Childhood Trauma and Suicide: The Mediating Effect of Stress and Sleep
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Measures
2.2.1. Childhood Trauma
2.2.2. Stress
2.2.3. Sleep Quality
2.2.4. Suicide Risk
2.3. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Correlational Analysis
3.3. Mediation Analysis
3.3.1. Common Method Bias
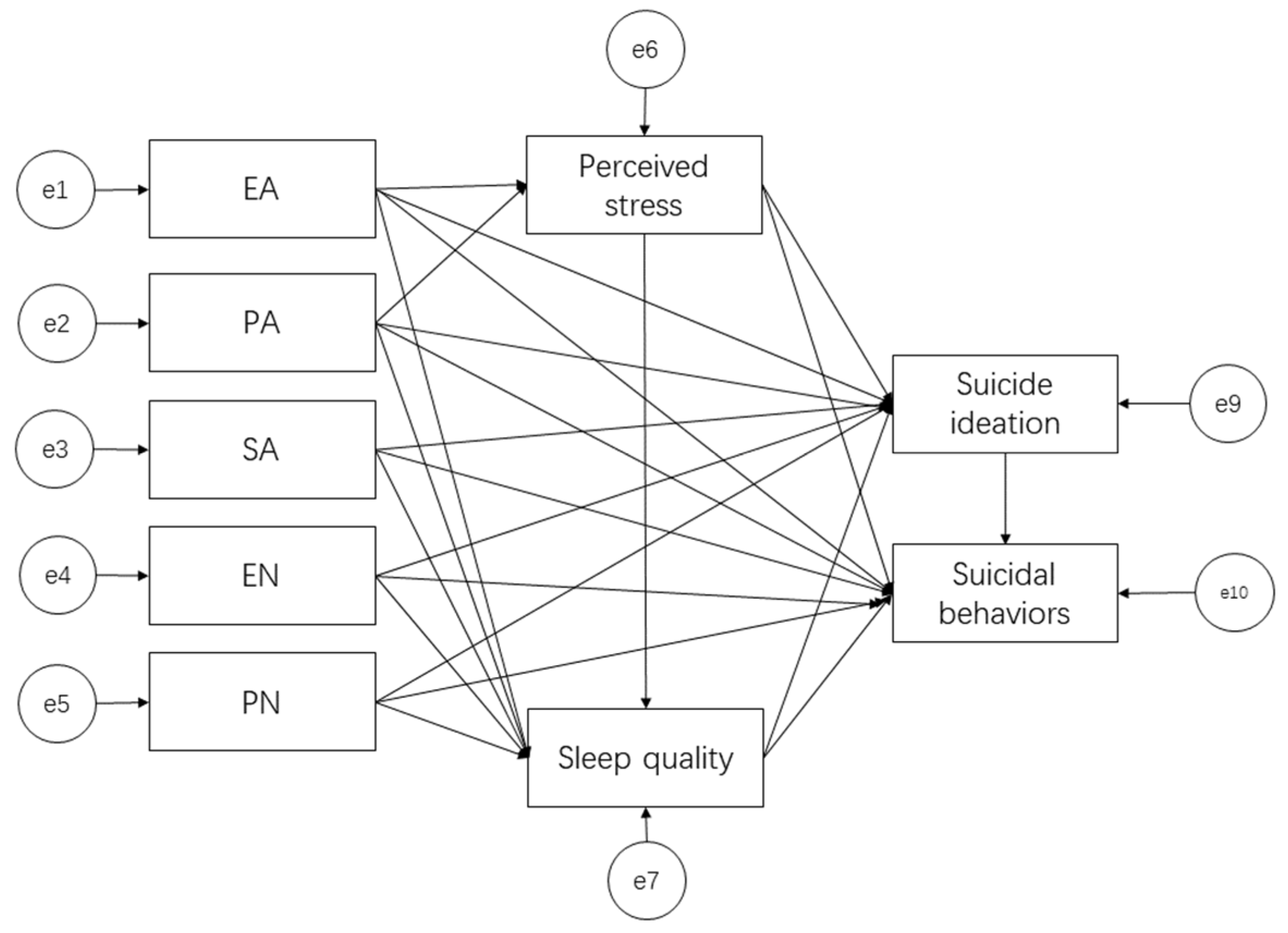
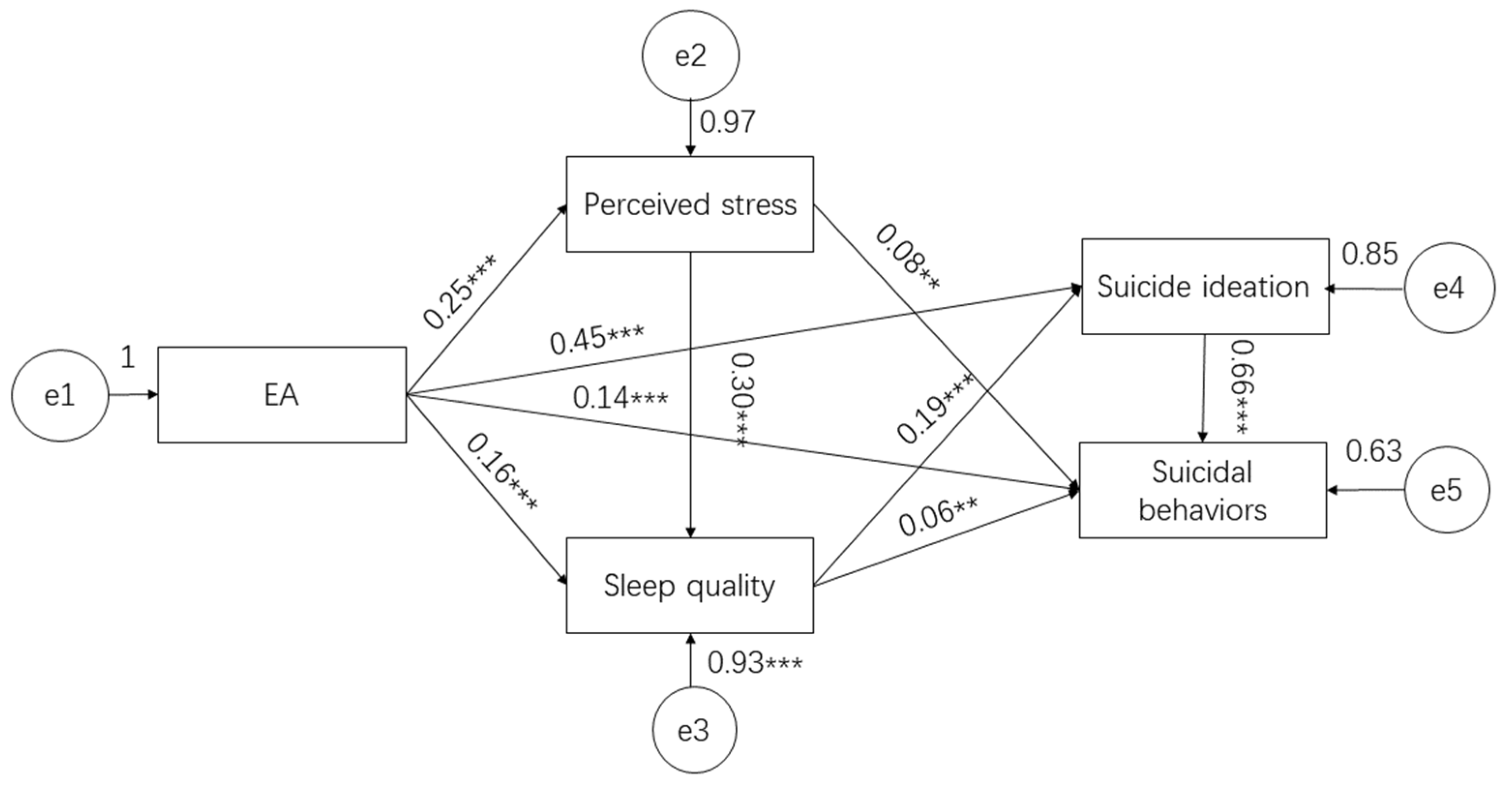
3.3.2. SEM
3.3.3. Mediation Analysis
- Model 1: EA ® perceived stress ® sleep quality ® suicidal ideation ® suicide behaviors;
- Model 2: EA ® perceived stress ® sleep quality ® suicide behaviors;
- Model 3: EA ® perceived stress ® suicide behaviors;
- Model 4: EA ® sleep quality ® suicidal ideation ® suicide behaviors;
- Model 5: EA ® sleep quality ® suicide behaviors;
- Model 6: EA ® suicidal ideation ® suicide behaviors.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nock, M.K.; Green, J.G.; Hwang, I.; McLaughlin, K.A.; Sampson, N.A.; Zaslavsky, A.M.; Kessler, R.C. Prevalence, Correlates, and Treatment of Lifetime Suicidal Behavior Among Adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry 2013, 70, 300–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nock, M.K.; Borges, G.; Bromet, E.J.; Alonso, J.; Angermeyer, M.; Beautrais, A.; Bruffaerts, R.; Chiu, W.T.; de Girolamo, G.; Gluzman, S.; et al. Cross-National Prevalence and Risk Factors for Suicidal Ideation, Plans and Attempts. Br. J. Psychiatry 2008, 192, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Turecki, G.; Brent, D.A. Suicide and Suicidal Behaviour. Lancet 2016, 387, 1227–1239. [Google Scholar] [CrossRef]
- Feng, J.; Li, S.; Chen, H. Impacts of Stress, Self-Efficacy, and Optimism on Suicide Ideation Among Rehabilitation Patients with Acute Pesticide Poisoning. PLoS ONE 2015, 10, e0118011. [Google Scholar] [CrossRef] [PubMed]
- Gradus, J.L.; Qin, P.; Lincoln, A.K.; Miller, M.; Lawler, E.; Sørensen, H.T.; Lash, T.L. Posttraumatic Stress Disorder and Completed Suicide. Am. J. Epidemiol. 2010, 171, 721–727. [Google Scholar] [CrossRef]
- Agnew-Blais, J.; Danese, A. Childhood Maltreatment and Unfavourable Clinical Outcomes in Bipolar Disorder: A Systematic Review and Meta-Analysis. Lancet Psychiatry 2016, 3, 342–349. [Google Scholar] [CrossRef]
- Lew, B.L.; Huen, J.; Yu, P.; Yuan, L.; Wang, D.F.; Ping, F.; Abu Talib, M.; Lester, D.; Jia, C.X. Associations Between Depression, Anxiety, Stress, Hopelessness, Subjective Well-Being, Coping Styles and Suicide in Chinese University Students. PLoS ONE 2019, 14, e0217372. [Google Scholar] [CrossRef]
- Pigeon, W.R.; Pinquart, M.; Conner, K. Meta-Analysis of Sleep Disturbance and Suicidal Thoughts and Behaviors. J. Clin. Psychiatry 2012, 73, e1160–e1167. [Google Scholar] [CrossRef]
- Kearns, J.C.; Coppersmith, D.D.L.; Santee, A.C.; Insel, C.; Pigeon, W.R.; Glenn, C.R. Sleep Problems and Suicide Risk in Youth: A Systematic Review, Developmental Framework, and Implications for Hospital Treatment. Gen. Hosp. Psychiatry 2022, 63, 141–151. [Google Scholar] [CrossRef]
- Otsuka, Y.; Kaneita, Y.; Itani, O.; Nakagome, S.; Jike, M.; Ohida, T. Relationship Between Stress Coping and Sleep Disorders Among the General Japanese Population: A Nationwide Representative Survey. Sleep Med. 2017, 37, 38–45. [Google Scholar] [CrossRef]
- Wu, R.; Zhu, H.; Wang, Y.; Jiang, C.-L. The Effect of Stress on Suicide and Sleep Disturbance. Prog. Physiol. Sci. 2019, 50, 161–166. (In Chinese) [Google Scholar]
- Kripke, D.F.; Kline, L.E.; Nievergelt, C.M.; Murray, S.S.; Shadan, F.F.; Dawson, A.; Poceta, J.S.; Cronin, J.; Jamil, S.M.; Tranah, G.J.; et al. Genetic Variants Associated with Sleep Disorders. Sleep Med. 2015, 16, 217–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jakob, H.; Wagner, K.V.; Claudia, L.; Scharf, S.H.; Xiao-Dong, W.; Miriam, W.; Felix, H.; Theo, R.; Ulrike, S.; Chadi, T. The Involvement of FK506-Binding Protein 51 (FKBP5) in the Behavioral and Neuroendocrine Effects of Chronic Social Defeat Stress. Neuropharmacology 2012, 62, 332–339. [Google Scholar] [CrossRef]
- Roy, A.; Gorodetsky, E.; Yuan, Q.; Goldman, D.; Enoch, M.A. Interaction of FKBP5, a Stress-Related Gene, with Childhood Trauma Increases the Risk for Attempting Suicide. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2010, 35, 1674–1683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Womersley, J.S.; Nothling, J.; Toikumo, S.; Malan-Müller, S.; van den Heuvel, L.L.; McGregor, N.W.; Seedat, S.M.J.; Hemmings, S.M.J. Childhood Trauma, the Stress Response and Metabolic Syndrome: A Focus on DNA Methylation. Eur. J. Neurosci. 2021, 55, 2253–2296. [Google Scholar] [CrossRef]
- Lutz, P.E.; Mechawar, N.; Turecki, G. Neuropathology of Suicide: Recent Findings and Future Directions. Mol. Psychiatry 2017, 22, 1395–1412. [Google Scholar] [CrossRef]
- Bernstein, D.; Fink, L.; Bernstein, D. Childhood Trauma Questionnaire: A Retrospective Self-Report-Manual; The Psychological Corporation: San Antonio, TX, USA, 1998. [Google Scholar]
- Bernstein, D.P.; Stein, J.A.; Newcomb, M.D.; Walker, E.; Pogge, D.; Ahluvalia, T.; Stokes, J.; Handelsman, L.; Medrano, M.; Desmond, D.; et al. Development and Validation of a Brief Screening Version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003, 27, 169–190. [Google Scholar] [CrossRef]
- Jansen, K.; Cardoso, T.A.; Fries, G.R.; Branco, J.C.; Silva, R.A.; Kauer-Sant’Anna, M.; Kapczinski, F.; Magalhaes, P.V.S. Childhood Trauma, Family History, and Their Association with Mood Disorders in Early Adulthood. Acta Psychiatr. Scand. 2016, 134, 281–286. [Google Scholar] [CrossRef]
- Xie, P.; Wu, K.; Zheng, Y.; Guo, Y.; Yang, Y.; He, J.; Ding, Y.; Peng, H. Prevalence of Childhood Trauma and Correlations between Childhood Trauma, Suicidal Ideation, and Social Support in Patients with Depression, Bipolar Disorder, and Schizophrenia in Southern China. J. Affect. Disord. 2018, 228, 41–48. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences (Rev. Ed.). Technometrics 1988, 31, 499–500. [Google Scholar]
- Wei, L.; Qian, B.; Wang, W.; Wu, X.; Zhen, W.; Min, Z. Chinese Version of the Perceived Stress Scale-10: A Psychometric Study in Chinese University Students. PLoS ONE 2017, 12, e0189543. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Carpenter, J.S.; Andrykowski, M.A. Psychometric Evaluation of the Pittsburgh Sleep Quality Index. J. Psychosom. Res. 1998, 45, 5–13. [Google Scholar] [CrossRef]
- Liu, X.C.; Tang, M.Q. Reliability and Validity of the Pittsburgh Sleep Quality Index (Chinese Version). Chinese J. Psychiatry 1996, 29, 103–107. [Google Scholar]
- Beck, A.T.; Kovacs, M.; Weissman, A. Assessment of Suicidal Intention: The Scale for Suicide Ideation. J. Consult. Clin. Psychol. 1979, 47, 343–352. [Google Scholar] [CrossRef]
- Beck, A.T.; Brown, G.K.; Steer, R.A. Psychometric Characteristics of the Scale for Suicide Ideation with Psychiatric Outpatients. Behav. Res. Ther. 1997, 35, 1039–1046. [Google Scholar] [CrossRef]
- Zhang, J.; Lester, D.; Zhao, S.; Zhou, C. Suicidal Ideation and Its Correlates: Testing the Interpersonal Theory of Suicide in Chinese Students. Arch. Suicide Res. 2013, 17, 236–241. [Google Scholar] [CrossRef]
- de Beurs, D.P.; Fokkema, M.; O’Connor, R.C. Optimizing the Assessment of Suicidal Behavior: The Application of Curtailment Techniques. J. Affect. Disord. 2016, 196, 218–224. [Google Scholar] [CrossRef] [Green Version]
- Osman, A.; Bagge, C.L.; Gutierrez, P.M.; Konick, L.C.; Kopper, B.A.; Barrios, F.X. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with Clinical and Nonclinical Samples. Assessment 2001, 8, 443–454. [Google Scholar] [CrossRef]
- Zhao, J.; Zhao, J.; Rong, X.; Yang, X.; Zhang, X. Suicide Exposure and Its Modulatory Effects on Relations between Life Events and Suicide Risk in Chinese College Students. Nan Fang Yi Ke Da Xue Xue Bao (J. South. Med. Univ.) 2013, 33, 1111–1116. [Google Scholar]
- Byrne, B.M. Structural Equation Modeling with AMOS, EQS, and LISREL: Comparative Approaches to Testing for the Factorial Validity of a Measuring Instrument. Int. J. Test. 2001, 1, 55–86. [Google Scholar] [CrossRef]
- Bentler, P.M. Comparative Fit Indexes in Structural Models. Psychol. Bull. 1990, 107, 238. [Google Scholar] [CrossRef] [PubMed]
- Kline, R. Principles and Practice of Structural Equation Modeling, 2nd ed.; Guilford Publications: New York, NY, USA, 2005. [Google Scholar]
- Kshtriya, S.; Kobezak, H.M.; Popok, P.; Lawrence, J.; Lowe, S.R. Social Support as a Mediator of Occupational Stressors and Mental Health Outcomes in First Responders. J. Community Psychol. 2020, 48, 2252–2263. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Q.; Dong, M.-X.; Yao, J.; Li, W.-X.; Ye, D.-Q. Parental Alcoholism, Adverse Childhood Experiences, and Later Risk of Personal Alcohol Abuse among Chinese Medical Students. Biomed. Environ. Sci. 2008, 21, 411–419. [Google Scholar] [CrossRef]
- King, E.; Steenson, C.; Shannon, C.; Mulholland, C. Prevalence Rates of Childhood Trauma in Medical Students: A Systematic Review. BMC Med. Educ. 2017, 17, 159. [Google Scholar] [CrossRef] [Green Version]
- Devi, F.; Shahwan, S.; Teh, W.L.; Sambasivam, R.; Zhang, Y.J.; Lau, Y.W.; Ong, S.H.; Fung, D.; Gupta, B.; Chong, S.A.; et al. The Prevalence of Childhood Trauma in Psychiatric Outpatients. Ann. Gen. Psychiatry 2019, 18, 15. [Google Scholar] [CrossRef] [Green Version]
- Wu, R.; Zhu, H.; Wang, Z.J.; Jiang, C.L. A Large Sample Survey of Suicide Risk among University Students in China. BMC Psychiatry 2021, 21, 474. [Google Scholar] [CrossRef]
- Khosravani, V.; Kamali, Z.; Jamaati Ardakani, R.; Samimi Ardestani, M. The Relation of Childhood Trauma to Suicide Ideation in Patients Suffering from Obsessive–Compulsive Disorder with Lifetime Suicide Attempts. Psychiatry Res. 2017, 255, 139. [Google Scholar] [CrossRef]
- Alter, S.; Wilson, C.; Sun, S.; Harris, R.E.; Wang, Z.; Vitale, A.; Hazlett, E.A.; Goodman, M.; Ge, Y.; Yehuda, R.; et al. The Association of Childhood Trauma with Sleep Disturbances and Risk of Suicide in US Veterans. J. Psychiatr. Res. 2021, 136, 54–62. [Google Scholar] [CrossRef]
- Norman, R.E.; Byambaa, M.; De, R.; Butchart, A.; Scott, J.; Vos, T. The Long-Term Health Consequences of Child Physical Abuse, Emotional Abuse, and Neglect: A Systematic Review and Meta-Analysis. PLoS Med. 2012, 9, e1001349. [Google Scholar] [CrossRef] [Green Version]
- Gama, C.M.F.; Portugal, L.C.L.; Gonçalves, R.M.; de Souza Junior, S.; Vilete, L.M.P.; Mendlowicz, M.V.; Figueira, I.; Volchan, E.; David, I.A.; de Oliveira, L.; et al. The Invisible Scars of Emotional Abuse: A Common and Highly Harmful Form of Childhood Maltreatment. BMC Psychiatry 2021, 21, 156. [Google Scholar] [CrossRef] [PubMed]
- Strathearn, L.; Giannotti, M.; Mills, R.; Kisely, S.; Najman, J.; Abajobir, A. Long-Term Cognitive, Psychological, and Health Outcomes Associated with Child Abuse and Neglect. Pediatrics 2020, 146, e20200438. [Google Scholar] [CrossRef] [PubMed]
- Martins, C.M.S.; Von Werne Baes, C.; Tofoli, S.M.d.C.; Juruena, M.F. Emotional Abuse in Childhood Is a Differential Factor for the Development of Depression in Adults. J. Nerv. Ment. Dis. 2014, 202, 774–782. [Google Scholar] [CrossRef]
- Nelson, J.; Klumparendt, A.; Doebler, P.; Ehring, T. Childhood Maltreatment and Characteristics of Adult Depression: Meta-Analysis. Br. J. Psychiatry 2017, 210, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Christ, C.; De Waal, M.M.; Dekker, J.J.M.; van Kuijk, I.; Van Schaik, D.J.F.; Kikkert, M.J.; Goudriaan, A.E.; Beekman, A.T.F.; Messman-Moore, T.L. Linking Childhood Emotional Abuse and Depressive Symptoms: The Role of Emotion Dysregulation and Interpersonal Problems. PLoS ONE 2019, 14, e0211882. [Google Scholar] [CrossRef]
- Trockel, M.; Karlin, B.E.; Taylor, C.B.; Brown, G.K.; Manber, R. Effects of Cognitive Behavioral Therapy for Insomnia on Suicidal Ideation in Veterans. Sleep 2015, 38, 259–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCauley, E.; Berk, M.S.; Asarnow, J.R.; Adrian, M.; Cohen, J.; Korslund, K.; Avina, C.; Hughes, J.; Harned, M.; Gallop, R.; et al. Efficacy of Dialectical Behavior Therapy for Adolescents at High Risk for Suicide: A Randomized Clinical Trial. JAMA Psychiatry 2018, 75, 777–785. [Google Scholar] [CrossRef] [Green Version]
- Mohamadi, J.; Ghazanfari, F.; Drikvand, F.M. Comparison of the Effect of Dialectical Behavior Therapy, Mindfulness Based Cognitive Therapy and Positive Psychotherapy on Perceived Stress and Quality of Life in Patients with Irritable Bowel Syndrome: A Pilot Randomized Controlled Trial. Psychiatr. Q. 2019, 90, 565–578. [Google Scholar] [CrossRef]
- Wu, R.; Zhong, S.Y.; Wang, G.H.; Wu, M.Y.; Xu, J.F.; Zhu, H.; Liu, L.L.; Su, W.J.; Cao, Z.Y.; Jiang, C.L. The Effect of Brief Mindfulness Meditation on Suicidal Ideation, Stress and Sleep Quality. Arch. Suicide Res. 2021, 1–16. [Google Scholar] [CrossRef]
- Xiong, W.; Huang, J.; Zhu, A. The Relationship of Sleep Quality among Internship Nurses with Clinical Learning Environment and Mental Stress: A Cross-Sectional Survey. Sleep Med. 2021, 83, 151–158. [Google Scholar] [CrossRef]
| Variables | N | % | |
|---|---|---|---|
| Sex | Male | 214 | 27.4 |
| Female | 566 | 72.6 | |
| Education | Undergraduate | 647 | 82.9 |
| Graduate | 133 | 17.1 | |
| Major | Liberal Arts | 208 | 39.5 |
| Science and Engineering | 472 | 60.5 | |
| School | Key University | 273 | 35 |
| General University | 222 | 28.5 | |
| Vocational college | 285 | 36.5 |
| Variables | M (SD) | Prevalence | ||||||
|---|---|---|---|---|---|---|---|---|
| All | SSI Total ≥ 6 | SBQ Total ≥ 7 | ||||||
| Cutoffs | n | % | n | % | n | % | ||
| CTQ EA | 7.38 (2.97) | CTQ EA ≥ 13 | 60 | 7.7 | 44.0 | 73.3 | 46.0 | 76.7 |
| CTQ PA | 6.07 (2.08) | CTQ PA ≥ 10 | 47 | 6.0 | 33.0 | 70.2 | 27.0 | 57.4 |
| CTQ SA | 5.86 (2.03) | CTQ SA ≥ 8 | 95 | 7.9 | 42.0 | 44.2 | 36.0 | 37.9 |
| CTQ EN | 10.36 (4.69) | CTQ EN ≥ 15 | 135 | 17.3 | 79.0 | 58.5 | 65.0 | 48.1 |
| CTQ PN | 7.92 (2.82) | CTQ PN ≥ 10 | 199 | 25.5 | 90.0 | 45.2 | 73.0 | 36.7 |
| CTQ Total | 37.59 (10.89) | |||||||
| PSS Total | 19.60 (4.94) | |||||||
| PSQI Total | 6.63 (3.00) | PSQI Total > 7 | 281 | 36.0 | ||||
| SSI Total | 5.35 (5.11) | SSI Total ≥ 6 | 262 | 33.6 | ||||
| SBQ Total | 5.23 (2.88) | SBQ Total ≥ 7 | 206 | 26.4 | ||||
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1 CTQ EA | 1.00 | ||||||||
| 2 CTQ PA | 0.60 *** | ||||||||
| 3 CTQ SA | 0.33 *** | 0.39 *** | |||||||
| 4 CTQ EN | 0.48 *** | 0.33 *** | 0.22 *** | ||||||
| 5 CTQ PN | 0.45 *** | 0.37 *** | 0.31 *** | 0.65 *** | |||||
| 6 CTQ Total | 0.77 *** | 0.67 *** | 0.53 *** | 0.84 *** | 0.79 *** | ||||
| 7 PSS Total | 0.25 *** | 0.19 *** | 0.07 | −0.06 | −0.01 | 0.09 * | |||
| 8 PSQI Total | 0.23 *** | 0.20 *** | 0.10 ** | 0.18 *** | 0.17 *** | 0.24 *** | 0.34 *** | ||
| 9 SSI Total | 0.50 *** | 0.35 *** | 0.11 ** | 0.35 *** | 0.28 *** | 0.44 *** | 0.21 *** | 0.30 *** | |
| 10 SBQ Total | 0.50 *** | 0.29 *** | 0.14 *** | 0.29 *** | 0.22 *** | 0.40 *** | 0.27 *** | 0.32 *** | 0.76 *** |
| Percentile 95%CI | |||
|---|---|---|---|
| Model Pathways | The Standardized Meditating Effects | Lower | Upper |
| Model 1 | 0.25 × 0.30 × 0.19 × 0.66 = 0.01 | 0.003 | 0.022 |
| Model 2 | 0.25 × 0.30 × 0.06 = 0.005 | 0.0003 | 0.013 |
| Model 3 | 0.25 × 0.08 = 0.02 | 0.006 | 0.040 |
| Model 4 | 0.16 × 0.19 × 0.66 = 0.02 | 0.005 | 0.045 |
| Model 5 | 0.16 × 0.06 = 0.01 | 0.001 | 0.026 |
| Model 6 | 0.45 × 0.66 = 0.30 | 0.218 | 0.382 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, R.; Zhu, H.; Wu, M.-Y.; Wang, G.-H.; Jiang, C.-L. Childhood Trauma and Suicide: The Mediating Effect of Stress and Sleep. Int. J. Environ. Res. Public Health 2022, 19, 8493. https://doi.org/10.3390/ijerph19148493
Wu R, Zhu H, Wu M-Y, Wang G-H, Jiang C-L. Childhood Trauma and Suicide: The Mediating Effect of Stress and Sleep. International Journal of Environmental Research and Public Health. 2022; 19(14):8493. https://doi.org/10.3390/ijerph19148493
Chicago/Turabian StyleWu, Ran, Hong Zhu, Meng-Yang Wu, Guang-Hai Wang, and Chun-Lei Jiang. 2022. "Childhood Trauma and Suicide: The Mediating Effect of Stress and Sleep" International Journal of Environmental Research and Public Health 19, no. 14: 8493. https://doi.org/10.3390/ijerph19148493
APA StyleWu, R., Zhu, H., Wu, M.-Y., Wang, G.-H., & Jiang, C.-L. (2022). Childhood Trauma and Suicide: The Mediating Effect of Stress and Sleep. International Journal of Environmental Research and Public Health, 19(14), 8493. https://doi.org/10.3390/ijerph19148493





