Abstract
Since the long-term mental health impact of COVID-19 is not yet fully understood, the present study explored changes in mental health outcomes and pandemic-related coping behaviors across four pandemic stages. The main objective was to gain insights into the dynamics of mental health and coping, considering different pandemic features at different assessment waves. The final sample consisted of N = 243 adults from the Austrian general population. Data were collected at four timepoints (between June 2020 and December 2021) via LimeSurvey, an open-source online survey tool. Symptoms of posttraumatic stress disorder (PTSD), adjustment disorder (AD), anxiety, and depression were assessed using validated instruments: Primary Care PTSD Screen for DSM-5 (PC-PTSD-5), AD-New Module 8 (ADNM-8), and Patient Health Questionnaire (PHQ4). We also administered the Pandemic Coping Scale (PCS) to address pandemic-related coping behaviors. Cochran’s Q test and repeated measures ANOVAs were applied to assess changes over time. The results indicated that prevalence rates of AD (χ2(2) = 16.88, p = 0.001), depression (χ2(3) = 18.69, p < 0.001), and anxiety (χ2(3) = 19.10, p < 0.001) significantly changed across four assessment waves. Changes in mean scores of the assessed mental health outcomes were also observed. For pandemic-related coping, we found differences in the subscales: healthy lifestyle: F(3, 651) = 5.11, prevention adherence: F(2.73, 592.35) = 21.88, and joyful activities: F(3, 651) = 5.03. Taken together, our study showed a higher mental health burden in wintertime than in summertime, indicating an increased need for psychosocial support in times of stricter measures, higher incidences, and higher death rates. Furthermore, the observed decrease in adaptive coping behaviors suggests that easy-to-implement coping strategies should be actively promoted in order to maintain mental health during and in the aftermath of pandemics.
1. Introduction
While Austria was not considered as one of the countries most severely affected by COVID-19 (i.e., infectious disease caused by the SARS-CoV-2 virus), it found itself in the spotlight of the pandemic early on following an outbreak in an Austrian ski resort, which contributed to the rapid spread of the virus in Europe [1]. Since March 2020, four hard nationwide lockdowns have been implemented, along with multiple strict regulations on the regional level, gravely impacting the daily lives of Austrian citizens (see Table 1). Specifically, in December 2021, Austria was the only country in Europe that was in a full lockdown. Given that preventive measures have been very strict not only at the beginning, but also at later pandemic stages, increased symptoms of mental health disorders could be expected.

Table 1.
COVID-19 situation at four timepoints of data collection.
During the first lockdown, increased levels of depression and anxiety symptoms were found in the Austrian general population [2]. A longitudinal study conducted from April to October 2020 revealed different patterns for different mental health outcomes: whereas suicidal ideation remained stable, and depressive and anxiety symptoms started increasing only shortly before the second lockdown, an immediate increase in domestic violence was observed following both lockdowns [3]. In Vienna, the capital of Austria, a significant increase in anxiety, depression, fatigue, and loneliness has been evident in the first pandemic year, with 46% of the participants representative of the Viennese population reporting mental health deterioration [4]. However, since prospective studies covering later stages of the pandemic are lacking, little is known about long-term trajectories of mental health in the Austrian population. For several other countries, longitudinal data on the mental health effects of the pandemic are more readily available, but with mostly short assessment periods. In the USA, Breslau et al. [5] applied a longitudinal design with two timepoints, showing higher psychological distress during the pandemic (May 2020) than before the pandemic (February 2019). In Spain, distinct patterns were present for symptoms of depression, anxiety, and posttraumatic stress disorder (PTSD): whereas anxiety and PTSD symptomatology showed a downward trend over three timepoints (at the beginning of the confinement, after a month, and after two months), depressive symptoms decreased only at the last assessment [6]. In the UK, a study conducted during the first 6 weeks of lockdown [7] noted increases in suicidal ideation, decreases in anxiety symptoms, and, remarkably, no significant changes in loneliness levels or depressive symptoms. In a German study covering a period of three months (May–June 2020) symptoms of mental health disorders were highest at the beginning, then remained stable or decreased only marginally, pointing toward the presence of a habituation mechanism evolving over time [8]. Similarly, a prospective English study observed a rapid decline in mental health problems during the first weeks of lockdown, with symptoms plateauing as lockdown measures were progressively eased [9].
While the loosening of preventive measures represents a plausible explanation for the observed changes in mental health over time in relation to COVID-19, other factors might also account for these changes. For instance, daily COVID-19 infection rates and decreased human mobility have been associated with significant increases in the prevalence of anxiety and depression [10]. A positive link has also been found between mental health problems and cumulative stress, resulting from co-occurring pandemic-related stressors [11]. On the other hand, becoming accustomed to the “COVID-19 way of life” might lead to an improvement in mental health as pandemic progresses. Previous research has shown that people have the capacity to successfully adapt and even flourish following large-scale stressful events [12,13]. Psychological adjustment is likely to be shaped by distinct individual characteristics, but also by the socio-political context in different pandemic stages [14,15]. This highlights the need to consider country-specific factors when investigating and interpreting the mental health effects of the pandemic.
In light of the multiple pandemic stages, each bearing different challenges, coping behaviors of the general population are likely to change and evolve. Being flexible, i.e., paying attention to changing situational demands and responding to them by using varying cognitive, emotional, and behavioral strategies may become essential for maintaining stable mental health [16,17]. An Italian longitudinal study conducted between March and May 2020 found lower levels of avoidant coping behaviors at baseline than at the final assessment [18]. Another Italian study launched only a month later noted an increased utilization of adaptive coping strategies at later timepoints [19]. Further longitudinal analyses of coping behaviors are urgently needed to better understand the mechanisms underlying psychological adjustments to COVID-19. Additionally, pandemic-related coping behaviors (e.g., adherence to containment measures; [20]) should be explored further.
Taken together, several international studies have investigated trajectories of mental health, but only a few have explored changes in coping behaviors. Most longitudinal studies have covered rather short intervals, e.g., several weeks [21] or a few months [8]. Studies that include almost the entire period of the pandemic up to this point and consider other mental health disorders are thus still lacking. Longitudinal analysis using data collected in several waves for a longer period would be particularly beneficial, considering the dynamics of the pandemic with regard to seasonal aspects, rates of infections, morbidity, and levels of restrictions, all of which may impact mental health and lead to potential habituation or (failed) adjustment mechanisms. For Austria, only a few studies on mental health during COVID-19 pandemic exist so far, and there are no studies on mental health and coping in later stages of the pandemic. Moreover, there are very little data on adjustment disorders (AD) in the Austrian general population.
The present study aims to address these research gaps by exploring the trajectories of various mental health outcomes and pandemic-related coping behaviors over 18 months of the pandemic in Austria. The main objective is to better understand the dynamics of mental health and coping, with specific aims to:
- Determine the point prevalence of AD, PTSD, depression, and anxiety in the general population of Austria in four pandemic stages;
- Compare the prevalence rates across the four stages;
- Examine pandemic-related coping behaviors employed by the general population of Austria; and
- Examine the differences in the use of coping behaviors across four pandemic stages.
2. Materials and Methods
The present study is part of an overarching project investigating the mental health impact of the COVID-19 pandemic across 11 European countries (ADJUST study; [22,23]). The study was preregistered in the OSF registry (https://doi.org/10.17605/OSF.IO/8XHYG). Each of the contributing countries collected data, with small modifications according to the local situation. Since Austria was the only country with a lockdown from November to December 2021, a fourth wave of data collection was administered in Austria, in addition to three waves conducted in all participating countries. The data reported in this paper stem from the general population sample of Austrian adults. The participants were assessed repeatedly at up to four assessment waves between June 2020 and December 2021 using open-source online survey tool LimeSurvey. Table 1 illustrates the COVID-19 situation in Austria during the four waves. Ethical approval was granted by the Ethics Committee of the University of Vienna, Reference Number: 00554. All participants provided informed consent prior to survey beginning.
2.1. Sampling
To increase the sample’s variability, participants of the first wave (baseline; T1) were recruited using different strategies. We distributed flyers in public spaces, shared our study link via social media, and contacted relevant stakeholders (e.g., universities, psychosocial support services), professional organizations (e.g., companies, theatres), as well as leisure and interest groups (e.g., gyms, clubs for senior citizens), asking them to distribute our study invitation to their staff or members. Interested individuals could access the survey by a website link or a QR code. After reading study information and providing consent on the first survey page, they could start answering our survey questions.
Inclusion criteria were: (1) age 18 or over, (2) sufficient skills in German language, and (3) willingness to participate. Participants who agreed to take part in the subsequent waves (n = 525) provided their e-mail and were re-contacted after approximately 6, 12, and 16 months (T2, T3 and T4, respectively).
2.2. Measures
The instruments relevant for the study are presented in the following section. The core set of instruments within the ADJUST study is described elsewhere [22].
The Adjustment Disorder New Module-8 (ADNM-8) is a brief measure of AD symptoms according to the ICD-11 [24]. It has demonstrated good reliability, convergent and factorial validity [24,25].
The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) is a 5-item screening measure for PTSD according to the DSM-5 criteria [26]. It has shown excellent diagnostic accuracy, high acceptability and good performance characteristics [27,28,29].
The 4-item Patient Health Questionnaire (PHQ-4) is an ultra-brief screening tool for depression and anxiety [30]. It consists of two subscales measuring depression (PHQ-2) and anxiety (GAD-2). Evidence for good psychometric properties and high applicability of PHQ-4 across different contexts has been provided [31].
The Pandemic Coping Scale (PCS) is a 13-item measure of coping behaviors specific for a pandemic [32]. The scale was constructed by a group of professionals in the field of traumatic stress, based on existing recommendations and studies on coping during a pandemic. It has shown sufficient factor validity and reliability [32].
The measures were assessed in all four waves. Internal consistency was determined using Cronbach’s α for all measures and all waves of assessment (for details see Table 2).

Table 2.
Internal consistency of the included measures across four assessment waves.
2.3. Data Analysis
Using the established cut-offs, we calculated prevalence rates of probable self-reported AD (ADNM-8 > 22), PTSD (PC-PTSD-5 > 3), depression (PHQ-2 > 2), and anxiety (GAD-2 > 2) for each timepoint. We then compared the differences in prevalence rates of AD, PTSD, depression, and anxiety between four timepoints using Cochran’s Q, followed by a post-hoc analysis. We then conducted one-way repeated measures ANOVAs to compare mean scores of all mental health outcomes and coping behaviors across four assessment waves. Finally, a two-way mixed ANOVA was used to test for gender differences in mental health outcomes and coping strategies.
As assessed by Normal Q-Q Plot, the variables mostly followed a normal distribution. The distributions of PHQ-4 and one PCS subscale were slightly left-skewed, which was not considered problematic, given the large sample size and application of analyses that are robust to violations of normality [33]. We applied the Bonferroni correction [34] to account for multiple tests in the post hoc analyses, and the Greenhouse-Geisser correction if the assumption of sphericity was violated (as assessed by the Mauchly’s test of sphericity).
Complete case analysis was used in order to avoid additional layer of measurement error in the data [35]. To rule out a possible bias introduced by the exclusion of incomplete cases, we performed multiple imputation using Fully Conditional Specifications [36,37] as sensitivity analysis. The analysis with estimated missing values in the mental health outcomes (n = 1001) revealed comparable results, as illustrated in the Appendix A.
Partial eta squared (η2) was applied as a measure of effect size, with η2 = 0.01, η2 = 0.06, and η2 = 0.14 reflecting a small, medium, and large effect, respectively [38]. All analyses were performed with SPSS Statistics Version 26 (IBM, Armonk, NY, USA).
3. Results
3.1. Sample Characteristics
After exclusion of participants not living in Austria at the time of the study or not completing any of the primary outcome measures, the original T1 sample included N = 1001 participants, of which 767 did not provide data on all relevant measures on all occasions. The final sample consisted of N = 234 participants, aged between 21 and 81 years (M = 48.75, SD = 15.03), responding to the four waves from all federal states of Austria. Their sociodemographic characteristics are shown in Table 3. Regarding health-related characteristics, the vast majority of participants described their health as “very good” (45.7%, n = 107) or “good” (32.9%, n = 77). One-fifth of the sample (19.7%, n = 46) indicated to be at risk for severe or life-threatening symptoms of the coronavirus disease, with old age and pre-existing conditions being the most frequently mentioned reasons for being at risk.

Table 3.
Sociodemographic characteristics of the final sample (N = 234).
An independent-samples t-test was run to determine if there were differences in mean age and education between participants who responded to all waves and those who did not. Inspection of boxplots indicated there were no outliers in the data. Normal Q-Q Plot showed a normally distributed age in both samples. There was homogeneity of variances, as assessed by Levene’s test (p = 0.102 for age; p = 0.119 for education). The respondents were statistically significantly older (M = 48.75, SD = 15.03) than non-respondents (M = 44.59, SD = 13.83), t(999) = 3.95, p < 0.001. The respondents were also slightly better educated (M = 3.49, SD = 0.74) than non-responders (M = 3.30, SD = 0.80), t(999) = 3.32, p = 0.001. Respondents and non-respondents did not differ in terms of gender, as assessed by Fisher’s exact test, p = 0.771.
3.2. Longitudinal Changes in Mental Health Outcomes
The estimated prevalence rates of the assessed mental health outcomes at four timepoints are depicted in Table 4. The prevalence rates of self-reported probable AD differed significantly across four waves, χ2(2) = 16.88, p = 0.001 (n = 221). Pairwise comparison using Dunn’s test with a Bonferroni correction indicated that the prevalence rates statistically significantly changed between T1 and T2 (p = 0.001), and between T2 and T3 (p = 0.009). Regarding probable depression and anxiety disorder, the percentage of participants at risk was also statistically significantly different at the different time points, with χ2(3) = 18.69 for depression and χ2(3) = 19.10 for anxiety disorder (p < 0.001; n = 220). According to the Dunn’s test, statistically significant increase in the percentage of participants at risk for probable depression was detected between T1 and T4 (p = 0.02), and T3 and T4 (p = 0.001), whereas a significant decrease was detected between T2 and T3 (p = 0.02). Similarly, prevalence of probable anxiety disorder significantly increased between T1 and T4 (p = 0.01), and T3 and T4 (p < 0.001). The observed decrease between T2 and T3 was nearly significant, with p = 0.055.

Table 4.
Prevalence rates of probable mental health disorders at four timepoints.
After establishing the prevalence rates, we explored changes in mean scores of the assessed mental health outcomes. The AD, depression, and anxiety scores significantly changed across four assessment waves, with highest values at T2 and T4. Table 5 provides the results on the main effect of time, including post hoc analyses.

Table 5.
Means, standard deviations, and repeated measures ANOVA statistics for mental health outcomes.
As shown in Table 6, the interaction effect between gender and time (GxT) on the assessed mental health outcomes was not statistically significant. Therefore, an analysis of the main effect for gender was performed, indicating significantly higher scores for female participants than male participants on all mental health outcomes across all timepoints, with the largest effect observed for anxiety symptoms. On average, females’ scores were 1.911 points (95% CI [0.45, 3.38]) higher for ADNM-8, 0.36 points (95% CI [0.03, 0.69]) higher for PHQ-2, and 0.62 points (95% CI [0.27, 0.98]) higher for GAD-2. All details regarding gender differences are depicted in Table 6.

Table 6.
Descriptive statistics and two-way ANOVA statistics of mental health outcomes for males and females.
Due to an extremely low number of participants who completed PC-PTSD-5 at all timepoints (n = 13), ANOVA could not be conducted for this measure. Thus, only mean values of PC-PTSD-5 at each timepoint are reported.
3.3. Longitudinal Changes in Pandemic-Related Coping Behaviors
One-way repeated measures ANOVA showed a significant decrease in the total score of PCS over time, F(2.89, 626.12) = 6.54, p < 0.001, partial η2 = 0.03. The highest mean score was observed at T1 (27.27 ± 6.33) and the lowest at T4 (25.86 ± 6.30), with T2 and T3 means in between (26.36 ± 6.44 and 26.34 ± 6.49). Changes on the PCS subscales between the four timepoints are presented in Table 7. As shown in Table 8, the interaction effect between gender and time (GxT) on the assessed coping behaviors was not statistically significant. Therefore, we conducted an analysis of the main effect for gender. Significantly higher scores for female participants were found on subscales “Healthy lifestyle” and “Daily structure”.

Table 7.
Means, standard deviations, and repeated measures ANOVA statistics for pandemic-related coping behaviors.

Table 8.
Descriptive statistics and two-way ANOVA statistics of pandemic-related coping for males and females.
4. Discussion
The present study focused on adjustment disorder (AD) acknowledging that the dynamics of the pandemic has challenged the population’s adjustment capacity. Overall, we did not assess the pandemic as a traumatic experience because it is not life-threatening for the majority of the population. However, for some people, the pandemic includes life-threatening and traumatic aspects which our study also addressed. Moreover, we included depression and anxiety symptoms as common reactions to chronic stress. Thus, our longitudinal design could foster the planning of mental health services especially for the part of population that suffers from failed adjustment or a limited capacity to adjust to the pandemic. For this planning, the changes in coping over time in response to environmental factors, such as the stringency of preventive measures, might also be of relevance.
Specifically, this study compared pandemic-related coping behaviors and symptoms of AD, PTSD, depression, and anxiety during the 18 months of COVID-19 in Austria. Across the four assessment waves, we found rather high point prevalence rates and mean scores for all mental health outcomes. This held true for the complete-case analysis as well as the analysis using imputed missing values. The highest values for anxiety and depression were identified at T4 (December 2021), when Austria was under strict lockdown conditions. For all disorders we screened for, we observed lower prevalence and mean scores in summertime (T1 and T3), than in wintertime (T2 and T4), the latter being characterized by stricter regulations, higher incidence and death rates. In wintertime, the participants did not engage in as many joyful activities, indicating that pandemic fatigue or resignation in periods with stricter regulations might hinder adaptive coping behaviors. Furthermore, a gradual decrease in healthy lifestyle and prevention adherence suggests that even well-educated, older individuals did not fully comply with the pandemic regime for a longer period of time. This contradicts studies reporting more adaptive coping behaviors in later assessment waves [18], possibly due to the different timepoints implemented in our study. Maintaining daily structure, which had a positive effect on mental health in earlier COVID-19 studies [39] seemed to be equally relevant at all four timepoints.
With regards to gender differences, we observed higher values in women on all mental health outcomes at all timepoints. This finding is in line with the existing literature [10,23]. Although the trajectories of mental health slightly differed between male and female participants (e.g., depression score being highest at T2 in women, and at T4 in men), they followed the same pattern as in the overall sample, with fewer symptoms of mental health disorders reported in summertime than in wintertime. Regarding coping, women were more likely to use all pandemic-related coping behaviors at all timepoints. These gender differences have been observed in previous studies, with different coping behaviors being more common among female participants [17,40]. Further work is required to examine whether and how these differences in coping behaviors are related to mental health.
Overall, our results suggest that changes in the general population during COVID-19 pandemic depend on multiple factors. Both changes in mental health and in coping behaviors might be attributed to the changing pandemic situation, e.g., different incidence and containment measures, but might also depend on the season. Thus, our findings add to the studies covering shorter assessment intervals (e.g., [8]), by indicating that mental health and coping patterns change even in the later stages of the pandemic. Over time, individuals tend to adopt less healthy coping behaviors and manifest greater psychopathological symptoms. In order to provide adequate psychosocial support, the varying mental health challenges and needs of the general population need to be acknowledged.
Taken together, our study shows that the pandemic-related restrictions have left their mark on the people of Austria. Hence, it cannot be expected that everyone can successfully adjust to the changes caused by COVID-19. This highlights the need for a broad mental health campaign in order to address mental health needs and foster psychological adjustment in the general population, e.g., focusing on healthy behaviors and adaptive coping in periods of more restrictive measures. In addition, large mental health campaigns might deliver psychoeducation or inform the population how, where, and when to seek help. Finally, our findings on different mental health problems and coping behaviors might help to optimize psychosocial services all over Austria.
Strengths and Limitations
To the best of our knowledge, this is the first longitudinal study on the mental health impact of COVID-19 covering almost all pandemic stages so far, with rather large intervals between the assessment waves. Apart from previously investigated trajectories of depression, anxiety, and PTSD (e.g., [3,6]), we also assessed changes in symptoms of AD. This is particularly relevant given that AD might be the most important, widespread mental health outcome of the pandemic [41]. It develops in response to stressors such as illness, relationship problems, financial or work-related issues, which are all relevant in this context [23,42]. Moreover, we provided some initial reports of pandemic-related coping behaviors adopted by the general population in different pandemic stages. Considering the long assessment period, another strength of the study is the relatively high number of participants who responded to all waves (45% of those who agreed to be re-contacted). Furthermore, the sample was well-distributed in terms of income and age.
An important limitation was that the participants were highly educated and predominantly female, which hampers the generalizability of the results. Although we have covered four distinct pandemic stages, we did not collect data in the very first months of the pandemic, which was declared to have begun in March 2020 [43]. Furthermore, while the internal consistency was satisfactory for most measures, low and unstable values were observed for some of the PCS subscales. Given the early stage, exploratory character of the study, we neither formulated hypotheses nor found it feasible to analyze possible predictors and groups at-risk. Associations between trajectories of mental health outcomes, coping behaviors, and sociodemographic characteristics other than gender should also be examined in future studies. Finally, our findings could not be contrasted with mental health trajectories before the pandemic, as, to our knowledge, no comparable epidemiological studies which included AD existed in Austria.
5. Conclusions
The present study paves the way for future research to explore the longitudinal impact of COVID-19 on mental health. Our findings highlight the need to consider governmental restrictions and the differing pandemic-related situations when investigating mental health trajectories. Importantly, findings of the present study also underline the importance of promoting easy-to-implement coping strategies (e.g., joyful activities) to foster healthy peri- and post-adjustment. Even in times of improving pandemic situation, the psychological burden of COVID-19 should be acknowledged and adequately addressed.
Author Contributions
Conceptualization, B.L.-S. and I.Z.N.; methodology, B.L.-S., I.Z.N. and A.L.; formal analysis, I.Z.N.; investigation, B.L.-S., I.Z.N. and A.L.; writing—original draft, I.Z.N.; writing—review and editing, I.Z.N. and B.L.-S.; visualization, I.Z.N.; supervision, B.L.-S. and A.L.; project administration, B.L.-S. and A.L. All authors have read and agreed to the published version of the manuscript.
Funding
The Article Processing Charges (APCs) were covered by the University of Vienna through its Open Access Publishing Fund.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the University of Vienna (reference number: 00554; date of approval: 29 May 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The entire dataset cannot be made publicly available since the analysis is still in progress. After the completion of the ongoing work, excerpts of the data can be obtained from the first authors upon reasonable request.
Acknowledgments
The authors thank Stella Perziani for assisting with the literature research and Jeremy Somers for proofreading the article.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Appendix A.1. Multiple Imputation as Sensitivity Analysis
Complete case analysis was used for data analysis, in order to avoid additional layer of measurement error in the data [35]. To rule out a possible bias introduced by the exclusion of incomplete cases, we performed multiple imputation using Fully Conditional Specifications (FCS; [36,37]) as sensitivity analysis. FSC was chosen because this method is suitable for categorical as well as continuous predictors. The number of imputed data sets corresponded to the percentage of incomplete cases, namely: m = 80 for ADNM-8, PHQ-2, GAD-2, and pandemic-related coping strategies, and m = 90 for PC-PTSD-5. All variables of the respective data analysis were included in the imputation model. Additional variables, i.e., auxiliary variables, were selected for the imputation model based on their correlation with the incomplete variables in the present and earlier studies (e.g., [23]). Thus, an inclusive approach of multiple imputation was applied.
As illustrated in the charts below, the analysis with estimated missing values in the mental health outcomes (n = 1001) revealed comparable results. The mean scores of the mental health outcomes in the imputed dataset were slightly higher, but followed the same pattern as in the original, non-imputed dataset. Slightly higher values stemming from the imputed dataset might indicate that participants with less mental health problems were more likely to respond to all waves. With regard to pandemic-related coping behaviors, the scores stemming from the imputed data dataset were slightly lower, suggesting that participants who employed more coping behaviors were also more likely to respond to all waves. However, these assumptions would need to be tested in a more rigorous matter in order to draw reliable conclusions.
Appendix A.1.1. Changes in Mental Health Outcomes
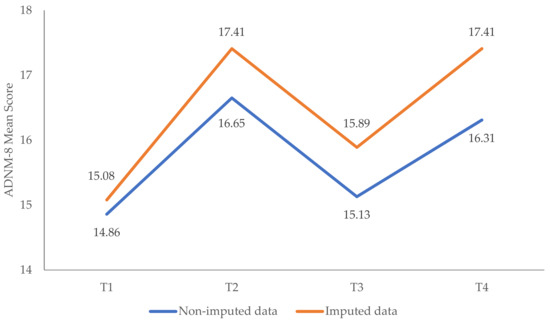
Figure A1.
Changes in symptoms of adjustment disorder (ADNM-8) over time: imputed vs. non-imputed results. Note: Imputed dataset: n = 1001. Non-imputed dataset: n = 221.
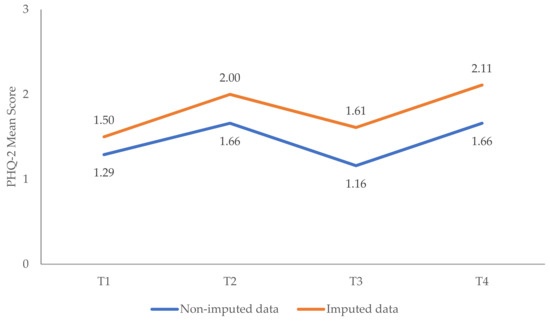
Figure A2.
Changes in symptoms of depression (PHQ-2) over time: imputed vs. non-imputed results. Note: Imputed dataset: n = 1001. Non-imputed dataset: n = 220.
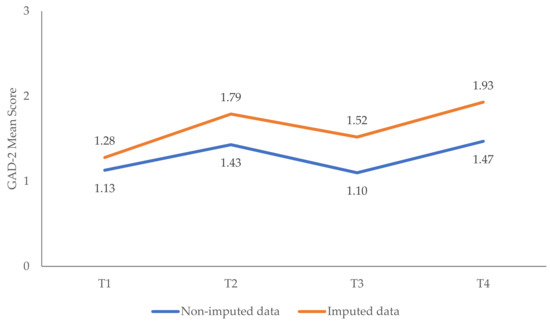
Figure A3.
Changes in symptoms of anxiety (GAD-2) over time: imputed vs. non-imputed results. Note: Imputed dataset: n = 1001. Non-imputed dataset: n = 220.
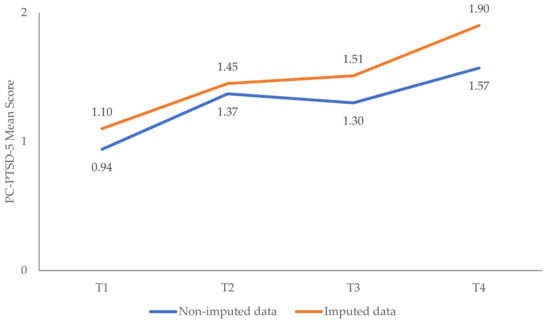
Figure A4.
Changes in symptoms of PTSD (PC-PTSD-5) over time: imputed vs. non-imputed results. Note: Imputed dataset: n = 1001. Non-imputed dataset: nt1 = 221. nt2,3 = 35. nt4 = 46.
Appendix A.1.2. Changes in Pandemic-Related Coping Behaviors
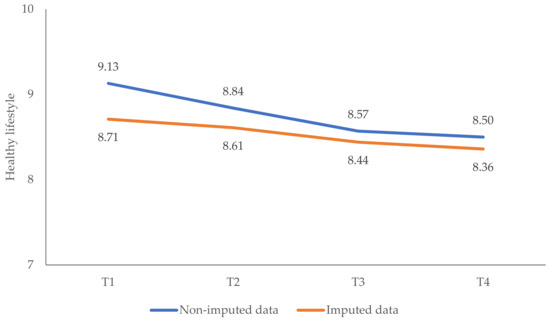
Figure A5.
Changes over time in the subscale “Healthy lifestyle”: imputed vs. non-imputed results. Note: Imputed dataset: n = 1001. Non-imputed dataset: n = 218.
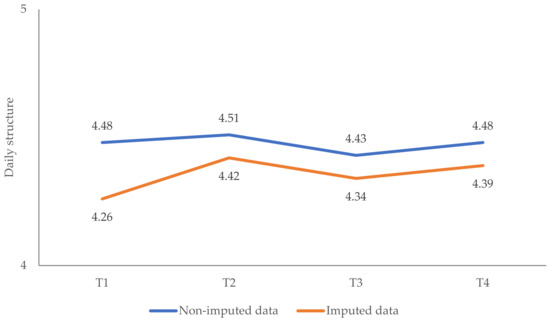
Figure A6.
Changes over time in the subscale “Daily structure”: imputed vs. non-imputed results. Note: Imputed dataset: n = 1001. Non-imputed dataset: n = 218.
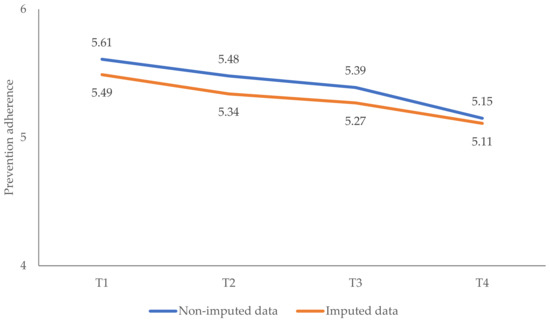
Figure A7.
Changes over time in the subscale “Prevention adherence”: imputed vs. non-imputed results. Note: Imputed dataset: n = 1001. Non-imputed dataset: n = 218.

Figure A8.
Changes over time in the subscale “Joyful activities”: imputed vs. non-imputed results. Note: Imputed dataset: n = 1001. Non-imputed dataset: n = 218.
References
- Felbermayr, G.; Hinz, J.; Chowdhry, S. Après-ski: The Spread of Coronavirus from Ischgl through Germany. Ger. Econ. Rev. 2021, 22, 415–446. [Google Scholar] [CrossRef]
- Pieh, C.; Budimir, S.; Probst, T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease [COVID-19] lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. Available online: http://www.sciencedirect.com/science/article/pii/S0022399920307480 (accessed on 1 June 2022). [CrossRef] [PubMed]
- Niederkrotenthaler, T.; Laido, Z.; Kirchner, S.; Braun, M.; Metzler, H.; Waldhör, T.; Strauss, M.; Garcia, D.; Till, B. Mental health over nine months during the SARS-CoV2 pandemic: Representative cross-sectional survey in twelve waves between April and December 2020 in Austria. J. Affect. Disord. 2022, 296, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Zandonella, M. Follow-Up zur Psychosozialen Situation der WienerInnen Während der Pandemie [Follow-Up on the Psychosocial Situation of the Viennese during the Pandemic]; SORA Institute for Social Research and Consulting: Vienna, Austria, 2021. Available online: https://www.digital.wienbibliothek.at/wbrup/download/pdf/3676800?originalFilename=true (accessed on 1 June 2022).
- Breslau, J.; Finucane, M.L.; Locker, A.R.; Baird, M.D.; Roth, E.A.; Collins, R.L. A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev. Med. 2021, 143, 106362. [Google Scholar] [CrossRef]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.A.; Saiz, J.; Muñoz, M. Mental health consequences of the COVID-19 outbreak in Spain. A longitudinal study of the alarm situation and return to the new normality. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 107, 110219. [Google Scholar] [CrossRef]
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry 2020, 218, 326–333. [Google Scholar] [CrossRef]
- Mata, J.; Wenz, A.; Rettig, T.; Reifenscheid, M.; Möhring, K.; Krieger, U.; Friedel, S.; Fikel, M.; Cornesse, C.; Blom, A.G.; et al. Health behaviors and mental health during the COVID-19 pandemic: A longitudinal population-based survey in Germany. Soc. Sci. Med. 2021, 287, 114333. [Google Scholar] [CrossRef]
- Fancourt, D.; Steptoe, A.; Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. Lancet Psychiatry 2021, 8, 141–149. [Google Scholar] [CrossRef]
- Santomauro, D.F.; Herrera, A.M.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Rudenstine, S.; Schulder, T.; Bhatt, K.J.; McNeal, K.; Ettman, C.K.; Galea, S. Suicidal ideation during COVID-19: The contribution of unique and cumulative stressors. Psychiatry Res. 2022, 310, 114475. [Google Scholar] [CrossRef]
- Chen, S.; Bonanno, G.A. Psychological adjustment during the global outbreak of COVID-19: A resilience perspective. Psychol. Trauma 2020, 12, S51–S54. [Google Scholar] [CrossRef]
- Vazquez, C.; Valiente, C.; García, F.E.; Contreras, A.; Peinado, V.; Trucharte, A.; Bentall, R.P. Post-traumatic growth and stress-related responses during the COVID-19 pandemic in a national representative sample: The role of positive core beliefs about the world and others. J. Happiness Stud. 2021, 22, 2915–2935. [Google Scholar] [CrossRef]
- Sandbakken, E.M.; Moss, S.M. “Now We Are All in the Same Boat. At the Same Time, We Are Not.” Meaning-Making and Coping under COVID-19 Lockdown in Norway. Hu Arenas 2021, 1–25. [Google Scholar] [CrossRef]
- Santabárbara, J.; Lasheras, I.; Lipnicki, D.M.; Bueno-Notivol, J.; Pérez-Moreno, M.; López-Antón, R.; De la Cámara, C.; Lobo, A.; Gracia-García, P. Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 109, 110207. Available online: https://www.sciencedirect.com/science/article/pii/S0278584620305236 (accessed on 1 June 2022). [CrossRef]
- Dawson, D.L.; Golijani-Moghaddam, N. COVID-19: Psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. J. Context. Behav. Sci. 2020, 17, 126–134. [Google Scholar] [CrossRef]
- Eisenbeck, N.; Carreno, D.F.; Wong, P.T.; Hicks, J.A.; María, R.-R.G.; Puga, J.L.; Greville, J.; Testoni, I.; Biancalani, G.; López, A.C.C.; et al. An international study on psychological coping during COVID-19: Towards a meaning-centered coping style. Int. J. Clin. Health Psychol. 2022, 22, 100256. [Google Scholar] [CrossRef]
- Quaglieri, A.; Lausi, G.; Fraschetti, A.; Burrai, J.; Barchielli, B.; Pizzo, A.; Cordellieri, P.; De Gennaro, L.; Gorgoni, M.; Ferlazzo, F.; et al. “Stay at Home” in Italy during the COVID-19 Outbreak: A Longitudinal Study on Individual Well-Being among Different Age Groups. Brain. Sci. 2021, 11, 993. [Google Scholar] [CrossRef]
- Gullo, S.; Misici, I.; Teti, A.; Liuzzi, M.; Chiara, E. Going through the lockdown: A longitudinal study on the psychological consequences of the coronavirus pandemic. Res. Psychother. 2020, 23, 494. [Google Scholar] [CrossRef]
- Galende, N.; Redondo, I.; Dosil-Santamaria, M.; Ozamiz-Etxebarria, N. Factors Influencing Compliance with COVID-19 Health Measures: A Spanish Study to Improve Adherence Campaigns. Int. J. Environ. Res. Public Health 2022, 19, 4853. Available online: https://www.mdpi.com/1660-4601/19/8/4853/htm (accessed on 1 June 2022). [CrossRef]
- Shi, L.; Lu, Z.-A.; Que, J.-Y.; Huang, X.-L.; Lu, Q.-D.; Liu, L.; Zheng, Y.-B.; Liu, W.-J.; Ran, M.-S.; Yuan, K.; et al. Long-Term Impact of COVID-19 on Mental Health among the General Public: A Nationwide Longitudinal Study in China. Int. J. Environ. Res. Public Health 2021, 18, 8790. [Google Scholar] [CrossRef]
- Lotzin, A.; Acquarini, E.; Ajdukovic, D.; Ardino, V.; Böttche, M.; Bondjers, K.; Bragesjö, M.; Dragan, M.; Grajewski, P.; Figueiredo-Braga, M.; et al. Stressors, coping and symptoms of adjustment disorder in the course of the COVID-19 pandemic—Study protocol of the European Society for Traumatic Stress Studies [ESTSS] pan-European study. Eur. J. Psychotraumatol. 2020, 11, 1780832. [Google Scholar] [CrossRef] [PubMed]
- Lotzin, A.; Krause, L.; Acquarini, E.; Ajdukovic, D.; Ardino, V.; Arnberg, F.; Böttche, M.; Bragesjö, M.; Dragan, M.; Figueiredo-Braga, M.; et al. Risk and protective factors, stressors, and symptoms of adjustment disorder during the COVID-19 pandemic—First results of the ESTSS COVID-19 pan-European ADJUST Study. Eur. J. Psychotraumatol. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Kazlauskas, E.; Gegieckaite, G.; Eimontas, J.; Zelviene, P.; Maercker, A. A Brief Measure of the International Classification of Diseases—11 Adjustment Disorder: Investigation of Psychometric Properties in an Adult Help-Seeking Sample. Psychopathol. 2018, 51, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Ben-Ezra, M.; Mahat-Shamir, M.; Lorenz, L.; Lavenda, O.; Maercker, A. Screening of adjustment disorder: Scale based on the ICD-11 and the Adjustment Disorder New Module. J. Psychiatr. Res. 2018, 103, 91–96. Available online: https://www.sciencedirect.com/science/article/pii/S0022395618303595 (accessed on 1 June 2022). [CrossRef]
- Prins, A.; Bovin, M.J.; Kimerling, R.; Kaloupek, D.G.; Marx, B.P.; Pless-Kaiser, A.; Schnurr, P.P. The Primary Care PTSD Screen for DSM-5 [PC-PTSD-5]: National Center for PTSD. 2015. Available online: https://www.ptsd.va.gov/professional/assessment/screens/pc-ptsd.asp (accessed on 1 June 2022).
- Bovin, M.J.; Kimerling, R.; Weathers, F.W.; Prins, A.; Marx, B.P.; Post, E.P.; Schnurr, P.P. Diagnostic Accuracy and Acceptability of the Primary Care Posttraumatic Stress Disorder Screen for the Diagnostic and Statistical Manual of Mental Disorders [Fifth Edition] Among US Veterans. JAMA Netw. Open 2021, 4, e2036733. [Google Scholar] [CrossRef]
- Prins, A.; Bovin, M.; Smolenski, D.J.; Marx, B.P.; Kimerling, R.; Jenkins-Guarnieri, M.A.; Kaloupek, D.; Schnurr, P.P.; Kaiser, A.P.; Leyva, Y.E.; et al. The Primary Care PTSD Screen for DSM-5 [PC-PTSD-5]: Development and Evaluation within a Veteran Primary Care Sample. J. Gen. Intern. Med. 2016, 31, 1206–1211. [Google Scholar] [CrossRef]
- Spoont, M.R.; Williams, J.W.; Kehle-Forbes, S.; Nieuwsma, J.A.; Mann-Wrobel, M.C.; Gross, R. Does This Patient Have Posttraumatic Stress Disorder? Rational Clinical Examination Systematic Review. JAMA 2015, 314, 501–510. Available online: https://www.ptsd.va.gov/professional/articles/article-pdf/id44256.pdf (accessed on 1 June 2022). [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.; Löwe, B. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics 2009, 50, 613–621. [Google Scholar] [CrossRef]
- Khubchandani, J.; Brey, R.; Kotecki, J.; Kleinfelder, J.; Anderson, J. The Psychometric Properties of PHQ-4 Depression and Anxiety Screening Scale among College Students. Arch. Psychiatr. Nurs. 2016, 30, 457–462. [Google Scholar] [CrossRef]
- Lotzin, A.; Ketelsen, R.; Krause, L.; Schäfer, I. Pandemic Coping Scale-Validation of a Brief Measure of Coping in a German Sample during the COVID-19 Pandemic. Available online: https://www.researchsquare.com/article/rs-400361/latest.pdf (accessed on 1 June 2022).
- Knief, U.; Forstmeier, W. Violating the normality assumption may be the lesser of two evils. Behav. Res. Methods 2021, 53, 2576–2590. [Google Scholar] [CrossRef]
- Haynes, W. Bonferroni Correction. In Encyclopedia of Systems Biology; Dubitzky, W., Wolkenhauer, O., Cho, K.-H., Yokota, H., Eds.; Springer: New York, NY, USA, 2013; p. 154. [Google Scholar]
- Cheema, J.R. University of Illinois at Urbana-Champaign Some General Guidelines for Choosing Missing Data Handling Methods in Educational Research. J. Mod. Appl. Stat. Methods 2014, 13, 53–75. [Google Scholar] [CrossRef]
- Huque, H.; Carlin, J.B.; Simpson, J.A.; Lee, K.J. A comparison of multiple imputation methods for missing data in longitudinal studies. BMC Med. Res. Methodol. 2018, 18, 168. [Google Scholar] [CrossRef]
- White, I.R.; Royston, P.; Wood, A.M. Multiple imputation using chained equations: Issues and guidance for practice. Stat. Med. 2010, 30, 377–399. [Google Scholar] [CrossRef]
- Richardson, J.T.E. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Fullana, M.A.; Hidalgo-Mazzei, D.; Vieta, E.; Radua, J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J. Affect. Disord. 2020, 275, 80–81. [Google Scholar] [CrossRef]
- Fluharty, M.; Fancourt, D. How have people been coping during the COVID-19 pandemic? Patterns and predictors of coping strategies amongst 26,016 UK adults. BMC Psychol. 2021, 9, 107. [Google Scholar] [CrossRef]
- Brunet, A.; Rivest-Beauregard, M.; Lonergan, M.; Cipolletta, S.; Rasmussen, A.; Meng, X.; Nematollah, J.; Sara, R.; Julia, S.; Adam, D.B.; et al. PTSD is not the emblematic disorder of the COVID-19 pandemic; adjustment disorder is. BMC Psychiatry 2022, 22, 300. [Google Scholar] [CrossRef]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact and associated factors during the initial stage of the Coronavirus [COVID-19] Pandemic among the general population in Spain. Front. Psychol. 2020, 11, 1540. [Google Scholar] [CrossRef]
- WHO. WHO Characterizes COVID-19 as a Pandemic. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed on 1 June 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).