Factors Affecting the Occurrence of Mental Health Problems in Female Cancer Survivors: A Nationwide Cohort Study
Abstract
:1. Introduction
Purpose of Study
- Identifying general and clinical characteristics of study participants;
- Identifying the incidence and risk of anxiety disorders according to the cancer survivorship stage and health-related behaviors of the study participants;
- Identifying the incidence and risk of depressive disorders according to the cancer survivorship stage and health-related behaviors of the study participants.
2. Materials and Methods
2.1. Research Design
2.2. Data Source
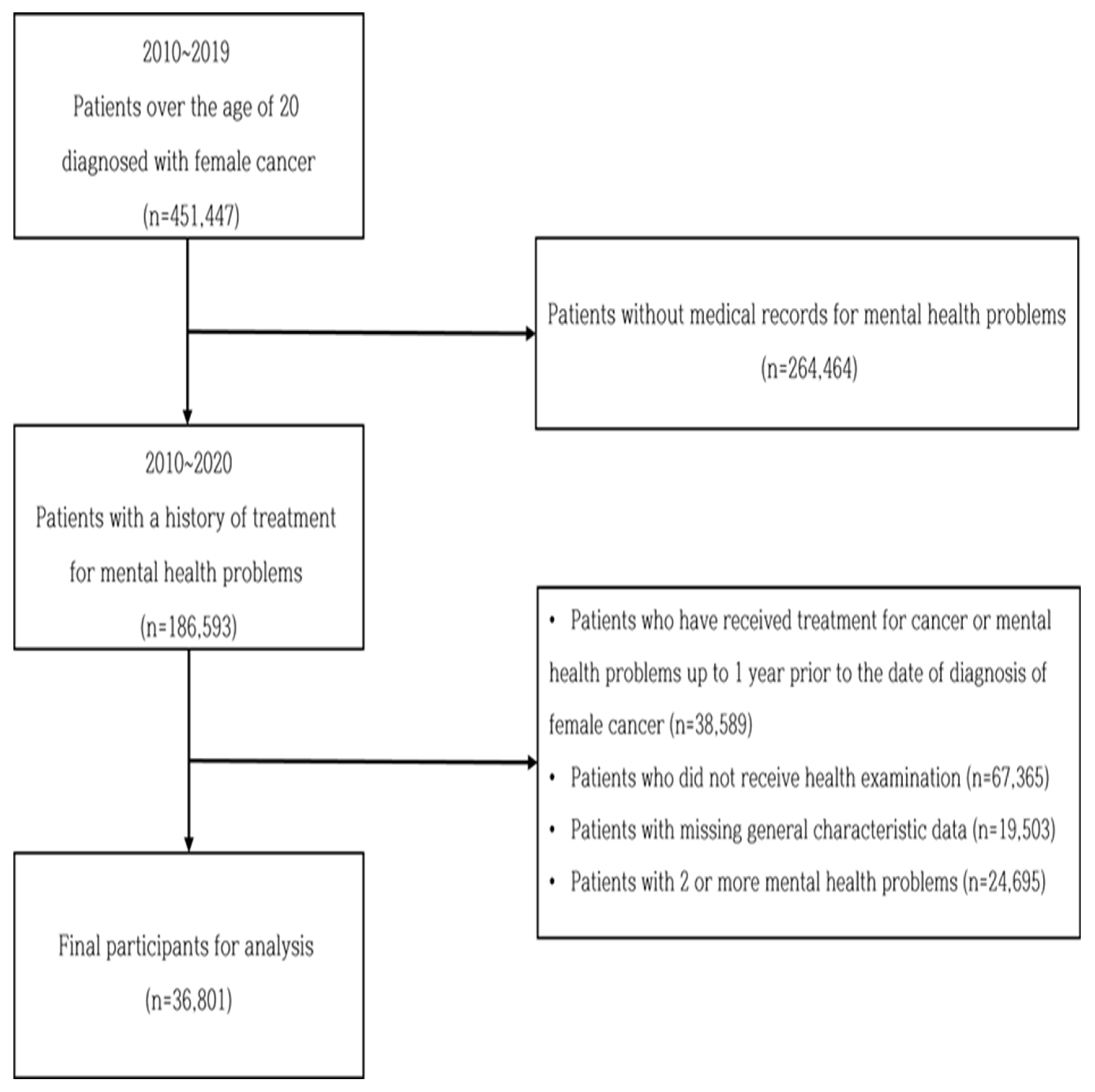
2.3. Study Participants and Data Collection Process
2.4. Measurement
2.4.1. General Characteristics
2.4.2. Survivorship Stage
2.4.3. Health-Related Behaviors
2.4.4. Study Outcome: Mental Health Case Ascertainment
2.5. Ethical Consideration
2.6. Statistical Analysis
3. Results
3.1. General Characteristics of Study Participants
3.2. Incidence Rate and Risk of Mental Health Problems According to Cancer Survivorship Stage and Health-Related Behavior
3.2.1. Incidence Rate of Mental Health Problems
3.2.2. Risk of Mental Health Problems
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Cancer Information Center. 2020 Cancer Statistics. Available online: https://www.cancer.go.kr/ (accessed on 1 April 2022).
- Song, E.A.; Kweon, Y.; Hwang, Y.Y.; An, M. Health-realted Quality of Life and Its related factors among cancer survivors and general adults: Focusing on lifestyle behaviors and mental health. Korean J. Adult Nurs. 2020, 32, 385–398. [Google Scholar] [CrossRef]
- Bergerot, C.D.; Clark, K.L.; Obenchain, R.; Philip, E.J.; Loscalzo, M. Breast and gynecological cancer patients risk factors associated with biopsychosocial problem-related distress. Psychooncology 2018, 27, 1013–1020. [Google Scholar] [CrossRef] [PubMed]
- Linden, W.; Vodermaier, A.; Mackenzie, R.; Greig, D. Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. J. Affect. Disord. 2012, 141, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Gotze, H.; Friedrich, M.; Taubenheim, S.; Dietz, A.; Lordick, F.; Mehnert, A. Depression and anxiety in long-term survivors 5 and 10 years after cancer diagnosis. Support. Care Cancer 2020, 28, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H. Update on distress management for cancer patients. J. Korean Med. Assoc. 2019, 62, 167–173. [Google Scholar] [CrossRef]
- Wang, Y.H.; Li, J.Q.; Shi, J.F.; Que, J.Y.; Liu, J.J.; Lappin, J.M.; Leung, J.; Ravindran, A.V.; Chen, W.Q.; Qiao, Y.L.; et al. Depression and anxiety in relation to cancer incidence and mortality: A systematic review and meta-analysis of cohort studies. Mol. Psychiatry 2020, 25, 1487–1499. [Google Scholar] [CrossRef]
- Walker, J.; Mulick, A.; Magill, N.; Symeonides, S.; Gourley, C.; Burke, K.; Belot, A.; Quartagno, M.; Niekerk, M.; Toynbee, M.; et al. Major depression and survival in people with cancer. Psychosom. Med. 2021, 85, 410–416. [Google Scholar] [CrossRef]
- Lee, E.S.; Park, J.S. The comparison of Health promotion behavior, post traumatic growth and quality of life according to stages of survivorship in patients with female genital neoplasm. Korean J. Adult Nurs. 2013, 25, 312–321. [Google Scholar] [CrossRef]
- Back, S.Y.; Choi, J.Y. A comparative study on the characteristics of cancer patients and cancer survivors. Asian Oncol. Nurs. 2018, 18, 11–20. [Google Scholar] [CrossRef]
- Tollosa, D.N.; Holliday, E.; Hure, A.; Tavener, M.; James, E.L. A 15-year follow-up study on long-term adherence to health behavior recommendations in women diagnosed with breast cancer. Breast Cancer Res. Treat. 2020, 182, 727–738. [Google Scholar] [CrossRef]
- International Agency for Research on Cancer (IARC). List of Classification by Cancer Sites with Sufficient or Limited Evidence in Human, IARC Monographys Volumes 1–130. Available online: https://monographs.iarc.who.int/agents-classified-by-the-iarc/ (accessed on 1 April 2022).
- Antwi, G.O.; Rhodes, D.L. Association between e-cigarette use and depression in US cancer survivors: A cross-sectional study. J. Cancer Surviv. 2022; Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Han, X.; Robison, L.A.; Jensen, R.E.; Smith, T.G.; Yabroff, K.R. Factors associated with health-related quality of life among cancer survivors in the united states. JNCI Cancer Spectrum. 2021, 5, pkaa123. [Google Scholar] [CrossRef] [PubMed]
- Meglio, A.D.; Gbenou, A.S.; Martin, E.; Pistilli, B.; Ligibel, J.A.; Crane, T.E.; Flaysakier, J.D.; Minvielle, E.; Vanlemmens, L.; Guenancia, C. Unhealthy behaviors after breast cancer: Capitalizing on a teachable moment to promote lifestyle lmprovements. Cancer 2021, 127, 2774–2787. [Google Scholar] [CrossRef] [PubMed]
- Kaul, S.; Avila, J.C.; Jupiter, D.; Rodriguez, A.M.; Kirchhoff, A.C.; Kuo, Y.F. Modifable health-related factors (smoking, physical activity and body mass index) and health care use and costs among adult cancer survivors. J. Cancer Res. Clin. Oncol. 2017, 143, 2469–2480. [Google Scholar] [CrossRef]
- Kim, H.J. Factors influencing quality of life among cancer survivors: Based on the korean national health and nutrition examination survey(KNHANES) for 2019. Korean J. Rehabil. Nurs. 2021, 42, 109–119. [Google Scholar]
- Cho, H.M.; Yoo, E.K. Effect of depression, family support on resilience in patients with gynecological cancer. J. Korea Soc. Wellness 2015, 10, 183–195. [Google Scholar]
- Carreira, H.; Williams, R.; Funston, G.; Stanway, S.; Bhaskaran, K. Associations between breast cancer survivorship and adverse mental health outcomes: A matched population-based cohort study in the United Kingdom. PLoS Med. 2021, 18, e1003504. [Google Scholar] [CrossRef]
- Cho, O.H.; Hwang, K.H. Association between sleep quality, anxiety and depression among Korean breast cancer survivors. Nurs. Open 2021, 8, 1030–1037. [Google Scholar] [CrossRef]
- Doege, D.; Thong, M.S.; Koch-Gallenkamp, L.; Jansen, L.; Bertram, H.; Eberle, A.; Holleczek, B.; Pritzkuleit, R.; Waldmann, A.; Zeissig, S.R.; et al. Age-specificprevalence and determinants of depression in long-term breast cancer survivors compared to female population controls. Cancer Med. 2020, 9, 8713–8721. [Google Scholar] [CrossRef]
- Lee, Y.H.; Han, K.D.; Ko, S.H.; Ko, K.S.; Lee, K.U. Data analytic process of a nationwide population-based study using national health information database established by National Health Insurance Service. Diabetes Metab. J. 2016, 40, 79–82. [Google Scholar] [CrossRef]
- Korean Society for the Study of Obesity. 2020 Korean Society for the Study of Obesity Guideline: Quick Reference Guideline. Available online: general.kosso.or.kr/html (accessed on 1 April 2022).
- The Korean Society of Lipid and Atherosclerosis. Korean Guidelines for the Management of Dyslipidemia, 4th ed. Available online: lipid.or.kr/indexm.php (accessed on 1 April 2022).
- Korean Diabetes Association. 2021 Clinical Practice Guidelines for Diabetes. Available online: www.diabetes.or.kr/bbs/?code=guide (accessed on 1 April 2022).
- Klapheke, A.K.; Keegan, T.; Ruskin, R.; Cress, R.D. Depressive symptoms and health-related quality of life in older woman with gynecologic cancers. J. Geriatr. Oncol. 2020, 11, 820–827. [Google Scholar] [CrossRef] [PubMed]
- Heo, J.; Chun, M.; Oh, Y.T.; Noh, O.K. Psychiatric comorbidities among endometrial cancer survivors in south korea: A nationwide population-based, longitudinal study. J. Gyneco. Oncol. 2019, 30, e15. [Google Scholar] [CrossRef] [PubMed]
- Endo, M.; Matsui, K.; Akaho, R.; Mitsui, K.; Yan, Y.; Lmai, Y.; Ueda, Y.; Muto, G.; Deshpande, G.A.; Terao, Y.; et al. Depressive and anxiety symptoms among Japanese cancer survivors: Japan Cancer survivorship research project. BMC Cancer 2022, 22, 134. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Lee, H.R. Comparison of distress and body image according to the stages of cancer survivorship in gynecological cancer patients. Asian Oncol. Nurs. 2014, 14, 15–22. [Google Scholar] [CrossRef] [Green Version]
- Boyes, A.W.; Girgis, A.; D’Este, C.A.; Zucca, A.C.; Lecathelinais, C.; Carey, M.L. Prevalence and Predictors of the Short-Term Trajectory of Anxiety and Depression in the First Year After a Cancer Diagnosis: A Population-Based Longitudinal Study. J. Clin. Oncol. 2013, 31, 2724–2729. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.H.; Choi, C.K.; Kim, H.Y.; Heo, Y.R.; Shin, M.H. Association between alcohol drinking status and depressive symptoms in Korean adults. Chonnam Med. J. 2021, 57, 68–75. [Google Scholar] [CrossRef]
- LI, J.; Wang, H.; Li, M.; Shen, Q.; Li, X.; Zhang, Y.; Peng, J.; Rong, X.; Peng, Y. Effect of alcohol use disorders and alcohol intake on the risk of subsequent depressive symptoms: A systematic review and meta-analysis of cohort studies. Addiction 2019, 115, 1224–1243. [Google Scholar] [CrossRef]
- Lazaris, R.S.; Folkman, S. Stress, Appraisal, and Coping, 1st ed.; Springer: New York, NY, USA, 1984. [Google Scholar]
- Park, S.M.; Han, M.A.; Park, J.; Ryu, S.Y.; Choi, S.W.; Shin, H.H.; Joo, M.H. Association between smoking, drinking and depression among Korean adults: The 5th Korea National Health and Nutrition Examination Survey. Korean J. Health Promot. 2016, 16, 111–118. [Google Scholar] [CrossRef] [Green Version]
- National Cancer Center. Cancer Survivors Health Care Guidelines, 1st ed. Available online: cancer.go.kr (accessed on 1 April 2022).
| Variable | Category | n | % | Mean ± SD | |
|---|---|---|---|---|---|
| Age (years) (at cancer diagnosis) | 56.6 ± 10.3 | ||||
| <30 | 126 | 0.3 | |||
| 30~39 | 1657 | 4.5 | |||
| 40~49 | 10,715 | 29.1 | |||
| 50~59 | 13,826 | 37.6 | |||
| 60~69 | 7615 | 20.7 | |||
| ≥70 | 2862 | 7.8 | |||
| Survival stage | Acute SS | 1198 | 3.3 | ||
| Extended SS | 7052 | 19.2 | |||
| Permanent SS | 28,551 | 77.6 | |||
| Cancer type | Breast | 27,464 | 74.6 | ||
| Cervical | 4873 | 13.2 | |||
| Ovarian | 2329 | 6.3 | |||
| Endometrial | 2135 | 5.8 | |||
| History | Diabetes | Yes | 3188 | 8.7 | |
| Hypertension | Yes | 8573 | 23.3 | ||
| Heart disease | Yes | 868 | 2.4 | ||
| Health-related behavior | Smoking | Nonsmoker | 35,012 | 95.1 | |
| Former smoker | 886 | 2.4 | |||
| Current smoker | 903 | 2.5 | |||
| Drinking | Nondrinker | 30,382 | 82.6 | ||
| Drinker | 6419 | 17.4 | |||
| Physical activity | Insufficient | 26,988 | 73.3 | ||
| Average or health-promoting | 9813 | 26.7 | |||
| BMI (Kg/m2) | <18.5 | 1155 | 3.1 | 23.8 ± 3.4 | |
| 18.5~22.9 | 15,397 | 41.8 | |||
| 23~24.9 | 8705 | 23.7 | |||
| 25~29.9 | 9899 | 26.9 | |||
| ≥30 | 1645 | 4.5 | |||
| Systolic BP (mmHg) | 121.4 ± 15.5 | ||||
| Diastolic BP (mmHg) | 74.9 ± 9.9 | ||||
| Fasting blood glucose (mg/dL) | <100 | 24,028 | 65.3 | ||
| 100~125 | 10,211 | 27.7 | |||
| ≥126 | 2562 | 7.0 | |||
| Total cholesterol (mg/dL) | <200 | 19,789 | 53.8 | ||
| 200~239 | 11,96 | 32.5 | |||
| ≥240 | 5048 | 13.7 | |||
| High-density lipoprotein (HDL) cholesterol (mg/dL) | <40 | 2726 | 7.4 | ||
| ≥40 | 34,075 | 92.6 | |||
| Low-density lipoprotein (LDL) cholesterol (mg/dL) | <130 | 24,567 | 66.8 | ||
| 130~159 | 8120 | 22.1 | |||
| ≥160 | 4114 | 11.2 | |||
| Triglycerides (mg/dL) | <150 | 28,128 | 76.4 | ||
| 150~199 | 4769 | 13.0 | |||
| ≥200 | 3904 | 10.6 | |||
| Variables | Participants (n) | Events (n) | Follow-Up Duration (Person-Years) | Incidence Rate (Per 1000 Person-Years) | Model 1 | Model 2 | Model 3 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | HR | 95% CI | p-Value | ||||||||||
| All Cause Anxiety Disorders | 36,801 | 14,698 | 15,402,585 | 0.95 | ||||||||||||||
| Cancer type | Breast | 27,464 | 10,689 | 10,500,933 | 1.02 | 1 (ref.) | 1 (ref.) | 1 (ref.) | ||||||||||
| Cervical | 4873 | 2280 | 2,932,235 | 0.78 | 1.09 | 1.04 | 1.14 | 0.00 | 1.09 | 1.04 | 1.14 | 0.00 | 1.08 | 1.03 | 1.13 | 0.00 | ||
| Ovarian | 2329 | 816 | 927,158 | 0.88 | 0.85 | 0.79 | 0.91 | <0.0001 | 0.85 | 0.79 | 0.91 | <0.0001 | 0.85 | 0.79 | 0.91 | <0.0001 | ||
| Endometrial | 2135 | 913 | 1042,259 | 0.88 | 1.06 | 0.99 | 1.13 | 0.10 | 1.06 | 0.99 | 1.13 | 0.10 | 1.06 | 0.99 | 1.14 | 0.09 | ||
| SS | Acute SS | 1198 | 276 | 49,907 | 5.53 | 1.42 | 1.26 | 1.60 | <0.0001 | 1.38 | 1.22 | 1.55 | <0.0001 | |||||
| Extended SS | 7052 | 1761 | 643,081 | 2.74 | 0.94 | 0.89 | 0.99 | 0.02 | 0.93 | 0.88 | 0.98 | 0.00 | ||||||
| Permanent SS | 28,551 | 12,661 | 14,709,597 | 0.86 | 1 (ref.) | 1 (ref.) | ||||||||||||
| Health -related behavior | Smoking | Nonsmoker | 35,012 | 14,121 | 14,845,414 | 0.95 | 1 (ref.) | 1 (ref.) | ||||||||||
| Former smoker | 886 | 296 | 305,749 | 0.97 | 0.86 | 0.77 | 0.97 | 0.01 | 0.86 | 0.77 | 0.97 | 0.01 | ||||||
| Current smoker | 903 | 281 | 251,422 | 1.12 | 0.80 | 0.71 | 0.90 | 0.00 | 0.80 | 0.71 | 0.90 | 0.00 | ||||||
| Drinking | Nondrinker | 30,382 | 12,451 | 13,060,663 | 0.95 | 1 (ref.) | 1 (ref.) | |||||||||||
| Drinker | 6419 | 2247 | 2,341,922 | 0.96 | 0.91 | 0.87 | 0.95 | <0.0001 | 0.91 | 0.87 | 0.96 | 0.00 | ||||||
| Physical activity | Average or health-promoting | 9813 | 3862 | 4,699,042 | 0.82 | 1 (ref.) | 1 (ref.) | |||||||||||
| Insufficient | 26,988 | 10,836 | 10,703,543 | 1.01 | 1.02 | 0.99 | 1.06 | 0.25 | 1.02 | 0.98 | 1.06 | 0.39 | ||||||
| Variables | Participant (n) | Events (n) | Follow-Up Duration (Person-Years) | Incidence Rate (Per 1000 Person-Years) | Model 1 (Unadjusted) | Model 2 | Model 3 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | HR | 95% CI | p-Value | ||||||||||
| All cause depressive disorders | 36,801 | 6168 | 5,703,419 | 1.08 | ||||||||||||||
| Cancer type | Breast | 27,464 | 4346 | 3,904,167 | 1.11 | 1 (ref.) | 1 (ref.) | 1 (ref.) | ||||||||||
| Cervical | 4873 | 911 | 1,038,435 | 0.88 | 1.14 | 1.06 | 1.22 | 0.00 | 1.04 | 0.97 | 1.12 | 0.26 | 1.14 | 1.06 | 1.23 | 0.00 | ||
| Ovarian | 2329 | 506 | 389,607 | 1.30 | 1.40 | 1.27 | 1.53 | <0.0001 | 1.40 | 1.28 | 1.54 | <0.0001 | 1.40 | 1.27 | 1.53 | <0.0001 | ||
| Endometrial | 2135 | 405 | 371,210 | 1.09 | 1.18 | 1.07 | 1.31 | 0.00 | 1.17 | 1.06 | 1.30 | 0.00 | 1.18 | 1.07 | 1.31 | 0.00 | ||
| SS | Acute SS | 1198 | 227 | 42,045 | 5.40 | 3.14 | 2.74 | 3.61 | <0.0001 | 2.99 | 2.60 | 3.42 | <0.0001 | |||||
| Extended SS | 7052 | 1394 | 393,356 | 3.54 | 2.16 | 2.02 | 2.30 | <0.0001 | 2.14 | 2.00 | 2.28 | <0.0001 | ||||||
| Permanent SS | 28,551 | 4547 | 5,268,018 | 0.86 | 1 (ref.) | |||||||||||||
| Health-related behavior | Smoking | Nonsmoker | 35,012 | 5822 | 5,444,966 | 1.07 | 1 (ref.) | 1 (ref.) | ||||||||||
| Former smoker | 886 | 178 | 145,752 | 1.22 | 1.25 | 1.08 | 1.46 | 0.00 | 1.32 | 1.14 | 1.54 | 0.00 | ||||||
| Current smoker | 903 | 168 | 112,701 | 1.49 | 1.17 | 1.01 | 1.37 | 0.04 | 1.21 | 1.04 | 1.41 | 0.02 | ||||||
| Drinking | Nondrinker | 30,382 | 5204 | 4,869,048 | 1.07 | 1 (ref.) | 1 (ref.) | |||||||||||
| Drinker | 6419 | 964 | 834,371 | 1.16 | 0.89 | 0.82 | 0.95 | 0.00 | 0.96 | 0.89 | 1.03 | 0.26 | ||||||
| Physical activity | Average or health-promoting | 9813 | 1500 | 1,590,097 | 0.94 | 1 (ref.) | 1 (ref.) | |||||||||||
| Insufficient | 26,988 | 4668 | 4,113,322 | 1.13 | 1.14 | 1.08 | 1.21 | <0.0001 | 1.09 | 1.02 | 1.15 | 0.01 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.Y.; Lee, Y.; Koh, S.B. Factors Affecting the Occurrence of Mental Health Problems in Female Cancer Survivors: A Nationwide Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 8615. https://doi.org/10.3390/ijerph19148615
Kim SY, Lee Y, Koh SB. Factors Affecting the Occurrence of Mental Health Problems in Female Cancer Survivors: A Nationwide Cohort Study. International Journal of Environmental Research and Public Health. 2022; 19(14):8615. https://doi.org/10.3390/ijerph19148615
Chicago/Turabian StyleKim, So Young, Yeonju Lee, and Sang Baek Koh. 2022. "Factors Affecting the Occurrence of Mental Health Problems in Female Cancer Survivors: A Nationwide Cohort Study" International Journal of Environmental Research and Public Health 19, no. 14: 8615. https://doi.org/10.3390/ijerph19148615
APA StyleKim, S. Y., Lee, Y., & Koh, S. B. (2022). Factors Affecting the Occurrence of Mental Health Problems in Female Cancer Survivors: A Nationwide Cohort Study. International Journal of Environmental Research and Public Health, 19(14), 8615. https://doi.org/10.3390/ijerph19148615







