Analysis of Survival of Patients Hospitalized with COVID-19 in Espírito Santo, Brazil
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lauer, S.A.; Grantz, K.H.; Bi, Q.; Jones, F.K.; Zheng, Q.; Meredith, H.R.; Azman, A.S.; Reich, N.G.; Lessler, J. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Ann. Intern. Med. 2020, 172, 577–582. [Google Scholar] [CrossRef] [Green Version]
- Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. The ep-idemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi 2020, 41, 145–151. [Google Scholar]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; The Northwell COVID-19 Research Consortium. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef]
- Maciel, E.L.; Jabor, P.; Goncalves Júnior, E.; Tristão-Sá, R.; Lima, R.D.C.D.; Reis-Santos, B.; Lira, P.; Bussinguer, E.C.A.; Zandonade, E. Fatores associados ao óbito hospitalar por COVID-19 no Espírito Santo, Epidemiol. Serv. Saúde. Brasilia 2020, 29, e2020413. [Google Scholar]
- Galvão, M.H.R.; Roncalli, A.G. Fatores Associados a Maior Risco de Ocorrência de Óbito por COVID-19: Análise de Sobrevivência Com Base em Casos Confirmados. Rev. Bras. Epidemiol. 2020, 23. [Google Scholar] [CrossRef] [PubMed]
- Salinas-Escudero, G.; Carrillo-Vega, M.F.; Granados-García, V.; Martínez-Valverde, S.; Toledano-Toledano, F.; Garduño-Espinosa, J. A survival analysis of COVID-19 in the Mexican population. BMC Public Health 2020, 20, 1616. [Google Scholar]
- Agarwal, N.; Biswas, B.; Singh, C.; Nair, R.; Mounica, G.; Jha, A.R.; Das, K.M. Early Determinants of Length of Hospital Stay: A Case Control Survival Analysis among COVID-19 Patients admitted in a Tertiary Healthcare Facility of East India. J. Prim. Care Community Health 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.L. An Introduction to Survival Analysis. Princ. Pract. Clin. Res. 2018, 373–381. [Google Scholar] [CrossRef]
- Llaro-Sánchez, M.K.; Gamarra-Villegas, B.E.; Campos-Correa, K.E. Características clínico-epidemiológicas y análisis de sobrevida en fallecidos por COVID-19 atendidos en establecimientos de la Red Sabogal-Callao 2020. Horiz. Med. 2020, 20. [Google Scholar]
- Chen, S.; Sun, H.; Heng, M.; Tong, X.; Geldsetzer, P.; Wang, Z.; Wu, P.; Yang, J.; Hu, Y.; Wang, C.; et al. Factors Predicting Progression to Severe COVID-19: A Competing Risk Survival Analysis of 1753 Patients in Community Isolation in Wuhan, China. Engineering 2021. [Google Scholar] [CrossRef] [PubMed]
- Anderegg, N.; Panczak, R.; Egger, M.; Low, N.; Riou, J. Survival among people hospitalized with COVID-19 in Switzerland: A nationwide population-based analysis. BMC Med. 2022, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Ministério Da Saúde. Boletim Epidemiológico Especial: Covid-19. Semana Epidemiológica 48. 28/11 a 4/12/2021. [In-ternet] 2021 [cited Feb 14, 2022]. Available online: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/boletins/boletins-epidemiologicos/edicoes/2021/boletim-epidemiologico-vol-52-no-48.pdf/view (accessed on 30 December 2021).
- Espírito Santo. Boletim Epidemiológico Covid-19. Informe Epidemiológico semana 48. [Internet] 2021 [cited Feb 14, 2022]. Available online: https://saude.es.gov.br/coronavirus_boletim_epidemiologico (accessed on 31 December 2021).
- Instituto Brasileiro de Geografia e Estatística. Panorama [Internet]. 2022 [cited Feb 14, 2022]. Available online: https://cidades.ibge.gov.br/brasil/panorama (accessed on 14 February 2022).
- Espírito Santo. Espírito Santo é Primeiro Lugar em Transparência dos Dados do Coronavírus [internet]. Available online: https://www.es.gov.br/Noticia/espirito-santo-e-primeiro-lugar-em-transparencia-dos-dados-do-coronavirus (accessed on 31 December 2021).
- Secretaria de Estado da Saúde do Espírito Santo (ES). E-SUS VIGILÂNCIA EM SAÚDE (E-SUS VS). 2020. Available online: https://saude.es.gov.br (accessed on 10 September 2021).
- Sousa, G.J.B.; Garces, T.S.; Cestari, V.R.F.; Florêncio, R.S.; Moreira, T.M.M.; Pereira, M.L.D. Mortality and survival of COVID-19. Epidemiol. Infect. 2020, 148. [Google Scholar] [CrossRef] [PubMed]
- Teich, V.D.; Klajner, S.; Almeida, F.A.S.; Dantas, A.C.B.; Laselva, C.R.; Torritesi, M.G.; Canero, T.R.; Berwanger, O.; Rizzo, L.V.; Reis, E.P.; et al. Características epidemiológicas e clínicas dos pacientes com COVID-19 no Brasil. Einstein São Paulo 2020, 18. [Google Scholar] [CrossRef]
- Santos, P.S.A.; Mateus, S.R.M.; de Oliveira Silva, M.F.; de Souza Figueiredo, P.T.; Campolino, R.G. Perfil epidemiológico da mortalidade de pacientes internados por Covid-19 na unidade de terapia intensiva de um hospital universitário. Braz. J. Dev. Curitiba 2021, 7, 45981–45992. [Google Scholar]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020, 180, 934–943. [Google Scholar] [CrossRef] [Green Version]
- Liu, K.; Chen, Y.; Lin, R.; Han, K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J. Infect. 2020, 80, e14–e18. [Google Scholar] [CrossRef] [Green Version]
- Nascimento, M.D.M. COVID-19 and death of older adults in the Northeast region of Brazil: A survival analysis. J. Health NPEPS 2021, 6, 56–72. [Google Scholar] [CrossRef]
- Campos, H.; Sobreira Sena, A.L.; Menezes Reis, R. Complicações cardiovasculares associadas ao COVID-19. SAPIENS-Rev. Divulg. Cient. 2021, 2, 39–49. [Google Scholar]
- Seif, M.; Sharafi, M.; Ghaem, H.; Kasraei, F. Factors associated with survival of Iranian patients with COVID-19: Comparison of Cox regression and mixture cure model. Trop. Dis. Travel Med. Vaccines 2022, 8, 1–7. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Qu, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. China medical treatment expert group for COVID-19 2020. Clinical Characteristics of coronavirus disease in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Lu, W.; Yu, S.; Liu, H.; Suo, L.; Tang, K.; Hu, J.; Shi, Y.; Hu, K. Survival Analysis and Risk Factors in COVID-19 Patients. Disaster Med. Public Heath. Prep. 2021, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Lopes-Júnior, L.C.; Bomfim, E.; Da Silveira, D.S.C.; Pessanha, R.M.; Schuab, S.I.P.C.; Lima, R.A.G. Effectiveness of mass testing for control of COVID-19: A systematic review protocol. BMJ Open 2020, 10, e040413. [Google Scholar] [CrossRef]
- Lopes-Júnior, L.C.; Siqueira, P.C.; Maciel, E.L.N. School reopening and risks accelerating the COVID-19 pandemic: A systematic review and meta-analysis protocol. PLoS ONE 2021, 16, e0260189. [Google Scholar] [CrossRef]
- OSHA. Occupational Safety and Health Administration. Guidance on Preparing Workplaces for COVID-19; US Department of Labor: Washington, DC, USA, 2020.
- Bahia. Secretaria da Saúde do Estado; Superintendência de Vigilância e Proteção da Saúde; Diretoria de Vigilância e Atenção à Saúde do Trabalhador; Centro Estadual de Referência em Saúde do Trabalhador. Orientações Técnicas Para a Investigação e Notificação de Casos de COVID-19 Relacionados ao Trabalho; Nobre LCC e Castro JSM, organizadores; SUS/BAHIA: Salvador, Brasil, 2020. [Google Scholar]
- Bolina, A.F.; Bomfim, E.; Lopes-Júnior, L.C. Frontline Nursing Care: The COVID-19 Pandemic and the Brazilian Health System. SAGE Open Nurs. 2020, 6. [Google Scholar] [CrossRef]
- da Silva Junior, F.J.G.; Silva Sales, J.C.; de Souza Monteiro, C.F.; Costa, A.P.C.; Campos, L.R.B.; Miranda, P.I.G.; Monteiro, T.A.D.S.; Lima, R.A.G.; Lopes-Junior, L.C. Impact of COVID-19 pandemic on mental health of young people and adults: A systematic review protocol of observational studies. BMJ Open 2020, 10, e039426. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef]
- Dietz, W.; Santos-Burgoa, C. Obesity and its Implications for COVID-19 Mortality. Obesity 2020, 28, 1005. [Google Scholar] [CrossRef] [Green Version]
- Simonnet, A.; Chetboun, M.; Poissy, J.; Raverdy, V.; Noulette, J.; Duhamel, A.; Labreuche, J.; Mathieu, D.; Pattou, F.; Jourdain, M.; et al. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity 2020, 28, 1195–1199. [Google Scholar] [CrossRef] [PubMed]
- Honce, R.; Schultz-Cherry, S. Impact of Obesity on Influenza A Virus Pathogenesis, Immune Response, and Evolution. Front. Immunol. 2019, 10, 1071. [Google Scholar] [CrossRef] [PubMed]
- da Silva, A.L.O.; Moreira, J.C.; Martins, S.R. COVID-19 e tabagismo: Uma relação de risco. Cad. Saúde Pública 2020, 36, e00072020. [Google Scholar] [CrossRef] [PubMed]
- Jehi, L.; Ji, X.; Milinovich, A.; Erzurum, S.; Merlino, A.; Gordon, S.; Young, J.B.; Kattan, M.W. Development and validation of a model for individualized prediction of hospitalization risk in 4,536 patients with COVID-19. PLoS ONE 2020, 15, e0237419. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Tao, Z.-W.; Wang, L.; Yuan, M.-L.; Liu, K.; Zhou, L.; Wei, S.; Deng, Y.; Liu, J.; Liu, H.-G.; et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin. Med. J. 2020, 133, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Yu, J.; He, W.; Chen, L.; Yuan, G.; Dong, F.; Chen, W.; Cao, Y.; Yang, J.; Cai, L.; et al. Risk factors for death in 1859 subjects with COVID-19. Leukemia 2020, 34, 2173–2183. [Google Scholar] [CrossRef]
- Vardavas, C.I.; Nikitara, K. COVID-19 and smoking: A systematic review of the evidence. Tob. Induc. Dis. 2020, 18, 20. [Google Scholar] [CrossRef]
- Engin, A.B.; Engin, E.D.; Engin, A. Two important controversial risk factors in SARS-CoV-2 infection: Obesity and smoking. Environ. Toxicol. Pharmacol. 2020, 78, 103411. [Google Scholar] [CrossRef]
- Pecly, I.M.D.; Azevedo, R.B.; Muxfeldt, E.S.; Botelho, B.G.; Albuquerque, G.G.; Diniz, P.H.P.; Silva, R.; Rodrigues, C.I.S. COVID-19 and chronic kidney disease: A comprehensive review. J. Bras. de Nefrol. 2021, 43, 383–399. [Google Scholar] [CrossRef]
- Yamada, T.; Mikami, T.; Chopra, N.; Miyashita, H.; Chernyavsky, S.; Miyashita, S. Patients with chronic kidney disease have a poorer prognosis of coronavirus disease 2019 (COVID-19): An experience in New York City. Int. Urol. Nephrol. 2020, 52, 1405–1406. [Google Scholar] [CrossRef]
- Yang, K.; Sheng, Y.; Huang, C.; Jin, Y.; Xiong, N.; Jiang, K.; Lu, H.; Liu, J.; Yang, J.; Dong, Y.; et al. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: A multicentre, retrospective, cohort study. Lancet Oncol. 2020, 21, 904–913. [Google Scholar] [CrossRef]
- Bellan, M.; Patti, G.; Hayden, E.; Azzolina, D.; Pirisi, M.; Acquaviva, A.; Aimaretti, G.; Valletti, P.A.; Angilletta, R.; Arioli, R.; et al. Fatality rate and predictors of mortality in an Italian cohort of hospitalized COVID-19 patients. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Jiménez, E.; Fontán-Vela, M.; Valencia, J.; Fernandez-Jimenez, I.; Álvaro-Alonso, E.A.; Izquierdo-García, E.; Cebas, A.L.; Ruiz-Elvira, E.G.; Troya, J.; Tebar-Martinez, A.J.; et al. Characteristics, complications and outcomes among 1549 patients hospitalised with COVID-19 in a secondary hospital in Madrid, Spain: A retrospective case series study. BMJ Open 2020, 10, e042398. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization. Neurology and COVID-19. Scientific Report September 29, 2021. Available online: https://iris.paho.org/handle/10665.2/55676 (accessed on 24 June 2022).



| Death due to COVID-19 | Total | ||||||
|---|---|---|---|---|---|---|---|
| No | Yes | ||||||
| N | % | N | % | N | % | ||
| Sociodemographic variables | Categories | ||||||
| Age range | 0–59 years | 4681 | 59.1 | 453 | 24 | 5134 | 52.4 |
| Education | Elementary school | 1599 | 38.9 | 594 | 48.9 | 2193 | 41.2 |
| Pregnant women | No | 3550 | 44.8 | 847 | 44.9 | 4397 | 44.8 |
| Race/Color | Nonwhite | 3577 | 45.2 | 894 | 47.4 | 4471 | 45.6 |
| Sex | Male | 4278 | 54 | 1034 | 54.9 | 5312 | 54.2 |
| Place of Notification | Tertiary | 4861 | 61.4 | 1265 | 67.1 | 6126 | 62.5 |
| PCD | No | 7628 | 96.3 | 1838 | 97.5 | 9466 | 96.5 |
| Homeless | No | 7715 | 97.4 | 1876 | 99.5 | 9591 | 97.8 |
| Household Health Region | Metropolitan | 4792 | 60.5 | 1527 | 81 | 6319 | 64.4 |
| Household Health Region | Metropolitan | 4726 | 59.7 | 1537 | 81.5 | 6263 | 63.9 |
| Zone | Urban | 6778 | 85.6 | 1727 | 91.6 | 8505 | 86.7 |
| Health Professional | No | 7013 | 88.5 | 1742 | 92.4 | 8755 | 89.3 |
| Work-related Infection | No | 5822 | 73.5 | 1609 | 85.4 | 7431 | 75.8 |
| Clinical Variables | |||||||
| Fever | Yes | 4542 | 57.3 | 1197 | 63.5 | 5739 | 58.5 |
| Difficulty Breathing | Yes | 2824 | 35.7 | 1188 | 63 | 4012 | 40.9 |
| Flapping Wing Nose | Yes | 69 | 0.9 | 36 | 1.9 | 105 | 1.1 |
| Intercostal Tachycardia | Yes | 141 | 1.8 | 46 | 2.4 | 187 | 1.9 |
| Cyanosis | Yes | 51 | 0.6 | 41 | 2.2 | 92 | 0.9 |
| O2 Saturation < 95% | Yes | 1745 | 22 | 1020 | 54.1 | 2765 | 28.2 |
| Coma | Yes | 20 | 0.3 | 22 | 1.2 | 42 | 0.4 |
| Coughing | Yes | 5208 | 65.7 | 1287 | 68.3 | 6495 | 66.2 |
| Sputum Production | Yes | 437 | 5.5 | 108 | 5.7 | 545 | 5.6 |
| Nasal or Conjunctival Congestion | Yes | 946 | 11.9 | 201 | 10.7 | 1147 | 11.7 |
| Runny Nose | Yes | 2034 | 25.7 | 429 | 22.8 | 2463 | 25.1 |
| Sore Throat | Yes | 1474 | 18.6 | 297 | 15.8 | 1771 | 18.1 |
| Difficulty Swallowing | Yes | 254 | 3.2 | 62 | 3.3 | 316 | 3.2 |
| Diarrhea | Yes | 1171 | 14.8 | 252 | 13.4 | 1423 | 14.5 |
| Nausea/Vomiting | Yes | 1057 | 13.3 | 218 | 11.6 | 1275 | 13 |
| Cephalea | Yes | 3079 | 38.9 | 555 | 29.4 | 3634 | 37.1 |
| Irritability/Confusion | Yes | 106 | 1.3 | 37 | 2 | 143 | 1.5 |
| Adynamia/Weakness | Yes | 2403 | 30.3 | 805 | 42.7 | 3208 | 32.7 |
| Pharyngeal Exudate | Yes | 64 | 0.8 | 17 | 0.9 | 81 | 0.8 |
| Conjunctivitis | Yes | 40 | 0.5 | 7 | 0.4 | 47 | 0.5 |
| Convulsion | Yes | 22 | 0.3 | 9 | 0.5 | 31 | 0.3 |
| Loss of Sense of Smell | Yes | 712 | 9 | 148 | 7.9 | 860 | 8.8 |
| Loss of Taste | Yes | 804 | 10.2 | 156 | 8.3 | 960 | 9.8 |
| Comorbidities | |||||||
| Chronic Pulmonary Disease | Yes | 336 | 4.2 | 197 | 10.5 | 533 | 5.4 |
| Chronic Cardiovascular Disease * | Yes | 2816 | 35.6 | 1208 | 64.1 | 4024 | 41 |
| Chronic Kidney Disease | Yes | 140 | 1.8 | 100 | 5.3 | 240 | 2.4 |
| Chronic Liver Disease | Yes | 20 | 0.3 | 31 | 1.6 | 51 | 0.5 |
| Diabetes Mellitus | Yes | 1368 | 17.3 | 643 | 34.1 | 2011 | 20.5 |
| Immunodeficiency | Yes | 41 | 0.5 | 27 | 1.4 | 68 | 0.7 |
| HIV Infection | Yes | 30 | 0.4 | 9 | 0.5 | 39 | 0.4 |
| Neoplasm (Solid or Hematological Tumor) | Yes | 58 | 0.7 | 40 | 2.1 | 98 | 1 |
| Smoking | Yes | 177 | 2.2 | 155 | 8.2 | 332 | 3.4 |
| Bariatric Surgery | Yes | 17 | 0.2 | 1 | 0.1 | 18 | 0.2 |
| Obesity | Yes | 505 | 6.4 | 442 | 23.4 | 947 | 9.7 |
| Tuberculosis | Yes | 4 | 0.1 | 7 | 0.4 | 11 | 0.1 |
| Neoplasms | Yes | 92 | 1.2 | 101 | 5.4 | 193 | 2 |
| Chronic Neurological Disease | Yes | 191 | 2.4 | 217 | 11.5 | 408 | 4.2 |
| Dependent Variable (Death from COVID-19) | p-Value * | OR | 95% CI | ||
|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||
| Work-related infection | No | <0.001 | 3.80 | 1.89 | 7.65 |
| Yes | - | 1 | - | - | |
| Age group | 0–59 years | - | 1 | - | - |
| 60–79 years | <0.001 | 3.59 | 2.94 | 4.39 | |
| 80 years or older | <0.001 | 8.30 | 6.40 | 10.77 | |
| Education | Illiterate | 0.018 | 1.42 | 1.06 | 1.89 |
| Elementary School | 0.061 | 1.34 | 0.99 | 1.81 | |
| High School | 0.002 | 1.68 | 1.21 | 2.32 | |
| Higher Education | - | 1 | - | - | |
| Chronic Cardiovascular Disease | No | - | 1 | - | - |
| Yes | <0.001 | 1.73 | 1.45 | 2.07 | |
| Chronic Kidney Disease | No | - | 1 | - | - |
| Yes | 0.001 | 2.66 | 1.68 | 4.19 | |
| Immunodeficiency | No | - | 1 | - | - |
| Yes | <0.001 | 4.4 | 1.78 | 11.55 | |
| Smoking | No | - | 1 | - | - |
| Yes | <0.001 | 2.73 | 1.90 | 3.91 | |
| Obesity | No | - | 1 | - | - |
| Yes | <0.001 | 8.33 | 6.69 | 10.8 | |
| Neoplasms | No | - | 1 | - | - |
| Yes | <0.001 | 5.40 | 3.27 | 8.93 | |
| Chronic Neurological Disease | No | - | 1 | - | - |
| Yes | <0.001 | 5.3 | 4.00 | 8.50 | |
| Variables | Qui-Square | p-Value * |
|---|---|---|
| Work-related Infection | 0.16 | 0.694 |
| Age Group | 7.86 | 0.020 |
| Education | 16.46 | 0.001 |
| Chronic Cardiovascular Disease ** | 7.44 | 0.006 |
| Chronic Kidney Disease | 5.81 | 0.016 |
| Immunodeficiency | 0.29 | 0.590 |
| Smoking | 19.4 | <0.001 |
| Obesity | 22.9 | <0.001 |
| Neoplasms | 0.94 | 0.333 |
| Chronic Neurological Disease | 16.9 | <0.001 |
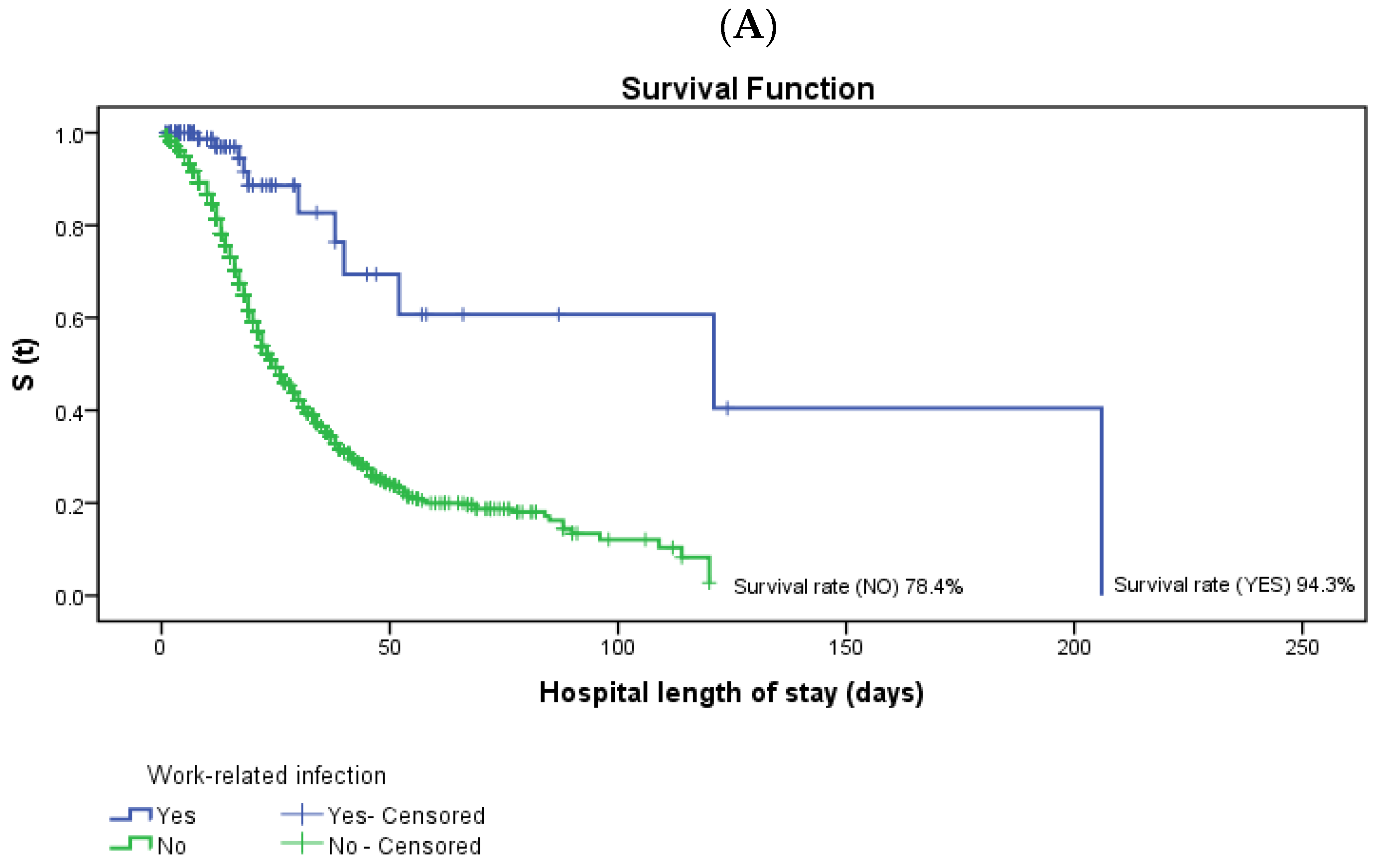
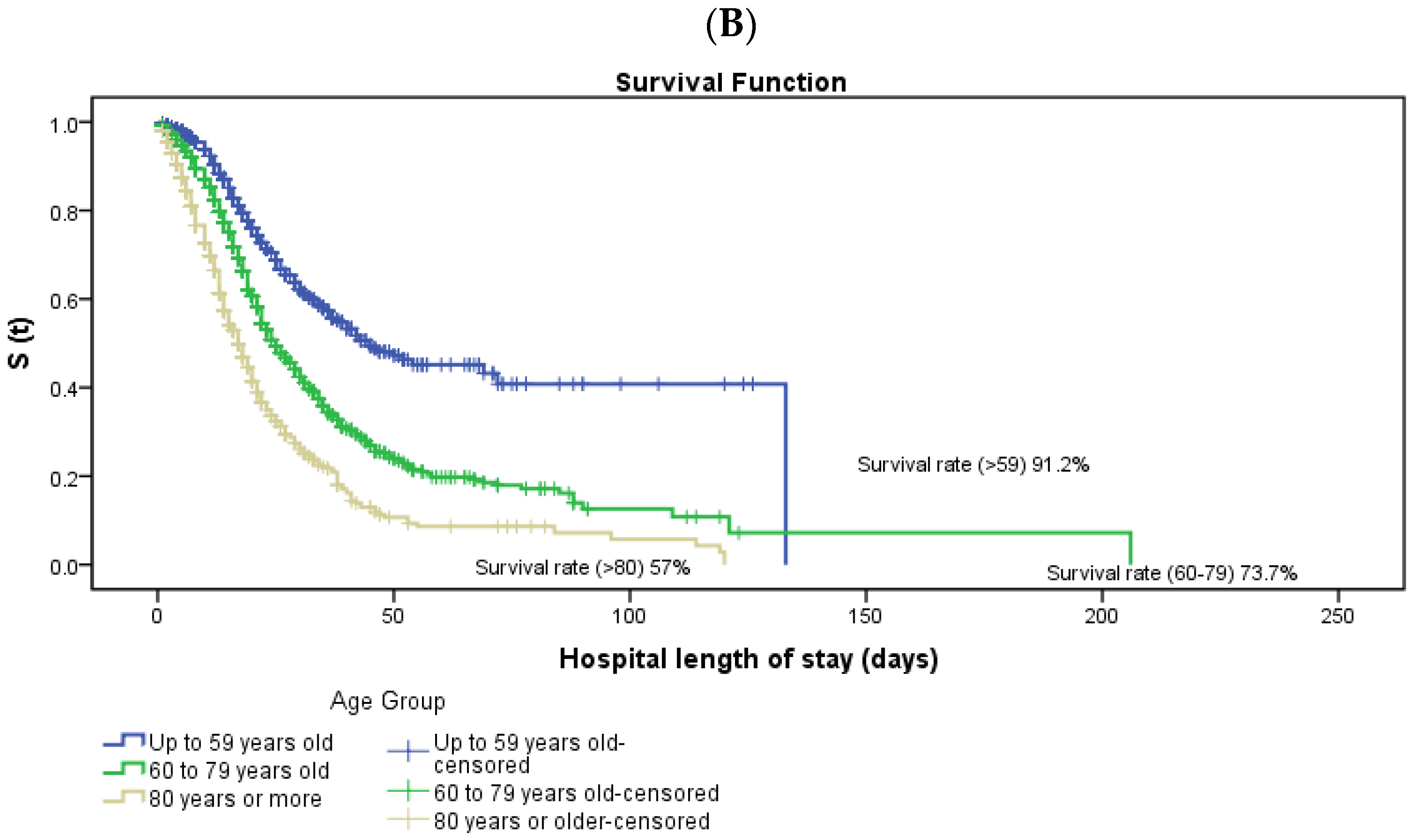
| Variables | Categories | Survival Rate (Days) | Mean | ±Standard Deviation | Lower Limit | Upper Limit | Log-Rank p-Value | |
|---|---|---|---|---|---|---|---|---|
| N | % | |||||||
| Work-related Infection | Yes | 183 | 94.3 | 121.2 | 23.2 | 75.7 | 166.7 | <0.001 |
| No | 5582 | 78.4 | 39.5 | 1.3 | 37.0 | 42.0 | ||
| General | 5765 | 78.8 | 44.9 | 2.9 | 39.2 | 50.6 | ||
| Age Group | 0–59 years | 4494 | 91.2 | 71.0 | 3.3 | 64.5 | 77.5 | <0.001 |
| 60–79 years | 2409 | 73.7 | 45.9 | 3.8 | 38.4 | 53.4 | ||
| 80 years or older | 672 | 57.0 | 26.6 | 1.6 | 23.4 | 29.8 | ||
| General | 7575 | 80.8 | 48.9 | 3.2 | 42.7 | 55.1 | ||
| Education | Illiterate | 77 | 72.5 | 28.8 | 2.8 | 23.2 | 34.3 | 0.001 |
| Elementary School | 565 | 72.8 | 38.9 | 2.2 | 34.7 | 43.1 | ||
| High School | 323 | 82.0 | 37.7 | 1.9 | 33.9 | 41.5 | ||
| Higher Education | 200 | 78.7 | 40.8 | 4.4 | 32.2 | 49.4 | ||
| General | 1165 | 77.1 | 44.5 | 3.0 | 38.7 | 50.4 | ||
| Obesity | Yes | 483 | 53.3 | 35.7 | 3.6 | 28.7 | 42.7 | 0.001 |
| No | 7068 | 83.7 | 47.6 | 1.7 | 44.3 | 50.9 | ||
| General | 7551 | 80.7 | 48.2 | 3.0 | 42.3 | 54.1 | ||
| Neoplasms | Yes | 83 | 47.4 | 24.5 | 2.4 | 19.9 | 29.2 | <0.001 |
| No | 7478 | 81.4 | 49.3 | 3.1 | 43.1 | 55.4 | ||
| General | 7561 | 80.8 | 48.2 | 3.0 | 42.4 | 54.1 | ||
| Chronic Neurological Disease | Yes | 180 | 46.3 | 28.8 | 2.8 | 23.2 | 34.4 | <0.001 |
| No | 7380 | 82.3 | 52.8 | 3.4 | 46.1 | 59.5 | ||
| General | 7560 | 80.8 | 48.2 | 3.0 | 42.4 | 54.1 | ||
| Chronic Cardiovascular Disease * | Yes | 2675 | 69.9 | 37.2 | 1.4 | 34.4 | 40.0 | <0.001 |
| No | 4883 | 88.3 | 61.6 | 5.7 | 50.4 | 72.8 | ||
| General | 7558 | 80.8 | 48.2 | 3.0 | 42.4 | 54.1 | ||
| Chronic Kidney Disease | Yes | 135 | 59.2 | 34.1 | 4.5 | 25.4 | 42.8 | <0.001 |
| No | 7425 | 81.3 | 48.5 | 3.0 | 42.6 | 54.4 | ||
| General | 7560 | 80.8 | 48.2 | 3.0 | 42.3 | 54.1 | ||
| Immunodeficiency | Yes | 40 | 59.7 | 25.7 | 2.4 | 21.0 | 30.4 | 0.127 |
| No | 7520 | 80.9 | 48.5 | 3.0 | 42.6 | 54.4 | ||
| General | 7560 | 80.8 | 48.2 | 3.0 | 42.4 | 54.1 | ||
| Smoking | Yes | 171 | 53.4 | 35.5 | 3.6 | 28.4 | 42.5 | <0.001 |
| No | 7389 | 81.7 | 49.1 | 3.4 | 42.5 | 55.8 | ||
| General | 7560 | 80.8 | 48.2 | 3.0 | 42.4 | 54.1 | ||
| Variables | p-Value | HR 1 | 95%CI to HR | p-Value | HR 1 | 95%CI to HR | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | ||||||
| Work-related Infection | No | <0.001 | 5.60 | 2.90 | 10.81 | <0.001 | 4.33 | 2.21 | 8.46 |
| Yes | - | 1 | - | - | - | 1 | - | - | |
| Age Group ** | 0–59 years | - | 1 | - | - | - | 1 | - | - |
| 60–79 years | <0.001 | 2.16 | 1.89 | 2.48 | <0.001 | 1.62 | 1.38 | 1.89 | |
| 80 years or older | <0.001 | 4.33 | 3.59 | 5.23 | <0.001 | 2.56 | 2.13 | 3.08 | |
| Education ** | Illiterate | 0.025 | 1.35 | 1.04 | 1.76 | 0.105 | 1.23 | 0.96 | 1.58 |
| Elementary School | 0.016 | 1.22 | 1.04 | 1.43 | 0.142 | 1.22 | 0.94 | 1.59 | |
| High School | 0.667 | 0.96 | 0.80 | 1.15 | 0.128 | 1.24 | 0.94 | 1.64 | |
| Higher Education | - | 1 | - | - | - | 1 | - | - | |
| Obesity ** | No | - | 1 | - | - | - | 1 | - | - |
| Yes | <0.001 | 2.72 | 2.31 | 3.20 | <0.001 | 2.28 | 1.99 | 2.60 | |
| Neoplasms * | No | - | 1 | - | - | - | 1 | - | - |
| Yes | <0.001 | 1.99 | 1.62 | 2.43 | <0.001 | 1.81 | 1.40 | 2.35 | |
| Chronic Neurological Disease ** | No | - | 1 | - | - | - | 1 | - | - |
| Yes | <0.001 | 3.05 | 2.44 | 3.80 | <0.001 | 1.68 | 1.39 | 2.02 | |
| Chronic Cardiovascular Disease ** | No | - | 1 | - | - | - | 1 | - | - |
| Yes | <0.001 | 2.20 | 1.90 | 2.50 | 0.028 | 118 | 1.02 | 1.37 | |
| Chronic Kidney Disease ** | No | - | 1 | - | - | - | 1 | - | - |
| Yes | <0.001 | 1.73 | 1.41 | 2.11 | 0.004 | 1.50 | 1.14 | 1.99 | |
| Immunodeficiency * | No | - | 1 | - | - | - | 1 | - | - |
| Yes | 0.134 | 1.34 | 0.91 | 1.96 | 0.379 | 1.24 | 0.78 | 1.99 | |
| Smoking ** | No | - | 1 | - | - | - | 1 | - | - |
| Yes | <0.001 | 2.52 | 1.95 | 3.26 | 0.001 | 1.41 | 1.15 | 1.75 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garbin, J.R.T.; Leite, F.M.C.; Lopes-Júnior, L.C.; Dell’Antonio, C.S.d.S.; Dell’Antonio, L.S.; Santos, A.P.B.d. Analysis of Survival of Patients Hospitalized with COVID-19 in Espírito Santo, Brazil. Int. J. Environ. Res. Public Health 2022, 19, 8709. https://doi.org/10.3390/ijerph19148709
Garbin JRT, Leite FMC, Lopes-Júnior LC, Dell’Antonio CSdS, Dell’Antonio LS, Santos APBd. Analysis of Survival of Patients Hospitalized with COVID-19 in Espírito Santo, Brazil. International Journal of Environmental Research and Public Health. 2022; 19(14):8709. https://doi.org/10.3390/ijerph19148709
Chicago/Turabian StyleGarbin, Juliana Rodrigues Tovar, Franciéle Marabotti Costa Leite, Luís Carlos Lopes-Júnior, Cristiano Soares da Silva Dell’Antonio, Larissa Soares Dell’Antonio, and Ana Paula Brioschi dos Santos. 2022. "Analysis of Survival of Patients Hospitalized with COVID-19 in Espírito Santo, Brazil" International Journal of Environmental Research and Public Health 19, no. 14: 8709. https://doi.org/10.3390/ijerph19148709
APA StyleGarbin, J. R. T., Leite, F. M. C., Lopes-Júnior, L. C., Dell’Antonio, C. S. d. S., Dell’Antonio, L. S., & Santos, A. P. B. d. (2022). Analysis of Survival of Patients Hospitalized with COVID-19 in Espírito Santo, Brazil. International Journal of Environmental Research and Public Health, 19(14), 8709. https://doi.org/10.3390/ijerph19148709








