A New Health Promotion Program That Includes Wadaiko Rhythm Exercise to Maintain the Health of Persons Excluded from Receiving Specific Health Guidance
Abstract
:1. Introduction
2. Materials and Methods
2.1. Outline of the Town Surveyed and Selection of Participants
2.2. Structure of Health Promotion Program
2.3. Evaluation Items and Data Collection
2.4. Design of the Intervention Program
2.5. Statistical Analysis
3. Results
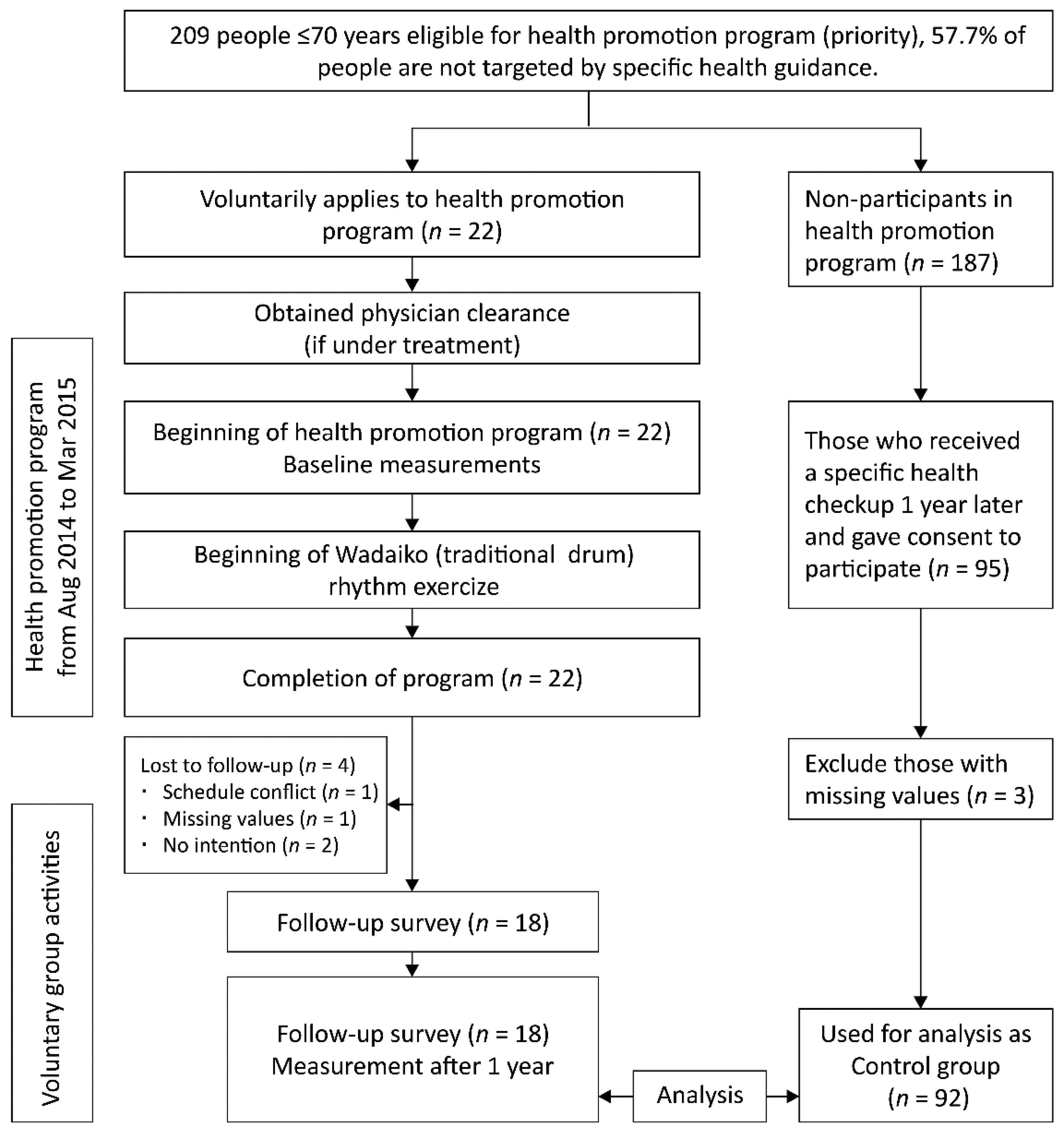
3.1. Workflow of Our Research
3.2. Baseline Measurements
3.3. Changes in Blood Measurements
3.4. The Influential Factors of Change
3.5. Impressions of the Wadaiko Rhythm Exercise
4. Discussion
4.1. Influential Elements in the Health Promotion Program
4.2. Decrease in LDL-C without Specific Influential Factors
4.3. HbA1c among Antihyperglycemic Drug Users
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Health, Labor and Welfare. Reference Materials for Promoting Health Japan 21 (The Second Term). Available online: http://www.mhlw.go.jp/bunya/kenkou/dl/kenkounippon21_02.pdf (accessed on 30 June 2021). (In Japanese)
- Specified Non-Profit Organization Japan Health Education Organization. New Health Education: The Road to Health Promotion Learned from Theory and Case; HOKENDOHJIN: Tokyo, Japan, 2013; pp. 12–45. (In Japanese) [Google Scholar]
- Ministry of Health, Labor and Welfare. Standard Specific Health Checkups/Health Guidance Program. Available online: https://www.mhlw.go.jp/seisakunitsuite/bunya/kenkou_iryou/kenkou/seikatsu/dl/hoken-program2.pdf (accessed on 30 June 2021).
- Lee, S.C.; Hairi, N.N.; Moy, F.M. Metabolic Syndrome Among Non-Obese Adults in the Teaching Profession in Melaka, Malaysia. J. Epidemiol. 2017, 27, 130–134. [Google Scholar] [CrossRef]
- Ohashi, Y.; Shimamoto, K.; Sato, S.; Iso, H.; Kita, Y.; Kitamura, A.; Saito, I.; Kiyohara, Y.; Kawano, H.; Nakagawa, H.; et al. Association of Obesity and Other Cardiovascular Risk Factors with Stroke: The Japan Arteriosclerosis Longitudinal Study-Existing Cohorts Combined (JALS-ECC). Nihon Koshu Eisei Zasshi. 2011, 58, 1007–1015. [Google Scholar]
- Ijzelenberg, W.; Hellemans, I.M.; van Tulder, M.W.; Heymans, M.W.; Rauwerda, J.A.; van Rossum, A.C.; Seidell, J.C. The Effect of a Comprehensive Lifestyle Intervention on Cardiovascular Risk Factors in Pharmacologically Treated Patients with Stable Cardiovascular Disease Compared to Usual Care: A Randomised Controlled Trial. BMC Cardiovasc. Disord. 2012, 12, 71. [Google Scholar] [CrossRef] [Green Version]
- Kimura, A.; Fukuda, H.; Haniu, T.; Oka, F.; Ooike, M.; Haruyama, Y. Efficacy of Exercise Class at a Community Clinic for Middle-Aged and Elderly Patients with Lifestyle-Related Diseases Treated at the Clinic. Jpn. J. Health Hum. Ecol. 2010, 76, 195–206. [Google Scholar] [CrossRef] [Green Version]
- Kelley, G.A.; Kelley, K.S.; Tran, Z.V. Aerobic Exercise and Lipids and Lipoproteins in Women: A Meta-Analysis of Randomized Controlled Trials. J. Womens Health 2004, 13, 1148–1164. [Google Scholar] [CrossRef] [Green Version]
- Kelley, G.A.; Kelley, K.S. Aerobic Exercise and Lipids and Lipoproteins in Men: A Meta-Analysis of Randomized Controlled Trials. J. Mens Health Gend. 2006, 3, 61–70. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Kim, D.; Kim, C. Resistance Training for Glycemic Control, Muscular Strength, and Lean Body Mass in Old type 2 Diabetic Patients: A Meta-Analysis. Diabetes Ther. 2017, 8, 459–473. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health, Labor and Welfare. The National Health and Nutrition Survey in Japan. 2015. Available online: http://www.mhlw.go.jp/bunya/kenkou/eiyou/dl/h27-houkoku.pdf (accessed on 30 June 2021).
- Kanamori, S.; Kai, Y.; Aida, J.; Kondo, K.; Kawachi, I.; Hirai, H.; Shirai, K.; Ishikawa, Y.; Suzuki, K.; The JAGES Group. Social Participation and the Prevention of Functional Disability in Older Japanese: The JAGES Cohort Study. PLoS ONE 2014, 9, e99638. [Google Scholar] [CrossRef]
- Kanamori, S.; Kai, Y.; Kondo, K.; Hirai, H.; Ichida, Y.; Suzuki, K.; Kawachi, I. Participation in Sports Organizations and the Prevention of Functional Disability in Older Japanese: The AGES Cohort Study. PLoS ONE 2012, 7, e51061. [Google Scholar] [CrossRef]
- Shigematsu, R.; Nakanishi, R.; Saitoh, M.; Okura, T.; Nakagaichi, M.; Nakata, Y.; Sakai, T.; Nakamura, Y.; Kurimoto, M.; Tanaka, K. Reasons for Older Adults Independently Continuing Exercise After a Supervised Square-Stepping Exercise Intervention. Nihon Koshu Eisei Zasshi. 2011, 58, 22–29. [Google Scholar]
- Gjestvang, C.; Abrahamsen, F.; Stensrud, T.; Haakstad, L.A.H.; Haakstad, L. Motives and Barriers to Initiation and Sustained Exercise Adherence in a Fitness Club Setting-A One-Year Follow-Up Study. Scand. J. Med. Sci. Sports 2020, 30, 1796–1805. [Google Scholar] [CrossRef]
- Kobayashi, R.; Shirahama, K.; Moriyama, H.; Kanemura, N. The Effects of the Functional Training Program Using Japanese Drum in Public Health Center on the Stress and Sleep Condition. Jpn. J. Occup. Med. Traumatol. 2006, 54, 25–28. [Google Scholar]
- Mizuno, E.; Sakuma, H. Wadaiko Performance Enhances Synchronized Motion of Mentally Disabled Persons. Percept. Mot. Ski. 2013, 116, 187–196. [Google Scholar] [CrossRef]
- Nakao, S.; Takata, S.; Komatsu, K.; Tanaka, T.; Tamura, E.; Kashihara, M.; Osawa, T.; Masuda, Y.; Nishikawa, K.; Yamada, M.; et al. Three Dimensional Motion Analyses for Rehabilitation Version of Awa Odori Exercise and the Expectancy of Physical Effects. J. Med. Invest. 2011, 58, 259–263. [Google Scholar] [CrossRef] [Green Version]
- Haruyama, Y.; Muto, T.; Nakate, M.; Yamasaki, A.; Tarumi, F. Changes in measurements related to metabolic syndrome among individuals with national health insurance after specific health guidance. Nihon Koshu Eisei Zasshi Jpn. J. Public Health 2012, 59, 731–742. [Google Scholar]
- Prefecture Hiroshima. Population Aging Rate by City Town (as of 2021.1.1). Available online: https://www.pref.hiroshima.lg.jp/soshiki/64/koureikaritsu.html (accessed on 30 June 2021). (In Japanese).
- Ministry of Health, Labor and Welfare. Standards for Physical Activities for Health Promotion 2013. Available online: http://www.mhlw.go.jp/stf/houdou/2r9852000002xple-att/2r9852000002xpqt.pdf (accessed on 30 June 2021).
- Kanda, Y. Investigation of the Freely Available Easy-to-Use Software “EZR” for Medical Statistics. Bone Marrow Transpl. 2013, 48, 452–458. [Google Scholar] [CrossRef] [Green Version]
- Ebrahim, S.; Thompson, P.W.; Baskaran, V.; Evans, K. Randomized Placebo-Controlled Trial of Brisk Walking in the Prevention of Postmenopausal Osteoporosis. Age Ageing 1997, 26, 253–260. [Google Scholar] [CrossRef] [Green Version]
- Inoue, S. Urban Walkability and Lifestyle Related Diseases. J. Liveable City Stud. 2011, 2, 39–50. Available online: https://repository.kulib.kyoto-u.ac.jp/dspace/handle/2433/192402 (accessed on 30 June 2021). (In Japanese).
- Cabinet Office. Awareness Survey on Daily Life of Elderly (Summary Version). 2014. Available online: https://www8.cao.go.jp/kourei/ishiki/h26/sougou/zentai/index.html (accessed on 30 June 2021). (In Japanese)
- Winkelman, M. Complementary Therapy for Addiction: “Drumming Out Drugs”. Am. J. Public Health 2003, 93, 647–651. [Google Scholar] [CrossRef]
- Hopstock, L.A.; Deraas, T.S.; Henriksen, A.; Martiny-Huenger, T.; Grimsgaard, S. Changes in adiposity, physical activity, cardiometabolic risk factors, diet, physical capacity and well-being in inactive women and men aged 57–74 years with obesity and cardiovascular risk–A 6-month complex lifestyle intervention with 6-month follow-up. PLoS ONE 2021, 16, e0256631. [Google Scholar] [CrossRef]
- Calder, A.J.; Hargreaves, E.A.; Hodge, K. Great Expectations: A Qualitative Analysis of the Factors That Influence Affective Forecasts for Exercise. Int. J. Environ. Res. Public Health 2020, 17, 551. [Google Scholar] [CrossRef] [Green Version]
- Friedrich, M.; Goluch-Koniuszy, Z. The Effectiveness of Nutritional Education Among Women Aged 60–85 on the Basis of Anthropometric Parameters and Lipid Profiles. Rocz. Panstw. Zakl. Hig. 2017, 68, 253–260. [Google Scholar]
- Kamran, A.; Sharifirad, G.; Heydari, H.; Sharifian, E. The Effect of Theory Based Nutritional Education on Fat Intake, Weight and Blood Lipids. Electron. Physician. 2016, 8, 3333–3342. [Google Scholar] [CrossRef] [Green Version]
- Velázquez-López, L.; Muñoz-Torres, A.V.; Medina-Bravo, P.; Vilchis-Gil, J.; Klϋnder-Klϋnder, M.; Escobedo-de la Peña, J. Multimedia Education Program and Nutrition Therapy Improves HbA1C, Weight, and Lipid Profile of Patients with type 2 Diabetes: A Randomized Clinical Trial. Endocrine 2017, 58, 236–245. [Google Scholar] [CrossRef]
- Aubin, M.; Godin, G.; Vézina, L.; Maziade, J.; Desharnais, R. Hypercholesterolemia Screening: Does Knowledge of Blood Cholesterol Level Affect Dietary Fat Intake? Can. Fam. Physician 1998, 44, 1289–1297. [Google Scholar]
- Hartley, L.; May, M.D.; Loveman, E.; Colquitt, J.L.; Rees, K. Dietary Fibre for the Primary Prevention of Cardiovascular Disease. Cochrane Database Syst. Rev. 2016, 1, CD011472. [Google Scholar] [CrossRef]
- Lattimer, J.M.; Haub, M.D. Effects of Dietary Fiber and Its Components on Metabolic Health. Nutrients 2010, 2, 1266–1289. [Google Scholar] [CrossRef] [Green Version]
- Chen, H.S.; Jap, T.S.; Chen, R.L.; Lin, H.D. A Prospective Study of Glycemic Control During Holiday Time in Type 2 Diabetic Patients. Diabetes Care. 2004, 27, 326–330. [Google Scholar] [CrossRef] [Green Version]
- Otaki, N.; Yokoro, M.; Yano, M.; Imamura, T.; Akita, M.; Tanino, N.; Fukuo, K. Social contact impacts physical activity and sedentary behavior among older adults in Japan due to COVID-19. BMC Geriatr. 2022, 22, 491. [Google Scholar] [CrossRef]
- Seifert, A.; Hassler, B. Impact of the COVID-19 Pandemic on Loneliness Among Older Adults. Front Sociol. 2020, 5, 590935. [Google Scholar] [CrossRef]
- Cohen-Mansfield, J.; Muff, A.; Meschiany, G.; Lev-Ari, S. Adequacy of Web-Based Activities as a Substitute for In-Person Activities for Older Persons During the COVID-19 Pandemic: Survey Study. J. Med. Internet Res. 2021, 23, e25848. [Google Scholar] [CrossRef]
| Characteristic | Intervention Group (n = 18) | Control Group (n = 92) | p Value |
|---|---|---|---|
| Age, years (SD) | 65.2 (3.4) | 64.1 (4.5) | 0.39 |
| Sex, female, n (%) | 16 (88.9) | 59 (64.1) | 0.05 |
| Body mass index, kg/cm2 (SD) | 23.6 (3.6) | 22.1 (2.6) | 0.21 |
| TG, mg/dL (SD) | 112.6 (39.4) | 105.2 (48.6) | 0.21 |
| HDL-C, mg/dL (SD) | 64.8 (14.3) | 66.1 (15.5) | 0.75 |
| LDL-C, mg/dL (SD) | 140.8 (30.5) | 131.9 (29.5) | 0.24 |
| HbA1c, % (SD) | 5.87 (0.40) | 5.61 (0.46) | <0.01 |
| Anti-hypertensive drugs, n (%) a | 8 (44.4) | 24 (26.1) | 0.16 |
| Insulin injections or antihyperglycemic drugs, n (%) a | 4 (22.2) | 5 (5.4) | 0.04 |
| Cholesterol-reducing drugs, n (%) a | 8 (44.4) | 28 (30.4) | 0.28 |
| History of stroke, n (%) | 0 (0.0) | 3 (3.3) | 1 |
| History of heart disease, n (%) | 2 (11.1) | 3 (3.3) | 0.19 |
| History of chronic kidney failure, n (%) | 0 (0.0) | 0 (0.0) | — |
| History of smoking, n (%) | 3 (16.7) | 31 (33.7) | 0.18 |
| Exercise habits, n (%) b | 9 (50.0) | 34 (37.0) | 0.31 |
| Baseline | 1 Year | p Value | 95% CI | |||
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Intervention group (n = 18) | TG, mg/dL (SD) | 112.61 (39.38) | 88.11 (28.47) | 0.02 * | −44.73 | −4.27 |
| 111.5 (91.25–121.25) | 86.0 (68.75–112.5) | 0.02 * | ||||
| HDL-C, mg/dL (SD) | 64.83 (14.31) | 70.89 (14.66) | <0.01 ** | 2.46 | 9.65 | |
| 60.5 (56.25–75.50) | 70 (64.00–78.25) | <0.01 ** | ||||
| LDL-C, mg/dL (SD) | 140.83 (30.46) | 129.06 (29.71) | 0.13 | −27.38 | 3.82 | |
| 140.5 (127–157.5) | 130.5 (111.50–141.75) | 0.21 | ||||
| HbA1c, % (SD) | 5.87 (0.40) | 5.82 (0.46) | 0.41 | −0.19 | 0.08 | |
| 5.8 (5.650–5.975) | 5.75 (5.5–5.800) | 0.07 | ||||
| Control group (n = 92) | TG, mg/dL (SD) | 105.17 (48.60) | 106.25 (50.76) | 0.80 | −7.22 | 9.38 |
| 93.0 (72.00–129.75) | 95.5 (70.50–129.0) | 0.97 | ||||
| HDL-C, mg/dL (SD) | 66.12 (15.47) | 64.41 (15.85) | 0.02 * | −3.19 | −0.22 | |
| 66.0 (55.75–74.25) | 61 (53.75–74.00) | 0.045 | ||||
| LDL-C, mg/dL (SD) | 131.86 (29.54) | 128.02 (27.79) | 0.07 | −7.98 | 0.31 | |
| 133.0 (110–152.0) | 128.5 (109.75–145.00) | 0.10 | ||||
| HbA1c, % (SD) | 5.61 (0.46) | 5.57 (0.51) | 0.06 | −0.07 | 0.00 | |
| 5.6 (5.375–5.800) | 5.60 (5.3–5.725) | 0.04 * | ||||
| Intervention Group (n = 18) | Control Group (n = 92) | p Value | 95% CI | ||
|---|---|---|---|---|---|
| LL | UL | ||||
| TG, mg/dL (SD) | −24.50 (40.68) | 1.08 (40.08) | 0.02 * | −46.10 | −5.05 |
| −28.5 (−41–9.5) | 0.0 (−24–20.5) | 0.03 * | |||
| HDL-C, mg/dL (SD) | 6.06 (7.23) | −1.71 (7.16) | <0.01 ** | 4.10 | 11.42 |
| 5.5 (1.75–10.75) | −1.0 (−6.00–3.00) | <0.01 ** | |||
| LDL-C, mg/dL (SD) | −11.78 (31.37) | −3.84 (20.00) | 0.17 | −19.27 | 3.39 |
| −5.5 (−15.50–7.75) | −2.0 (−13.25–5.50) | 0.63 | |||
| HbA1c, %; (SD) | −0.06 (0.28) | −0.04 (0.18) | 0.70 | −0.120 | 0.081 |
| −0.1 (−0.2–0.0) | 0.0 (−0.1–0.1) | 0.18 | |||
| Variable | TG | HDL-C | LDL-C | HbA1c | ||||
|---|---|---|---|---|---|---|---|---|
| Estimate | p Value | Estimate | p Value | Estimate | p Value | Estimate | p Value | |
| (Intercept) | 131.810 | 0.044 * | 5.583 | 0.649 | 27.598 | 0.462 | 0.074 | 0.819 |
| Sex | 2.518 | 0.860 | −2.786 | 0.302 | 4.878 | 0.553 | −0.068 | 0.338 |
| Age | −1.517 | 0.093 | 0.020 | 0.905 | −0.603 | 0.245 | −0.001 | 0.902 |
| Body mass index | −2.172 | 0.166 | −0.264 | 0.373 | −0.142 | 0.875 | 0.000 | 0.985 |
| Exercise habits | 8.646 | 0.268 | −0.473 | 0.748 | 5.637 | 0.211 | −0.007 | 0.865 |
| Health promotion program | −22.652 | 0.040 * | 8.038 | <0.001 *** | −7.784 | 0.217 | −0.027 | 0.618 |
| Former smokers | 23.596 | 0.103 | −3.005 | 0.270 | 8.844 | 0.288 | −0.032 | 0.661 |
| Smokers | 20.572 | 0.303 | −4.414 | 0.243 | 13.884 | 0.229 | −0.049 | 0.625 |
| Cholesterol-reducing drugs | 8.511 | 0.339 | 0.319 | 0.849 | 4.750 | 0.355 | −0.020 | 0.647 |
| Anti-hypertensive drugs | −7.491 | 0.431 | 0.899 | 0.616 | 1.205 | 0.826 | −0.069 | 0.147 |
| Insulin injection or antihyperglycemic drugs | 25.318 | 0.090 | 0.045 | 0.987 | −0.892 | 0.917 | 0.208 | 0.006 ** |
| Multiple R-squared | 0.18 | 0.164 | 0.070 | 0.097 | ||||
| Adjusted R-squared | 0.097 | 0.080 | −0.024 | 0.006 | ||||
| F-statistic | 2.168 on 10 and 99 DF | 1.944 on 10 and 99 DF | 0.7418 on 10 and 99 DF | 1.069 on 10 and 99 DF | ||||
| p-value | 0.026 | 0.048 | 0.684 | 0.394 | ||||
| Final model | ||||||||
| (Intercept) | 1.076 | 0.798 | −1.707 | 0.024 * | −0.052 | 0.007 ** | ||
| Health promotion program | −25.576 | 0.015 * | 7.762 | <0.001 *** | Excluded all | |||
| Insulin injection or antihyperglycemic drugs | 0.164 | 0.016 * | ||||||
| Multiple R-squared | 0.053 | 0.140 | 0.053 | |||||
| Adjusted R-squared | 0.045 | 0.133 | 0.044 | |||||
| F-statistic | 6.101 on 1 and 108 DF | 17.64 on 1 and 108 DF | 6 on 1 and 108 DF | |||||
| p-value | 0.015 | < 0.001 | 0.016 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okuda, S.; Tunematsu, M.; Tabuchi, K.; Kobayashi, T.; Kakehashi, M.; Nakatani, H. A New Health Promotion Program That Includes Wadaiko Rhythm Exercise to Maintain the Health of Persons Excluded from Receiving Specific Health Guidance. Int. J. Environ. Res. Public Health 2022, 19, 8520. https://doi.org/10.3390/ijerph19148520
Okuda S, Tunematsu M, Tabuchi K, Kobayashi T, Kakehashi M, Nakatani H. A New Health Promotion Program That Includes Wadaiko Rhythm Exercise to Maintain the Health of Persons Excluded from Receiving Specific Health Guidance. International Journal of Environmental Research and Public Health. 2022; 19(14):8520. https://doi.org/10.3390/ijerph19148520
Chicago/Turabian StyleOkuda, Suzumi, Miwako Tunematsu, Keiji Tabuchi, Toshio Kobayashi, Masayuki Kakehashi, and Hisae Nakatani. 2022. "A New Health Promotion Program That Includes Wadaiko Rhythm Exercise to Maintain the Health of Persons Excluded from Receiving Specific Health Guidance" International Journal of Environmental Research and Public Health 19, no. 14: 8520. https://doi.org/10.3390/ijerph19148520
APA StyleOkuda, S., Tunematsu, M., Tabuchi, K., Kobayashi, T., Kakehashi, M., & Nakatani, H. (2022). A New Health Promotion Program That Includes Wadaiko Rhythm Exercise to Maintain the Health of Persons Excluded from Receiving Specific Health Guidance. International Journal of Environmental Research and Public Health, 19(14), 8520. https://doi.org/10.3390/ijerph19148520






