Knowledge, Attitudes, and Stigma: The Perceptions of Tuberculosis in Equatorial Guinea
Abstract
1. Introduction
2. Materials and Methods
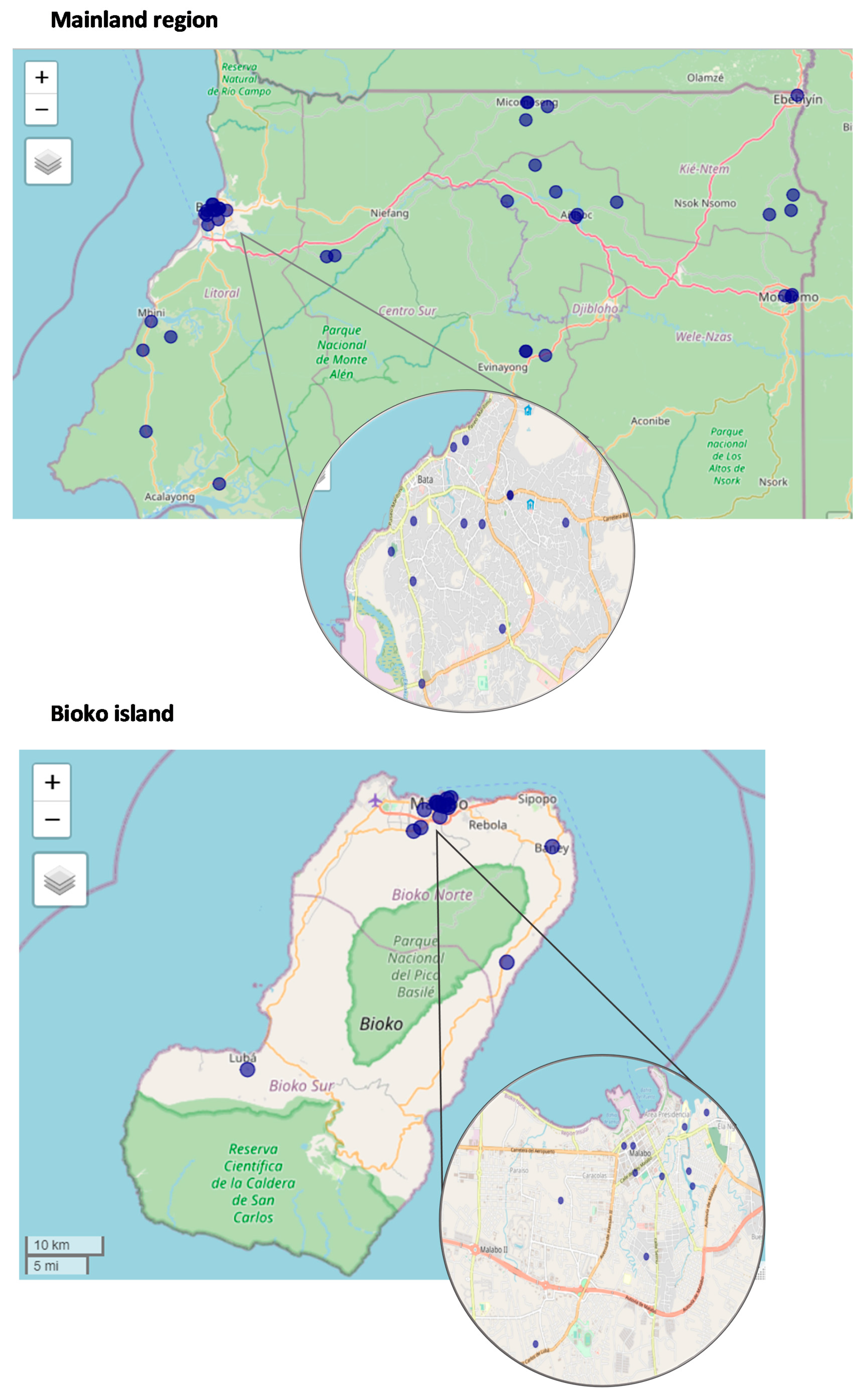
2.1. Study Area and Population
2.2. Study Design, Sample, and Data Collection
2.3. Variables
2.3.1. Knowledge Score
2.3.2. Attitudes Score
2.3.3. Stigma Score
2.3.4. Socio-Economic Factors
2.4. Data Analysis
3. Results
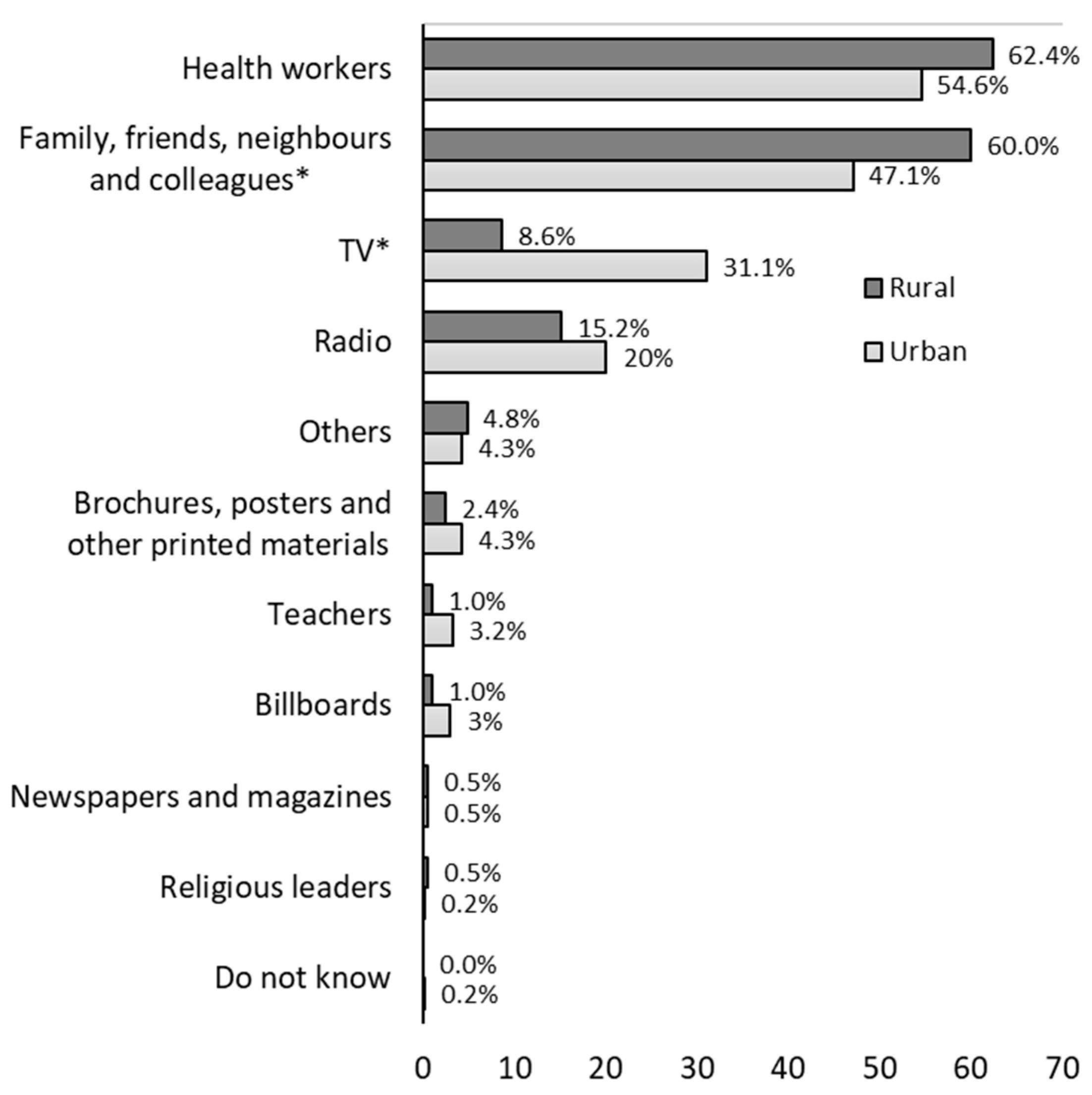
3.1. Factors Associated to TB Knowledge
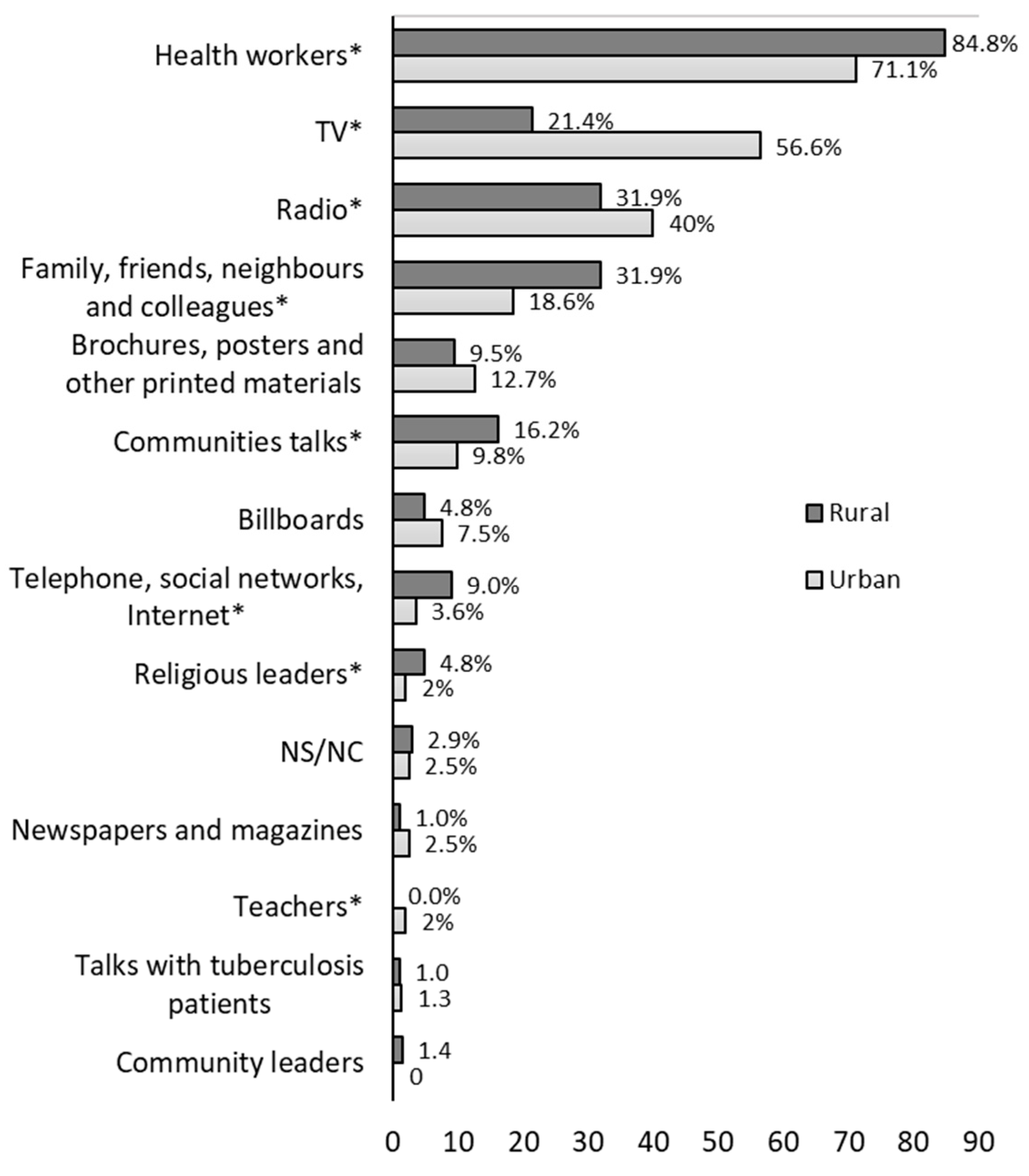
3.2. Factors Associated to TB Attitudes
3.3. Factors Associated to TB Stigma
4. Discussion
4.1. Knowledge
4.2. Attitudes
4.3. Stigma
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chakaya, J.; Khan, M.; Ntoumi, F.; Aklillu, E.; Fatima, R.; Mwaba, P.; Kapata, N.; Mfinanga, S.; Hasnain, S.E.; Katoto, P.D. Global Tuberculosis Report 2020–Reflections on the Global TB Burden, Treatment and Prevention Efforts. Int. J. Infect. Dis. 2021, 113, S7–S12. [Google Scholar] [CrossRef]
- Zumla, A.; Petersen, E.; Nyirenda, T.; Chakaya, J. Tackling the Tuberculosis Epidemic in Sub-Saharan Africa–Unique Opportunities Arising from the Second European Developing Countries Clinical Trials Partnership (EDCTP) Programme 2015–2024. Int. J. Infect. Dis. 2015, 32, 46–49. [Google Scholar] [CrossRef]
- WHO. Global Strategy for Tuberculosis Research and Innovation; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- WHO. Tuberculosis Profile: Equatorial Guinea. Available online: https://worldhealthorg.shinyapps.io/tb_profiles/?_inputs_&entity_type=%22country%22&lan=%22EN%22&iso2=%22GQ%22 (accessed on 22 June 2022).
- WHO. Global Health Observatory. Tuberculosis Treatment Coverage. Equatorial Guinea. 2019. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/tuberculosis-treatment-coverage (accessed on 18 October 2021).
- World Health Organization. WHO TB Burden Estimates. Available online: https://www.who.int/teams/global-tuberculosis-programme/data (accessed on 4 August 2021).
- Fagundez, G.; Perez-Freixo, H.; Eyene, J.; Momo, J.C.; Biyé, L.; Esono, T.; Ondó Mba Ayecab, M.; Benito, A.; Aparicio, P.; Herrador, Z. Treatment Adherence of Tuberculosis Patients Attending Two Reference Units in Equatorial Guinea. PLoS ONE 2016, 11, e0161995. [Google Scholar] [CrossRef] [PubMed]
- Tsegaye, D.; Abiy, E.; Mesele, T.; Tadesse, T. Delay in Seeking Health Care and Associated Factors among Pulmonary Tuberculosis Patients in North Wollo Zone, Northeast Ethiopia: Institution Based Crosssectional Study. Arch Clin. Microbiol. 2016, 7, 17. [Google Scholar] [CrossRef]
- Tola, H.H.; Tol, A.; Shojaeizadeh, D.; Garmaroudi, G. Tuberculosis Treatment Non-Adherence and Lost to Follow Up among TB Patients with or without HIV in Developing Countries: A Systematic Review. Iran J. Public Health 2015, 44, 1–11. [Google Scholar]
- World Health Organization. A Guide to Developing Knowledge, Attitude and Practice Surveys; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Datiko, D.G.; Habte, D.; Jerene, D.; Suarez, P. Knowledge, Attitudes, and Practices Related to TB among the General Population of Ethiopia: Findings from a National Cross-Sectional Survey. PLoS ONE 2019, 14, e0224196. [Google Scholar] [CrossRef] [PubMed]
- Storla, D.G.; Yimer, S.; Bjune, G.A. A Systematic Review of Delay in the Diagnosis and Treatment of Tuberculosis. BMC Public Health 2008, 8, 15. [Google Scholar] [CrossRef] [PubMed]
- Suleiman, M.M.A.; Sahal, N.; Sodemann, M.; El Sony, A.; Aro, A.R.; Suleiman, A. Tuberculosis Stigma in Gezira State, Sudan: A Case-Control Study. Int. J. Tuberc. Lung Dis. 2013, 17, 388–393. [Google Scholar] [CrossRef]
- Baral, S.C.; Karki, D.K.; Newell, J.N. Causes of Stigma and Discrimination Associated with Tuberculosis in Nepal: A Qualitative Study. BMC Public Health 2007, 7, 1–10. [Google Scholar] [CrossRef]
- Thapa, B.; Prasad, B.M.; Chadha, S.S.; Tonsing, J. Serial Survey Shows Community Intervention May Contribute to Increase in Knowledge of Tuberculosis in 30 Districts of India. BMC Public health 2016, 16, 1–8. [Google Scholar] [CrossRef]
- Balogun, M.R.; Sekoni, A.O.; Meloni, S.T.; Odukoya, O.O.; Onajole, A.T.; Longe-Peters, O.A.; Ogunsola, F.T.; Kanki, P.J. Predictors of Tuberculosis Knowledge, Attitudes and Practices in Urban Slums in Nigeria: A Cross-Sectional Study. Pan Afr. Med. J. 2019, 32, 60. [Google Scholar] [CrossRef] [PubMed]
- Islam, Q.S.; Islam, M.A.; Islam, S.; Ahmed, S.M. Prevention and Control of Tuberculosis in Workplaces: How Knowledgeable Are the Workers in Bangladesh? BMC Public Health 2015, 15, 1291. [Google Scholar] [CrossRef] [PubMed]
- Hossain, S.; Zaman, K.; Quaiyum, A.; Banu, S.; Husain, A.; Islam, A.; Borgdorff, M.; van Leth, F. Factors Associated with Poor Knowledge among Adults on Tuberculosis in Bangladesh: Results from a Nationwide Survey. J. Health Popul. Nutr. 2015, 34, 2. [Google Scholar] [CrossRef] [PubMed]
- Bashorun, A.O.; Linda, C.; Omoleke, S.; Kendall, L.; Donkor, S.D.; Kinteh, M.A.; Danso, B.; Leigh, L.; Kandeh, S.; D’Alessandro, U.; et al. Knowledge, Attitude and Practice towards Tuberculosis in Gambia: A Nation-Wide Cross-Sectional Survey. BMC Public Health 2020, 20, 1566. [Google Scholar] [CrossRef]
- Molyneux, C.S.; Mung’Ala-Odera, V.; Harpham, T.; Snow, R.W. Maternal Responses to Childhood Fevers: A Comparison of Rural and Urban Residents in Coastal Kenya. Trop Med. Int. Health 1999, 4, 836–845. [Google Scholar] [CrossRef]
- El Instituto Nacional de Estadística de Guinea Ecuatorial (INEGE). Anuario Estadístico de Guinea Ecuatorial 2021; INEGE: Malabo, Equatorial Guinea, 2021. [Google Scholar]
- Chadha, V.K. Sample Size Determination in Health Studies. NTI Bull. 2006, 42, 55–62. [Google Scholar]
- WHO. Advocacy, Communication and Social Mobilization for TB Control: A Guide to Developing Knowledge, Attitude and Practice Surveys; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Fotso, J.-C.; Kuate-Defo, B. Measuring Socioeconomic Status in Health Research in Developing Countries: Should We Be Focusing on Households, Communities or Both? Soc. Indic. Res. 2005, 72, 189–237. [Google Scholar] [CrossRef]
- Vyas, S.; Kumaranayake, L. Constructing Socio-Economic Status Indices: How to Use Principal Components Analysis. Health Policy Plan. 2006, 21, 459–468. [Google Scholar] [CrossRef]
- Espelt, A.; Marí-Dell’Olmo, M.; Penelo, E.; Bosque-Prous, M. Applied Prevalence Ratio Estimation with Different Regression Models: An Example from a Cross-National Study on Substance Use Research. Adicciones 2016, 29, 105–112. [Google Scholar] [CrossRef]
- Adane, K.; Spigt, M.; Johanna, L.; Noortje, D.; Abera, S.F.; Dinant, G.-J. Tuberculosis Knowledge, Attitudes, and Practices among Northern Ethiopian Prisoners: Implications for TB Control Efforts. PLoS ONE 2017, 12, e0174692. [Google Scholar] [CrossRef]
- Angelo, A.T.; Geltore, T.E.; Asega, T. Knowledge, Attitude, and Practices Towards Tuberculosis Among Clients Visiting Tepi General Hospital Outpatient Departments, 2019. Infect Drug Resist. 2020, 13, 4559–4568. [Google Scholar] [CrossRef] [PubMed]
- Fana, T.E.; Ijeoma, E.; Sotana, L. Knowledge, Attitudes, and Prevention Practices of Drug Resistant Tuberculosis in the Eastern Cape Province, South Africa. Tuberc. Res. Treat. 2019, 2019, 8978021. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bati, J.; Legesse, M.; Medhin, G. Community’s Knowledge, Attitudes and Practices about Tuberculosis in Itang Special District, Gambella Region, South Western Ethiopia. BMC Public Health 2013, 13, 734. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.R.; Muñoz-Torrico, M.; Duarte, R.; Galvão, T.; Bonini, E.H.; Arbex, F.F.; Arbex, M.A.; Augusto, V.M.; Rabahi, M.F.; de Queiroz Mello, F.C. Risk Factors for Tuberculosis: Diabetes, Smoking, Alcohol Use, and the Use of Other Drugs. J. Bras. De Pneumol. 2018, 44, 145–152. [Google Scholar] [CrossRef]
- Kwedi Nolna, S.; Kammogne, I.D.; Ndzinga, R.; Afanda, B.; Ntonè, R.; Boum, Y.; Nolna, D. Community Knowledge, Attitudes and Practices in Relation to Tuberculosis in Cameroon. Int. J. Tuberc. Lung Dis. 2016, 20, 1199–1204. [Google Scholar] [CrossRef]
- Naidoo, P.; Simbayi, L.; Labadarios, D.; Ntsepe, Y.; Bikitsha, N.; Khan, G.; Sewpaul, R.; Moyo, S.; Rehle, T. Predictors of Knowledge about Tuberculosis: Results from SANHANES I, a National, Cross-Sectional Household Survey in South Africa. BMC Public Health 2016, 16, 276. [Google Scholar] [CrossRef]
- Tolossa, D.; Medhin, G.; Legesse, M. Community Knowledge, Attitude, and Practices towards Tuberculosis in Shinile Town, Somali Regional State, Eastern Ethiopia: A Cross-Sectional Study. BMC Public Health 2014, 14, 804. [Google Scholar] [CrossRef]
- Hassan, A.O.; Olukolade, R.; Ogbuji, Q.C.; Afolabi, S.; Okwuonye, L.C.; Kusimo, O.C.; Osho, J.A.; Osinowo, K.A.; Ladipo, O.A. Knowledge about Tuberculosis: A Precursor to Effective TB Control-Findings from a Follow-Up National KAP Study on Tuberculosis among Nigerians. Tuberc. Res. Treat 2017, 2017, 6309092. [Google Scholar] [CrossRef]
- Luba, T.R.; Tang, S.; Liu, Q.; Gebremedhin, S.A.; Kisasi, M.D.; Feng, Z. Knowledge, Attitude and Associated Factors towards Tuberculosis in Lesotho: A Population Based Study. BMC Infect. Dis. 2019, 19, 1–10. [Google Scholar] [CrossRef]
- Chang, S.-H.; Cataldo, J.K. A Systematic Review of Global Cultural Variations in Knowledge, Attitudes and Health Responses to Tuberculosis Stigma. Int. J. Tuberc. Lung Dis. 2014, 18, 168–173. [Google Scholar] [CrossRef]
- Chen, X.; Du, L.; Wu, R.; Xu, J.; Ji, H.; Zhang, Y.; Zhu, X.; Zhou, L. Tuberculosis-Related Stigma and Its Determinants in Dalian, Northeast China: A Cross-Sectional Study. BMC Public Health 2021, 21, 6. [Google Scholar] [CrossRef] [PubMed]
- Pengpid, S.; Peltzer, K. Knowledge, Attitudes, and Practices Regarding Tuberculosis in Timor-Leste: Results from the Demographic and Health Survey 2016. J. Prev. Med. Public Health 2019, 52, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Teo, A.K.J.; Tan, R.K.J.; Smyth, C.; Soltan, V.; Eng, S.; Ork, C.; Sok, N.; Tuot, S.; Hsu, L.Y.; Yi, S. Characterizing and Measuring Tuberculosis Stigma in the Community: A Mixed-Methods Study in Cambodia. Open Forum Infect Dis. 2020, 7, ofaa422. [Google Scholar] [CrossRef]
- Tadesse, S. Stigma against Tuberculosis Patients in Addis Ababa, Ethiopia. PLoS ONE 2016, 11, e0152900. [Google Scholar] [CrossRef] [PubMed]
- Creel, A.H.; Rimal, R.N.; Mkandawire, G.; Böse, K.; Brown, J.W. Effects of a Mass Media Intervention on HIV-Related Stigma: ‘Radio Diaries’ Program in Malawi. Health Educ. Res. 2011, 26, 456–465. [Google Scholar] [CrossRef]
- Smith, R.A.; Zhu, X.; Quesnell, M. Stigma and Health/Risk Communication. In Oxford Research Encyclopedia of Communication: Health and Risk Message Design and Processing; Nussbaum, J., Ed.; Oxford University Press: New York, NY, USA, 2016; pp. 1–33. [Google Scholar] [CrossRef]
| Variable | Total (n = 770) | Rural (n = 210) | Urban (n = 560) | p-Value * |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Sex | 0.008 | |||
| Female | 408 (53.0) | 95 (45.2) | 313 (55.9) | |
| Male | 362 (47.0) | 115 (54.8) | 247 (44.1) | |
| Age | 0.002 | |||
| ≤45 years | 384 (49.9) | 86 (41.0) | 298 (53.2) | |
| >45 years | 386 (50.1) | 124 (59.0) | 262 (46.8) | |
| Marital status | 0.043 | |||
| Widowed | 103 (13.4) | 37 (17.6) | 66 (11.8) | |
| Married | 413 (53.6) | 116 (55.2) | 297 (53.0) | |
| Single | 243 (31.6) | 53 (25.2) | 190 (33.9) | |
| Divorced/separated | 11 (1.4) | 4 (1.9) | 7 (1.3) | |
| Educational status | <0.001 | |||
| Primary and lower | 265 (34.4) | 98 (46.7) | 167 (29.8) | |
| Secondary | 174 (22.6) | 52 (24.8) | 122 (21.8) | |
| Above secondary | 331 (43.0) | 60 (28.6) | 271 (48.4) | |
| Religion | 0.001 | |||
| Catholic | 616 (80.0) | 185 (88.1) | 431 (77.0) | |
| Other religions | 154 (20.0) | 25 (11.9) | 129 (23.0) | |
| Wage-employment | <0.001 | |||
| Yes | 223 (29.0) | 40 (19.0) | 183 (32.7) | |
| No | 547 (71.0) | 170 (81.0) | 377 (67.3) | |
| Wealth | <0.001 | |||
| Poorest | 154 (20.0) | 110 (52.4) | 44 (7.9) | |
| Second | 153 (19.9) | 67 (31.9) | 86 (15.4) | |
| Middle | 155 (20.1) | 14 (6.7) | 141 (25.2) | |
| Fourth | 152 (19.7) | 12 (5.7) | 140 (25.0) | |
| Richest | 156 (20.3) | 7 (3.3) | 149 (26.6) | |
| Overcrowding index | <0.001 | |||
| ≤1.4 points | 385 (50.0) | 140 (66.7) | 245 (43.8) | |
| >1.4 points | 385 (50.0) | 70 (33.3) | 315 (56.3) | |
| Population type | 0.110 | |||
| Non-TB cases | 486 (63.1) | 144 (68.6) | 342 (61.1) | |
| TB case in the family | 254 (33.0) | 61 (29.0) | 193 (34.5) | |
| TB case | 30 (3.9) | 5 (2.4) | 25 (4.5) |
| Variable (Reference) | High Knowledge | Good Attitude | Low Stigma |
|---|---|---|---|
| PR (95% CI) | PR (95% CI) | PR (95% CI) | |
| Sex (Male) | |||
| Female | 0.75 (0.62–0.91) | ||
| Age (over 45 years old) | |||
| 45 years and less | 1.30 (1.06–1.60) | ||
| TB case in the household (Non-TB cases) | |||
| TB case | 2.48 (1.87–3.30) | ||
| TB case in the family | 1.49 (1.22–1.81) | ||
| Religion (Other religions) | |||
| Catholic | 1.35 (1.04–1.76) | ||
| Wage-employment (No) | |||
| Yes | 1.21 (1.02–1.44) | ||
| Education level (Primary and lower) | |||
| Secondary | 1.20 (0.90–1.60) | ||
| Above secondary | 1.37 (1.06–1.78) | ||
| Wealth (Poor) | |||
| Second to richest | 1.39 (1.01–1.92) | ||
| Do you feel well informed about TB? (Yes) | |||
| No | 0.69 (0.58–0.83) | ||
| Where have you heard about TB? (No) | |||
| Radio—Yes | 1.32 (1.05–1.65) | ||
| TV—Yes | 0.76 (0.59–0.98) | ||
| Billboards—Yes | 1.86 (1.21–2.85) | ||
| Family, friends, neighbors, colleagues—Yes | 1.46 (1.20–1.77) | ||
| TB knowledge Score (Low) | 1.38 (1.15–1.67) | 1.34 (1.13–1.59) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vericat-Ferrer, M.; Ayala, A.; Ncogo, P.; Eyene-Acuresila, J.; García, B.; Benito, A.; Romay-Barja, M. Knowledge, Attitudes, and Stigma: The Perceptions of Tuberculosis in Equatorial Guinea. Int. J. Environ. Res. Public Health 2022, 19, 8227. https://doi.org/10.3390/ijerph19148227
Vericat-Ferrer M, Ayala A, Ncogo P, Eyene-Acuresila J, García B, Benito A, Romay-Barja M. Knowledge, Attitudes, and Stigma: The Perceptions of Tuberculosis in Equatorial Guinea. International Journal of Environmental Research and Public Health. 2022; 19(14):8227. https://doi.org/10.3390/ijerph19148227
Chicago/Turabian StyleVericat-Ferrer, Marta, Alba Ayala, Policarpo Ncogo, Juan Eyene-Acuresila, Belén García, Agustín Benito, and María Romay-Barja. 2022. "Knowledge, Attitudes, and Stigma: The Perceptions of Tuberculosis in Equatorial Guinea" International Journal of Environmental Research and Public Health 19, no. 14: 8227. https://doi.org/10.3390/ijerph19148227
APA StyleVericat-Ferrer, M., Ayala, A., Ncogo, P., Eyene-Acuresila, J., García, B., Benito, A., & Romay-Barja, M. (2022). Knowledge, Attitudes, and Stigma: The Perceptions of Tuberculosis in Equatorial Guinea. International Journal of Environmental Research and Public Health, 19(14), 8227. https://doi.org/10.3390/ijerph19148227






