Analysis of Attempted Suicide in a Pediatric Setting: Extracted Notes for Clinical Practice and Complexity of Help
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nock, M.K.; Green, J.G.; Hwang, I.; McLaughlin, K.A.; Sampson, N.A.; Zaslavsky, A.M.; Kessler, R.C. Prevalence, Correlates, and Treatment of Lifetime Suicidal Behavior among Adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry 2013, 70, 300–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eaton, D.K.; Kann, L.; Kinchen, S.; Shanklin, S.; Ross, J.; Hawkins, J.; Harris, W.A.; Lowry, R.; McManus, T.; Chyen, D.; et al. Youth Risk Behavior Surveillance—United States, 2007. MMWR Surveill. Summ. 2008, 57, 1–131. [Google Scholar] [PubMed]
- Lekečinskaitė, L.; Lesinskienė, S. Vaikų ir Jaunimo iki 20 M. Savižudybės Lietuvoje 2010–2015 M. Visuomenės Sveik. 2017, 2, 74–80. [Google Scholar]
- Hollis, C. Depression, Family Environment, and Adolescent Suicidal Behavior. J. Am. Acad. Child Adolesc. Psychiatry 1996, 35, 622–630. [Google Scholar] [CrossRef] [PubMed]
- Marttunen, M.J.; Aro, H.M.; Lönnqvist, J.K. Precipitant Stressors in Adolescent Suicide. J. Am. Acad. Child Adolesc. Psychiatry 1993, 32, 1178–1183. [Google Scholar] [CrossRef] [PubMed]
- Xing, X.-Y.; Tao, F.-B.; Wan, Y.-H.; Xing, C.; Qi, X.-Y.; Hao, J.-H.; Su, P.-Y.; Pan, H.-F.; Huang, L. Family Factors Associated with Suicide Attempts among Chinese Adolescent Students: A National Cross-Sectional Survey. J. Adolesc. Health 2010, 46, 592–599. [Google Scholar] [CrossRef]
- Grande, E.; Vichi, M.; Alicandro, G.; Simeoni, S.; Murianni, L.; Marchetti, S.; Zengarini, N.; Frova, L.; Pompili, M. Suicide among Adolescents in Italy: A Nationwide Cohort Study of the Role of Family Characteristics. Eur. Child. Adolesc. Psychiatry 2021, 30, 1037–1045. [Google Scholar] [CrossRef]
- Garnefski, N.; Diekstra, R.F.W. Adolescents from One Parent, Stepparent and Intact Families: Emotional Problems and Suicide Attempts. J. Adolesc. 1997, 20, 201–208. [Google Scholar] [CrossRef]
- Evans, R.; White, J.; Turley, R.; Slater, T.; Morgan, H.; Strange, H.; Scourfield, J. Comparison of Suicidal Ideation, Suicide Attempt and Suicide in Children and Young People in Care and Non-Care Populations: Systematic Review and Meta-Analysis of Prevalence. Child. Youth Serv. Rev. 2017, 82, 122–129. [Google Scholar] [CrossRef]
- Rafi Bazrafshan, M.; Sharif, F.; Molazem, Z.; Mani, A. The Effect of Paternal Addiction on Adolescent Suicide Attempts: A Qualitative Study. Int. J. High Risk Behav. Addict. 2016, 5, e22588. [Google Scholar] [CrossRef] [Green Version]
- Slesnick, N.; Feng, X.; Brakenhoff, B.; Brigham, G.S. Parenting under the Influence: The Effects of Opioids, Alcohol and Cocaine on Mother–Child Interaction. Addict. Behav. 2014, 39, 897–900. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.S.; Leventhal, B. Bullying and Suicide. A Review. Int. J. Adolesc. Med. Health 2008, 20, 133–154. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Leventhal, B.L.; Koh, Y.-J.; Boyce, W.T. Bullying Increased Suicide Risk: Prospective Study of Korean Adolescents. Arch. Suicide Res. 2009, 13, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Brunstein klomek, A.; Marrocco, F.; Kleinman, M.; Schonfeld, I.S.; Gould, M.S. Bullying, Depression, and Suicidality in Adolescents. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 40–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Litwiller, B.J.; Brausch, A.M. Cyber Bullying and Physical Bullying in Adolescent Suicide: The Role of Violent Behavior and Substance Use. J. Youth Adolesc. 2013, 42, 675–684. [Google Scholar] [CrossRef]
- Nock, M.K.; Joiner, T.E.; Gordon, K.H.; Lloyd-Richardson, E.; Prinstein, M.J. Non-Suicidal Self-Injury among Adolescents: Diagnostic Correlates and Relation to Suicide Attempts. Psychiatry Res. 2006, 144, 65–72. [Google Scholar] [CrossRef]
- Nanayakkara, S.; Misch, D.; Chang, L.; Henry, D. Depression and Exposure to Suicide Predict Suicide Attempt. Depress. Anxiety 2013, 30, 991–996. [Google Scholar] [CrossRef]
- Bearman, P.S.; Moody, J. Suicide and Friendships among American Adolescents. Am. J. Public Health 2004, 94, 89–95. [Google Scholar] [CrossRef]
- Lesinskiene, S.; Girdzijauskiene, S.; Gintiliene, G.; Butkiene, D.; Puras, D.; Goodman, R.; Heiervang, E. Epidemiological Study of Child and Adolescent Psychiatric Disorders in Lithuania. BMC Public Health 2018, 18, 548. [Google Scholar] [CrossRef] [Green Version]
- Shain, B.; Committee on Adolescence; Braverman, P.K.; Adelman, W.P.; Alderman, E.M.; Breuner, C.C.; Levine, D.A.; Marcell, A.V.; O’Brien, R.F. Suicide and Suicide Attempts in Adolescents. Pediatrics 2016, 138, e20161420. [Google Scholar] [CrossRef] [Green Version]
- Laido, Z.; Voracek, M.; Till, B.; Pietschnig, J.; Eisenwort, B.; Dervic, K.; Sonneck, G.; Niederkrotenthaler, T. Epidemiology of Suicide among Children and Adolescents in Austria, 2001–2014. Wien. Klin. Wochenschr. 2017, 129, 121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewinsohn, P.M.; Rohde, P.; Seeley, J.R.; Baldwin, C.L. Gender Differences in Suicide Attempts from Adolescence to Young Adulthood. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Bridge, J.A.; Asti, L.; Horowitz, L.M.; Greenhouse, J.B.; Fontanella, C.A.; Sheftall, A.H.; Kelleher, K.J.; Campo, J.V. Suicide Trends among Elementary School-Aged Children in the United States from 1993 to 2012. JAMA Pediatr. 2015, 169, 673–677. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hawton, K.; James, A. Suicide and Deliberate Self Harm in Young People. BMJ 2005, 330, 891–894. [Google Scholar] [CrossRef] [Green Version]
- Darré, T.; Consuela, K.A.C.; Saka, B.; Djiwa, T.; Ekouévi, K.D.; Napo-Koura, G. Suicidal Ideation and Suicide Attempts in Subjects Aged 15-19 in Lomé (Togo). BMC Res. Notes 2019, 12, 187. [Google Scholar] [CrossRef]
- Coimbra, D.G.; Pereira E Silva, A.C.; de Sousa-Rodrigues, C.F.; Barbosa, F.T.; de Siqueira Figueredo, D.; Araújo Santos, J.L.; Barbosa, M.R.; de Medeiros Alves, V.; Nardi, A.E.; de Andrade, T.G. Do Suicide Attempts Occur More Frequently in the Spring Too? A Systematic Review and Rhythmic Analysis. J. Affect. Disord. 2016, 196, 125–137. [Google Scholar] [CrossRef]
- Ajdacic-Gross, V.; Wang, J.; Bopp, M.; Eich, D.; Rössler, W.; Gutzwiller, F. Are Seasonalities in Suicide Dependent on Suicide Methods? A Reappraisal. Soc. Sci. Med. 2003. [Google Scholar] [CrossRef]
- Geoffroy, P.A.; Bellivier, F.; Scott, J.; Etain, B. Seasonality and Bipolar Disorder: A Systematic Review, from Admission Rates to Seasonality of Symptoms. J. Affect. Disord 2014, 168, 210–223. [Google Scholar] [CrossRef]
- Vyssoki, B.; Praschak-Rieder, N.; Sonneck, G.; Blüml, V.; Willeit, M.; Kasper, S.; Kapusta, N.D. Effects of Sunshine on Suicide Rates. Compr. Psychiatry 2012, 53, 535–539. [Google Scholar] [CrossRef]
- Grudet, C.; Malm, J.; Westrin, A.; Brundin, L. Suicidal Patients Are Deficient in Vitamin D, Associated with a pro-Inflammatory Status in the Blood. Psychoneuroendocrinology 2014, 50, 210–219. [Google Scholar] [CrossRef] [Green Version]
- Giraud, P.; Fortanier, C.; Fabre, G.; Ghariani, J.; Guillermain, Y.; Rouviere, N.; Chabrol, B.; Jouve, J.-L.; Simeoni, M.-C. [Suicide attempts by young adolescents: Epidemiological characteristics of 517 15-year-old or younger adolescents admitted in French emergency departments]. Arch. Pediatr. 2013, 20, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Holt, M.K.; Vivolo-Kantor, A.M.; Polanin, J.R.; Holland, K.M.; DeGue, S.; Matjasko, J.L.; Wolfe, M.; Reid, G. Bullying and Suicidal Ideation and Behaviors: A Meta-Analysis. Pediatrics 2015, 135, e496–e509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaffney, H.; Ttofi, M.M.; Farrington, D.P. Evaluating the Effectiveness of School-Bullying Prevention Programs: An Updated Meta-Analytical Review. Aggress. Violent Behav. 2019, 45, 111–133. [Google Scholar] [CrossRef]
- Cantone, E.; Piras, A.P.; Vellante, M.; Preti, A.; Daníelsdóttir, S.; D’Aloja, E.; Lesinskiene, S.; Angermeyer, M.C.; Carta, M.G.; Bhugra, D. Interventions on Bullying and Cyberbullying in Schools: A Systematic Review. Clin. Pract. Epidemiol. Ment. Health CP EMH 2015, 11, 58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laskyte, A.; Zemaitiene, N. [The types of deliberate self-harm and its prevalence among Lithuanian teenagers]. Medicina 2009, 45, 132–139. [Google Scholar] [CrossRef] [Green Version]
- Muehlenkamp, J.J.; Gutierrez, P.M. An Investigation of Differences between Self-Injurious Behavior and Suicide Attempts in a Sample of Adolescents. Suicide Life Threat. Behav. 2004, 34, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Brausch, A.M.; Muehlenkamp, J.J. Body Image and Suicidal Ideation in Adolescents. Body Image 2007, 4, 207–212. [Google Scholar] [CrossRef]
- Ross, S.; Heath, N. A Study of the Frequency of Self-Mutilation in a Community Sample of Adolescents. J. Youth Adolesc. 2002, 31, 67–77. [Google Scholar] [CrossRef] [Green Version]
- Brown, R.C.; Plener, P.L. Non-Suicidal Self-Injury in Adolescence. Curr. Psychiatry Rep. 2017, 19, 20. [Google Scholar] [CrossRef] [Green Version]
- Lauw, M.; How, C.H.; Loh, C. Deliberate Self-Harm in Adolescents. Singapore Med. J. 2015, 56, 306–309. [Google Scholar] [CrossRef] [Green Version]
- Favaro, A.; Santonastaso, P. Impulsive and Compulsive Self-Injurious Behavior in Bulimia Nervosa: Prevalence and Psychological Correlates. J. Nerv. Ment. Dis. 1998, 186, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Darche, M.A. Psychological Factors Differentiating Self-Mutilating and Non-Self-Mutilating Adolescent Inpatient Females. Psychiatr. Hosp. 1990, 21, 31–35. [Google Scholar]
- Tang, J.; Ma, Y.; Guo, Y.; Ahmed, N.I.; Yu, Y.; Wang, J. Association of Aggression and Non-Suicidal Self Injury: A School-Based Sample of Adolescents. PLoS ONE 2013, 8, e78149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwenck, C.; Christiansen, H.; Goetz, M. Children of Parents with Mental Illness (COPMI). In: The JM REY’S IACAPAP e-Textbook of Child and Adolescent Mental Health. p. 2. Available online: https://iacapap.org/content/uploads/J.13-COPMI-2020.pdf (accessed on 23 August 2021).
- Belfer, M.L. Child and Adolescent Mental Disorders: The Magnitude of the Problem across the Globe. J. Child Psychol. Psychiatry 2008, 49, 226–236. [Google Scholar] [CrossRef] [PubMed]
- Remschmidt, H.; Belfer, M. Mental Health Care for Children and Adolescents Worldwide: A Review. World Psychiatry 2005, 4, 147–153. [Google Scholar]
- Mann, J.J.; Michel, C.A.; Auerbach, R.P. Improving Suicide Prevention Through Evidence-Based Strategies: A Systematic Review. AJP 2021, 178, 611–624. [Google Scholar] [CrossRef]
- Doupnik, S.K.; Rudd, B.; Schmutte, T.; Worsley, D.; Bowden, C.F.; McCarthy, E.; Eggan, E.; Bridge, J.A.; Marcus, S.C. Association of Suicide Prevention Interventions with Subsequent Suicide Attempts, Linkage to Follow-up Care, and Depression Symptoms for Acute Care Settings: A Systematic Review and Meta-Analysis. JAMA Psychiatry 2020, 77, 1021–1030. [Google Scholar] [CrossRef]
- Mo, P.K.H.; Ko, T.T.; Xin, M.Q. School-Based Gatekeeper Training Programmes in Enhancing Gatekeepers’ Cognitions and Behaviours for Adolescent Suicide Prevention: A Systematic Review. Child Adolesc. Psychiatry Ment. Health 2018, 12, 29. [Google Scholar] [CrossRef]
- Grunau, M. Suicide Prevention Involves All of Us, Together. Can. J. Psychiatry 2017, 62, 295. [Google Scholar] [CrossRef]
- Olin, S.S.; Hoagwood, K.E.; Rodriguez, J.; Ramos, B.; Burton, G.; Penn, M.; Crowe, M.; Radigan, M.; Jensen, P.S. The Application of Behavior Change Theory to Family-Based Services: Improving Parent Empowerment in Children’s Mental Health. J. Child Fam. Stud. 2010, 19, 462–470. [Google Scholar] [CrossRef] [Green Version]
- Moskos, M.A.; Olson, L.; Halbern, S.R.; Gray, D. Utah Youth Suicide Study: Barriers to Mental Health Treatment for Adolescents. Suicide Life-Threat. Behav. 2007, 37, 179–186. [Google Scholar] [CrossRef]
- Ranahan, P. Mental Health Literacy: A Conceptual Framework for Future Inquiry into Child and Youth Care Professionals’ Practice with Suicidal Adolescents. Child Youth Care Forum 2010, 39, 11–25. [Google Scholar] [CrossRef]
- Sanchez, L.E.; Le, L.T. Suicide in Mood Disorders. Depress. Anxiety 2001, 14, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Rowan, A.B. Adolescent Substance Abuse and Suicide. Depress. Anxiety 2001, 14, 186–191. [Google Scholar] [CrossRef] [PubMed]
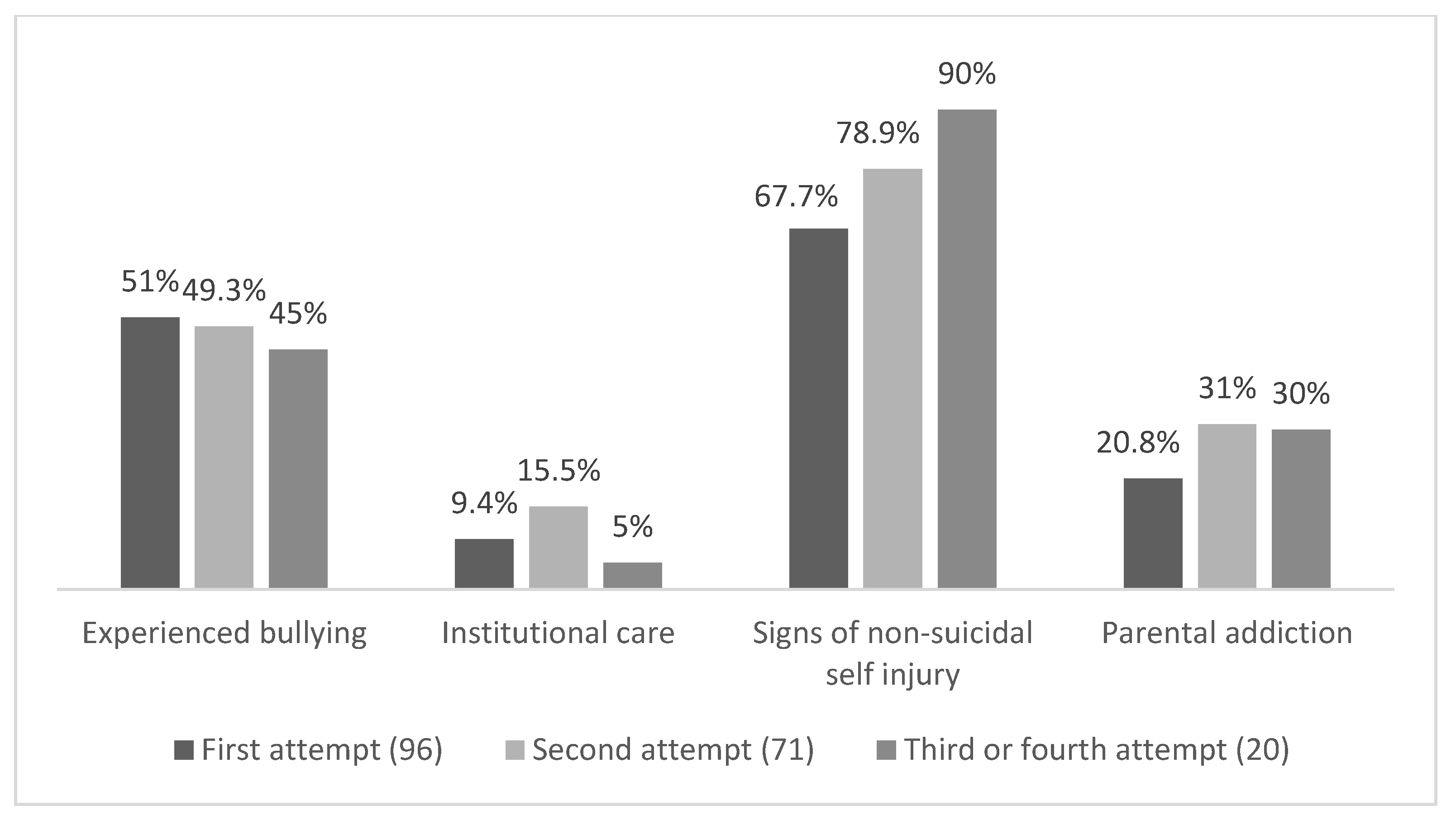
| First Suicide Attempt (96 (51.3%)) | Previous History of Suicide Attempt * (91 (48.7%)) | p Value | |
|---|---|---|---|
| Experienced bullying | 51.0 | 48.4 | 0.713 |
| Institutional care | 9.4 | 13.2 | 0.409 |
| Signs of non-suicidal self-injury | 67.7 | 81.3 | 0.033 |
| Parental addiction | 20.8 | 30.8 | 0.120 |
| Suicide in close surroundings | 21.9 | 11.0 | 0.045 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lesinskienė, S.; Kinčinienė, O.; Šambaras, R.; Žilinskas, E. Analysis of Attempted Suicide in a Pediatric Setting: Extracted Notes for Clinical Practice and Complexity of Help. Int. J. Environ. Res. Public Health 2022, 19, 8604. https://doi.org/10.3390/ijerph19148604
Lesinskienė S, Kinčinienė O, Šambaras R, Žilinskas E. Analysis of Attempted Suicide in a Pediatric Setting: Extracted Notes for Clinical Practice and Complexity of Help. International Journal of Environmental Research and Public Health. 2022; 19(14):8604. https://doi.org/10.3390/ijerph19148604
Chicago/Turabian StyleLesinskienė, Sigita, Odeta Kinčinienė, Rokas Šambaras, and Emilijus Žilinskas. 2022. "Analysis of Attempted Suicide in a Pediatric Setting: Extracted Notes for Clinical Practice and Complexity of Help" International Journal of Environmental Research and Public Health 19, no. 14: 8604. https://doi.org/10.3390/ijerph19148604
APA StyleLesinskienė, S., Kinčinienė, O., Šambaras, R., & Žilinskas, E. (2022). Analysis of Attempted Suicide in a Pediatric Setting: Extracted Notes for Clinical Practice and Complexity of Help. International Journal of Environmental Research and Public Health, 19(14), 8604. https://doi.org/10.3390/ijerph19148604





