Balancing Mission and Margins: What Makes Healthy Community Food Stores Successful
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
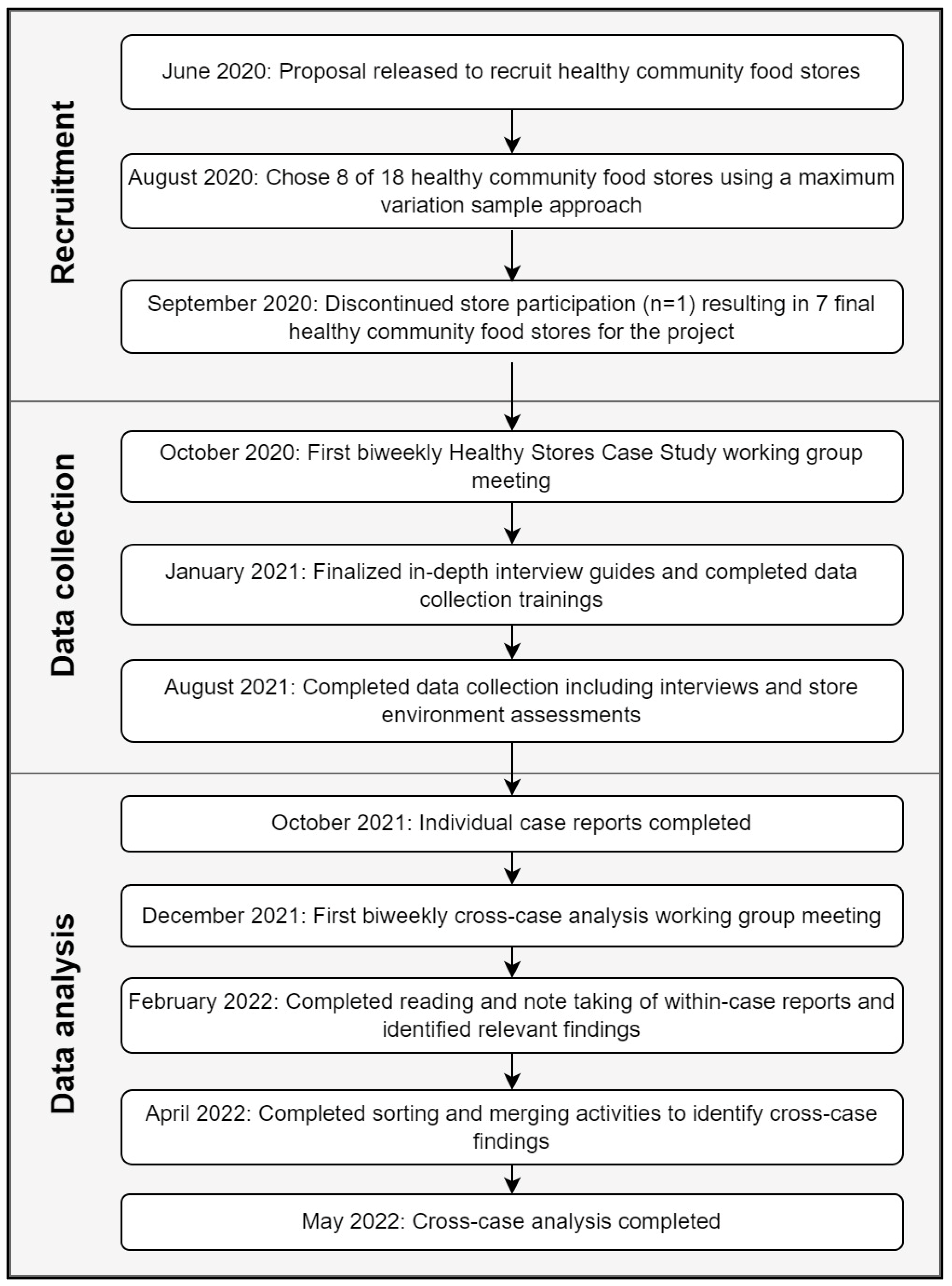
2.2. Recruitment and Data Collection
2.2.1. Recruitment
2.2.2. Data Collection
2.3. Analysis
2.3.1. Healthy Food Availability Healthy Eating Index (HFAHEI)
2.3.2. Food Affordability Indicator
2.3.3. Individual Case Reports
2.3.4. Stake Multiple Case Study Analysis
2.4. Ethical Considerations
3. Results
3.1. What Does Success Look like for a Healthy Community Store?
3.1.1. Store Commitment to Providing Healthy Food
“Let’s just say for instance, I brought in a case of a new product that’s low in fat, low in sugar, and I put it on my shelf. And people are hesitant to buy that product because of the perception that it’s probably less tasty to them… A lot of store owners, a lot of small business store owners are hesitant to even bring in that product from the very beginning for that very reason”.(Chicago store owner)
“Don’t give up if you don’t sell today…when I started, I started just bringing one banana, one case. Now we sell almost 12, 15 in every week”.
“The last thing [customers] need is for a spot like [our store] to carry soda and cookies and candy stuff, particularly at a discount. That would be not helpful for our mission”.(Boston store founder)
“…we don’t specifically say healthful as a criteria, but I think the combination of what we do prioritize, I think results in what many people would describe as healthful… those decisions are very intentional. Our fresh foods are the majority of what we prioritize from the merchandising standpoint”.(Minneapolis store leader)
3.1.2. Store Commitment to Making Healthy Foods Affordable
“Because sometimes, you know we’re smaller, we’re not getting a big bulk discount like a larger grocer would, so we don’t have the best costs in town and we’re trying to provide the best prices”.(Boston store employee)
“…the hard rub is that there’s a lot of people in poverty in our country and it’s gotten worse… they can’t afford food that is premised on not having people in poverty. So there is a disconnect there that we…can’t reconcile it. We can’t make the food at the price that they can afford”.(Minneapolis store leader)
“They’ll ask me, ‘are you sure you rang everything up?’—they can’t believe the amount of food they’re getting for that price. It can bring them to tears”.(Boston store employee)
3.1.3. Store Commitment to Reaching Community Members with Limited Economic Resources
“I feel like a lot of the mistrust with [the supermarket], too, is that you know just in the past, a lot of grocery stores in the neighborhood have not had that quality produce, quality products, just in general. And to be able to, you know, make sure people establish a trust issue, I feel like doing stuff with the kids, doing stuff with the youth, doing stuff more community based, and can kind of help, you know, instill that trust”.(Detroit store customer)
“Our customer mix is fairly indicative of the demographics of our community and that is our goal. I mean we really want our store to look and feel like our community”.(DC store manager)
3.2. What Strategies Lead to Healthy Community Store Success?
3.2.1. Having a Store Champion
“He’s constantly trying to expand his reach; he’s constantly trying to support more folks, whether it is through his store or just within the community”.(Buffalo store owner)
“If [store founder] couldn’t do it, no one could do it. He was basically trying to leverage everything that he had learned and everyone that he knew in order to make [the store] work”.(Boston store funder)
“[The store] was basically left to its own devices and there was no, no general oversight above the manager”.(Baltimore store leader)
3.2.2. Using Nontraditional Business Strategies
“…we have some funders who are non-profits who fund directly into the store, we have others who fund into [the parent non-profit] with the provision that those funds get passed directly through to the store, and then we have a few that are funding [the parent non-profit] in order to support [the parent non-profit’s] activities directly”.(DC store leader)
“…[letting] go some of our other [natural food] product standards in order to be more accessible in our community… have a more affordable option”.(Minneapolis store leader)
“We always want to be lower than those comp prices, but how much lower we are kind of depends on the cost, and you know how essential we think it is…like how much we think people want to see it in the store”.(Boston store employee)
3.2.3. Obtaining Innovative External Funding
“There were probably at least one, maybe two points, in our funding cycle and [store’s] sort of life cycle, where, you know, I felt, and I think [founder] would agree, you know, but for us [the foundation], [the store] would not still exist”.(Boston store funder)
“I’m not asking them to fund a food pantry where we’re giving food away. I’m asking them to fund a business, and so when people put money into a business, they expect a return generally on that investment. There isn’t one”.(Baltimore store leader)
3.2.4. Using a Dynamic Sourcing Model
“…reassurance to the farmer and with us that we’ll be buying that product, and we can count on them to deliver that product”.(Minneapolis store leader)
“This logistics company called us, and they said they had 300 cases of bags of snap peas. And [a supermarket chain] had rejected them because they didn’t quite like the quality… so I started asking the questions like ‘what’s the code date? what do they look like? what can we retail these for? what do they sell for elsewhere?’ These are like $3.99 you know, they’re 12 oz bag of snap peas, that you would see at [a supermarket chain]. And so we took them; we sent one pallet to each store and we’re selling them [for] 49 cents. And they had like two weeks of code on them so that was part of the determining factor to say ‘okay these are getting donated to us, this is not costing us anything;’ they dropped them off”.(Boston store employee)
“…the reason they were the only one is because we did reach out to several, and they were the only one that was willing to work with us... All of other independent grocers have more locations so they scaled their pricing way down... They allowed us to order in smaller quantities at a higher [unit] price”.(Baltimore store leader)
3.2.5. Implementing Healthy Food Marketing
“You don’t see beer, or you don’t see candy, what we do is put the cooler [of fruit cups and fresh produce] in front of you so the people see it right away”.(Buffalo store owner)
“When you walk into a corner store, like mine. You will find all the junk food a front…because those items are our items that are proven that are … well known for being an impulse buy”.(Chicago store owner)
3.2.6. Engaging the Local Community
“…they feel that he is part of the community. And so, people are very protective, very supportive... And so, he set up shop where others would not, and people appreciate that”.(Buffalo store stakeholder)
“We are a community-owned organization. Our owners are not investors, they are community members”.(Minneapolis store leader)
“…the store was never placed in a food desert, so there was no overriding reason to drive people to the store because they could go to a [grocery store chain], the [grocery store chain] was half a mile from our store”.(Baltimore store leader)
3.3. How Did Stores Balance Missions and Margins to Achieve Success?
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Key Concepts | Definitions |
|---|---|
| Food system | All the elements (environment, people, inputs, processes, infrastructure, institutions, markets, and trade) and activities that relate to the production, processing, distribution, marketing, preparation, and consumption of food and the outputs of these activities, including socioeconomic and environmental outcomes [63] |
| Food environment | The physical, social, economic, cultural, and political factors that impact the accessibility, availability, and adequacy of food within a community or region [64] |
| Food access | Availability, accessibility, affordability, accommodation, and acceptability of food [65] |
| Food desert | Low-income census tract with low access to a supermarket or large grocery store [66] |
| Food apartheid | An alternate term for food desert to acknowledge the human decisions and actions that have created these inequitable food environments [67] |
| Nutrition security | Consistent access to safe, healthy, affordable foods essential to optimal health and well-being [68] |
| Nutrition-related disease | Diseases associated with poor dietary patterns including heart disease, type 2 diabetes, and heart disease [69] |
Appendix B
References
- Rhone, A.; Ver Ploeg, M.; Dicken, C.; Williams, R.; Breneman, V. Low-Income and Low-Supermarket-Access Census Tracts, 2010–2015; EIB-165; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2017.
- Rhone, A.; Ver Ploeg, M.; Williams, R.; Breneman, V. Understanding Low-Income and Low-Access Census Tracts Across the Nation: Subnational and Subpopulation Estimates of Access to Healthy Food; EIB-209; U.S. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2019.
- Dickinson, M. Black agency and food access: Leaving the food desert narrative behind. City 2019, 23, 690–693. [Google Scholar] [CrossRef]
- Powell, L.M.; Slater, S.; Mirtcheva, D.; Bao, Y.; Chaloupka, F.J. Food store availability and neighborhood characteristics in the United States. Prev. Med. 2007, 44, 189–195. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services. Obama Administration Details Healthy Food Financing Initiative; The Administration for Children and Families: Washington, DC, USA, 2010.
- The Agricultural Act of 2014. H.R. 2642. 2014. Available online: https://www.congress.gov/bill/113th-congress/house-bill/2642 (accessed on 16 March 2022).
- Agricultural Improvement Act of 2018. H.R.2. 2018. Available online: https://www.congress.gov/bill/115th-congress/house-bill/2 (accessed on 16 March 2022).
- Allcott, H.; Diamond, R.; Dubé, J.-P.; Handbury, J.; Rahkovsky, I.; Schnell, M. Food Deserts and the Causes of Nutritional Inequality. Q. J. Econ. 2019, 134, 1793–1844. [Google Scholar] [CrossRef]
- Ghosh-Dastidar, M.; Hunter, G.; Collins, R.L.; Zenk, S.N.; Cummins, S.; Beckman, R.; Nugroho, A.K.; Sloan, J.C.; Wagner, L.; Dubowitz, T. Does opening a supermarket in a food desert change the food environment? Health Place 2017, 46, 249–256. [Google Scholar] [CrossRef]
- Dubowitz, T.; Ghosh-Dastidar, M.; Cohen, D.A.; Beckman, R.; Steiner, E.D.; Hunter, G.P.; Flórez, K.; Huang, C.; Vaughan, C.A.; Sloan, J.C.; et al. Diet and Perceptions Change With Supermarket Introduction In A Food Desert, But Not Because Of Supermarket Use. Health Aff. 2015, 34, 1858–1868. [Google Scholar] [CrossRef] [Green Version]
- Hollis-Hansen, K.; Vermont, L.; Zafron, M.L.; Seidman, J.; Leone, L. The introduction of new food retail opportunities in lower-income communities and the impact on fruit and vegetable intake: A systematic review. Transl. Behav. Med. 2019, 9, 837–846. [Google Scholar] [CrossRef]
- Caspi, C.E.; Pelletier, J.E.; Harnack, L.; Erickson, D.J.; Laska, M.N. Differences in healthy food supply and stocking practices between small grocery stores, gas-marts, pharmacies and dollar stores. Public Health Nutr. 2016, 19, 540–547. [Google Scholar] [CrossRef] [Green Version]
- Caspi, C.E.; Pelletier, J.E.; Harnack, L.J.; Erickson, D.J.; Lenk, K.; Laska, M.N. Pricing of Staple Foods at Supermarkets versus Small Food Stores. Int. J. Environ. Res. Public Health 2017, 14, 915. [Google Scholar] [CrossRef] [Green Version]
- Laska, M.N.; Borradaile, K.E.; Tester, J.; Foster, G.D.; Gittelsohn, J. Healthy food availability in small urban food stores: A comparison of four US cities. Public Health Nutr. 2010, 13, 1031–1035. [Google Scholar] [CrossRef] [Green Version]
- Gittelsohn, J.; Laska, M.N.; Karpyn, A.; Klingler, K.; Ayala, G.X. Lessons Learned from Small Store Programs to Increase Healthy Food Access. Am. J. Health Behav. 2014, 38, 307–315. [Google Scholar] [CrossRef] [Green Version]
- Ayala, G.X.; D’Angelo, H.; Gittelsohn, J.; Horton, L.; Ribisl, K.; Sindberg, L.S.; Olson, C.; Kharmats, A.; Laska, M.N. Who is behind the stocking of energy-dense foods and beverages in small stores? The importance of food and beverage distributors. Public Health Nutr. 2017, 20, 3333–3342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gittelsohn, J.; Ayala, G.X.; D’angelo, H.; Kharmats, A.; Ribisl, K.M.; Schmidt Sindberg, L.; Liverman, S.P.; Laska, M.N. Formal and informal agreements between small food stores and food and beverage suppliers: Store owner perspectives from four cities. J. Hunger. Environ. Nutr. 2018, 13, 517–530. [Google Scholar] [CrossRef]
- Laska, M.N.; Sindberg, L.S.; Ayala, G.X.; D’Angelo, H.; Horton, L.A.; Ribisl, K.M.; Kharmats, A.; Olson, C.; Gittelsohn, J. Agreements between small food store retailers and their suppliers: Incentivizing unhealthy foods and beverages in four urban settings. Food Policy 2018, 79, 324–330. [Google Scholar] [CrossRef]
- Jetter, K.M.; Cassady, D.L. Increasing Fresh Fruit and Vegetable Availability in a Low-Income Neighborhood Convenience Store: A Pilot Study. Health Promot. Pract. 2009, 11, 694–702. [Google Scholar] [CrossRef] [PubMed]
- Dannefer, R.; Williams, D.A.; Baronberg, S.; Silver, L. Healthy Bodegas: Increasing and Promoting Healthy Foods at Corner Stores in New York City. Am. J. Public Health 2012, 102, e27–e31. [Google Scholar] [CrossRef]
- Gittelsohn, J.; Trude, A.C.; Poirier, L.; Ross, A.; Ruggiero, C.; Schwendler, T.; Anderson Steeves, E. The Impact of a Multi-Level Multi-Component Childhood Obesity Prevention Intervention on Healthy Food Availability, Sales, and Purchasing in a Low-Income Urban Area. Int. J. Environ. Res. Public Health 2017, 14, 1371. [Google Scholar] [CrossRef] [Green Version]
- Steeves, E.A.; Penniston, E.; Rowan, M.; Steeves, J.; Gittelsohn, J. A Rural Small Food Store Pilot Intervention Creates Trends Toward Improved Healthy Food Availability. J. Hunger. Environ. Nutr. 2015, 10, 259–270. [Google Scholar] [CrossRef]
- Wensel, C.R.; Trude, A.C.B.; Poirier, L.; Alghamdi, R.; Trujillo, A.; Anderson Steeves, E.; Paige, D.; Gittelsohn, J. B’more Healthy Corner Stores for Moms and Kids: Identifying Optimal Behavioral Economic Strategies to Increase WIC Redemptions in Small Urban Corner Stores. Int. J. Environ. Res. Public Health 2019, 16, 64. [Google Scholar] [CrossRef] [Green Version]
- John, S.; Economos, C.; Rimm, E.; Cash, S.B.; Wilde, P. SNAP Financial Incentives Increase Fruit and Vegetable and Broader Food Spending in a Low-Income Grocery Retail Environment. In Proceedings of the 2020 APPAM Fall Research Conference, Washington, DC, USA, 11–13 November 2020. [Google Scholar]
- Thorndike, A.N.; Bright, O.-J.M.; Dimond, M.A.; Fishman, R.; Levy, D.E. Choice architecture to promote fruit and vegetable purchases by families participating in the Special Supplemental Program for Women, Infants, and Children (WIC): Randomized corner store pilot study. Public Health Nutr. 2017, 20, 1297–1305. [Google Scholar] [CrossRef] [Green Version]
- Trude, A.C.B.; Surkan, P.J.; Cheskin, L.J.; Gittelsohn, J. A multilevel, multicomponent childhood obesity prevention group-randomized controlled trial improves healthier food purchasing and reduces sweet-snack consumption among low-income African-American youth. Nutr. J. 2018, 17, 96. [Google Scholar] [CrossRef] [Green Version]
- Gittelsohn, J.; Kim, E.M.; He, S.; Pardilla, M. A Food Store–Based Environmental Intervention Is Associated with Reduced BMI and Improved Psychosocial Factors and Food-Related Behaviors on the Navajo Nation. J. Nutr. 2013, 143, 1494–1500. [Google Scholar] [CrossRef] [PubMed]
- Shin, A.; Surkan, P.J.; Coutinho, A.J.; Suratkar, S.R.; Campbell, R.K.; Rowan, M.; Sharma, S.; Dennisuk, L.A.; Karlsen, M.; Gass, A.; et al. Impact of Baltimore Healthy Eating Zones: An Environmental Intervention to Improve Diet Among African American Youth. Health Educ. Behav. 2015, 42, 97S–105S. [Google Scholar] [CrossRef] [PubMed]
- Harvey, D. Urban food co-op tackles economic empowerment. Race Poverty Environ. 2009, 16, 75–77. [Google Scholar]
- Creswell, J.W.; Poth, C.N. Qualitative Inquiry and Research Design: Choosing among Five Approaches; Sage Publications: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Gittelsohn, J.; Kasprzak, C.M.; Hill, A.B.; Sundermeir, S.M.; Laska, M.N.; Dombrowski, R.D.; DeAngelo, J.; Odoms-Young, A.; Leone, L.A. Increasing Healthy Food Access for Low-Income Communities: Protocol of the Healthy Community Stores Case Study Project. Int. J. Environ. Res. Public Health 2022, 19, 690. [Google Scholar] [CrossRef]
- Stake, R.E. Multiple Case Study Analysis; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Patton, M.Q. Qualitative Research & Evaluation Methods; Sage: Thousand Oaks, CA, USA, 2002. [Google Scholar]
- Glanz, K.; Sallis, J.F.; Saelens, B.E.; Frank, L.D. Nutrition Environment Measures Survey in Stores (NEMS-S): Development and Evaluation. Am. J. Prev. Med. 2007, 32, 282–289. [Google Scholar] [CrossRef]
- Odoms-Young, A.M.; Zenk, S.; Mason, M. Measuring Food Availability and Access in African-American Communities: Implications for Intervention and Policy. Am. J. Prev. Med. 2009, 36, S145–S150. [Google Scholar] [CrossRef]
- Hill, A.; Naar-King, S. Fruit and vegetable availability, quality, & consumption in Detroit’s food desert among African American adolescents with obesity. Food Nutr. 2014, 29, 14–19. [Google Scholar]
- Shaver, E.R.; Sadler, R.C.; Hill, A.B.; Bell, K.; Ray, M.; Choy-Shin, J.; Lerner, J.; Soldner, T.; Jones, A.D. The Flint Food Store Survey: Combining spatial analysis with a modified Nutrition Environment Measures Survey in Stores (NEMS-S) to measure the community and consumer nutrition environments. Public Health Nutr. 2018, 21, 1474–1485. [Google Scholar] [CrossRef] [Green Version]
- Santarossa, S.; Hill, A.B.; Sitarik, A.R.; Taylor, M.; Hawkins, S.; Scher, K.; Sohaski, A.; Baseer, M.; Dombrowski, R.; Plum, A.; et al. Food insecurity in Detroit: Exploring the relationship between patient-reported food insecurity and proximity to healthful grocery stores. Public Health Nutr. 2022, 25, 954–963. [Google Scholar] [CrossRef]
- Hill, A.B.; Sundermeir, S.M.; Kaur, R.; Dombrowski, R.D.; Gittelsohn, J. Healthy food availability for healthy eating: Evaluating the use of in-store measures in neighborhood food retail stores. Int. J. Environ. Res. Public Health 2022. under review. [Google Scholar]
- Franco, M.; Diez Roux, A.V.; Glass, T.A.; Caballero, B.; Brancati, F.L. Neighborhood Characteristics and Availability of Healthy Foods in Baltimore. Am. J. Prev. Med. 2008, 35, 561–567. [Google Scholar] [CrossRef]
- Campbell, E.A.; Shapiro, M.J.; Welsh, C.; Bleich, S.N.; Cobb, L.K.; Gittelsohn, J. Healthy Food Availability Among Food Sources in Rural Maryland Counties. J. Hunger. Environ. Nutr. 2017, 12, 328–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, A. “Treat everybody right”: Examining foodways to improve food access. J. Agric. Food Syst. Community Dev. 2021, 10, 9–16. [Google Scholar] [CrossRef]
- Gearing, M.; Dixit-Joshi, S.; May, L. Barriers That Constrain the Adequacy of Supplemental Nutrition Assistance Program (SNAP) Allotments: Survey Findings; U.S. Department of Agriculture, Food and Nutrition Service: Alexandria, VA, USA, 2021. Available online: https://fns-prod.azureedge.us/sites/default/files/resource-files/SNAP-Barriers-SurveyFindings.pdf (accessed on 26 May 2022).
- Bureau of Labor Statistics. Consumer Price Index: U.S. City Average, All Urban Consumers. 2021. Available online: https://www.bls.gov/cpi/data.htm (accessed on 1 May 2022).
- Dombrowski, R.D.; Bode, B.; Hill, A.B.; Kaur, R.; DeAngelo, J.; Colan-Ramos, U.; Odoms-Young, A. Ethno-cultural Differences Among Store Owners and Community Residents: Influences on Health Promoting Grocery Stores. Int. J. Environ. Res. Public Health 2022. under review. [Google Scholar]
- Kaur, R.; Winkler, M.R.; John, S.; DeAngelo, J.; Dombrowski, R.D.; Hickson, A.; Sundermeir, S.M.; Kasprzak, C.M.; Bode, B.; Hill, A.B.; et al. Exploring Community Engagement in Neighborhood Food Retail: Healthy Community Stores Case Study Project. Int. J. Environ. Res. Public Health 2022, 19, 6986. [Google Scholar] [CrossRef] [PubMed]
- Ford, A.F.; Reddick, K.; Browne, M.C.; Robins, A.; Thomas, S.B.; Crouse Quinn, S. Beyond the Cathedral: Building Trust to Engage the African American Community in Health Promotion and Disease Prevention. Health Promot. Pract. 2009, 10, 485–489. [Google Scholar] [CrossRef]
- Linnan, L.A.; Ferguson, Y.O. Beauty Salons: A Promising Health Promotion Setting for Reaching and Promoting Health among African American Women. Health Educ. Behav. 2006, 34, 517–530. [Google Scholar] [CrossRef] [PubMed]
- Meade, C.D.; Menard, J.M.; Luque, J.S.; Martinez-Tyson, D.; Gwede, C.K. Creating community-academic partnerships for cancer disparities research and health promotion. Health Promot. Pract. 2011, 12, 456–462. [Google Scholar] [CrossRef] [Green Version]
- Releford, B.J.; Frencher, S.K., Jr.; Yancey, A.K. Health promotion in barbershops: Balancing outreach and research in African American communities. Ethn. Dis. 2010, 20, 185–188. [Google Scholar]
- Cannuscio, C.C.; Tappe, K.; Hillier, A.; Buttenheim, A.; Karpyn, A.; Glanz, K. Urban Food Environments and Residents’ Shopping Behaviors. Am. J. Prev. Med. 2013, 45, 606–614. [Google Scholar] [CrossRef]
- Gustafson, A.; Lewis, S.; Perkins, S.; Wilson, C.; Buckner, E.; Vail, A. Neighbourhood and consumer food environment is associated with dietary intake among Supplemental Nutrition Assistance Program (SNAP) participants in Fayette County, Kentucky. Public Health Nutr. 2013, 16, 1229–1237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byker Shanks, C.; Ahmed, S.; Smith, T.; Houghtaling, B.; Jenkins, M.; Margetts, M.; Schultz, D.; Stephens, L. Availability, Price, and Quality of Fruits and Vegetables in 12 Rural Montana Counties, 2014. Prev. Chronic. Dis. 2015, 12, E128. [Google Scholar] [CrossRef] [PubMed]
- Krukowski, R.A.; West, D.S.; Harvey-Berino, J.; Elaine Prewitt, T. Neighborhood Impact on Healthy Food Availability and Pricing in Food Stores. J. Community Health 2010, 35, 315–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fretts, A.M.; Huber, C.; Best, L.G.; O’Leary, M.; LeBeau, L.; Howard, B.V.; Siscovick, D.S.; Beresford, S.A. Availability and Cost of Healthy Foods in a Large American Indian Community in the North-Central United States. Prev. Chronic. Dis. 2018, 15, E03. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Houghtaling, B.; Cater, M.; Bryant, D.J.; Brooks, A.; Holston, D. What is the availability, affordability, and quality of foods and beverages aligned with dietary guidance in Louisiana Supplemental Nutrition Assistance Program (SNAP) authorized stores? Prev. Med. Rep. 2021, 24, 101578. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Donate, A.P.; Riggall, A.J.; Meinen, A.M.; Malecki, K.; Escaron, A.L.; Hall, B.; Menzies, A.; Garske, G.; Nieto, F.J.; Nitzke, S. Evaluation of a pilot healthy eating intervention in restaurants and food stores of a rural community: A randomized community trial. BMC Public Health 2015, 15, 136. [Google Scholar] [CrossRef] [Green Version]
- Rushakoff, J.A.; Zoughbie, D.E.; Bui, N.; DeVito, K.; Makarechi, L.; Kubo, H. Evaluation of Healthy2Go: A country store transformation project to improve the food environment and consumer choices in Appalachian Kentucky. Prev. Med. Rep. 2017, 7, 187–192. [Google Scholar] [CrossRef]
- Samuels, S.E.; Craypo, L.; Boyle, M.; Crawford, P.B.; Yancey, A.; Flores, G. The California Endowment’s Healthy Eating, Active Communities program: A midpoint review. Am. J. Public Health 2010, 100, 2114–2123. [Google Scholar] [CrossRef]
- Gittelsohn, J.; Song, H.-J.; Suratkar, S.; Kumar, M.B.; Henry, E.G.; Sharma, S.; Mattingly, M.; Anliker, J.A. An Urban Food Store Intervention Positively Affects Food-Related Psychosocial Variables and Food Behaviors. Health Educ. Behav. 2009, 37, 390–402. [Google Scholar] [CrossRef]
- Dombrowski, R.D.; Kelley, M.A. Corner Store Owners as Health Promotion Agents in Low-Income Communities. Health Educ. Behav. 2019, 46, 905–915. [Google Scholar] [CrossRef]
- Healthy Food Access Program. HB2382. 2022. Available online: https://www.ilga.gov/legislation/BillStatus.asp?DocNum=2382&GAID=16&DocTypeID=HB&SessionID=110&GA=102 (accessed on 8 May 2022).
- United Nations. High Level Task Force on Global Food and Nutrition Security. All Food Systems Are Sustainable. Available online: https://www.un.org/en/issues/food/taskforce/wg3.shtml#:~:text=A%20food%20system%20is%20defined,the%20outputs%20of%20these%20activities%2C (accessed on 28 June 2022).
- Rideout, K.; Mah, C.L.; Minaker, L. Food Environments: An Introduction for Public Health Practice; National Collaborating Centre for Environmental Health: Vancouver, BC, Canada, 2015.
- Caspi, C.E.; Sorensen, G.; Subramanian, S.V.; Kawachi, I. The local food environment and diet: A systematic review. Health Place 2012, 18, 1172–1187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- U.S. Department of Agriculture Economic Research Service. Food Access Research Atlas Documentation. Available online: https://www.ers.usda.gov/data-products/food-access-research-atlas/documentation (accessed on 28 June 2022).
- Brones, A. Karen Washington: It’s Not a Food Desert, It’s Food Apartheid. Available online: https://www.guernicamag.com/karen-washington-its-not-a-food-desert-its-food-apartheid/ (accessed on 28 June 2022).
- U.S. Department of Agriculture. Our Commitment to Enhancing Food and Nutrition Security. Available online: https://www.usda.gov/nutrition-security (accessed on 28 June 2022).
- Centers for Disease Control and Prevention. About Nutrition. Available online: https://www.cdc.gov/nutrition/about-nutrition/index.html (accessed on 28 June 2022).

| Store Location | Operating Dates | Financial Model | Store Type | Store Size |
|---|---|---|---|---|
| Baltimore, MD, USA | 2018–2021 | Non-profit | Grocery store | 7000 sq ft |
| Boston, MA, USA | 2015–present | Non-profit | Grocery store | 3850 sq ft |
| Buffalo, NY, USA | 2007–present | For-profit | Corner store | -- |
| Chicago, IL, USA | 2003–present | For-profit | Corner store | 3500 sq ft |
| Detroit, MI, USA | 1984–present | For-profit | Supermarket | 65,000 sq ft |
| Minneapolis, MN, USA | 1970s–present | Co-op | Grocery store | 20,000 sq ft |
| Washington, DC, USA | 2014–present | For-profit | Market | 900 sq ft |
| Stores | |||||||
|---|---|---|---|---|---|---|---|
| Components of Success | BAL | BOS | BUFF | CHI | DC | DET | MINN |
| Store commitment to healthy food | |||||||
| Store acknowledged importance of healthy food (Intention) | √ | √ | √ | √ | √ | √ | √ |
| Store defined “healthy” (Action) | √ | √ | √ | ||||
| Store defined “healthy” food (Action) | √ | ||||||
| Store operationalized “healthy” (Action) | √ | √ | √ | √ | |||
| Store provided a wide variety of healthy foods 1 (Achievement) | √ | √ | √ | √ | |||
| Store commitment to affordable prices | |||||||
| Store acknowledged importance of affordable prices (Intention) | √ | √ | √ | √ | √ | √ | √ |
| Store altered business model to offer affordable prices (Action) | √ | √ | √ | √ | √ | √ | |
| Store provided affordable prices 2 (Achievement) | √ | √ | √ | ||||
| Store commitment to reaching community with limited economic resources | |||||||
| Store acknowledged importance of reaching community (Intention) | √ | √ | √ | √ | √ | √ | √ |
| Store engaged with community (Action) | √ | √ | √ | √ | √ | √ | |
| Store customer base reflected community 3 (Achievement) | √ | √ | √ | √ | √ | √ | |
| Stores | ||||||||
|---|---|---|---|---|---|---|---|---|
| Strategies | Examples | BAL | BOS | BUFF | CHI | DC | DET | MINN |
| Had a store champion | Store owner(s) | x | √ | √ | √ | √ | √ | |
| Store founder | ||||||||
| Non-profit board | ||||||||
| Used nontraditional business strategies | Non-profit, co-op model Lower profit margins Needs-based discounts | √ | √ | √ | √ | √ | ||
| Obtained innovative external funding | Grants City development funds Philanthropic funds | √ | √ | √ | √ | √ | ||
| Used a dynamic sourcing model | Sourced from a variety of vendors (wholesaler, farmer, gleaner) Opportunity buys Collective purchasing | √ | √ | √ | √ | |||
| Implemented healthy food marketing | Stocked healthy products Prominent healthy item placement Price discounts on healthy items Promoted healthy products | √ | √ | √ | √ | √ | √ | √ |
| Engaged local community | Input on store location Collaborated with CBOs Offered engagement activities (cooking classes, yoga) | √ | √ | √ | √ | √ | √ | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
John, S.; Winkler, M.R.; Kaur, R.; DeAngelo, J.; Hill, A.B.; Sundermeir, S.M.; Colon-Ramos, U.; Leone, L.A.; Dombrowski, R.D.; Lewis, E.C.; et al. Balancing Mission and Margins: What Makes Healthy Community Food Stores Successful. Int. J. Environ. Res. Public Health 2022, 19, 8470. https://doi.org/10.3390/ijerph19148470
John S, Winkler MR, Kaur R, DeAngelo J, Hill AB, Sundermeir SM, Colon-Ramos U, Leone LA, Dombrowski RD, Lewis EC, et al. Balancing Mission and Margins: What Makes Healthy Community Food Stores Successful. International Journal of Environmental Research and Public Health. 2022; 19(14):8470. https://doi.org/10.3390/ijerph19148470
Chicago/Turabian StyleJohn, Sara, Megan R. Winkler, Ravneet Kaur, Julia DeAngelo, Alex B. Hill, Samantha M. Sundermeir, Uriyoan Colon-Ramos, Lucia A. Leone, Rachael D. Dombrowski, Emma C. Lewis, and et al. 2022. "Balancing Mission and Margins: What Makes Healthy Community Food Stores Successful" International Journal of Environmental Research and Public Health 19, no. 14: 8470. https://doi.org/10.3390/ijerph19148470
APA StyleJohn, S., Winkler, M. R., Kaur, R., DeAngelo, J., Hill, A. B., Sundermeir, S. M., Colon-Ramos, U., Leone, L. A., Dombrowski, R. D., Lewis, E. C., & Gittelsohn, J. (2022). Balancing Mission and Margins: What Makes Healthy Community Food Stores Successful. International Journal of Environmental Research and Public Health, 19(14), 8470. https://doi.org/10.3390/ijerph19148470







