From Research into Practice: Converting Epidemiological Data into Relevant Information for Planning of Regional Health Services for Refugees in Germany
Abstract
:1. Introduction
- European Health Interview Survey (EHIS), general health, pain, chronic illness
- Patient Health Questionnaire-2 (PHQ-2; depression) and General Anxiety Disorder-2 (GAD2)
2. Materials and Methods
- Data of counties on all ASR living in Baden-Wuerttemberg stratified for sex and nationality (© Statistisches Bundesamt (Destatis), 2020|state: 18 March 2020/08:33:28; reporting date: 31 December 2018)
- Data of age-groups of recipients of asylum seeker benefits from the regional data-base (© Statistische Ämter des Bundes und der Länder, Deutschland, 2020; reporting date: 31 December 2018)
3. Results
3.1. Description of Sample
“The coordination with regard to the topic of health is only possible to a limited extent and we simply have to see where we have space for residents when we receive allocations from the initial reception centres of course, our first priority is the question of what kind of accommodation is best suited for residents, individuals or families with what needs, and only then, in second place, does the supply at the location also play a role.”(P3)
“In my area of responsibility, there is no planning of health… the healthcare… of people with a migrant background. I am also not aware of any systematic planning on the part of the health department or other offices.”(P7)
3.2. Types of Decisions Made
“If any needs have been reported so far, then it was immediately tried to involve any specialised institutions or to start some kind of cooperation, simply in order to be able to cover the needs. Yes, like it was with the social psychiatric services, for example. The need was acute and the corresponding [psychosocial centre] was called in and the cooperation was organised. We were able to cover some needs well in this way for others there were no capacities left.”(P7)
“We have to accommodate the people accordingly and then, in the same breath, so to speak, we are informed or have been informed that three of the five children are in wheelchairs. And then we have to accommodate them. (…) We were actually lucky that we had a suitable ground floor flat that we could make available to the family. We then had a ramp built, also at our own expense, to create access via the balcony, because there were two steps to climb.”(P4)
“But as soon as it came to psychological problems, we realised that there was almost no access to the regular systems. (…) And we said that this must change urgently, because the number of people with psychological problems or disorders has simply increased in the last two years. (…) And we have responded to this with this personnel recruitment.”(P5)
“In the area of health, I don’t even see the big decisions. For example, I think it is important that we support a project for traumatised refugees in the area of health (…). Because we saw that otherwise we wouldn’t be able to (…) treat people who otherwise couldn’t or wouldn’t want to go to treatment. These are the things that can be decided on a smaller scale. The difficult overall decisions are: what is the prognosis, how many refugees are coming, how many are leaving, how much accommodation capacity do I need, and if I no longer need a capacity, dismantling the accommodation and thus also dismantling staff, not only in social services, but in principle. So, just as we built up in 2015, we will also reduce again. These are the decisions.”(P1)
“For example, corona (…) has indeed influenced our lives very much and also made them very difficult. But at the same time, many have also benefited from it. One example is, with a lot of discussion, we managed to reduce the number of refugees in a reception centre. (…) And that was also done politically, had to be agreed, [among the different parties]. And we had a lot of discussions about that.”(P14)
“What effect do we want to achieve together, in the district or in our community, what do we want to work towards together?”(P10)
“The municipalities in our district pay a district levy. And the goal is to keep the district levy (…) in a fair ratio, so that the municipality can also, I don’t know, build a kindergarten. Yes, that’s the dilemma the district faces, we can’t just decide for ourselves.”(P1)
3.3. Decision-Making Processes
“You notice [a health issue] by how many police incidents you have, by how many disturbances within the accommodation you have, by how often a social worker says: ‘I have someone here, I can’t reach him at all with normal speech and writing, because he’s off somewhere in his head’.”(P5)
“Then I report it to my superior, who then forwards it to the head of the office, and then we see what conditions [are given] and to what extent we can change it, whether it is somehow offered by the ministry [government] or whether there are any offers here in the district that we don’t know about yet, or whether we have to do something to change it. So sometimes, it is tied to political decisions/sometimes there are infrastructures and sometimes there is nothing.”(P12)
“(…) there is a lack of scientific data and study basis. Especially for the health of refugees. And health data that is also collected explicitly for the group.”(P10)
“(…) in the end the politicians, the local politicians, the local council is the one who has to say, has to decide on the basis of the data we give them, from the health reporting, from the documentation we do on the project.”(P13)
“Because what I think is still a major shortcoming in health promotion for refugees or immigrants in general is that too little… exchange happens in a structured way. It is selective, like you know people. But I believe that this intersectionality should be expanded more strongly.”(P2)
“So, data protection, yes, unspeakable sometimes in this field… because actually it also prevents, it’s also a certain hindrance.”(P1)
3.4. Data Required for Decision-Making
“It would of course be nice for us the data transfer would be a bit more intensive then we would know exactly what kind of people we would have to adjust to and what we would actually have to offer.”(P3)
“In Germany we have a great lack of translation of health data. So that one can, so to speak, gain the health data, because many people experience a lot or know a lot, but (…) you cannot use that. (…) So the question is always how well you can link [experience and knowledge] to really get real data, to find out about certain problem areas.”(P14)
“To be quite honest, the bare figures were helpful because everyone understands them. And we have to be aware that in our committees, in the district council or in the municipal committees, there are people who have been elected. They may not have any in-depth knowledge of this topic. This means that it has to be presented in a relatively simple way.”(P1)
“And especially when there are political forces that are rather against refugees and do not want to invest money there. I think it is then also a higher responsibility, […] to make very transparent and easy to understand what [data tools] can and cannot do.”(P2)
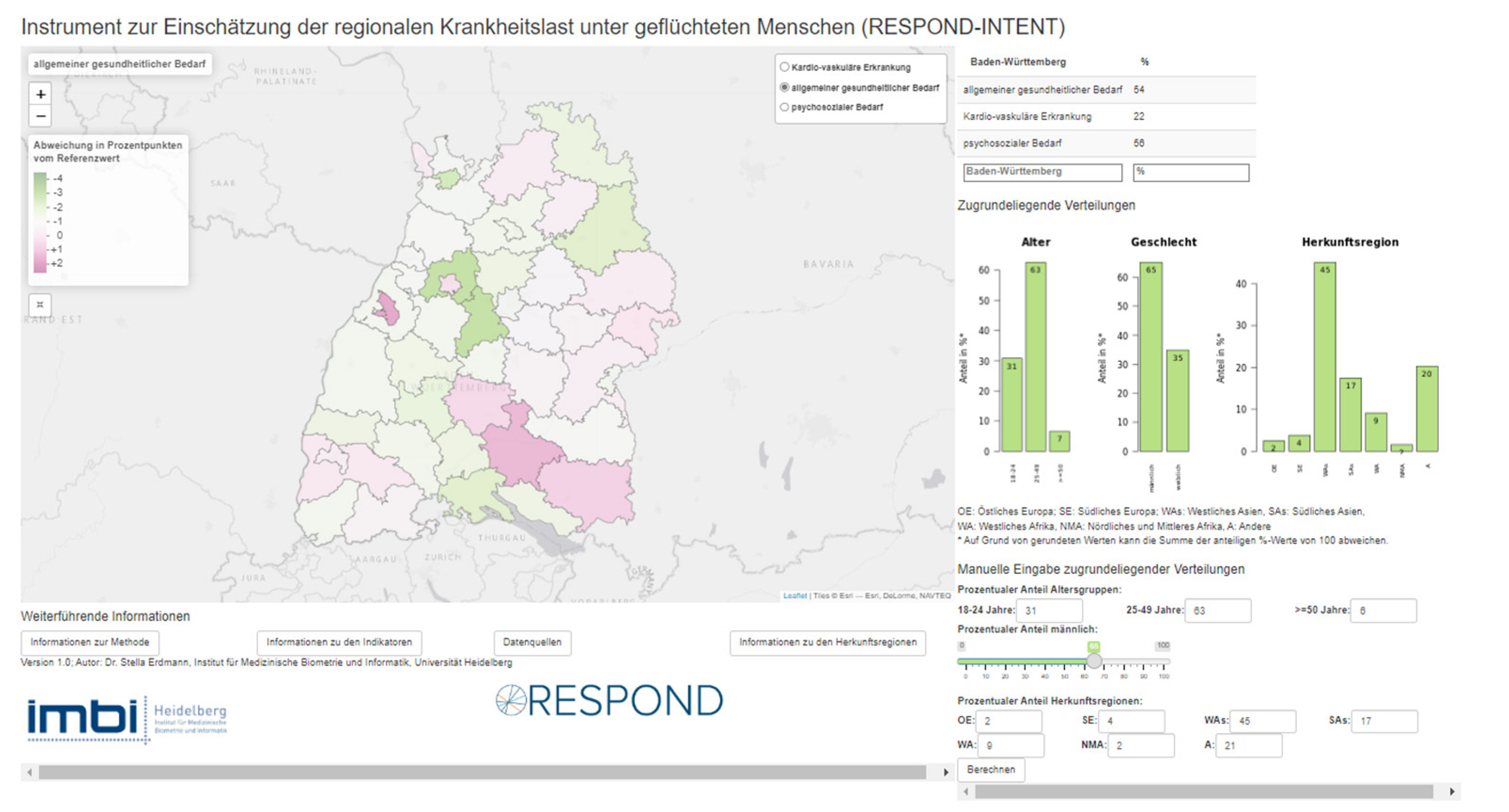
3.5. Usability and Usefulness of RESPOND-INTENT Dashboard
3.5.1. Usability
“Because people from the field often don’t have much time, they want information quickly.”(P10)
“And I know that in the past, when we didn’t work carefully, we suddenly argued with things that simply weren’t true and that’s why you always have to be clear when you work with data: Ok, are they all correct, can I read them well? And if that is not the case (…) then you can just quickly draw conclusions that are not at all reliable in reality. I consider that difficult.”(P5)
“Yes, so in three parts it is best. First of all to have tables or graphics, then someone introduces me to what I see on these tables and graphics and at the end there is a summarised sheet with ‘this is why you should do this’.”(P7)
3.5.2. Usefulness in Everyday Work
“So, it’s just very broad and generic. (…) That’s why I have to be honest and say that we look more at the individual case (…) what does [the person] have and what does [the person] need? And from that we conclude: oh, we have a larger group and for the larger group we have to do something.”(P1)
“I think it makes sense, and is also necessary, in order to get a very good, general overview at first. We don’t have any detailed data here, but we can already derive certain trends, so to speak.”(P10)
“I would use it as a basis in my work and (…) maybe I would also use it in meetings when it comes to financial topics, because I always need a good basis and a good line of argumentation and thus create a basis [for that]. So that would already be something where I think one could work with it and also take up arguments…”(P3)
“The situation at the beginning is of course completely different and the need is also different than if, for example, people with a migrant background who have been in Germany for a very long time were to be included or who are perhaps already in subsequent accommodation for which integration managers are responsible.”(P9)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations High Commissioner for Refugees. Global Trends—Forced Displacement in 2020; United Nations High Commissioner for Refugees: Copenhagen, Denmark, 2021. [Google Scholar]
- European Commission. Statistics on Migration to Europe: Seeking Asylum in Europe. Available online: https://ec.europa.eu/info/strategy/priorities-2019-2024/promoting-our-european-way-life/statistics-migration-europe_en#asylum (accessed on 7 April 2022).
- Abubakar, I.; Aldridge, R.W.; Devakumar, D.; Orcutt, M.; Burns, R.; Barreto, M.L.; Dhavan, P.; Fouad, F.M.; Groce, N.; Guo, Y.; et al. The UCL–Lancet Commission on Migration and Health: The health of a world on the move. Lancet 2018, 392, 2606–2654. [Google Scholar] [CrossRef] [Green Version]
- Bradby, H. Public Health Aspects of Migrants Health: A Review of the Evidence on Health Status for Refugees and Asylum Seekers in the European Region; World Health Organisation Regional Office for Europe: Copenhagen, Denmark, 2015; ISBN 978-92-890-5110-1. [Google Scholar]
- Lebano, A.; Hamed, S.; Bradby, H.; Gil-Salmerón, A.; Durá-Ferrandis, E.; Garcés-Ferrer, J.; Azzedine, F.; Riza, E.; Karnaki, P.; Zota, D.; et al. Migrants’ and refugees’ health status and healthcare in Europe: A scoping literature review. BMC Public Health 2020, 20, 1039. [Google Scholar] [CrossRef] [PubMed]
- Bozorgmehr, K.; Biddle, L.; Rohleder, S.; Puthoopparambil, S.; Jahn, R. What Is the Evidence on Availability and Integration of Refugee and Migrant Health Data in Health Information Systems in the WHO European Region? WHO Regional Office for Europe: Copenhagen, Denmark, 2019; ISBN 9289054425. [Google Scholar]
- Chiesa, V.; Chiarenza, A.; Mosca, D.; Rechel, B. Health records for migrants and refugees: A systematic review. Health Policy 2019, 123, 888–900. [Google Scholar] [CrossRef] [PubMed]
- Rechel, B.; Mladovsky, P.; Devillé, W. Monitoring migrant health in Europe: A narrative review of data collection practices. Health Policy 2012, 105, 10–16. [Google Scholar] [CrossRef] [Green Version]
- Biddle, L.; Menold, N.; Bentner, M.; Nöst, S.; Jahn, R.; Ziegler, S.; Bozorgmehr, K. Health monitoring among asylum seekers and refugees: A state-wide, cross-sectional, population-based study in Germany. Emerg. Themes Epidemiol. 2019, 16, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biddle, L.; Hintermeier, M.; Mohsenpour, A.; Sand, M.; Bozorgmehr, K. Monitoring the health and healthcare provision for refugees in collective accommodation centres: Results of the population-based survey RESPOND. J. Health Monit. 2021, 6, 7–29. [Google Scholar] [CrossRef] [PubMed]
- Gößwald, A.; Lange, M.; Dölle, R.; Hölling, H. Die erste Welle der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1): Gewinnung von Studienteilnehmenden, Durchführung der Feldarbeit und Qualitätsmanagement. Bundesgesundheitsbl 2013, 56, 611–619. [Google Scholar] [CrossRef] [Green Version]
- Santos-Hövener, C.; Schumann, M.; Schmich, P.; Gößwald, A.; Rommel, A.; Ziese, T.; Lampert, T. Verbesserung der Informationsgrundlagen zur Gesundheit von Menschen mit Migrationshintergrund. Projektbeschreibung und erste Erkenntnisse von IMIRA. J. Health Monit. 2019, 4, 49–61. [Google Scholar] [CrossRef]
- Brücker, H.; Rother, N.; Schupp, J. (Eds.) IAB-BAMF-SOEP-Befragung von Geflüchteten 2016; Studiendesign, Feldergebnisse Sowie Analysen zu Schulischer wie Beruflicher Qualifikation, Sprachkenntnissen Sowie Kognitiven Potenzialen; Stand: Februar 2018 (korrigierte Fassung der Veröffentlichung aus dem Jahr 2017); Bundesamt für Migration und Flüchtlinge: Nürnberg, Germany, 2018; ISBN 978-3-944674-13-1. [Google Scholar]
- Robert-Koch-Institut. Dashboard “Gesundheit in Deutschland Aktuell”. Available online: https://www.rki.de/DE/Content/Gesundheitsmonitoring/Studien/GEDA_Dashboard/GEDA_Dashboard_node.html (accessed on 19 April 2022).
- Bozorgmehr, K.; Nöst, S.; Thaiss, H.M.; Razum, O. Die gesundheitliche Versorgungssituation von Asylsuchenden. Bundesgesundheitsbl 2016, 59, 545–555. [Google Scholar] [CrossRef] [Green Version]
- Wahedi, K.; Biddle, L.; Jahn, R.; Ziegler, S.; Kratochwill, S.; Pruskil, S.; Noest, S.; Bozorgmehr, K. Medizinische Versorgung von Asylsuchenden in Erstaufnahmeeinrichtungen. Bundesgesundheitsbl 2020, 63, 1460–1469. [Google Scholar] [CrossRef]
- Wendel, K. Unterbringung von Flüchtlingen in Deutschland: Regelungen und Praxis der Bundesländer im Vergleich. 2014. Available online: https://www.proasyl.de/wp-content/uploads/2014/09/Laendervergleich_Unterbringung_2014-09-23_02.pdf (accessed on 7 June 2021).
- Spura, A.; Kleinke, M.; Robra, B.-P.; Ladebeck, N. Wie erleben Asylsuchende den Zugang zu medizinischer Versorgung? Bundesgesundheitsbl 2017, 60, 462–470. [Google Scholar] [CrossRef] [PubMed]
- Gold, A.W.; Perplies, C.; Rast, E.; Bozorgmehr, K.; Biddle, L. Gesundheitliche Versorgung von geflüchteten Menschen—Eine Erhebung unter Sozialarbeiter*innen in Baden-Württemberg. In Sektion Health Equity Studies & Migration—Report Series; heiDOK: Heidelberg, Germany, 2021; Volume 1. [Google Scholar] [CrossRef]
- Gottlieb, N.; Schülle, M. An overview of health policies for asylum-seekers in Germany. Health Policy 2021, 125, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Mirzoev, T.N.; Green, A.T. Planning, for Public Health Policy. In International Encyclopedia of Public Health; Elsevier: Amsterdam, The Netherlands, 2017; pp. 489–499. ISBN 9780128037089. [Google Scholar]
- Ozegowski, S.; Sundmacher, L. Wie “bedarfsgerecht” ist die Bedarfsplanung? Eine Analyse der regionalen Verteilung der vertragsärztlichen Versorgung. Gesundheitswesen 2012, 74, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Kolenikov, S. Calibrating Survey Data using Iterative Proportional Fitting (Raking). Stata J. 2014, 14, 22–59. [Google Scholar] [CrossRef] [Green Version]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm. Policy Ment. Health 2015, 42, 533–544. [Google Scholar] [CrossRef] [Green Version]
- Albert, B.; Tullis, T. Measuring the User Experience: Collecting, Analyzing, and Presenting Usability Metrics, 2nd ed.; Morgan Kauffmann: Burlington, MA, USA; Elsevier: Waltham, MA, USA, 2013; ISBN 978-0-12-415781-1. [Google Scholar]
- Nielsen Norman Group. Thinking Aloud: The #1 Usability Tool. Available online: https://www.nngroup.com/articles/thinking-aloud-the-1-usability-tool/ (accessed on 20 May 2022).
- VERBI Software. MAXQDA 2020; VERBI Software: Berlin, Germany, 2020. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Chang, W.; Cheng, J.; Allaire, J.; Sievert, C.; Schloerke, B.; Xie, Y.; Allen, J.; McPherson, J.; Dipert, A.; Borges, B. Shiny: Web Application Framework for R. Available online: https://CRAN.R-project.org/package=shiny (accessed on 3 May 2022).
- Perrier, V.; Meyer, F.; Granjon, D. shinyWidgets: Custom Inputs Widgets for Shiny. 2021. Available online: https://CRAN.R-project.org/package=shinyWidgets (accessed on 3 May 2022).
- Cheng, J.; Karambelkar, B.; Xie, Y. leaflet: Create Interactive Web Maps with the JavaScript ‘Leaflet’ Library. Available online: https://CRAN.R-project.org/package=leaflet (accessed on 3 May 2022).
- Karambelkar, B.; Schloerke, B. leaflet.extras: Extra Functionality for ‘leaflet’ Package. Available online: https://CRAN.R-project.org/package=leaflet.extras (accessed on 3 May 2022).
- Tennekes, M. tmap: Thematic Maps in R. J. Stat. Softw. 2018, 84, 1–39. [Google Scholar] [CrossRef] [Green Version]
- Wickham, H.; Miller, E. haven: Import and Export ‘SPSS’, ‘Stata’ and ‘SAS’ Files. Available online: https://CRAN.R-project.org/package=haven (accessed on 3 May 2022).
- Wickham, H.; Bryan, J. Readxl: Read Excel Files. Available online: https://CRAN.R-project.org/package=readxl (accessed on 3 May 2022).
- Pebesma, E. Simple Features for R: Standardized Support for Spatial Vector Data. R J. 2018, 10, 439–446. [Google Scholar] [CrossRef] [Green Version]
- Neuwirth, E. RColorBrewer: ColorBrewer Palettes. Available online: https://CRAN.R-project.org/package=RColorBrewer (accessed on 3 May 2022).
- Barthélemy, J.; Suesse, T. mipfp: An R Package for Multidimensional Array Fitting and Simulating Multivariate Bernoulli Distributions. J. Stat. Softw. Code Snippets 2018, 86, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Lovelace, R.; Dumont, M. Spatial Microsimulation with R; CRC Press: Boca Raton, FL, USA; Taylor & Francis Group: Boca Raton, FL, USA, 2016; ISBN 9781498711548. [Google Scholar]
- Oborn, E.; Barrett, M.; Racko, G. Knowledge translation in healthcare: Incorporating theories of learning and knowledge from the management literature. J. Health Organ. Manag. 2013, 27, 412–431. [Google Scholar] [CrossRef]
- Buse, K.; Mays, N.; Walt, G. Making Health Policy; McGraw-Hill: Maidenhead, UK; Open University Press: New York, NY, USA, 2012; ISBN 978-0-33-524634-2. [Google Scholar]
- Baumbusch, J.L.; Kirkham, S.R.; Khan, K.B.; McDonald, H.; Semeniuk, P.; Tan, E.; Anderson, J.M. Pursuing common agendas: A collaborative model for knowledge translation between research and practice in clinical settings. Res. Nurs. Health 2008, 31, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Rushmer, R.; Ward, V.; Nguyen, T.; Kuchenmüller, T. Knowledge Translation: Key Concepts, Terms and Activities. In Population Health Monitoring: Climbing the Information Pyramid; Verschuuren, M., van Oers, H., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 127–150. ISBN 978-3-319-76562-4. [Google Scholar]
- Blanchet, K.; Nam, S.L.; Ramalingam, B.; Pozo-Martin, F. Governance and Capacity to Manage Resilience of Health Systems: Towards a New Conceptual Framework. Int. J. Health Policy Manag. 2017, 6, 431–435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jahn, R.; Rohleder, S.; Qreini, M.; Erdmann, S.; Kaur, S.; Aluttis, F.; Bozorgmehr, K. Health monitoring of refugees in reception centres for asylum seekers: Decentralized surveillance network for the analysis of routine medical data. J. Health Monit. 2021, 6, 30–52. [Google Scholar] [CrossRef] [PubMed]
| Participant | Age Group | Gender | Affiliation | Work Experience | Responsibility | Type of Tasks (Assigned by the Study Team) |
|---|---|---|---|---|---|---|
| P1 | 40–49 | female | Office for Integration and Migration | 1–3 years | 3–29 accommodation facilities | organisational |
| P2 | 40–49 | female | NGO | 1–3 years | n.a. | operational |
| P3 | 30–39 | female | Office for Integration and Migration | 4–10 years | 3–29 accommodation facilities | organisational |
| P4 | 30–39 | male | City administration | 4–10 years | 100–400 ASR | operational |
| P5 | 30–39 | male | Office for Integration and Migration | 1–3 years | 3–29 accommodation facilities | organisational |
| P6 | 40–49 | female | NGO | 4–10 years | 100–400 ASR | operational |
| P7 | 30–39 | female | Office for Integration and Migration | 1–3 years | >4000 ASR | organisational |
| P8 | 40–49 | female | Office for Integration and Migration | 4–10 years | >4000 ASR | operational |
| P9 | 30–39 | female | Office for Integration and Migration | 4–10 years | >4000 ASR | operational |
| P10 | 30–39 | female | NGO | 1–3 years | >4000 ASR | operational |
| P11 | 50–59 | male | Health department | 4–10 years | n.a. | organisational |
| P12 | 40–49 | male | Office for Integration and Migration | 4–10 years | 100–400 ASR | organisational |
| P13 | 60–69 | male | Health department | 11–30 years | n.a. | organisational |
| P14 | 60–69 | female | Health department | 11–30 years | 3–29 accommodation facilities | organisational |
| Requirements Mentioned for Data Presentation | Practical Implications | Present in the RESPOND-INTENT Dashboard (Yes/No/Can Be Improved) |
|---|---|---|
| Content-related requirements | ||
| Introductory text “Also, [refers to an introductory text] maybe just very briefly: What can I actually do with this dashboard, what functions are there, what can I find out with it? (…) [like] a short guide.” (P10) “[Information] on the origin (…), what the thought behind it is, what benefits it can have.” (P4) | Dashboards should provide an introductory text with an explanatory and summarizing character so that users quickly understand what the data is about. | no |
| Lay-person language “Exactly, so what I think would be very important for me is to make the dashboard accessible to people without scientific training. So, as far as possible, to try to use terms in the application of the dashboard (…) that one might use quite naturally.” (P10) | Not all users might be familiar with technical terms (e.g., from the health field or statistics), thus the data display should use simple words so that lay persons may understand everything. | can be improved |
| Relevant health indicators “I think it’s really good that this division into three relatively/or two very specific needs/that you have separated into physical and mental [health], that’s very important, because they are two completely different pairs of shoes. (…) That is extremely important. Otherwise it would really be a tool that would not be usable.” (P5) | When selecting variables (e.g., health indicators) for a dashboard, their relevance to potential users should always be considered. | yes |
| Comparative datasets “If you can then say “the [health] need here is much higher than the overall average”, that would also be something that helps with an argument.” (P2) “So, it is important, of course, to always look at what the relation to the general population is.” (P13) | It is very helpful to include a comparative data set so that users can contextualise the data. This might be other population sub-groups or the general population. | no |
| Technical requirements | ||
| Interactive graphs “So, when I click on a district or a city and the statistics appear directly, I think it’s useful that I get the information directly.” (P12) | Easily accessible pop-up windows are helpful to provide further information on the data graphs. In the case of RESPOND-INTENT it concerns the districts on the map, however this might also work for lines or bars in graphs. | yes |
| Indicator information “And ideally, if I could wish, then in some way, when I move over here [the indicators and other terms]—such a beautiful bubble [window including more information] would somehow pop up.” (P2) | Background information about important buzzwords/terms (e.g., indicators) should be easily accessible and easy to find. Ideally, pop-up windows could be used. | no |
| Indicator selection and adjustment “So, it would be good if it could be possible to play around more with the data in order to get a little finer differentiation out of it.” (P5) | Users might want to explore the given data in more detail, therefore functions for manual adjustments and possibilities for users to interact with the data would be recommendable. | can be improved |
| Comparability functions “So, what we have just discussed, such a comparability between districts (…) is definitely not irrelevant.” (P11) | Dashboards could include functions to compare data across different geographical regions. For example, in the case of RESPOND-INTENT this would be a function to compare values of different districts. | no |
| Data export “So, what I would still like is if you could export them [the data], maybe as a pdf or also as an Excel file.” (P10) | Users might want to use the information provided by the dashboards for other purposes. Thus, an export function as PDF, Excel file or graph would be recommendable. | no |
| Timeliness and maintenance of data “The question would be, how is this maintained or how does the maintenance of this system work?” (P4) | To contextualise the data provided by the dashboard, it is recommendable to provide information about the timeliness and maintenance of the underlying database. | no |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hintermeier, M.; Gold, A.W.; Erdmann, S.; Perplies, C.; Bozorgmehr, K.; Biddle, L. From Research into Practice: Converting Epidemiological Data into Relevant Information for Planning of Regional Health Services for Refugees in Germany. Int. J. Environ. Res. Public Health 2022, 19, 8049. https://doi.org/10.3390/ijerph19138049
Hintermeier M, Gold AW, Erdmann S, Perplies C, Bozorgmehr K, Biddle L. From Research into Practice: Converting Epidemiological Data into Relevant Information for Planning of Regional Health Services for Refugees in Germany. International Journal of Environmental Research and Public Health. 2022; 19(13):8049. https://doi.org/10.3390/ijerph19138049
Chicago/Turabian StyleHintermeier, Maren, Andreas W. Gold, Stella Erdmann, Clara Perplies, Kayvan Bozorgmehr, and Louise Biddle. 2022. "From Research into Practice: Converting Epidemiological Data into Relevant Information for Planning of Regional Health Services for Refugees in Germany" International Journal of Environmental Research and Public Health 19, no. 13: 8049. https://doi.org/10.3390/ijerph19138049
APA StyleHintermeier, M., Gold, A. W., Erdmann, S., Perplies, C., Bozorgmehr, K., & Biddle, L. (2022). From Research into Practice: Converting Epidemiological Data into Relevant Information for Planning of Regional Health Services for Refugees in Germany. International Journal of Environmental Research and Public Health, 19(13), 8049. https://doi.org/10.3390/ijerph19138049






