Health Disparity Resulting from the Effect of Built Environment on Temperature-Related Mortality in a Subtropical Urban Setting
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
2.1.1. Mortality Data
2.1.2. Socioeconomic Data
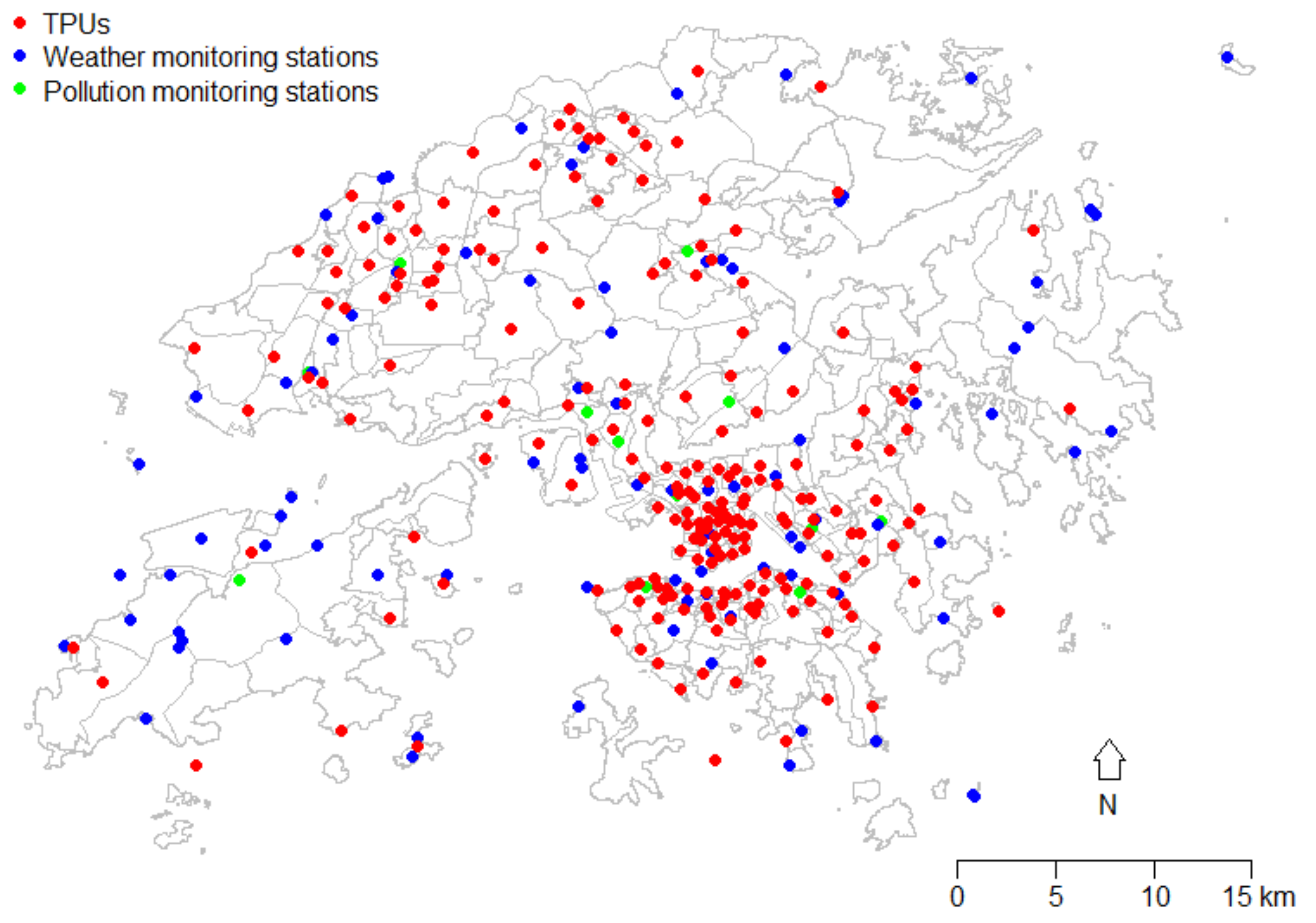
2.1.3. Meteorological and Pollution Data
2.1.4. Green Space Data
2.2. Statistical Methods
3. Results
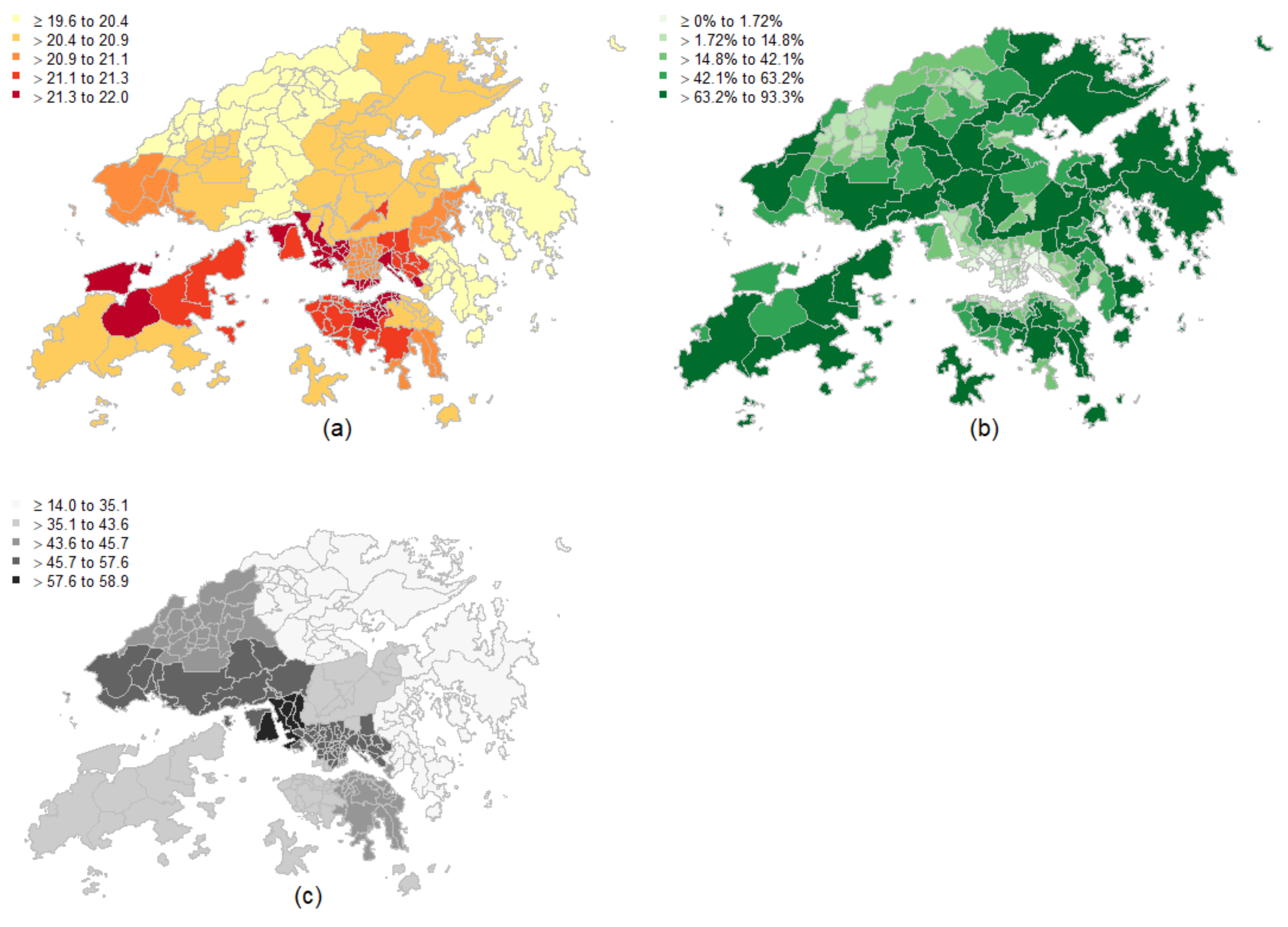
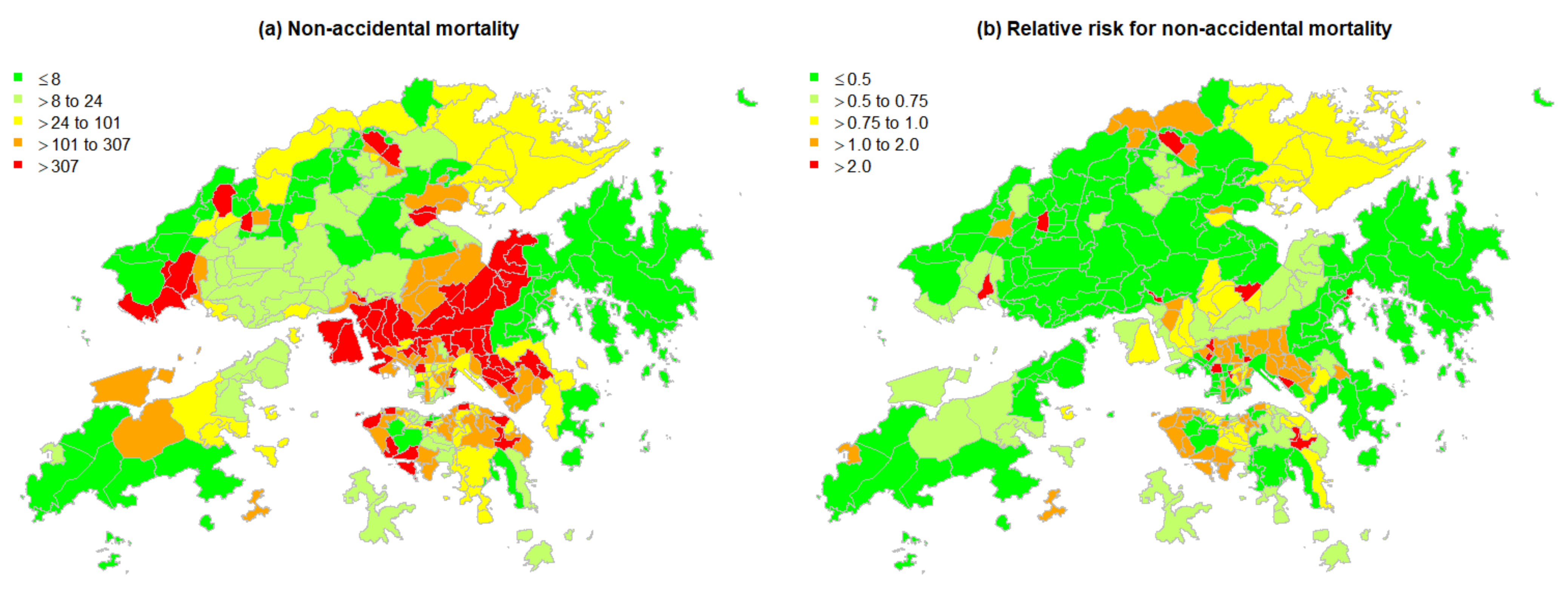
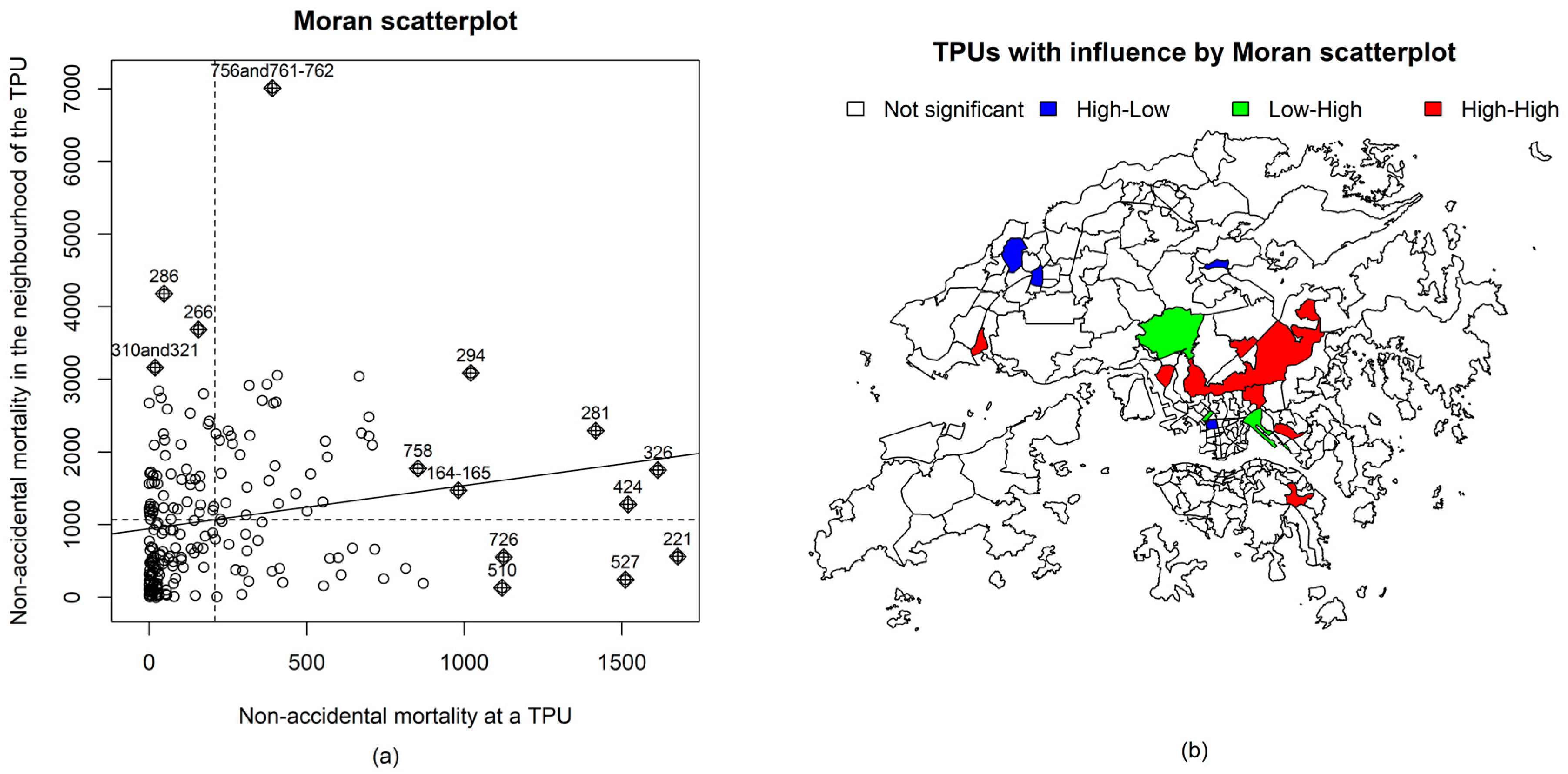
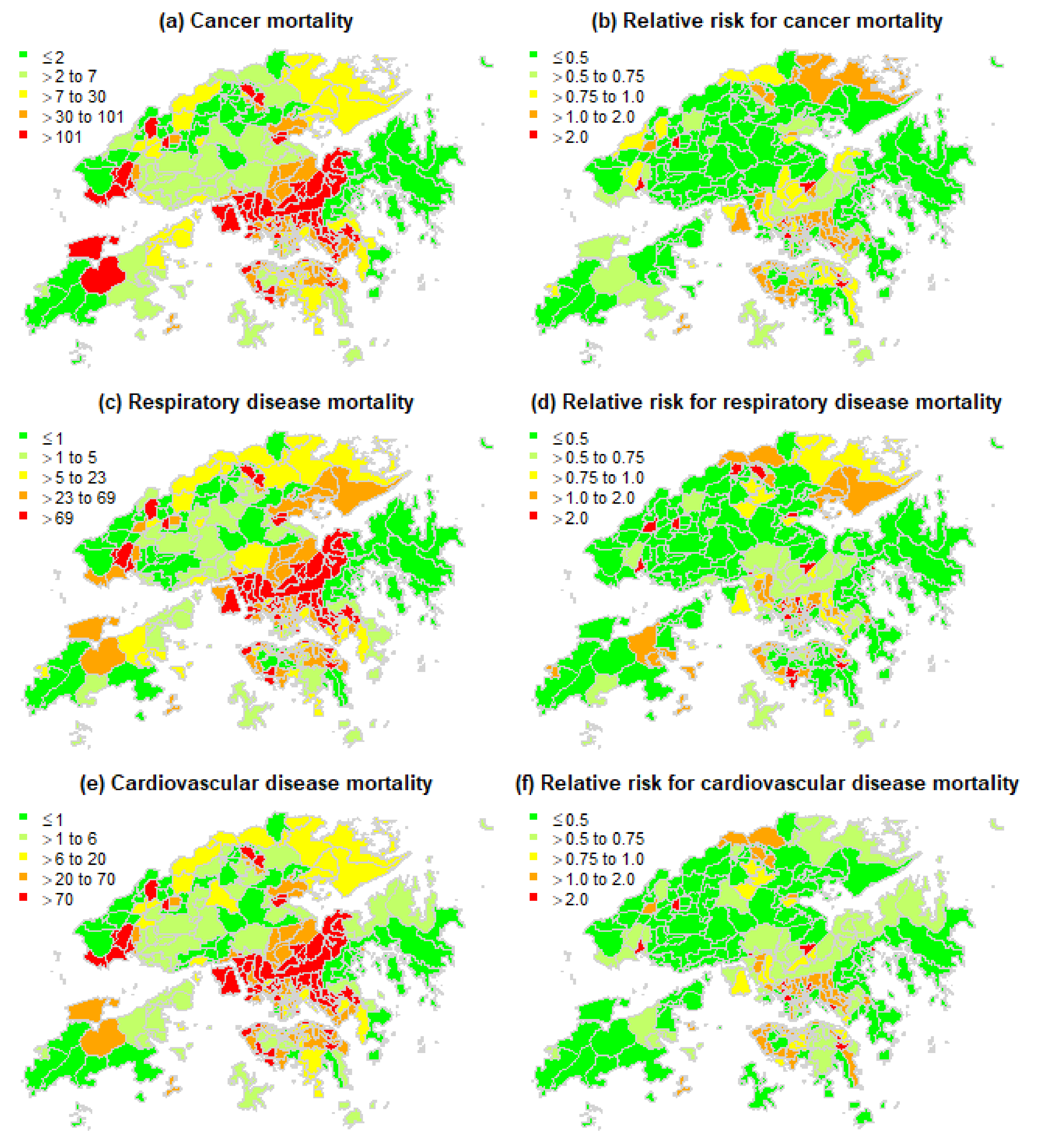
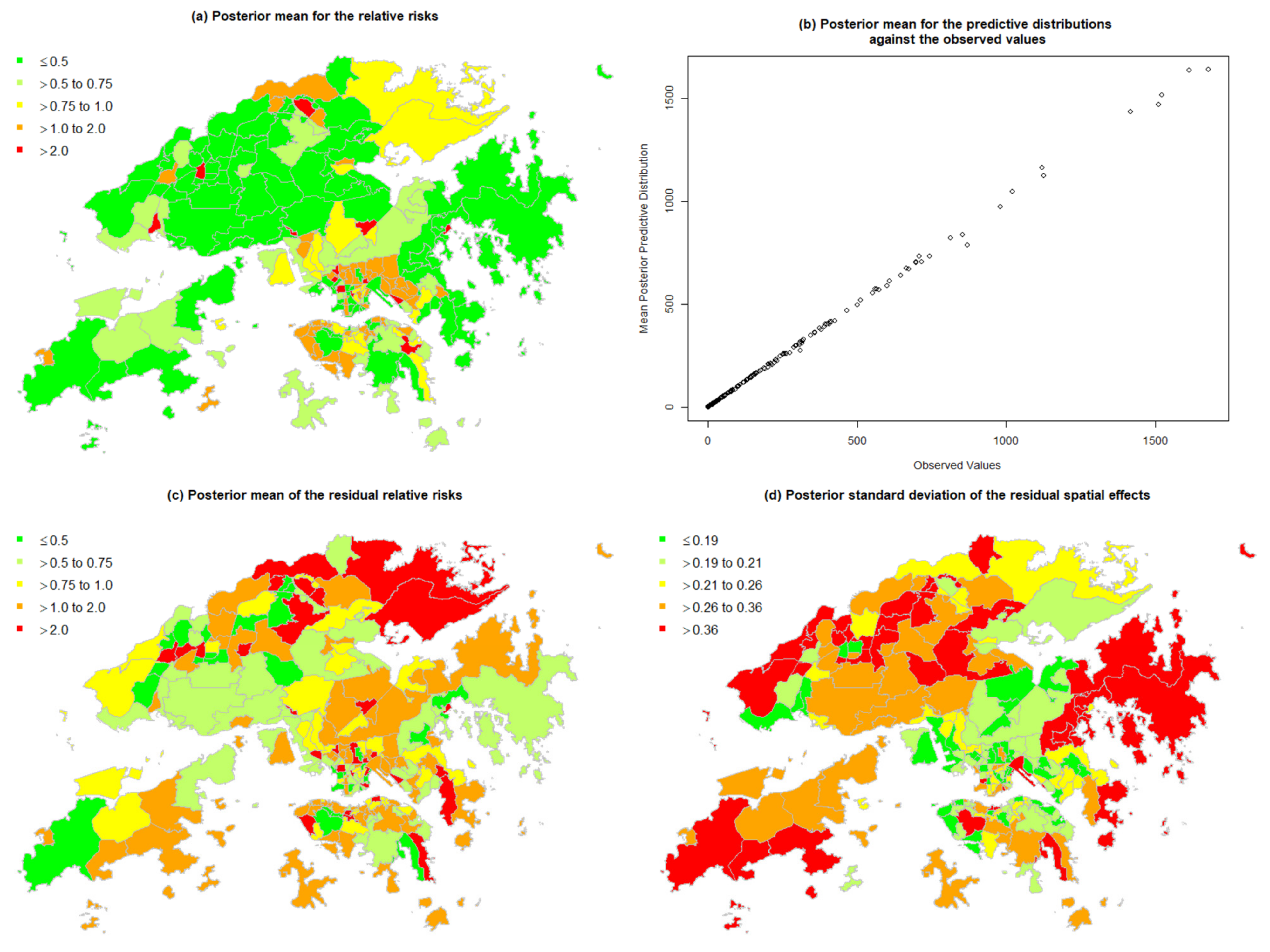
3.1. Spatial Patterns of Mortality and Temperature
3.2. Associations of Mortality and Temperature
3.2.1. Non-Accidental Mortality
3.2.2. Cancer Mortality
3.2.3. Respiratory Disease Mortality
3.2.4. Cardiovascular Disease Mortality
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Curriero, F.C.; Heiner, K.S.; Samet, J.M.; Zeger, S.L.; Strug, L.; Patz, J.A. Temperature and mortality in 11 cities of the eastern United States. Am. J. Epidemiol. 2002, 155, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.Y.; Honda, Y.; Hong, Y.C.; Pan, X.C.; Guo, Y.L.; Kim, H. Ambient temperature and mortality: An international study in four capital cities of East Asia. Sci. Total Environ. 2009, 408, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.G.; Bell, M.L. Weather-related mortality: How heat, cold, and heat waves affect mortality in the United States. Epidemiology 2009, 20, 205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braga, A.L.; Zanobetti, A.; Schwartz, J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ. Health Perspect. 2002, 110, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Medina-Ramon, M.; Schwartz, J. Temperature, temperature extremes, and mortality: A study of acclimatisation and effect modification in 50 US cities. Occup. Environ. Med. 2007, 64, 827–833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carder, M.; McNamee, R.; Beverland, I.; Elton, R.; Cohen, G.R.; Boyd, J.; Agius, R.M. The lagged effect of cold temperature and wind chill on cardiorespiratory mortality in Scotland. Occup. Environ. Med. 2005, 62, 702–710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, E.Y.Y.; Goggins, W.B.; Kim, J.J.; Griffiths, S.M. A study of intracity variation of temperature-related mortality and socioeconomic status among the Chinese population in Hong Kong. J. Epidemiol. Community Health 2012, 66, 322–327. [Google Scholar] [CrossRef] [Green Version]
- Goggins, W.B.; Chan, E.Y.Y.; Yang, C.; Chong, M. Associations between mortality and meteorological and pollutant variables during the cool season in two Asian cities with sub-tropical climates: Hong Kong and Taipei. Environ. Health 2013, 12, 59. [Google Scholar] [CrossRef] [Green Version]
- Goggins, W.B.; Chan, E.Y.Y. A study of the short-term associations between hospital admissions and mortality from heart failure and meteorological variables in Hong Kong: Weather and heart failure in Hong Kong. Int. J. Cardiol. 2017, 228, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Gouveia, N.; Hajat, S.; Armstrong, B. Socioeconomic differentials in the temperature–mortality relationship in São Paulo, Brazil. Int. J. Epidemiol. 2003, 32, 390–397. [Google Scholar] [CrossRef] [Green Version]
- Hajat, S.; Kovats, R.; Lachowycz, K. Heat-related and cold-related deaths in England and Wales: Who is at risk? Occup. Environ. Med. 2007, 64, 93–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, W.W.; Hu, W.B.; Mengersen, K.; Guo, Y.M.; Pan, X.C.; Connell, D.; Tong, S.L. Time course of temperature effects on cardiovascular mortality in Brisbane, Australia. Heart 2011, 97, 1089–1093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, S.; Chan, E.Y.Y.; Goggins, W.B.; Huang, Z. The Mortality Risk and Socioeconomic Vulnerability Associated with High and Low Temperature in Hong Kong. Int. J. Environ. Res. Public Health 2020, 17, 7326. [Google Scholar] [CrossRef] [PubMed]
- Jerrett, M.; Burnett, R.T.; Ma, R.; Pope III, C.A.; Krewski, D.; Newbold, K.B.; Thurston, G.; Shi, Y.; Finkelstein, N.; Calle, E.E.; et al. Spatial analysis of air pollution and mortality in Los Angeles. Epidemiology 2005, 16, 727–736. [Google Scholar] [CrossRef]
- Miller, K.A.; Siscovick, D.S.; Sheppard, L.; Shepherd, K.; Sullivan, J.H.; Anderson, G.L.; Kaufman, J.D. Long-term exposure to air pollution and incidence of cardiovascular events in women. N. Engl. J. Med. 2007, 356, 447–458. [Google Scholar] [CrossRef]
- Maheswaran, R.; Haining, R.P.; Pearson, T.; Law, J.; Brindley, P.; Best, N.G. Outdoor NOx and stroke mortality: Adjusting for small area level smoking prevalence using a Bayesian approach. Stat. Methods Med. Res. 2006, 15, 499–516. [Google Scholar] [CrossRef]
- Wong, C.-M.; Ou, C.-Q.; Chan, K.-P.; Chau, Y.-K.; Thach, T.Q.; Yang, L.; Chung, R.Y.-N.; Thomas, G.N.; Peiris, J.S.M.; Wong, T.-W.; et al. The effects of air pollution on mortality in socially deprived urban areas in Hong Kong, China. Environ. Health Perspect. 2008, 116, 1189–1194. [Google Scholar] [CrossRef] [Green Version]
- Goggins, W.B.; Chan, E.Y.Y.; Ng, E.; Ren, C.; Chen, L. Effect modification of the association between short-term meteorological factors and mortality by urban heat islands in Hong Kong. PLoS ONE 2012, 7, e38551. [Google Scholar]
- Bivand, R.S.; Pebesma, E.J.; Gomez-Rubio, V.; Pebesma, E.J. Applied Spatial Data Analysis with R; Springer: New York, NY, USA, 2013. [Google Scholar]
- Bell, B.S.; Broemeling, L.D. A Bayesian analysis for spatial processes with application to disease mapping. Stat. Med. 2000, 19, 957–974. [Google Scholar] [CrossRef]
- Dominici, F.; Daniels, M.; Zeger, S.L.; Samet, J.M. Air pollution and mortality: Estimating regional and national dose-response relationships. J. Am. Stat. Assoc. 2002, 97, 100–111. [Google Scholar] [CrossRef]
- MacNab, Y.C. Hierarchical Bayesian spatial modelling of small-area rates of non-rare disease. Stat. Med. 2003, 22, 1761–1773. [Google Scholar] [CrossRef] [PubMed]
- Blangiardo, M.; Cameletti, M. Spatial and Spatio-Temporal Bayesian Models with R-INLA; John Wiley & Sons: Chichester, UK, 2015. [Google Scholar]
- MacNab, Y.C. Mapping disability-adjusted life years: A Bayesian hierarchical model framework for burden of disease and injury assessment. Stat. Med. 2007, 26, 4746–4769. [Google Scholar] [CrossRef] [PubMed]
- Kandt, J.; Chang, S.S.; Yip, P.; Burdett, R. The spatial pattern of premature mortality in Hong Kong: How does it relate to public housing? Urban Stud. 2017, 54, 1211–1234. [Google Scholar] [CrossRef]
- Burnett, R.; Chen, H.; Szyszkowicz, M.; Fann, N.; Hubbell, B.; Pope, C.A.; Apte, J.S.; Brauer, M.; Cohen, A.; Weichenthal, S.; et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci. USA 2018, 115, 9592–9597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seposo, X.; Ueda, K.; Sugata, S.; Yoshino, A.; Takami, A. Short-term effects of air pollution on daily single-and co-morbidity cardiorespiratory outpatient visits. Sci. Total Environ. 2020, 729, 138934. [Google Scholar] [CrossRef] [PubMed]
- Ito, K.; De Leon, S.F.; Lippmann, M. Associations between ozone and daily mortality: Analysis and meta-analysis. Epidemiology 2005, 16, 446–457. [Google Scholar] [CrossRef]
- Wong, C.M.; Ma, S.; Hedley, A.J.; Lam, T.H. Effect of air pollution on daily mortality in Hong Kong. Environ. Health Perspect. 2001, 109, 335–340. [Google Scholar] [CrossRef]
- Chan, E.Y.Y. Climate Change and Urban Health: The Case of Hong Kong as a Subtropical City; Routledge: Abingdon, UK; New York, NY, USA, 2019. [Google Scholar]
- Goggins, W.B.; Chan, E.Y.Y.; Yang, C.Y. Weather, pollution, and acute myocardial infarction in Hong Kong and Taiwan. Int. J. Cardiol. 2013, 168, 243–249. [Google Scholar] [CrossRef]
- Schwartz, J. Air pollution and hospital admissions for the elderly in Detroit, Michigan. Am. J. Respir. Crit. Care Med. 1994, 150, 648–655. [Google Scholar] [CrossRef]
- Wilkinson, R.G. National mortality rates: The impact of inequality? Am. J. Public Health 1992, 82, 1082–1084. [Google Scholar] [CrossRef] [Green Version]
- Mackenbach, J.P.; Kunst, A.E.; Cavelaars, A.E.; Groenhof, F.; Geurts, J.J.; EU Working Group on Socioeconomic Inequalities in Health. Socioeconomic inequalities in morbidity and mortality in western Europe. Lancet 1997, 349, 1655–1659. [Google Scholar] [CrossRef] [Green Version]
- Yu, I.T.S.; Zhang, Y.H.; Tam, W.W.S.; Yan, Q.H.; Xu, Y.J.; Xun, X.J.; Wu, W.; Ma, W.J.; Tian, L.; Tse, L.A.; et al. Effect of ambient air pollution on daily mortality rates in Guangzhou, China. Atmos. Environ. 2012, 46, 528–535. [Google Scholar] [CrossRef]
- Mackenbach, J.P.; Bos, V.; Andersen, O.; Cardano, M.; Costa, G.; Harding, S.; Reid, A.; Hemström, O.; Valkonen, T.; Kunst, A.E. Widening socioeconomic inequalities in mortality in six Western European countries. Int. J. Epidemiol. 2003, 32, 830–837. [Google Scholar] [CrossRef]
- Wilkinson, R.G.; Pickett, K.E. Income inequality and socioeconomic gradients in mortality. Am. J. Public Health 2008, 98, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Humpel, N.; Owen, N.; Leslie, E. Environmental factors associated with adults’ participation in physical activity: A review. Am. J. Prev. Med. 2002, 22, 188–199. [Google Scholar] [CrossRef]
- Kaczynski, A.T.; Henderson, K.A. Environmental correlates of physical activity: A review of evidence about parks and recreation. Leis. Sci. 2007, 29, 315–354. [Google Scholar] [CrossRef]
- Mitchell, R.; Popham, F. Effect of exposure to natural environment on health inequalities: An observational population study. Lancet 2008, 372, 1655–1660. [Google Scholar] [CrossRef] [Green Version]
- Sugiyama, T.; Leslie, E.; Giles-Corti, B.; Owen, N. Associations of neighbourhood greenness with physical and mental health: Do walking, social coherence and local social interaction explain the relationships? J. Epidemiol. Community Health 2008, 62, e9. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Health Emergency and Disaster Risk Management Framework. Available online: https://www.who.int/hac/techguidance/preparedness/health-emergency-and-disaster-risk-management-framework-eng.pdf?ua=1 (accessed on 26 January 2022).
- Chan, E.Y.Y.; Lam, H.C.Y. Research in health-emergency and disaster risk management and its potential implications in the post covid-19 world. Int. J. Environ. Res. Public Health 2021, 18, 2520. [Google Scholar] [CrossRef]
- Hong Kong Observatory. Climate of Hong Kong. Available online: https://www.hko.gov.hk/en/cis/climahk.htm (accessed on 26 January 2022).
- Huang, Z.; Chan, E.Y.Y.; Wong, C.S.; Zee, B.C.Y. Clustering of socioeconomic data in Hong Kong for planning better community health protection. Int. J. Environ. Res. Public Health 2021, 18, 12617. [Google Scholar] [CrossRef]
- Barnett, A.G.; Tong, S.; Clements, A.C. What measure of temperature is the best predictor of mortality? Environ. Res. 2010, 110, 604–611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaeffer, L.; de Crouy-Chanel, P.; Wagner, V.; Desplat, J.; Pascal, M. How to estimate exposure when studying the temperature-mortality relationship? A case study of the Paris area. Int. J. Biometeorol. 2016, 60, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.W.; Yuan, L.; Perlin, S.A. Comparison of spatial interpolation methods for the estimation of air quality data. J. Expo. Sci. Environ. Epidemiol. 2004, 14, 404–415. [Google Scholar] [CrossRef] [Green Version]
- DATA.GOV.HK. Land Utilization in Hong Kong (Statistics). Available online: https://data.gov.hk/en-data/dataset/hk-pland-pland1-land-utilization-in-hong-kong-statistics (accessed on 26 January 2022).
- Besag, J.; York, J.; Mollie, A. Bayesian image restoration, with two applications in spatial statistics. Ann. Inst. Stat. Math. 1991, 43, 1–59. [Google Scholar] [CrossRef]
- Wang, X.; Yue, Y.R.; Faraway, J.J. Bayesian Regression Modeling with INLA; Chapman & Hall/CRC: Abingdon, UK; Taylor and Francis Group: Abingdon, UK, 2018. [Google Scholar]
- Spiegelhalter, D.J.; Best, N.G.; Carlin, B.P.; Van Der Linde, A. Bayesian measures of model complexity and fit. J. R. Stat. Soc. Ser. B 2002, 64, 583–639. [Google Scholar] [CrossRef] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing:: Vienna, Austria, 2019; Available online: https://www.R-project.org/ (accessed on 26 January 2022).
- Rue, H.; Martino, S.; Chopin, N. Approximate Bayesian inference for latent Gaussian model by using integrated nested Laplace approximations. J. R. Stat. Soc. Ser. B 2009, 71, 319–392. [Google Scholar] [CrossRef]
- Huang, Z.; Lin, H.; Liu, Y.; Zhou, M.; Liu, T.; Xiao, J.; Zeng, W.; Li, X.; Zhang, Y.; Ebi, K.L.; et al. Individual-level and community-level effect modifiers of the temperature–mortality relationship in 66 Chinese communities. BMJ Open 2015, 5, e009172. [Google Scholar] [CrossRef] [Green Version]
- Scoggins, A.; Kjellstrom, T.; Fisher, G.; Connor, J.; Gimson, N. Spatial analysis of annual air pollution exposure and mortality. Sci. Total Environ. 2004, 321, 71–85. [Google Scholar] [CrossRef]
- Zanobetti, A.; O’Neill, M.S.; Gronlund, C.J.; Schwartz, J.D. Susceptibility to mortality in weather extremes: Effect modification by personal and small area characteristics in a multi-city case-only analysis. Epidemiology 2013, 24, 809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gawda, A.; Majka, G.; Nowak, B.; Marcinkiewicz, J. Air pollution, oxidative stress, and exacerbation of autoimmune diseases. Cent. Eur. J. Immunol. 2017, 42, 305. [Google Scholar] [CrossRef]
- Benavides, R.; Montes, F.; Rubio, A.; Osoro, K. Geostatistical modelling of air temperature in a mountainous region of Northern Spain. Agric. For. Meteorol. 2007, 146, 173–188. [Google Scholar] [CrossRef]
- Ustrnul, Z.; Czekierda, D. Application of GIS for the development of climatological air temperature maps: An example from Poland. Meteorol. Appl. 2005, 12, 43–50. [Google Scholar] [CrossRef]
- Wakefield, J.; Shaddick, G. Health-exposure modeling and the ecological fallacy. Biostatistics 2016, 7, 438–455. [Google Scholar] [CrossRef] [Green Version]
- Gascon, M.; Triguero-Mas, M.; Martínez, D.; Dadvand, P.; Rojas-Rueda, D.; Plasència, A.; Nieuwenhuijsen, M.J. Residential green spaces and mortality: A systematic review. Environ. Int. 2016, 86, 60–67. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Lau, K.K.L.; Yu, R.; Wong, S.Y.; Kwok, T.T.; Woo, J. Neighbouring green space and mortality in community-dwelling elderly Hong Kong Chinese: A cohort study. BMJ Open 2017, 7, e015794. [Google Scholar] [CrossRef]
- Xu, L.; Ren, C.; Yuan, C.; Nichol, J.; Goggins, W.B. An ecological study of the association between area-level green space and adult mortality in Hong Kong. Climate 2017, 5, 55. [Google Scholar] [CrossRef] [Green Version]
- Cole, H.V.; Triguero-Mas, M.; Connolly, J.J.; Anguelovski, I. Determining the health benefits of green space: Does gentrification matter? Health Place 2019, 57, 1–11. [Google Scholar] [CrossRef]
- Markevych, I.; Schoierer, J.; Hartig, T.; Chudnovsky, A.; Hystad, P.; Dzhambov, A.M.; Fuertes, E. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ. Res. 2017, 158, 301–317. [Google Scholar] [CrossRef]
- Wolch, J.R.; Byrne, J.; Newell, J.P. Urban green space, public health, and environmental justice: The challenge of making cities ‘just green enough’. Landsc. Urban Plan. 2014, 125, 234–244. [Google Scholar] [CrossRef] [Green Version]
- Thach, T.-Q.; Zheng, Q.; Lai, P.-C.; Wong, P.P.-Y.; Chau, P.Y.-K.; Jahn, H.J.; Plass, D.; Katzschner, L.; Kraemer, A.; Wong, C.-M. Assessing spatial associations between thermal stress and mortality in Hong Kong: A small-area ecological study. Sci. Total Environ. 2015, 502, 666–672. [Google Scholar] [CrossRef]
| (a) Descriptive Statistics | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Area-Level Characteristic | Minimum | 25th Percentile | Median | 75th Percentile | Maximum | ||||||||||
| Indigenous degree score | −4.5 | −0.4 | 0.3 | 0.6 | 1.2 | ||||||||||
| Family resilience score | −4.2 | −0.4 | 0.2 | 0.5 | 2.4 | ||||||||||
| Individual productivity score | −3 | −0.6 | 0.1 | 0.6 | 3.1 | ||||||||||
| Populous grassroots score | −2.8 | −0.8 | 0 | 0.8 | 2.6 | ||||||||||
| Young-age score | −2.4 | −0.6 | −0.2 | 0.5 | 5.4 | ||||||||||
| PM2.5 (µg/m3) | 18.5 | 20.0 | 21.5 | 22.9 | 27.0 | ||||||||||
| NO2 (µg/m3) | 14.0 | 37.5 | 45.6 | 56.5 | 58.9 | ||||||||||
| O3 (µg/m3) | 32.0 | 33.0 | 41.1 | 43.5 | 62.5 | ||||||||||
| PM10 (µg/m3) | 28.4 | 30.6 | 32.0 | 34.3 | 43.7 | ||||||||||
| SO2 (µg/m3) | 4.6 | 6.1 | 9.3 | 9.8 | 11.6 | ||||||||||
| Minimum temperature (°C) | 19.6 | 20.6 | 21.0 | 21.3 | 22.0 | ||||||||||
| Rain (mm) | 2158 | 2579 | 2857 | 3033 | 3464 | ||||||||||
| Dew temperature (°C) | 18.8 | 19.1 | 19.4 | 19.8 | 20.3 | ||||||||||
| Relative humidity (%) | 72.9 | 78.9 | 80.5 | 81.6 | 85.5 | ||||||||||
| Green space density (%) | 0.0 | 3.4 | 32.4 | 57.0 | 93.3 | ||||||||||
| (b) Pearson Correlations | |||||||||||||||
| PC 1 | PC 2 | PC 3 | PC 4 | PC 5 | PM2.5 | NO2 | O3 | PM10 | SO2 | min.T | Rain | dew.T | RH | GS | |
| PC 1 | 1 | ||||||||||||||
| PC 2 | 0 | 1 | |||||||||||||
| PC 3 | 0 | 0 | 1 | ||||||||||||
| PC 4 | 0 | 0 | 0 | 1 | |||||||||||
| PC 5 | 0 | 0 | 0 | 0 | 1 | ||||||||||
| PM2.5 | 0.2 | −0.08 | −0.1 | 0.02 | 0.07 | 1 | |||||||||
| NO2 | 0.11 | −0.1 | 0.15 | 0.2 | −0.06 | 0.6 | 1 | ||||||||
| O3 | −0.23 | 0.06 | 0.07 | 0.02 | −0.03 | −0.77 | −0.75 | 1 | |||||||
| PM10 | 0.18 | −0.07 | −0.09 | 0 | 0.14 | 0.91 | 0.5 | −0.55 | 1 | ||||||
| SO2 | 0.02 | −0.14 | −0.01 | −0.01 | 0 | 0.66 | 0.54 | −0.71 | 0.59 | 1 | |||||
| min.T | −0.28 | −0.26 | 0.3 | 0.34 | −0.17 | 0.04 | 0.39 | 0.01 | 0.06 | 0.05 | 1 | ||||
| Rain | −0.05 | 0.03 | 0.27 | 0.15 | −0.11 | −0.36 | −0.05 | 0.22 | −0.45 | −0.44 | 0.18 | 1 | |||
| dew.T | −0.16 | −0.29 | 0.13 | 0 | −0.14 | −0.25 | −0.27 | 0.44 | −0.1 | −0.17 | 0.2 | −0.09 | 1 | ||
| RH | 0.08 | −0.01 | −0.06 | −0.07 | 0.01 | −0.34 | −0.41 | 0.44 | −0.18 | −0.28 | −0.37 | −0.01 | 0.64 | 1 | |
| GS | −0.2 | 0.37 | −0.21 | −0.11 | 0.07 | −0.29 | −0.41 | 0.31 | −0.22 | −0.1 | −0.31 | −0.17 | 0.06 | 0.28 | 1 |
| Non-Accidental Mortality (44,543 Cases) | Cancer Mortality (14,175 Cases) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariable | Multivariable (∆DIC = −38.0) | Univariable | Multivariable (∆DIC = −47.2) | |||||||||
| Mean | Lower | Upper | Mean | Lower | Upper | Mean | Lower | Upper | Mean | Lower | Upper | |
| Intercept | −6.756 | −12.788 | −0.748 | −8.04 | −13.781 | −2.339 | ||||||
| Indigenous degree | 0.104 | −0.046 | 0.254 | 0.124 | −0.015 | 0.262 | ||||||
| Family resilience | −0.158 | −0.319 | 0.002 | −0.167 | −0.314 | −0.020 | −0.084 | −0.213 | 0.045 | |||
| Individual productivity | −0.109 | −0.266 | 0.048 | −0.101 | −0.245 | 0.045 | ||||||
| Populous grassroots | 0.487 | 0.350 | 0.626 | 0.443 | 0.313 | 0.757 | 0.468 | 0.340 | 0.599 | 0.437 | 0.314 | 0.561 |
| Young age | −0.427 | −0.56 | −0.29 | −0.429 | −0.553 | −0.305 | −0.381 | −0.509 | −0.256 | −0.384 | −0.502 | −0.267 |
| NO2 | 0.026 | 0.006 | 0.045 | 0.011 | −0.004 | 0.026 | 0.024 | 0.006 | 0.041 | 0.010 | −0.004 | 0.023 |
| Minimum temperature | 0.562 | 0.206 | 0.918 | 0.034 | −0.259 | 0.326 | 0.555 | 0.232 | 0.877 | 0.044 | −0.234 | 0.323 |
| Green space density | −0.860 | −1.396 | −0.328 | −0.492 | −0.944 | −0.041 | −0.781 | −1.278 | −0.291 | −0.342 | −0.795 | 0.108 |
| Respiratory disease mortality (10,682 cases) | Cardiovascular disease mortality (9969 cases) | |||||||||||
| Univariable | Multivariable (∆DIC = −32.1) | Univariable | Multivariable (∆DIC = −36.4) | |||||||||
| Mean | Lower | Upper | Mean | Lower | Upper | Mean | Lower | Upper | Mean | Lower | Upper | |
| Intercept | −9.09 | −17.18 | −1.042 | −6.416 | −12.344 | −0.500 | ||||||
| Indigenous degree | 0.191 | 0.023 | 0.360 | 0.115 | −0.046 | 0.279 | 0.134 | −0.011 | 0.280 | |||
| Family resilience | −0.190 | −0.370 | −0.011 | −0.049 | −0.214 | 0.119 | −0.135 | −0.286 | 0.016 | |||
| Individual productivity | −0.243 | −0.412 | −0.074 | −0.227 | −0.387 | −0.067 | −0.125 | −0.275 | 0.026 | |||
| Populous grassroots | 0.432 | 0.273 | 0.596 | 0.347 | 0.191 | 0.508 | 0.442 | 0.307 | 0.582 | 0.411 | 0.281 | 0.545 |
| Young age | −0.400 | −0.555 | −0.247 | −0.404 | −0.551 | −0.260 | −0.373 | −0.507 | −0.242 | −0.384 | −0.510 | −0.260 |
| NO2 | 0.029 | 0.013 | 0.046 | 0.013 | −0.004 | 0.031 | 0.025 | 0.011 | 0.040 | 0.010 | −0.004 | 0.025 |
| Minimum temperature | 0.482 | 0.158 | 0.810 | −0.073 | −0.320 | 0.467 | 0.389 | 0.055 | 0.726 | −0.048 | −0.336 | 0.240 |
| Green space density | −1.058 | −1.598 | −0.525 | −0.552 | −0.836 | −0.268 | −0.883 | −1.395 | −0.379 | −0.592 | −1.045 | −0.141 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Z.; Chan, E.Y.-Y.; Wong, C.-S.; Liu, S.; Zee, B.C.-Y. Health Disparity Resulting from the Effect of Built Environment on Temperature-Related Mortality in a Subtropical Urban Setting. Int. J. Environ. Res. Public Health 2022, 19, 8506. https://doi.org/10.3390/ijerph19148506
Huang Z, Chan EY-Y, Wong C-S, Liu S, Zee BC-Y. Health Disparity Resulting from the Effect of Built Environment on Temperature-Related Mortality in a Subtropical Urban Setting. International Journal of Environmental Research and Public Health. 2022; 19(14):8506. https://doi.org/10.3390/ijerph19148506
Chicago/Turabian StyleHuang, Zhe, Emily Ying-Yang Chan, Chi-Shing Wong, Sida Liu, and Benny Chung-Ying Zee. 2022. "Health Disparity Resulting from the Effect of Built Environment on Temperature-Related Mortality in a Subtropical Urban Setting" International Journal of Environmental Research and Public Health 19, no. 14: 8506. https://doi.org/10.3390/ijerph19148506
APA StyleHuang, Z., Chan, E. Y.-Y., Wong, C.-S., Liu, S., & Zee, B. C.-Y. (2022). Health Disparity Resulting from the Effect of Built Environment on Temperature-Related Mortality in a Subtropical Urban Setting. International Journal of Environmental Research and Public Health, 19(14), 8506. https://doi.org/10.3390/ijerph19148506






