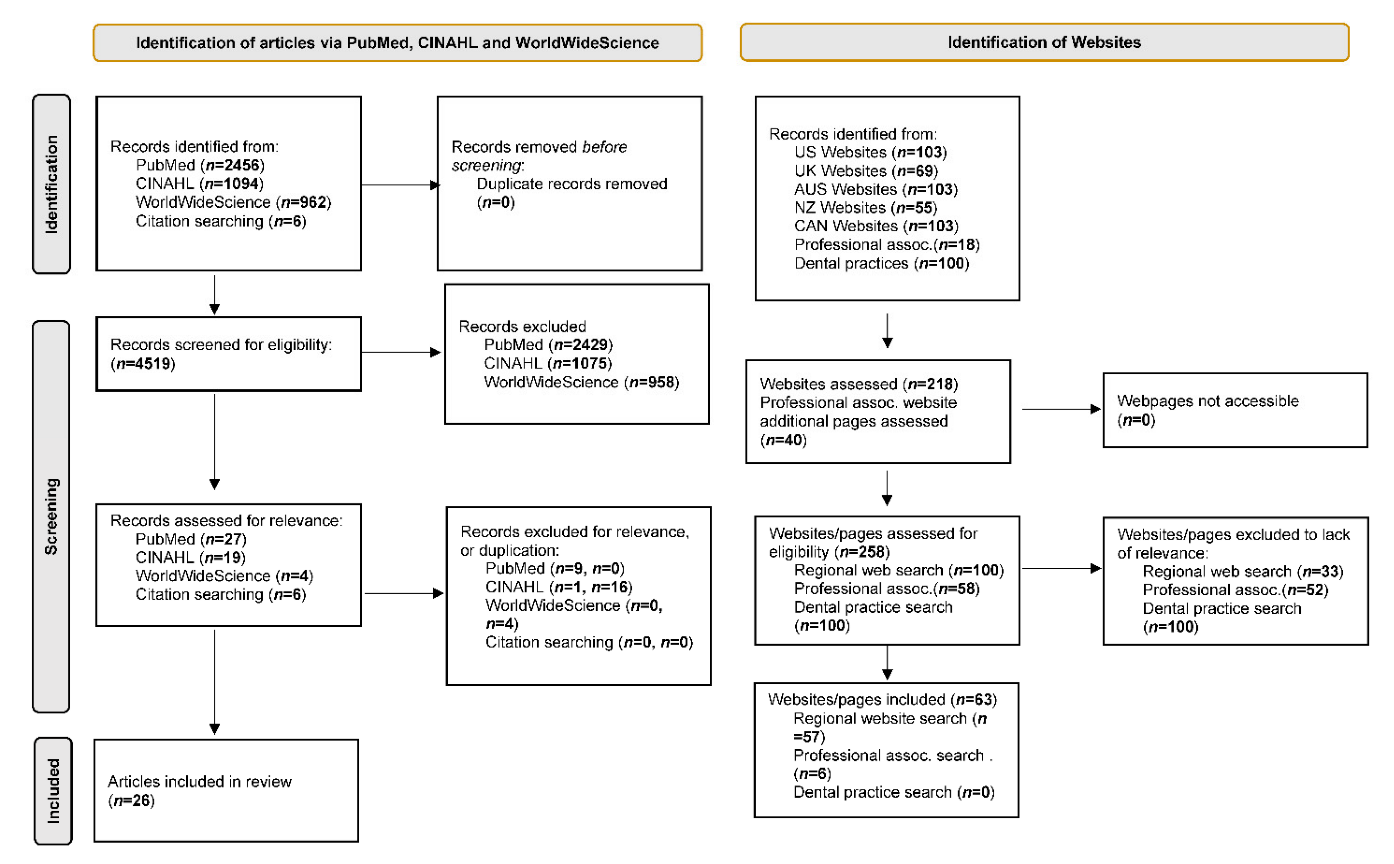
2.4. Screening
2.5. Extracting and Charting Results
3. Results
3.1. Search Results
3.2. Findings from Peer Review Literature
3.3. Findings from Google Searches
4. Discussion
4.1. Limitations of the Content of Available Eating Advice
4.2. Limitations of the Scoping Review
4.3. Future Research
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Reference | Author | Year | Country | Article Type | Study Type | Dietary Info | Study Duration | Study Population | Objective | Outcome Measures | Key Content (If Applicable) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| [19] | Moynihan PJ et al. | 2012 | UK | Primary Manuscript | Two cohort prospective parallel dietary intervention study | 2× one-to-one customised dietary interventions delivered by a CAN and the provision of an individually tailored nutrition education package to take home (Bradbury J et al. 2006. Journal of Dental Research. 85:463–8) | 6 months | N = 54 patients wearing IODs or CDs aged 40–80 years | To identify and describe dietary strategies appropriate for dental patients who receive dental care that includes the placement and maintenance of dental prostheses. | Chewing satisfaction questionnaires, dietary diary, serum antioxidant and vitamins | - |
| [22] | Prakash N et al. | 2012 | India | Primary Manuscript | Single-arm, non-controlled pilot study | Participants were explained the importance of a well-balanced diet and the benefits of regular nutritional status assessment | 6 and 9 months | N = 94 edentulous patients aged ≥ 50–80 years in need of complete dentures for the 1st time | To evaluate the effect of edentulousness and prosthetic treatment on the nutritional status of the elderly population | MNA questionnaire, anthropometric measurements, dietic assessment | - |
| [27] | Shigli K & Hebbal M. | 2012 | India | Primary Manuscript | Pilot non-randomised study | N/A | 1 month | N = 35 patients undergoing complete denture procedure | To assess these changes before and 1 month after placement of complete dentures in a dental hospital in Indore, Madhya Pradesh, India. | 10-item closed-ended questionnaire | Dietary guidance, based on the assessment of the edentulous patient’s nutrition history and diet, should be an integral part of comprehensive prosthodontic treatment. Nutrition support will improve the tolerance of the oral mucosa to new dentures and prevent rejection of dentures. As denture fabrication requires a series of appointments, dietary analysis and counselling can easily be incorporated into an edentulous patient’s treatment plan (Palmer CA. 2003. Gerodontic nutrition and dietary counselling for prosthodontic patients. Dent Clin N Am. 47: 355–371) |
| [28] | Matloff A. | 2013 | US | Editorial | N/A | N/A | N/A | N/A | N/A | N/A | tips on how to determine the safest texture for edentulous patients. Including cognition and motivation to eat, fatigue, positioning. Laryngeal function. I.e. involve SLT |
| [29] | Touger-Decker R et al. | 2013 | US | Opinion piece | N/A | N/A | N/A | N/A | N/A | N/A | Tooth Loss, Dentures, and Implants: Prudent measures for intervention include counselling individuals with dentures to use their knife and fork as their teeth to cut food into smaller sizes for biting and chewing ease and to moisten tough-to-chew foods. These measures can help facilitate eating pleasure and ultimately improve diet quality and nutritional status. Special populations affected by oral health issues; older adults: Diet and nutrition intervention for older adults with compromised oral integrity must target individual needs based on concurrent systemic diseases and disabilities and associated oral manifestations relative to the disease and disability and its treatment(s). It is incumbent upon dietetics practitioners to address oral health as part of nutrition and diet screening, assessment, intervention, and monitoring of older adults in particular, given their greater risk of compromised dentition and chronic disease as compared to younger counterparts |
| [23] | Bartlett DW et al. | 2013 | UK | Primary Manuscript | quasi experimental | Two printed pamphlets providing information on healthy diets: Eat well—a guide to healthy eating. London, United Kingdom: Food Standards Agency; 2005 and The good life. London, United Kingdom: Food Standards Agency; 2007. | 1 month | N = 35 edentulous patients attending Guy’s Hospital with complete dentures | To investigate how nutritional advice and denture adhesives may be associated with eating healthier foods | HEA3, NDNS and OHIP Edent questionnaires; Food intake | - |
| [30] | Mobley CC & Dounis G. | 2013 | US | Review | N/A | See paper | N/A | N/A | To identify and described dietary strategies appropriate for dental patients who receive dental care that includes the placement and maintenance of dental prostheses | N/A | Placement of a removable prosthesis should include a discussion involving patient-focused dietary strategies to promote healthful food choices, thus assisting patients to maintain optimum health. A first step is to identify a patient’s food-avoidance and modification behaviours. Then practitioners can provide guidelines for adopting food selection and preparation methods to ensure an adequate diet. Instructions for modifying foods to support healthful dietary habits and food choices can lead to positive dietary consequences and ensure patient-cantered care. Future research should focus on examining how a dental prosthesis supports a patient’s personal dietary preferences, adoption of dietary guidelines and optimum oral health. |
| [31] | Yoshida M et al. | 2014 | N/A | Review | N/A | N/A | N/A | N/A | N/A | N/A | Dietary instruction by a registered dietitian after denture treatment is reported to be essential (Allen PF. 2005. J Oral Rehabil. 32:623—8; Bradbury et al. 2006. J Dent Res. 85:463—8). |
| [32] | Rathee M et al. | 2015 | N/A | Review | N/A | N/A | N/A | N/A | N/A | N/A | Dietary Guidance for Geriatric Denture PopulationProsthetic reconstruction can require a series of appointments, dietary analysis and counselling can be easily incorporated into the treatment sequence. Hence, first few days swallowing should be practiced, such as liquid diet should be prescribed for first few days after insertion of denture. The use of soft foods is advocated for the next few days and a firm or regular diet can be eaten by the end of the week (Adams CD. 1961. J Prosthet Dent. 11:345-50; Detroit M. 1960. Nutrition for the denture patient. J Prosthet Dent. 10:53–60). |
| [24] | Wöstmann B et al. | 2016 | Germany | Primary Manuscript | Explorative intervention study | Individually tailored nutritional counselling was performed by a dietician based on the 3-day dietary record and dietary behaviour questionnaire (Lührmann et al. 1999. Eur J Nutr. 38:235–240), which were completed by the patients in advance of session | 12 months | N = 25 patients with fewer than ten pairs of opposing natural teeth (antagonists) and who were capable of feeding themselves were eligible and willing to participate | To investigate the impact of implant-prosthetic rehabilitation combined with nutritional counselling on the nutritional status of patients with severely reduced dentitions | OHIP-G14, MMS, MNA, dental status, chewing ability, labs, BMI, energy supply, 3-day dietary record | no information on what was advised is reported. |
| [15] | Suzuki H et al. | 2018 | Japan | Secondary Manuscript | Randomised controlled trial | Dietary advice pamphlets (20 min to read) given on trial entry and day of dentures from 2 sources: Test Intervention vs. American College of Prosthodontists [Felton et al. J Am Dent Assoc. 2011;142 Suppl 1:1S–20] (Control) | 3 and 6 months | N = 70 edentate patients who request new complete dentures | To reveal the combined effect of new complete dentures and simple dietary advice on the nutrient intake and masticatory function of elderly patients | BDHQ, Masticatory function-shearing and mixing | - |
| [14] | Amagai N et al. | 2017 | Japan | Primary Manuscript | Randomised controlled trial | Dietary advice pamphlets (20 min to read) given on trial entry and day of dentures from 2 sources: Japanese Ministry of Agriculture, Forestry and Fisheries [Geriatric version] (Intervention) vs. American College of Prosthodontists [Felton et al. J Am Dent Assoc. 2011;142 Suppl 1:1S–20] (Control) | 3 months | N = 70 edentulous subjects randomised 1:1 | To investigate the combined effect of complete denture renewal and simple dietary advice | OHIP-EDENT-J scores; Food intake | - |
| [18] | Kanazawa M et al. | 2019 | Japan | Secondary Manuscript | Randomised controlled trial | Dietary advice pamphlets (20 min to read) given on trial entry and day of dentures from 2 sources: Test Intervention vs. American College of Prosthodontists [Felton et al. J Am Dent Assoc. 2011;142 Suppl 1:1S–20] (Control) | 3 and 6 months | N = 70 edentate patients who request new complete dentures | To examine the medium-term effect of a new complete denture fabrication and dietary advice provided by dentists using unique pamphlets on nutrient intake in edentulous elderly patients. | BDHQ, energy intake (protein, lipids, carbohydrates), nutritional status (mineral and vitamin intake) | - |
| [16] | Suzuki H et al. | 2019 | Tokyo, Japan | Secondary Manuscript | Randomised controlled trial | Dietary advice pamphlets (20 min to read) given on trial entry and day of dentures from 2 sources: Test Intervention vs. American College of Prosthodontists [Felton et al. J Am Dent Assoc. 2011;142 Suppl 1:1S–20] (Control) | 3 and 6 months | N = 70 edentate patients who request new complete dentures | To clarify the influence of simple dietary advice on masticatory function in elderly individuals with new complete dentures | Masticatory function-shearing and mixing | - |
| [17] | Suzuki H et al. | 2019 | Tokyo, Japan | Secondary Manuscript | Randomised controlled trial | Dietary advice pamphlets (20 min to read) given on trial entry and day of dentures from 2 sources: Test Intervention vs. American College of Prosthodontists [Felton et al. J Am Dent Assoc. 2011;142 Suppl 1:1S–20] (Control) | 3 and 6 months | N = 70 edentate patients who request new complete dentures | To reveal the combined effect of new complete dentures and simple dietary advice on the nutritional statuses of elderly patients | MNA®-SF questionnaire | - |
| [13] | Komagamine Y et al. | 2016 | Japan | Study protocol | RCT protocol | Dietary advice pamphlets (20 min to read) given on trial entry and day of dentures from 2 sources: Test Intervention vs. American College of Prosthodontists [Felton et al. J Am Dent Assoc. 2011;142 Suppl 1:1S–20] (Control) | 3 and 6 months | N = 70 edentate patients who request new complete dentures | Protocol to investigate the effect of a simultaneous combination of simple dietary advice delivered by dentists and provision of new complete dentures on dietary intake in edentulous individuals who request new dentures | GOHAI, OHIP-EDENT-J questionnaires; Food intake (BDHQ); Nutritional status (MNA-SF); Anti-oxidant capacity, Anthropometry, Chewing and masticatory performance; Denture assessment (PDA); Cognitive assessment | Advice based on Japanese food Guide Spinning top to patient and person who does cooking at home. Who delivers, not stated. |
| [35] | Zelig R et al. | 2016 | N/A | Systematic review | N/A | N/A | N/A | N/A | N/A | N/A | Several authors of the studies in this review proposed that nutrition counselling should be provided, as appropriate, to individuals with missing teeth and dental prostheses.Oral health professionals can…[provide]…basic diet education or referring patients to registered dietitian/nutritionists (RD/RDN) (Touger-Decker & Mobley C. J Acad Nutr Diet. 2013;113(5):693–701).In turn, RD/RDNs should include nutrition-focused physical assessment of the oral cavity as part of their care of older adults. Moreover, nutrition interventions, including counselling, should be individualized to the patient’s dental status and ability to chew and swallow (Touger-Decker & Mobley C. J Acad Nutr Diet. 2013;113(5):693–701). |
| [37] | Zelig R et al. | 2022 | N/A | Systematic review and meta-analysis | N/A | N/A | N/A | N/A | To conduct a systematic review and meta-analysis to answer the following question: Among adults aged ≥ 60 years living in developed countries, what are the associations between tooth loss and nutritional status as assessed by a validated nutrition screening or assessment tool? | N/A | Credentialed dietitians can also identify tooth loss as part of the oral examination conducted during a nutrition assessment and by asking questions about oral factors affecting one’s ability to consume foods and fluids; these findings can be integrated into care plans to reduce risk of malnutrition. As part of interprofessional care, credentialed dietitians and other health care professionals should referpatients with tooth loss to oral health care professionals early on to optimize their oral health and prevent further tooth loss and oral disease. |
| [33] | Zelig R et al. | 2018 | US | Primary Manuscript | Retrospective cross-sectional study | N/A | N/A | N = 107 patients aged ≥ 65 who attended an urban northeast US dental school clinic | To explore the associations between nutritional and dentition status in older adults | MNA, MNA-SF, Self-MNA | - |
| [34] | Larson, M. | 2017 | US | Q&A | N/A | Harder or more solid foods, such as pieces of meat or harder pieces of vegetable’ and ‘alcohol consumption’ increases the risk of food impaction. | N/A | N/A | N/A | N/A | - |
| [25] | Nabeshima G et al. | 2018 | Japan | Primary Manuscript | Single-arm, non-controlled pilot study | 2× 20-min basic dietary counselling sessions by a nutritionist, and week 0 and ~5 aimed at increasing dietary fruit and vegetable intake and improving dietary habits with dietary feedback and advice for each patient via a custom-made leaflet in accordance with a previous study (Bradbury J et al. 2006J Dent Res. 2006;85:463–468) | 2 months + 1 week | N = 38 patients scheduled to receive RPDs, and who were currently eating < 350 g of vegetables per day | To investigate the effects of a counselling-based dietary intervention on nutritional status in partially dentate patients receiving RPDs | BDHQ, haematological biomarkers (vitamin C, α- and β-carotene), masticatory function | - |
| [36] | |||||||||||
| [26] | McCrum LA et al. | 2020 | UK | Primary Manuscript | feasibility study | 4× meetings with a trained researcher to target habit-formation around 3 dietary domains (fruit/vegetables, wholegrains, healthy proteins) | 8 months | N = 57 partially dentate older patients | To develop and test a habit-based tailored dietary intervention, in conjunction with oral rehabilitation amongst partially dentate older adults | SRBAI, MNA questionnaires; anthropometry | - |
| Region | Web Address | Title | Author/Creator | Type of Organisation | Citation | Year | Outcome Measures | Themes of Key Content |
|---|---|---|---|---|---|---|---|---|
| US | https://www.teethxpress.com/if-you-struggle-to-eat-nutrient-rich-foods-with-a-denture-dental-implants-may-help/ [Accessed 1 April 2021] | If you struggle to eat nutrient-rich foods with a denture, dental implants may help | Teethxpress | Denture manufacturer | Teethxpress. 2020. If you struggle to eat nutrient-rich foods with a denture, dental implants may help. [accessed on 24 March 2021]. https://www.teethxpress.com/if-you-struggle-to-eat-nutrient-rich-foods-with-a-denture-dental-implants-may-help/ | 2020 | N/A | Seek advice from a registered dietitian (RD) for advice on achieving a balanced diet with dentures. Achieving a balanced diet may involve vitamin supplements, juicing and swapping food sources |
| UK | https://www.nhs.uk/conditions/dentures/ [Accessed 1 April 2021] | Dentures (false teeth) | NHS | Healthcare organisation | NHS. 2018. Dentures (false teeth). [accessed on 25 March 2021]. https://www.nhs.uk/conditions/dentures/ | 2018 | N/A | Eat soft foods to start with Cut food cut into small pieces Eat slowly using both sides of mouth. Avoid chewing gum and sticky foods Avoid food with sharp edges. Can gradually return to old diet. |
| UK | https://www.glendental.co.uk/problem-dentures-chewing-gum-bad-breath/ [Accessed 1 April 2021] | The Problem with Dentures, Chewing Gum and Bad Breath. | Kotecha S | Dental practice | Kotecha S. 2019. The problem with dentures, chewing gum and bad breath. [accessed on 25 March 2021]. https://www.glendental.co.uk/problem-dentures-chewing-gum-bad-breath/ | 2019 | N/A | Mentions that there may be difficulty eating sticky, chewy or crunchy foods. A good fit modern denture will allow the patient to eat a wider range of foods. |
| AUS | https://www.inspiro.org.au/blog/looking-after-clean-your-dentures [Accessed 1 April 2021] | 9 tips on looking after your dentures and your mouth | Inspiro Community Health Service | Healthcare organisation | Inspiro Community Health Service. 2018. 9 tips on looking after your dentures and your mouth. [accessed on 26 March 2021]. https://www.inspiro.org.au/blog/looking-after-clean-your-dentures | 2018 | N/A | Recommends starting with soft foods and gives some examples e.g., soup. Recommends that when progressing to solids to cut food into small pieces and gives examples. States red meat might be hard to eat and suggests alternative cooking methods and food swaps for other sources of protein. Recommends rinsing with water when eating foods that tend to stick to dentures. Warns of issues of not being able to detect temperature of food. recommends small bites and slow thorough chewing. Gives advice on which teeth to chew and bit with. States denture adhesive could help. States that when adjusted to a denture the patient should be able to eat most foods but advises that care is still needed with hard, sharp and stick foods. |
| AUS | https://www.mydenturecare.com/en-au/expert-advice/living-with-dentures/eating-with-dentures/learning-to-eat-with-dentures/ [Accessed 1 April 2021] | My Denture Care. 2020. Learning to eat with dentures. [accessed on 29 March 2021]. https://www.mydenturecare.com/en-au/expert-advice/living-with-dentures/eating-with-dentures/learning-to-eat-with-dentures/ | My Denture Care (the official Polident website) | Dental supply manufacturer | My Denture Care. 2020. Learning to eat with dentures. [accessed on 29 March 2021]. https://www.mydenturecare.com/en-au/expert-advice/living-with-dentures/eating-with-dentures/learning-to-eat-with-dentures/ | 2020 | N/A | States that with time and practice patient will be able to enjoy many foods again Recommends eating slow and steady Recommends soft foods to help patient get used to dentures. Recommend which teeth to bite with and to use both sides of mouth. recommends trying harder foods (meat, apple) once more confident in eating with dentures. |
| NZ | https://www.healthinfo.org.nz/patientinfo/NZDAHealthyMouthHealthyAgeing.pdf [Accessed 1 April 2021] | Healthy Mouth, Healthy Ageing: ORAL HEALTH GUIDE FOR CAREGIVERS OF OLDER PEOPLE. | HealthInfo | Website | HealthInfo. 2010. Healthy Mouth, Healthy Ageing: ORAL HEALTH GUIDE FOR CAREGIVERS OF OLDER PEOPLE. [accessed on 29 March 2021]. https://www.healthinfo.org.nz/patientinfo/NZDAHealthyMouthHealthyAgeing.pdf | 2010 | N/A | Recommends cutting food into small pieces and bite sizes. Recommends mashing foods and avoiding stringy foods. Recommends moistening foods e.g., with sauces. |
| NZ | https://www.tirakaudental.co.nz/blog [Accessed 1 April 2021] | Blog | Ti Rakau Dental Centre | Dental practice | Ti Rakau Dental Centre. 2017. Blog. [accessed on 29 March 2021]. https://www.tirakaudental.co.nz/blog | 2017 | N/A | Explains how dentures differ from natural teeth and can move more when eating. Recommends starting with soft foods and gives examples (some healthy some discretionary foods). Recommends taking small bites and chewing on both sides and why this is importantRecommends avoiding very hot foods (temperature) |
| CAN | https://www.pearldentalburlington.com/blog/easy-tips-to-eat-with-new-dentures/ [Accessed 1 April 2021] | Easy Tips To Eat With New Dentures | Pearl Dental Burlington | Dental practice | Pearl Dental Burlington. 2015. Easy tips to eat with new dentures. [accessed on 30 March 2021]. https://www.pearldentalburlington.com/blog/easy-tips-to-eat-with-new-dentures/ | 2015 | N/A | Explains that dentures cannot be expected to be like natural teeth and that one has to learn to eat with them and recognised this can be frustrating as patients want to resume their usual diet. Recommends some things to try before eating in restaurants again and points out not to be disheartened if it is not easy at first. Points out it takes practice and patience. Start with soft foods Take smaller mouthfuls Chew slowly and evenly Cut food into tiny pieces rather that use teeth: try harder foods once more skilled States a denture adhesive might help to cope with harder foods. advises care with hot fluids Warns that liquids held in the mouth for a long time can loosen dentures. Recommend to bite and push and not bite and pull (as one would with natural teeth). |
| CAN | https://bakerdentureclinic.ca/getting-used-to-new-dentures/ [Accessed 1 April 2021] | Tips for Getting Used to New Dentures. | Baker Lanoue Denture Clinic | Denturist practice | Baker Lanoue Denture Clinic. 2020. Tips for getting used to new dentures. [accessed on 30 March 2021]. https://bakerdentureclinic.ca/getting-used-to-new-dentures/ | 2020 | N/A | Advises dentures will feel strange at first. Recommends limiting to softer foods at first Recommend progressing to more solid foods when patient feels more comfortable and cutting food into small pieces and eat slowly Recommends eating on both sides and avoiding sticky and hard foods. |
| Health Service Providers | |
| Author: | Inspiro Community Health Service |
| Country: | Australia |
| Citation: | Inspiro Community Health Service. 2018. 9 tips on looking after your dentures and your mouth. https://www.inspiro.org.au/blog/looking-after-clean-your-dentures [accessed on 26 March 2021]. |
| Author: | NHS (National Health Service) |
| Country: | UK |
| Citation: | NHS. 2018. Dentures (false teeth). https://www.nhs.uk/conditions/dentures/ [accessed on 25 March 2021]. |
| Author: | NHS (National Health Service) (Scotland) |
| Country: | UK |
| Citation: | NHS. 2020. Dentures (false teeth). https://www.nhsinform.scot/tests-and-treatments/dental-treatments/dentures-false-teeth [accessed on 25 March 2021]. |
| Author: | NHS 111 Wales |
| Country: | UK |
| Citation: | NHS 111 Wales. 2020. Dentures (false teeth). https://111.wales.nhs.uk/Dentures(falseteeth)/ [accessed on 26 March 2021]. |
| Health associations (including oral health) | |
| Author: | FillingGaps |
| Country: | New Zealand |
| Citation: | FillingGaps. 2015. Dentures. http://www.fillinggaps.co.nz/blog/dentures/ [accessed on 29 March 2021]. |
| Author: | British Nutrition Foundation |
| Country: | UK |
| Citation: | British Nutrition Foundation. 2018. Top tips for healthy ageing. https://www.nutrition.org.uk/healthyliving/healthyageing/top-tips-for-healthy-ageing?start=11 [accessed on 26 March 2021]. |
| Author: | Authority Dental Organisation (Tenacity Media, funders include oral B and Colgate |
| Country: | US |
| Citation: | Murphy C, Ballingham B. 2020. 99 Soft Food Diet Recipes (Eat After Tooth Extraction, Braces, Dentures): What is a soft food diet? List of foods to avoid and the best recipes. Authority Dental. https://www.pinterest.co.uk/pin/188447565635399787/ [accessed on 25 March 2021]. |
| Author: | Oral Health Foundation (Charity) |
| Country: | US |
| Citation | https://www.dentalhealth.org/diet-and-my-teeth [accessed on 10 June 2021] |
| Author: | American Academy of Implant Dentistry (Sung, on behalf of) |
| Country: | US |
| Citation: | Sung J, on behalf of the American Academy of Implant Dentistry. 2020. How Dental Implants Impact Eating and Nutrition. https://connect.aaid-implant.org/blog/dental-implants-nutrition [accessed on 25 March 2021]. |
| Author: | Sollitto M (Caregiver association and community) |
| Country: | US |
| Citation: | Sollitto, M. 2011. A dentist’s take on dentures. https://www.agingcare.com/articles/denture-care-for-false-teeth-148020.htm [accessed on 24 March 2021]. |
| Author: | Dentaly (by Tariq J) |
| Country: | US |
| Citation: | Tariq J. 2021. New Dentures: Pros, Cons, and What to Expect With Replacement Teeth. https://www.dentaly.org/us/dentures-false-teeth/new-dentures/ [accessed on 25 March 2021]. |
| Author: | Dental Reach (Saha A, on behalf of) |
| Country: | US |
| Citation:: | Saha A. 2019. Geriatric nutrition in complete denture patients. https://dentalreach.today/dental-education/geriatric-nutrition-in-complete-denture-patients/ [accessed on 25 March 2021]. |
| Dental supply manufacturers | |
| Author: | My Denture Care (the official Polident website) |
| Country: | Australia |
| Citation: | My Denture Care. 2020. Food denture wearers should be wary of. https://www.mydenturecare.com/en-au/expert-advice/living-with-dentures/eating-with-dentures/food-denture-wearers-should-be-wary-of/ [accessed on 29 March 2021]. |
| Author: | Bonjela Teething Gel |
| Country: | Australia |
| Citation: | Bonjela Teething Gel. 2018. Denture Care. https://www.bonjela.com.au/tips-advice/everyday-care/denture-care/ [accessed on 29 March 2021]. |
| Author: | Denture Living (site from P&G Fixodent) |
| Country: | US |
| Citation: | Denture living. 2020. Foods to Eat for New Denture Wearers. https://www.dentureliving.com/en-us/advice-tips/living-with-dentures/eating-and-chewing/foods-to-eat-for-new-denture-wearers [accessed on 24 March 2021]. |
| Author: | Teethxpress |
| Country: | US |
| Citation: | Teethxpress. 2020. If you struggle to eat nutrient-rich foods with a denture, dental implants may help. https://www.teethxpress.com/if-you-struggle-to-eat-nutrient-rich-foods-with-a-denture-dental-implants-may-help/ [accessed on 24 March 2021]. |
| Author: | Colgate |
| Country: | US |
| Citation: | Colgate. 2020. Eating with dentures. https://www.colgate.com/en-us/oral-health/dentures/eating-with-dentures [accessed on 25 March 2021]. |
| Dental/Denturist practices | |
| Author: | The Point Dental |
| Country: | Australia |
| Citation: | The Point Dental. 2020. EATING WITH ALL-ON-4 IMPLANTS. https://www.thepointdental.com.au/eating-with-all-on-4-implants/ [accessed on 29 March 2021]. |
| Author: | Heatherton Dental |
| Country: | Australia |
| Citation: | Heatherton Dental. 2020. Partial Dentures. https://heathertondental.com.au/partial-dentures/ [accessed on 29 March 2021]. |
| Author: | Discount Denture |
| Country: | Australia |
| Citation: | Discount Dentures. 2018. 5 foods to avoid if you have dentures. https://www.discountdentures.com.au/5-foods-to-avoid-if-you-have-dentures/ [accessed on 29 March 2021]. |
| Author: | Emergency Denture Repairs |
| Country: | Australia |
| Citation: | Emergency Denture Repairs. 2020. Dental Care Tips and Advice–FAQs. https://www.emergencydenturerepair.com.au/faq/ [accessed on 29 March 2021]. |
| Author: | Denture Health Care |
| Country: | Australia |
| Citation: | Denture Health Care. 2018. 5 best ways to treat your denture pain. https://denturehealthcare.com.au/5-best-ways-to-treat-your-denture-pain/ [accessed on 29 March 2021]. |
| Author: | Doncaster Dental Group |
| Country: | Australia |
| Citation: | Doncaster Dental Group. 2020. Partial tooth replacement with a partial denture. http://www.doncasterdental.com.au/partial_dentures [accessed on 29 March 2021]. |
| Author: | T Dental Surgery |
| Country: | Australia |
| Citation: | T dental surgery. 2020. Our services. https://www.tdental.com.au/denture [accessed on 29 March 2021]. |
| Author: | Australia Dental Burpengary |
| Country: | Australia |
| Citation: | Australia Dental Burpengary. 2019. Dentures. https://burpengarydentist.com/seniors-dental-health/dentures/ [accessed on 29 March 2021]. |
| Author: | Direct Denture Care |
| Country: | Australia |
| Citation: | Direct Denture Care. 2019. TYPES OF DENTURES by Direct Denture Care. https://www.directdenturecare.com.au/types-of-dentures-by-direct-denture-care/ [accessed on 29 March 2021]. |
| Author: | Aspen Dental Practice |
| Country: | Australia |
| Citation: | Aspen Dental Practice. 2021. Living with Dentures: Making the transition to dentures. https://www.aspendental.com/dentures/denture-advice [accessed on 29 March 2021]. |
| Author: | Pearl Dental Burlington |
| Country: | Canada |
| Citation: | Pearl Dental Burlington. 2015. Easy tips to eat with new dentures. https://www.pearldentalburlington.com/blog/easy-tips-to-eat-with-new-dentures/ [accessed on 30 March 2021]. |
| Author: | Le Denture Clinic |
| Country: | Canada |
| Citation: | Le Denture Clinic. 2016. Blog. http://www.nancyledentureclinic.com/article-blog [accessed on 30 March 2021]. |
| Author: | Classic Denture Centre |
| Country: | Canada |
| Citation: | Classic Denture Centre. 2020. Partial Dentures. https://classicdenture.ca/partial-dentures/ [accessed on 30 March 2021]. |
| Author: | Ottawa Denture Implant Centre |
| Country: | Canada |
| Citation: | Ottawa Denture Implant Centre. 2017. Resources. https://ottawadentures.com/resources/ [accessed on 30 March 2021]. |
| Author: | Breezemaxweb |
| Country: | Canada |
| Citation: | Accent Denture Services. 2020. How to eat with new dentures and foods you should avoid. https://accentdentureservices.com/eat-new-dentures-foods-avoid/ [accessed on 30 March 2021]. |
| Author: | Baker Lanoue Denture Clinic |
| Country: | Canada |
| Citation: | Baker Lanoue Denture Clinic. 2020. Tips for getting used to new dentures. https://bakerdentureclinic.ca/getting-used-to-new-dentures/ [accessed on 30 March 2021]. |
| Author: | Accent Denture Services |
| Country: | Canada |
| Citation: | Accent Denture Services. 2018. Lifestyle adjustment after dentures. https://accentdentureservices.com/lifestyle-adjustment-after-dentures/ [accessed on 30 March 2021]. |
| Author: | Bajic Denture Clinic |
| Country: | Canada |
| Citation: | Bajic Denture Clinic. 2016. The best recipe for healthy, confident eating: properly fitted dentures. https://www.bajicdentures.ca/best-recipe-for-healthy-confident-eating-properly-fitted-dentures/ [accessed on 30 March 2021]. |
| Author: | Apple Denture and Implant Solutions |
| Country: | Canada |
| Citation: | Apple Denture and Implant Solutions. 2020. How to eat all foods again with implant dentures. https://appledentures.ca/how-to-eat-all-foods-again-with-implant-dentures/ [accessed on 30 March 2021]. |
| Author: | Kelowna Denture Clinic |
| Country: | Canada |
| Citation: | Kelowna Denture Clinic. 2016. What to eat when eating is a challenge? https://kelownadentureclinic.com/foods-to-follow-oral-surgery/ [accessed on 30 March 2021]. |
| Author: | Dumbrava V |
| Country: | Canada |
| Citation: | Dumbrava V. 2020. The Best Foods for New Denture Wearers. https://calgarydentureclinic.net/blog/The+Best+Foods+for+New+Denture+Wearers/285 [accessed on 30 March 2021]. |
| Author: | Migneault F |
| Country: | Canada |
| Citation: | Migneault F. 2015. Nutrition. https://www.francismigneault.com/denturist-services/nutrition/ [accessed on 30 March 2021]. |
| Author: | Willow Dental Care Langley |
| Country: | Canada |
| Citation: | Willow Dental Care Langley. 2011. Instructions for complete denture patients. https://www.willowdentallangley.com/instructions-for-complete-denture-patients/ [accessed on 30 March 2021]. |
| Author: | Spy Hill Dental Clinic |
| Country: | Canada |
| Citation: | Spy Hill Dental Clinic. 2021. How to eat with new dentures. https://www.spyhilldental.ca/how-to-eat-with-new-dentures/ [accessed on 30 March 2021]. |
| Author: | Ti Rakau Dental Centre |
| Country: | New Zealand |
| Citation: | Ti Rakau Dental Centre. 2017. Blog. https://www.tirakaudental.co.nz/blog [accessed on 30 March 2021]. |
| Author: | Ponsonby accidental and emergency dental |
| Country: | New Zealand |
| Citation: | Ponsonby accidental and emergency dental. 2021. Frequently Asked Questions (Dental FAQs). https://ponsonbyaedental.co.nz/dental-frequently-asked-questions-faqs/ [accessed on 29 March 2021]. |
| Author: | Stock L |
| Country: | UK |
| Citation: | Stock L. 2012. Why missing teeth can result in weight gain. https://gdconline.co.uk/missing-teeth-can-result-weight-gain/ [accessed on 25 March 2021]. |
| Author: | Dentata Charta Dental Centre |
| Country: | UK |
| Citation: | Dentata Charta Dental Centre. 2021. Dentures. https://dentatacharta.co.uk/treatments/dentures/ [accessed on 26 March 2021]. |
| Author: | TDC Implant Centres |
| Country: | UK |
| Citation: | TDC Implant Centres: Smile In A Day. 2019. Considering Dentures? https://www.smileinaday.co.uk/denture-wearers/ [accessed on 26 March 2021]. |
| Author: | Oldland Dental Practice |
| Country: | UK |
| Citation: | Oldland Dental Practice. 2015. Denture Care. https://www.oldlanddental.co.uk/documents/denture.pdf [accessed on 25 March 2021]. |
| Author: | Freedom Dental |
| Country: | UK |
| Citation: | Freedom Dental. 2015. NHS Dentures in Cheadle Hulme, Cheshire. https://www.freedomdental.co.uk/nhs-dentures-cheadle-hulme-cheshire.html [accessed on 26 March 2021]. |
| Author: | The Dental Practice Fallowfield |
| Country: | UK |
| Citation: | The Dental Practice Fallowfield. 2020. Dentures. http://www.thedentalpracticefallowfield.co.uk/dentures/ [accessed on 25 March 2021]. |
| Author: | Birches Head Denture Clinic |
| Country: | UK |
| Citation: | Birches Head Denture Clinic. 2019. How to eat well and live a healthy life with dentures. https://www.birchesheaddentureclinic.co.uk/latest-news/how-to-eat-well-and-live-a-healthy-life-with-dentures [accessed on 25 March 2021]. |
| Author: | Kotecha S |
| Country: | UK |
| Citation: | Kotecha S. 2019. The problem with dentures, chewing gum and bad breath. https://www.glendental.co.uk/problem-dentures-chewing-gum-bad-breath/ [accessed on 25 March 2021]. |
| Author: | Dental Solutions of Columbus |
| Country: | US |
| Citation: | Dental Solutions of Columbus. 2018. How long after oral surgery until I can eat solid food? https://columbusdentalsolutions.com/solid-food-after-oral-surgery/ [accessed on 24 March 2021]. |
| Author: | Paparisto M |
| Country: | US |
| Citation: | Paparisto M. 2019. Can Anything Be Done to Prevent Nutrition Deficiency in Denture Wearers? https://www.twogetherdentures.com/nutrition-deficiency-in-denture-wearers/ [accessed on 25 March 2021]. |
| Author | Shtarkman G |
| Country: | US |
| Citation: | Dr. Glenn Shtarkman. Advanced Dental Center. 2017. 7 Simple Tips for Eating with Your New Dentures. https://www.bestclevelandsmiles.com/blog/7-simple-tips-eating-new-dentures/ [accessed on 24 March 2021]. |
| Author: | Dental One Associates |
| Country: | US |
| Citation: | Dental One Associates. 2014. How to eat comfortably while wearing new dentures. https://www.dentalone-ga.com/blog/how-to-eat-comfortably-while-wearing-new-dentures/ [accessed on 25 March 2021]. |
| Author | Triangle Dentistry |
| Country | US |
| Citation | Triangle Dentistry. 2019. Common problems with dentures and how to fix them. https://triangledentistry.com/common-problems-with-dentures-and-how-to-fix-them/ [accessed on 24 March 2021]. |
| Author: | McGin C, McGin W |
| Country: | US |
| Citation: | McGin C, McGin W. 2018. Putnam dentist provides 5 tips for eating with dentures this summer. https://www.quietcornerdental.com/blog/putnam-dentist-provides-5-tips-eating-dentures-summer/ [accessed on 25 March 2021]. |
| Author: | Collaborative Dental |
| Country: | US |
| Citation: | Collaborative Dental. 2016. Ten tips for new denture wearers. https://collaborative-dental.com/ten-tips-new-denture-wearers/#[accessed on 25 March 2021]. |
| Other sources | |
| Author: | MD Monthly (website) |
| Country: | Australia |
| Citation: | MD Monthly. 2020. Guidelines on Eating After All-On-4 Implants. https://mdmonthly.com/guidelines-on-eating-after-all-on-4-implants/ [accessed on 29 March 2021]. |
| Author: | Veloso M (website) |
| Country: | Canada |
| Citation: | Veloso M. 2008. A healthy diet as we grow older. https://www.medbroadcast.com/channel/nutrition/diet-and-aging/a-healthy-diet-as-we-grow-older [accessed on 30 March 2021]. |
| Author: | HealthInfo (website) |
| Country: | New Zealand |
| Citation: | HealthInfo. 2010. Healthy Mouth, Healthy Ageing: ORAL HEALTH GUIDE FOR CAREGIVERS OF OLDER PEOPLE. https://www.healthinfo.org.nz/patientinfo/NZDAHealthyMouthHealthyAgeing.pdf [accessed on 29 March 2021]. |
| Author: | Electric Teeth |
| Country: | UK |
| Citation: | Love J, Wheeler G. 2021. Dentures: a guide to types of false teeth & their costs. https://www.electricteeth.com/uk/false-teeth-dentures/ [accessed on 25 March 2021]. |
| Author: | Dock Pharmacy |
| Country: | UK |
| Citation: | Dock Pharmacy. 2021. DENTURES (FALSE TEETH) Health Advice. https://dockpharmacy.co.uk/health-az/conditions/dentures [accessed on 26 March 2021]. |
| Author: | Vu TA (For WikiHow) |
| Country: | US |
| Citation: | Vu TA. 2020. How to eat with dentures: WikiHow. https://www.wikihow.com/Eat-with-Dentures [accessed on 25 March 2021]. |
| Author: | FabOverFifty (website) |
| Country: | US |
| Citation: | FabOverFifty. 2014. Advice to chew on for new denture wearers. https://www.faboverfifty.com/health/new-denture-wearers/ [accessed on 25 March 2021]. |
References
- Tsakos, G.; Herrick, K.; Sheiham, A.; Watt, R.G. Edentulism and fruit and vegetable intake in low-income adults. J. Dent. Res. 2019, 89, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Ojima, T.; Nagahata, T.; Kondo, I.; Ninomiya, T.; Yoshita, K.; Ara, Y.; Ohkubo, T.; Murakami, K.; Nishi, M.; et al. Having few remaining teeth is associated with a low nutrient intake and low serum albumin levels in middle-aged and older Japanese individuals: Findings from the NIPPON DATA2010. Environ. Health Prev. Med. 2019, 24, 1. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Yoshihara, A.; Ogawa, H.; Sato, M.; Muramatsu, K.; Watanabe, R.; Ansai, T.; Miyazaki, H. Longitudinal association of dentition status with dietary intake in Japanese adults aged 75 to 80 years. J. Oral. Rehabil. 2016, 43, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Mendonça, N.; Granic, A.; Mathers, J.; Hill, T.R.; Siervo, M.; Adamson, A.J.; Jagger, C. Prevalence and determinants of low protein intake in very old adults: Insights from the Newcastle 85+ Study. Eur. J. Nutr. 2018, 57, 2713–2722. [Google Scholar] [CrossRef]
- Moynihan, P.J.; Butler, T.J.; Thomason, J.M.; Jepson, N.J.A. Nutrient intake in partially dentate patients: The effect of prosthetic rehabilitation. J. Dent. 2000, 28, 557–563. [Google Scholar] [CrossRef]
- Hamada, O.M.; Garrett, N.R.; Roumanas, E.D.; Kapur, K.K.; Freymiller, E.; Han, T.; Diener, T.M.; Chen, T.; Levin, S. A randomized clinical trial comparing the efficacy of mandibular implant-supported overdentures and conventional dentures in diabetic patients. Part IV: Comparisons of dietary intake. J. Prosthet. Dent. 2001, 85, 53–60. [Google Scholar] [CrossRef][Green Version]
- Madhuri, S.; Hegde, S.S.; Ravi, S.; Deepti, A.; Simpy, M. Comparison of chewing ability, oral health related quality of life and nutritional status before and after insertion of complete denture amongst edentulous patients in a Dental College of Pune. Ethiop. J. Health Sci. 2014, 24, 253–260. [Google Scholar] [CrossRef]
- McGowan, L.; McCrum, L.; Watson, S.; Cardwell, C.; McGuinness, B.; Rutherford, H.; Paice, V.; Moore, C.; Brocklehurst, P.R.; Woodside, J.V.; et al. The impact of oral rehabilitation coupled with healthy dietary advice on the nutritional status of adults: A systematic review and meta-analysis. Crit. Rev. Food Sci. Nutr. 2019, 60, 2127–2147. [Google Scholar] [CrossRef]
- Moynihan, P.; Varghese, R. Impact of Wearing Dentures on Dietary Intake, Nutritional Status, and Eating: A Systematic Review. JDR Clin. Trans. Res. 2021. Epub ahead of print. [Google Scholar] [CrossRef]
- Hyland, R.M.; Ellis, J.S.; Thomason, J.M.; Elfeky, A.; Moynihan, P.J. A qualitative study on patient perspectives of how conventional and implant-supported dentures affect eating. J. Dent. 2009, 37, 718–723. [Google Scholar] [CrossRef]
- Al-Sultani, H.F.; Field, J.C.; Thomason, J.M.; Moynihan, P.J. The Impact of Replacement Conventional Dentures on Eating Experience. JDR Clin. Trans. Res. 2019, 4, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Moynihan, P.; Varghese, R. Eating Advice for People Who Wear Dentures: Protocol for a Scoping Review of Health Education Literature. Available online: https://doi.org/10.25909/16550601 (accessed on 1 May 2022).
- Komagamine, Y.; Kanazawa, M.; Iwaki, M.; Jo, A.; Suzuki, H.; Amagai, N.; Minakuchi, S. Combined effect of new complete dentures and simple dietary advice on nutritional status in edentulous patients: Study protocol for a randomized controlled trial. Trials 2016, 17, 539. [Google Scholar] [CrossRef] [PubMed]
- Amagai, N.; Komagamine, Y.; Kanazawa, M.; Iwaki, M.; Jo, A.; Suzuki, H.; Minakuchi, S. The effect of prosthetic rehabilitation and simple dietary counseling on food intake and oral health related quality of life among the edentulous individuals: A randomized controlled trial. J. Dent. 2017, 65, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Kanazawa, M.; Komagamine, Y.; Iwaki, M.; Jo, A.; Amagai, N.; Minakuchi, S. The effect of new complete denture fabrication and simplified dietary advice on nutrient intake and masticatory function of edentulous elderly: A randomized-controlled trial. Clin. Nutr. 2018, 37, 1441–1447. [Google Scholar] [CrossRef]
- Suzuki, H.; Kanazawa, M.; Komagamine, Y.; Iwaki, M.; Jo, A.; Amagai, N.; Minakuchi, S. Influence of simplified dietary advice combined with new complete denture fabrication on masticatory function of complete denture wearers. J. Oral. Rehabil. 2019, 46, 1100–1106. [Google Scholar] [CrossRef]
- Suzuki, H.; Kanazawa, M.; Komagamine, Y.; Iwaki, M.; Jo, A.; Amagai, N.; Minakuchi, S. Changes in the nutritional statuses of edentulous elderly patients after new denture fabrication with and without providing simple dietary advice. J. Prosthodont. Res. 2019, 63, 288–292. [Google Scholar] [CrossRef]
- Kanazawa, M.; Suzuki, H.; Komagamine, Y.; Iwaki, M.; Jo, A.; Amagai, N.; Minakuchi, S. Combined effects of new complete denture fabrication and simplified dietary advice on nutrient intake in edentulous elderly patients for 6 months. Clin. Oral. Investig. 2019, 23, 2245–2252. [Google Scholar] [CrossRef]
- Moynihan, P.; Elfeky, A.; Ellis, J.S.; Seal, C.; Hyland, R.M.; Thomason, J.M. Do implant supported dentures facilitate efficacy of eating more healthily? J. Dent. 2012, 40, 843–850. [Google Scholar] [CrossRef]
- Ellis, J.S.; Elfeky AMoynihan, P.; Seal, C.; Hyland, R.M.; Thomason, J.M. The impact of dietary advice on edentulous adults’ denture satisfaction and oral health-related quality of life 6 months after intervention. Clin. Oral. Implants Res. 2010, 21, 386–391. [Google Scholar] [CrossRef]
- Bradbury, J.; Thomason, J.M.; Jepson, N.J.A.; Walls, A.W.G.; Allan, P.F.; Moynihan, P.J. Nutrition counselling increases fruit and vegetable consumption in the edentulous. J. Dent. Res. 2006, 85, 463–468. [Google Scholar] [CrossRef]
- Prakash, N.; Kalavathy, N.; Sridevi, J.; Premnath, K. Nutritional status assessment in complete denture wearers. Gerodontology 2012, 29, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D.W.; Maggio, B.; Targett, D.; Fenlon, M.R.; Thomas, J. A preliminary investigation into the use of denture adhesives combined with dietary advice to improve diets in complete denture wearers. J. Dent. 2013, 41, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Wöstmann, B.; Simon, T.; Neuhäuser-Berthold, M.; Rehmann, P. Pilot study on the influence of nutritional counselling and implant therapy on the nutritional status in dentally compromised patients. PLoS ONE 2016, 11, e0147193. [Google Scholar]
- Nabashima, G.; Fueki, K.; Ubanmochi, Y.; Wajkabayashi, N. Effect of dietary counselling with prosthetic restoration on fruit and vegetable intake in partially dentate patients: A prospective study. J. Oral Rehab. 2018, 45, 618–626. [Google Scholar] [CrossRef] [PubMed]
- McCrum, L.A.; Watson, S.; McGowan, L.; McGuinness, B.; Cardwell, C.; Clarke, M.; Woodside, J.V.; McKenna, G. Development and feasibility of a tailored habit-based dietary intervention coupled with natural tooth replacement on the nutritional status of older patients. Pilot Feasibility Stud. 2020, 24, 120. [Google Scholar] [CrossRef]
- Shigli, K.; Hebbal, M. Does prosthodontic rehabilitation change the eating patterns among completely edentulous patients? Gerodontology 2012, 29, 48–53. [Google Scholar] [CrossRef]
- Matloff, A. No teeth, no dentures: Is a regular diet possible? ASHA Lead. 2013, 18, 32–33. [Google Scholar] [CrossRef]
- Touger-Decker, R.; Mobley, C. Academy of Nutrition and Dietetics. Position of the Academy of Nutrition and Dietetics: Oral health and nutrition. J. Acad. Nutr. Diet. 2013, 113, 693–701. [Google Scholar] [CrossRef]
- Mobley, C.; Dounis, G. Dietary guidance for people wearing removable prostheses. J. Am. Dent. Assoc. 2013, 144, 11–15. [Google Scholar] [CrossRef]
- Yoshida, M.; Suzuki, R.; Kikutani, T. Nutrition and oral status in elderly people. Jpn. Dent. Sci. Rev. 2014, 50, 9–14. [Google Scholar] [CrossRef]
- Rathee, M.; Singla, S.; Bhoria, M.; Kundu, R. Role of Nutrition Assessment and Dietary Counselling in Geriatric Denture Population—An Overview. J. Oral Health Res. 2015, 6, 1–5. [Google Scholar]
- Zelig, R.; Touger-Decker, R.; Chung, M.; Byham-Gray, L. Associations between tooth loss, with or without dental prostheses, and malnutrition risk in older adults. Top. Clin. Nutr. 2016, 31, 232–247. [Google Scholar] [CrossRef]
- Larson, M. My husband often doesn’t bother to put in his dentures when eating at home. Chunks of food get stuck in his throat from time to time. They eventually pass, but it’s still worrisome. Is this dangerous? Mayo. Clin. Health Lett. 2017, 35, 8. [Google Scholar]
- Zelig, R.; Singer, R.S.; Hoskin, E.R.; Marcus, A.F.; Verdino, G.; Radler, D.R. Dentition and malnutrition risk in community-dwelling older adults. J. Aging Res. Clin. Pract. 2018, 7, 107–114. [Google Scholar]
- Kossioni, A.E.; Hajto-Bryk, J.; Janssens, B.; Maggi, S.; Marchini, L.; McKenna, G.; Müller, F.; Petrovic, M.; Roller-Wirnsberger, R.E.; Schimmel, M.; et al. Practical guidelines for physicians in promoting oral health in frail older adults. J. Am. Med. Dir. Assoc. 2018, 19, 1039–1046. [Google Scholar] [CrossRef]
- Zelig, R.; Goldstein, S.; Touger-Decker, R.; Firestone, E.; Golden, A.; Johnson, Z.; Kaseta, A.; Sackey, J.; Tomesko, J.; Parrott, J.S. Tooth loss and nutritional status in older adults: A systematic review and meta-analysis. JDR Clin. Trans. Res. 2022, 7, 4–15. [Google Scholar] [CrossRef]
| Author/Year | Country | Diet Intervention/Advice | Study Population (n) | Objective | Evaluation Measures |
|---|---|---|---|---|---|
| Studies with primary date pertaining to dietary advice for patients with dentures | |||||
| Randomised controlled trials | |||||
| Komagamine et al., 2016 [13]; Amagai et al., 2017 [14]; Suzuki et al., 2018 [15]; 2019a [16]; 2019b [17]; Kanazawa et al., 2019 [18] | Japan | Dietary advice pamphlets (20 min to read) given on trial entry and day of dentures from two sources: Japanese Ministry of Agriculture, Forestry and Fisheries [Geriatric version] (Intervention) vs. American College of Prosthodontists [citing Felton et al. 2011 as control intervention. | Edentulous participants (70) randomised 1:1 | Randomised controlled trial to investigate the combined effect of complete denture renewal and ‘simple’ dietary advice | OHIP-EDENT-J scores; Energy and nutrient intake; Masticatory function; MNA®-SF questionnaire; Antioxidant capacity; Anthropometry |
| Quasi-experimental studies | |||||
| Moynihan et al., 2012 [19] Ellis et al., 2010 [20] (based on Bradbury et al., 2006 [21]). | UK | 2 × one-to-one customised dietary interventions delivered by a community nutrition assistant and the provision of an individually tailored nutrition education package to take home. Aimed to increase fruits, vegetables, and fibre (recipes for denture wearers, e.g., seed free were provided). | Patients wearing IODs or CDs aged 40–80 years (54) | Two-cohort prospective parallel dietary intervention study to identify and describe dietary strategies appropriate for dental patients who receive dental care that includes the placement and maintenance of dental prostheses | Dietary intake, Serum antioxidant status; Chewing satisfaction |
| Prakash et al., 2012 [22] | India | Participants were explained the importance of a well-balanced diet and the benefits of regular nutritional status assessment. | Edentulous patients aged ≥50–80 years in need of complete dentures for the 1st time. (94) | Single-armed study to evaluate the effect of edentulousness and prosthetic treatment on the nutritional status of the elderly population | MNA questionnaire, anthropometric measurements, diet assessment |
| Bartlett et al., 2013 [23] | UK | Two printed pamphlets providing information on healthy eating based on Eat well: a guide to healthy eating: Food Standards Agency UK 2005 and The good life. Food Standards Agency UK; 2007 (no denture-specific advice). | Edentulous patients attending Guy’s Hospital with complete dentures (35) | To investigate how nutritional advice and denture adhesives may be associated with eating healthier foods | Dietary intake (Health Equality Audit questionnaire). Eating ability (questionnaire from UK NDNS survey) OHIP Edent |
| Wöstmann et al., 2016 [24] | Germany | Individually tailored nutritional counselling was performed by a dietitian based on assessment of dietary intake and behaviour conducted in advance of the session. | Patients < 10 pairs of opposing natural teeth (25) | Intervention study to investigate the impact of implant-supported dentures and nutritional counselling on the nutritional status | 3-day dietary record; MNA and BMI (nutritional status); Dental status including chewing ability; OHIP-G14, |
| Nabeshim et al., 2018 [25] | Japan | 2 × 20-min basic dietary counselling sessions by a nutritionist, aimed at increasing fruit and vegetable intake and improving dietary habits with feedback and advice via a custom-made leaflet in accordance with Bradbury et al. (2006). | Patients (38) scheduled to receive RPDs, and currently eating < 350 g vegetables/day | Single-armed study to investigate the effects of dietary intervention on nutritional status in partially dentate patients receiving RPDs | Dietary intake (assessed by questionnaire) Serum vitamin C, α- and β-carotene); Masticatory function. |
| McCrum et al., 2020 [26] | UK | 4 × meetings with a trained researcher to target habit-formation around three dietary domains (fruit/vegetables, wholegrains, healthy proteins). | Partially dentate older patients (57) | Feasibility study to develop and test a habit-based tailored dietary intervention, in conjunction with oral rehabilitation amongst partially dentate older adults | SRBAI, MNA questionnaires; anthropometry |
| Articles with narrative information pertaining to eating with dentures (no primary data) | |||||
| Shigli and Hebbal 2012 [27] | India | Authors recommend that dietary guidance, based on an assessment of the patient’s nutrition and dietary history, should be an integral part of prosthodontic treatment. As denture fabrication requires a series of appointments, dietary analysis and counselling can easily be incorporated into an edentulous patient’s treatment plan. | Patients undergoing complete denture procedure (35) | Single-armed study to assess these changes before and 1 month after placement of complete dentures in a dental hospital in Indore, Madhya Pradesh, India | 10-item closed-ended questionnaire |
| Matloff, 2013 [28] | US | Author includes tips on how to determine the safest texture for edentulous patients. Including cognition and motivation to eat, fatigue, positioning (sit at 90 degrees), not speaking while eating. Involvement of a speech and language therapist to assess patient. | N/A | N/A | N/A |
| Touger-Decker et al., 2013 [29] | US | Advises cutting food into smaller sizes for biting and chewing ease. Moistening tough-to-chew foods. Dietary intervention should consider patient’s systemic diseases and disabilities and associated oral manifestations. | N/A | N/A | N/A |
| Mobley and Dounis 2013 [30] | US | Placement of a removable prosthesis should include a discussion involving patient-focused dietary strategies to promote healthful food choices, thus assisting patients to maintain optimum health. A first step is to identify a patient’s food-avoidance and modification behaviours. Then, practitioners can provide guidelines for adopting food selection and preparation methods to ensure an adequate diet. Instructions for modifying foods to support healthful dietary habits and food choices can lead to positive dietary consequences and ensure patient-centred care. | N/A | To identify and describe dietary strategies appropriate for dental patients who receive dental care that includes the placement and maintenance of dental prostheses | N/A |
| Yoshida et al., 2014 [31] | N/A | Dietary instruction by a registered dietitian after denture treatment is reported to be essential (citing Allen 2005; Bradbury et al., 2006). | N/A | N/A | N/A |
| Rathee et al., 2015 [32] | N/A | Prosthetic reconstruction can require a series of appointments, dietary analysis and counselling can be incorporated into the treatment sequence. In the first few days after insertion of denture, swallowing should be practiced, and a liquid diet prescribed. ‘Soft foods’ is advocated for the next few days, then a regular diet by the end of the week (citing Adams 1961; Detroit 1960). | N/A | N/A | N/A |
| Zelig et al., 2016 [33] | N/A | Discussion states: Several included studies proposed that nutrition support should be provided to individuals who wear dental prostheses. Oral health professionals can address diet and nutrition as part of their treatment plan by providing basic diet education or referring patients to registered dietitian. Nutrition intervention should be tailored to dental status and ability to chew and swallow. | N/A | N/A | N/A |
| Larson 2017 [34] | US | Harder or more solid foods, such as pieces of meat or harder pieces of vegetable’ and ‘alcohol consumption’ increases the risk of food impaction. | N/A | N/A | N/A |
| Zelig et al., 2018 [35] | US | Discussion states: the use of nutritional screening tools by oral healthcare professionals could help to provide timely referrals to primary care physicians or Registered Dietitians/Nutritionists. Referrals to community assistance programs (such as Meals on Wheels) could also be made as appropriate to prevent decline in nutrition status. No specific reference to wearing dentures made. | Patients aged ≥ 65 who attended an urban northeast US dental school clinic (107) | To explore the associations between nutritional and dentition status in older adults | MNA, MNA-SF, Self-MNA |
| Kossioni et al., 2018 [36] | Europe | Physicians need, appropriate teaching at both undergraduate and postgraduate levels and through continuing education courses to enable them to provide dietary advice. The physician should offer all patients advice on healthy and unhealthy dietary habits. Older people with dentures often face chewing difficulties-patients and caregivers should be advised on appropriate food selection and preparation, including cutting it into small portions, chopping, mashing, or moistening before chewing. | N/A | To describe practice guidelines and tools for physicians for promoting oral health in frail older adults, based on the competencies previously described in European recommendations | N/A |
| Al-Sultani et al., 2018 [12] | UK | Qualitative data from patients receiving new dentures showed eating problems with dentures persisted following new dentures (e.g., need to avoid foods with seeds and nuts when using fixative due to food entrapment; need to slice or stew apples; avoidance of sticky food when using fixative as pull off denture) indicating that eating advice to overcome these obstacles is warranted. | Complete denture wearers undergoing denture replacement (35) | To assess eating related quality of life before and after insertion of replacement complete dentures | ESIRE questionnaire (Kelly et al., 2012 [11]) ESIRE Score and qualitative data (verbatim quotes from patients). |
| Zelig et al., 2020 [37] | US | Discussion suggests all health professionals can screen for tooth loss and lack of occlusion through oral examination during annual physicals or well visits and can refer accordingly to oral health professionals and credentialed dietitians. Dietitians can ask about oral factors affecting one’s ability to consume foods and fluids; these findings can be integrated into care plans to reduce risk of malnutrition. | N/A | To conduct evidence synthesis addressing the question: Among adults aged ≥ 60 years living in developed countries, what are the associations between tooth loss and nutritional status as assessed by a validated nutrition screening or assessment tool? | N/A |
| McGowan et al., 2020 [8] | UK | Discussion concluded: Few interventions were theory-based, and intervention components were poorly described. Overall, narrative synthesis indicated support for dietary intervention coupled with oral rehabilitation on diet. | N/A | To synthesize literature relating to oral rehabilitation coupled with dietary intervention in adults. | N/A |
| Recommendation for Dietary Intervention | Supporting Citations |
|---|---|
| Moistening food to ease chewing. | [29,36] |
| Cut food into smaller pieces to ease biting. | [29] |
| Mash food. | [36] |
| Modify recipes to make them ‘seed free’. | [19] |
| Identify patient’s food avoidances and modifications to food preparation and integrate healthier eating advice around limitations. | [30,33] |
| Sit upright when eating. | [28] |
| Avoid speaking with a food bolus in mouth. | [28] |
| Provide advice on adopting food selection (no specific example provided). | [30,36] |
| Provide advice on how to modify food preparation (no specific examples provided). | [30,36] |
| Eat liquid food for first few days, followed by ‘soft diet’ for a few days then wean to regular diet by one week (for patients new to dentures). | [32] |
| Advise that hard foods (meat pieces, hard vegetables) and consuming alcohol can increase risk of food impaction (choking). | [34] |
| Avoid sticky foods as pull denture away from fixative. | [12] |
| Avoid foods with seeds and nuts that can get trapped under denture especially if using fixative. | [12] |
| Slice apples or stew. | [12] |
| Practitioners should use a nutrition screening tool and refer those at nutritional risk to a registered dietitian. | [35] |
| Integrate a series of personalised dietary intervention with appointments for denture fabrication. | [27,33] |
| Seek expertise of speech and language therapist for correct level of textural modification. | [28] |
| Seek advice of dietitian (who should enquire about chewing ability). | [31,33,37] |
| Advice | No of Mentions | Specific Details and or Contraindications |
|---|---|---|
| Eat soft foods (easy to chew). | 38 | Mostly with reference to the early stages post insertion |
| Cut food into tiny pieces/bite sized pieces. | 34 | Tiny pieces of food can cause choking; bite-sized is correct |
| Avoid tough, crunchy, or hard food. | 32 | Especially in early stages |
| Chew on both sides (back teeth) to keep dentures more stable while you eat. | 29 | Avoiding small food items that tend to be eaten on one side was also advised |
| Avoid sticky foods. | 28 | Dried fruit, peanut butter, chewing gum were examples |
| Chew/eat slowly (thoroughly). | 27 | Especially, to avoid risk of choking |
| Avoid hot foods; denture insulating can risk burning your mouth. | 20 | Test temperature on lip |
| You will be able to eat your normal diet. | 16 | Gives a false sense of hope as unlikely to restore to full dentate function |
| Avoid foods with sharp/hard edges. | 14 | e.g., crusty bread, nuts |
| Start with liquids, purees (use a blender, smoothies) liquid meal replacements. | 12 | No mention of degree of textural modification |
| Take small bites/mouthfuls. | 10 | |
| Avoid (tough) (red) meat or ‘chewy foods’. | 9 | Only tough red meat needs to be avoided |
| Take it slowly; gradually progress from soft to harder foods. | 9 | Risk denture damage Risk of choking |
| Avoid seeds (tiny bits) as they get stuck beneath denture. | 9 | Possible alternative would be to rinse mouth after eating seeds |
| Adhesives can help (stop food getting trapped/help cope with harder foods). | 8 | |
| Drink water (liquid) while eating. | 8 | To stops starchy foods sticking, to ease chewing/swallowing) |
| Bite using canines not incisors. | 8 | |
| Don’t use toothpicks. | 7 | |
| You will need to prepare food differently. | 7 | |
| Stewed or slow-cooked meats. | 7 | |
| Take a multivitamin and mineral supplement. | 5 | Most authoritative advice recommends only vitamin D |
| Avoid spicy foods. | 4 | Relevant for sore mouths |
| Avoid coffee due to diuretic. | 3 | Authoritative advice includes coffee as part of fluid intake |
| Speak to a dietitian (or nutritionist). | 3 | |
| Eat a balanced diet (‘proper nutrition’). | 3 | No indication of what constitutes a balanced diet was provided |
| Moisten foods. | 2 | |
| Taste [flavour] can be diminished. | 2 | |
| Avoid foods you need to bite into (pizza). | 1 | |
| Avoid mints with eucalyptus oil as can dissolve acrylic dentures. | 1 | |
| If problems with eating (after time) see your dentist. | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moynihan, P.; Varghese, R. Eating Advice for People Who Wear Dentures: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 8846. https://doi.org/10.3390/ijerph19148846
Moynihan P, Varghese R. Eating Advice for People Who Wear Dentures: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(14):8846. https://doi.org/10.3390/ijerph19148846
Chicago/Turabian StyleMoynihan, Paula, and Roshan Varghese. 2022. "Eating Advice for People Who Wear Dentures: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 14: 8846. https://doi.org/10.3390/ijerph19148846
APA StyleMoynihan, P., & Varghese, R. (2022). Eating Advice for People Who Wear Dentures: A Scoping Review. International Journal of Environmental Research and Public Health, 19(14), 8846. https://doi.org/10.3390/ijerph19148846






