Infodemic, Institutional Trust, and COVID-19 Vaccine Hesitancy: A Cross-National Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. Measures
2.3. Data Handling and Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 13 February 2022).
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Tram, K.H.; Saeed, S.; Bradley, C.; Fox, B.; Eshun-Wilson, I.; Mody, A.; Geng, E. Deliberation, dissent, and distrust: Understanding distinct drivers of Coronavirus Disease 2019 vaccine hesitancy in the United States. Clin. Infect. Dis. 2021, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Luk, T.T.; Zhao, S.; Wu, Y.; Wong, J.Y.; Wang, M.P.; Lam, T.H. Prevalence and determinants of SARS-CoV-2 vaccine hesitancy in Hong Kong: A population-based survey. Vaccine 2021, 39, 3602–3607. [Google Scholar] [CrossRef]
- Machida, M.; Nakamura, I.; Kojima, T.; Saito, R.; Nakaya, T.; Hanibuchi, T.; Takamiya, T.; Odagiri, Y.; Fukushima, N.; Kikuchi, H. Acceptance of a COVID-19 vaccine in Japan during the COVID-19 pandemic. Vaccines 2021, 9, 210. [Google Scholar] [CrossRef]
- Zarocostas, J. How to fight an infodemic. Lancet 2020, 395, 676. [Google Scholar] [CrossRef]
- Loomba, S.; de Figueiredo, A.; Piatek, S.J.; de Graaf, K.; Larson, H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat. Hum. Behav. 2021, 5, 337–348. [Google Scholar] [CrossRef]
- Rathore, F.A.; Farooq, F. Information overload and infodemic in the COVID-19 pandemic. J. Pak. Med. Assoc. 2020, 70, S162–S165. [Google Scholar] [CrossRef]
- Niederdeppe, J.; Fowler, E.F.; Goldstein, K.; Pribble, J. Does local television news coverage cultivate fatalistic beliefs about cancer prevention? J. Commun. 2010, 60, 230–253. [Google Scholar] [CrossRef] [Green Version]
- Crook, B.; Stephens, K.K.; Pastorek, A.E.; Mackert, M.; Donovan, E.E. Sharing health information and influencing behavioral intentions: The role of health literacy, information overload, and the Internet in the diffusion of healthy heart information. Health Commun. 2016, 31, 60–71. [Google Scholar] [CrossRef] [PubMed]
- Hong, H.; Kim, H.J. Antecedents and consequences of information overload in the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9305. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.L. COVID-19 information seeking on digital media and preventive behaviors: The mediation role of worry. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 677–682. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, L.; Basdeo, D.; Wang, H. Public trust, information sources and vaccine willingness related to the COVID-19 pandemic in Trinidad and Tobago: An online cross-sectional survey. Lancet Reg. Health Am. 2021, 3, 100051. [Google Scholar] [CrossRef]
- Trent, M.; Seale, H.; Chughtai, A.A.; Salmon, D.; MacIntyre, C.R. Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: A comparative survey of five large cities in the United States, United Kingdom, and Australia. Vaccine 2021, 40, 2498–2505. [Google Scholar] [CrossRef]
- Sturgis, P.; Brunton-Smith, I.; Jackson, J. Trust in science, social consensus and vaccine confidence. Nat. Hum. Behav. 2021, 5, 1528–1534. [Google Scholar] [CrossRef]
- Islam, M.S.; Sarkar, T.; Khan, S.H.; Kamal, A.M.; Hasan, S.M.; Kabir, A.; Yeasmin, D.; Islam, M.A.; Chowdhury, K.I.A.; Anwar, K.S. COVID-19–related infodemic and its impact on public health: A global social media analysis. Am. J. Trop. Med. Hyg. 2020, 103, 1621–1629. [Google Scholar] [CrossRef]
- Shahi, G.K.; Dirkson, A.; Majchrzak, T.A. An exploratory study of COVID-19 misinformation on twitter. Online Soc. Netw. Media 2021, 22, 100104. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e132. [Google Scholar] [CrossRef]
- The Policy Institute. Coronavirus: Vaccine Misinformation and the Role of Social Media. Available online: https://www.kcl.ac.uk/policy-institute/assets/coronavirus-vaccine-misinformation.pdf (accessed on 10 February 2022).
- Farooq, A.; Laato, S.; Islam, A.N. Impact of online information on self-isolation intention during the COVID-19 pandemic: Cross-sectional study. J. Med. Internet Res. 2020, 22, e19128. [Google Scholar] [CrossRef]
- Brennen, J.S.; Simon, F.M.; Howard, P.N.; Nielsen, R.K. Types, Sources, and Claims of COVID-19 Misinformation. Reuters Institute for the Study of Journalism Factsheet 2020, April. Available online: https://reutersinstitute.politics.ox.ac.uk/sites/default/files/2020-04/Brennen%20-%20COVID%2019%20Misinformation%20FINAL%20(3).pdf (accessed on 8 February 2022).
- Soroya, S.H.; Farooq, A.; Mahmood, K.; Isoaho, J.; Zara, S. From information seeking to information avoidance: Understanding the health information behavior during a global health crisis. Inf. Process Manag. 2021, 58, 102440. [Google Scholar] [CrossRef] [PubMed]
- Hara, M.; Ishibashi, M.; Nakane, A.; Nakano, T.; Hirota, Y. Differences in COVID-19 vaccine acceptance, hesitancy, and confidence between healthcare workers and the general population in Japan. Vaccines 2021, 9, 1389. [Google Scholar] [CrossRef]
- Lee, J.; Sniderman, B.; Marquad, B.; Galletto, N.; Geeanpersadh, P.; Cherny, M. Embedding Trust into COVID-19 Recovery. Four Dimensions of Stakeholder Trust. Deloitte Insights 2020, 1–15. Available online: https://www2.deloitte.com/content/dam/insights/us/articles/6720_embedding-trust-into-COVID-19-recovery/DI_Embedding-trust-COVID-recovery.pdf (accessed on 5 February 2022).
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef] [PubMed]
- Kwok, K.O.; Li, K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef] [PubMed]
- Heyerdahl, L.W.; Dielen, S.; Nguyen, T.; Van Riet, C.; Kattumana, T.; Simas, C.; Vandaele, N.; Vandamme, A.; Vandermeulen, C.; Giles-Vernick, T. Doubt at the core: Unspoken vaccine hesitancy among healthcare workers. Lancet Reg. Health Eur. 2022, 12, 100289. [Google Scholar] [CrossRef]
- Al-Mulla, R.; Abu-Madi, M.; Talafha, Q.M.; Tayyem, R.F.; Abdallah, A.M. COVID-19 vaccine hesitancy in a representative education sector population in Qatar. Vaccines 2021, 9, 665. [Google Scholar] [CrossRef]

| Variable | Variable | ||||
|---|---|---|---|---|---|
| Age | n | % | COVID-19 infection of the respondent | n | % |
| 18–29 | 1349 | 21.8 | No | 5828 | 94.1 |
| 30–59 | 3423 | 55.3 | Yes | 324 | 5.2 |
| ≥60 | 1421 | 23.0 | Unknown/prefer not to answer | 41 | 0.7 |
| Sex | COVID-19 infection of family members | ||||
| Male | 3090 | 49.9 | No | 5624 | 90.8 |
| Female | 3103 | 50.1 | Yes | 521 | 8.4 |
| Education | Unknown/prefer not to answer | 48 | 0.8 | ||
| ≤Secondary | 1365 | 22.0 | Jurisdiction | ||
| ≥Tertiary | 2826 | 45.6 | Hong Kong | 1025 | 16.6 |
| Unknown/prefer not to answer | 2002 | 32.3 | Japan | 1032 | 16.7 |
| Occupation | Singapore | 1086 | 17.5 | ||
| Professional/service worker | 4033 | 65.1 | South Korea | 1084 | 17.5 |
| Manual worker | 561 | 9.1 | UK | 988 | 16.0 |
| Other/prefer not to answer | 1599 | 25.8 | US | 978 | 15.8 |
| Income | Uptake of COVID-19 vaccines | ||||
| Lowest quartile | 1525 | 24.6 | Yes | 3249 | 52.5 |
| 2nd quartile | 1529 | 24.7 | No | 2944 | 47.5 |
| 3rd quartile | 1855 | 29.9 | Acceptance of COVID-19 vaccines, mean (SD) | 5.56 | (1.72) |
| Highest quartile | 959 | 15.5 | Perceived information overload, mean (SD) | 4.18 | (1.49) |
| Unknown/prefer not to answer | 325 | 5.3 | Belief in misinformation, median (IQR) | 4 | (2–5) |
| Area | Trust in the government, median (IQR) | 5 | (3.5–6) | ||
| Urban | 4922 | 79.5 | Trust in healthcare professionals, median (IQR) | 5 | (5–6) |
| Rural | 1271 | 20.5 | Trust in NGOs, median (IQR) | 4 | (4–5) |
| Chronic disease | |||||
| No | 5056 | 81.6 | |||
| Yes | 1012 | 16.3 | |||
| Unknown/prefer not to answer | 125 | 2.0 |
| Willingness to Accept COVID-19 Vaccines | Uptake of COVID-19 Vaccines | |||
|---|---|---|---|---|
| b † | [95% CI] | b ‡ | [95% CI] | |
| Age (ref: 18–29) | ||||
| 30–59 | 0.12 * | [0.01, 0.22] | 0.44 *** | [0.29, 0.60] |
| ≥60 | 0.69 *** | [0.57, 0.82] | 1.41 *** | [1.21, 1.61] |
| Sex (ref: male) | ||||
| Female | −0.15 *** | [−0.23, −0.06] | −0.37 *** | [−0.49, −0.24] |
| Education (ref: ≤secondary) | ||||
| ≥Tertiary | 0.25 *** | [0.14, 0.36] | 0.26 ** | [0.09, 0.44] |
| Unknown | 0.21 *** | [0.09, 0.34] | 0.41 *** | [0.23, 0.60] |
| Occupation (ref: professional or service worker) | ||||
| Manual worker | −0.07 | [−0.22, 0.08] | −0.05 | [−0.27, 0.18] |
| Other | −0.01 | [−0.12, 0.09] | −0.09 | [−0.25, 0.08] |
| Income (ref: lowest quartile) | ||||
| 2nd quartile | 0.24 *** | [0.13, 0.36] | 0.21 * | [0.03, 0.39] |
| 3rd quartile | 0.41 *** | [0.30, 0.53] | 0.35 *** | [0.18, 0.53] |
| Highest quartile | 0.47 *** | [0.33, 0.60] | 0.40 *** | [0.19, 0.61] |
| Unknown | 0.04 | [−0.16, 0.24] | 0.16 | [−0.16, 0.48] |
| Area (ref: urban) | ||||
| Rural | −0.12 * | [−0.23, −0.01] | −0.07 | [−0.24, 0.10] |
| Chronic disease (ref: no) | ||||
| Yes | 0.15 ** | [0.04, 0.27] | 0.30 ** | [0.12, 0.48] |
| Unknown | −0.08 | [−0.38, 0.22] | −0.14 | [−0.59, 0.31] |
| COVID-19 infection of the respondent (ref: no) | ||||
| Yes | 0.07 | [−0.15, 0.30] | 0.67 *** | [0.29, 1.06] |
| Unknown | 0.18 | [−0.49, 0.84] | 1.44 ** | [0.40, 2.48] |
| COVID-19 infection of the respondent’s family members (ref: no) | ||||
| Yes | 0.05 | [−0.14, 0.23] | 0.33 * | [0.03, 0.63] |
| Unknown | 0.06 | [−0.55, 0.67] | −0.51 | [−1.48, 0.47] |
| Society (ref: Hong Kong) | ||||
| Japan | 0.47 *** | [0.32, 0.62] | −1.60 *** | [−1.85, −1.34] |
| Singapore | 1.16 *** | [1.01, 1.30] | 1.36 *** | [1.16, 1.56] |
| South Korea | 0.90 *** | [0.76, 1.05] | −0.92 *** | [−1.14, −0.71] |
| UK | 1.40 *** | [1.25, 1.56] | 2.11 *** | [1.88, 2.35] |
| US | 0.95 *** | [0.79, 1.11] | 1.72 *** | [1.49, 1.94] |
| Willingness to Accept COVID-19 Vaccines | Uptake of COVID-19 Vaccines | |||||||
|---|---|---|---|---|---|---|---|---|
| Model 1a | Model 2a | Model 3a | Model 4a | Model 1b | Model 2b | Model 3b | Model 4b | |
| IO | 0.20 *** | 0.12 *** | 0.09 | 0.10 *** | 0.13 *** | 0.08 ** | 0.11 | 0.06 * |
| [0.16, 0.23] | [0.09, 0.15] | [−0.02, 0.19] | [0.07, 0.13] | [0.08, 0.18] | [0.02, 0.13] | [-0.08, 0.29] | [0.01, 0.11] | |
| MI | −0.31 *** | −0.24 *** | −0.26 *** | −0.63 *** | −0.20 *** | −0.15 *** | −0.17 *** | −0.47 *** |
| [−0.34, −0.29] | [−0.27, −0.21] | [−0.29, −0.23] | [−0.73, −0.53] | [−0.25, −0.15] | [−0.20, −0.10] | [−0.22, −0.12] | [−0.65, −0.28] | |
| Trust in the government | 0.25 *** | 0.19 *** | 0.07 * | 0.18 *** | 0.01 | 0.01 | ||
| [0.22, 0.28] | [0.11, 0.27] | [0.00, 0.14] | [0.12, 0.24] | [−0.14, 0.16] | [−0.11, 0.14] | |||
| Trust in healthcare professionals | 0.27 *** | 0.33 *** | 0.23 *** | 0.16 *** | 0.45 *** | 0.27 ** | ||
| [0.23, 0.32] | [0.24,0.43] | [0.14, 0.31] | [0.09, 0.24] | [0.27, 0.64] | [0.10, 0.43] | |||
| Trust in NGOs | 0.02 | −0.06 | −0.10 ** | 0.03 | −0.15 | −0.21 ** | ||
| [−0.01, 0.06] | [−0.15,0.02] | [−0.17, −0.02] | [−0.03, 0.09] | [−0.30, 0.01] | [−0.35, −0.08] | |||
| IO × Trust in government | 0.02 * | 0.05 ** | ||||||
| [0.00, 0.04] | [0.01, 0.08] | |||||||
| IO × Trust in healthcare professionals | −0.00 | −0.02 | ||||||
| [−0.02, 0.02] | [−0.15, 0.01] | |||||||
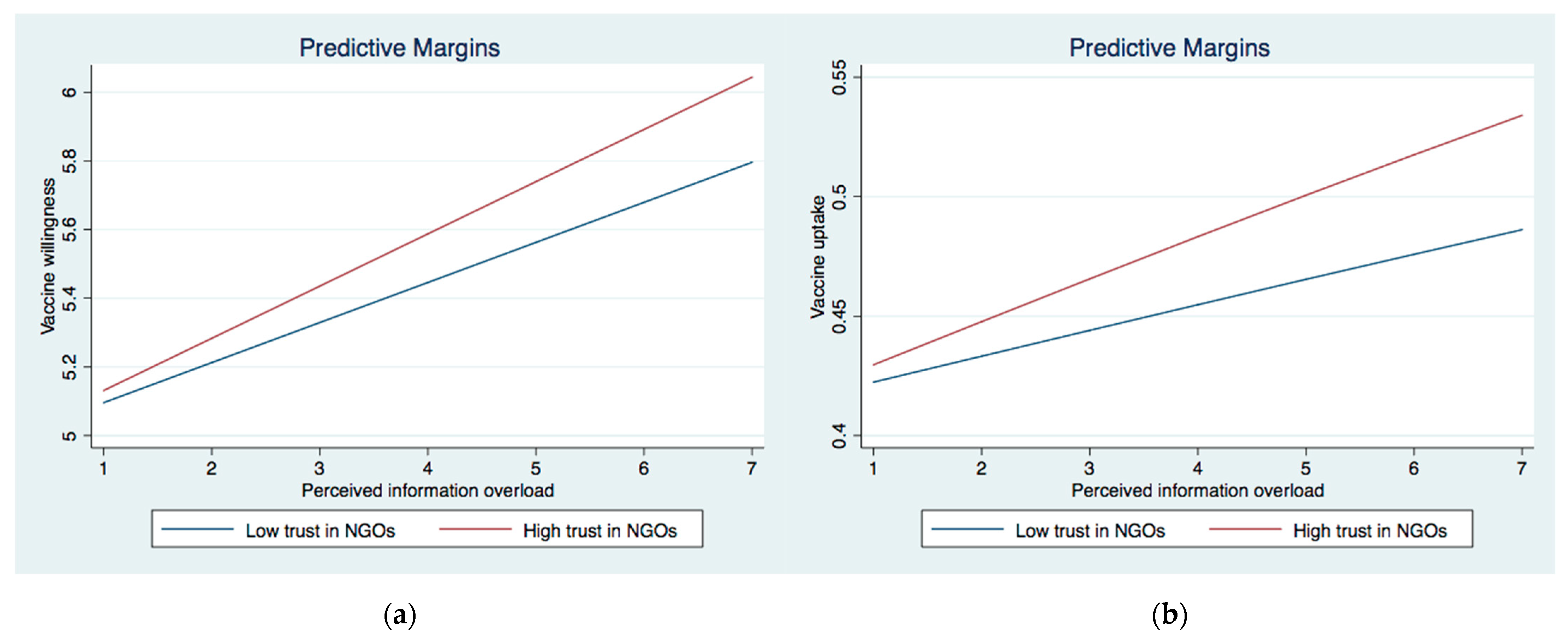
| IO × Trust in NGOs | 0.03 * | 0.05 * | ||||||
| [0.01, 0.05] | [0.01, 0.08] | |||||||
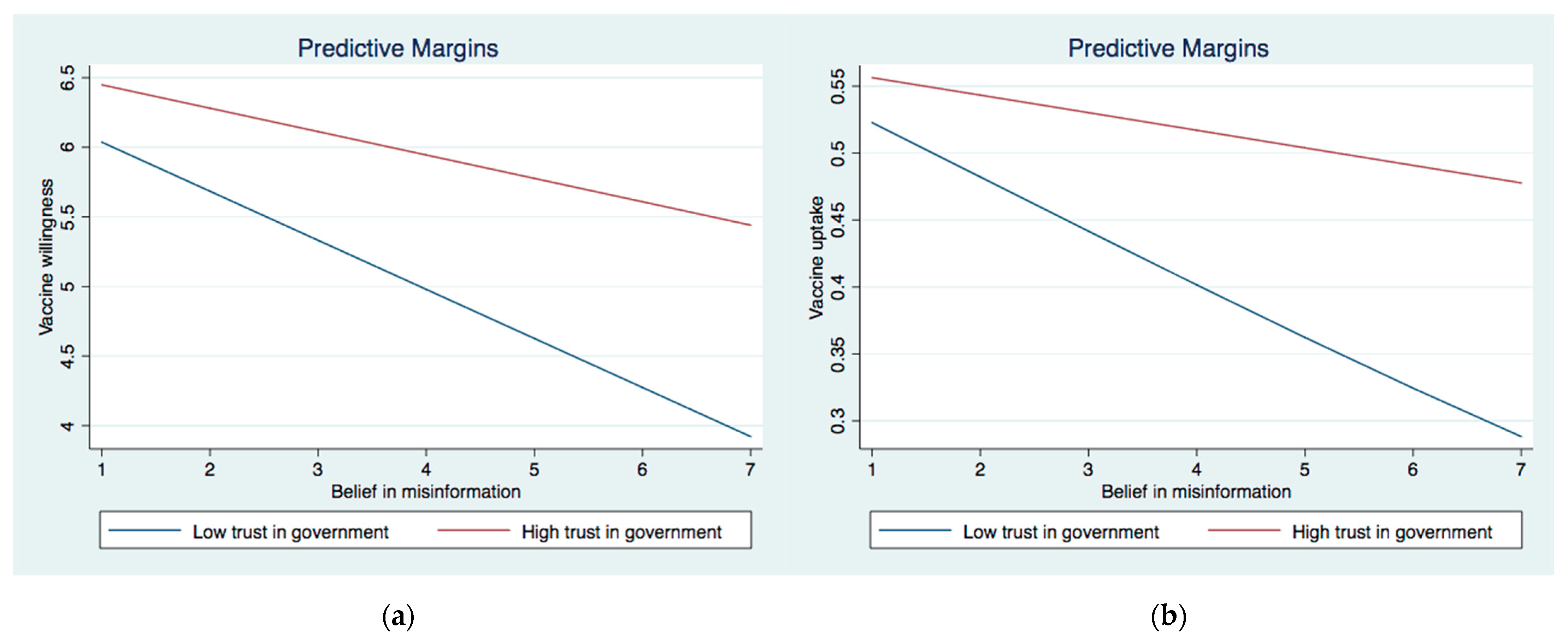
| MI × Trust in government | 0.06 *** | 0.05 ** | ||||||
| [0.04, 0.07] | [0.02, 0.08] | |||||||
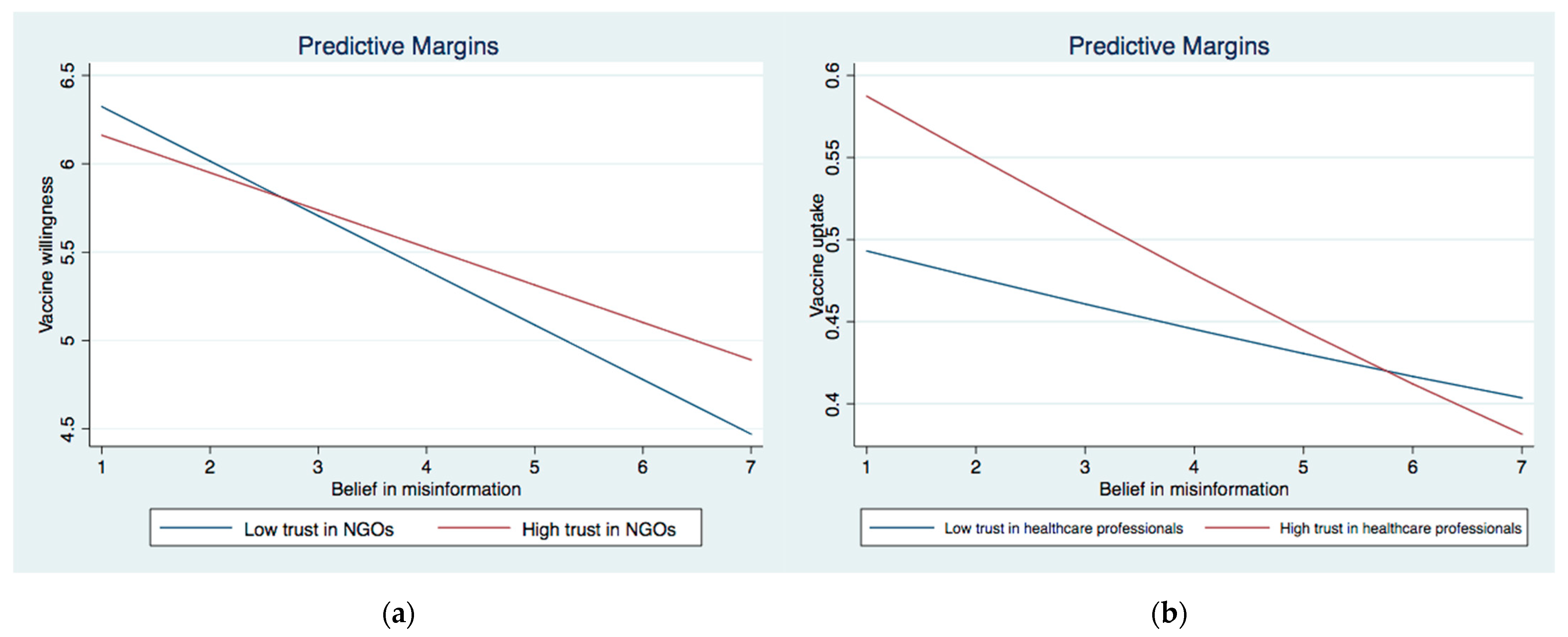
| MI × Trust in healthcare professionals | −0.01 | −0.05 * | ||||||
| [−0.03, 0.01] | [−0.09, −0.01] | |||||||
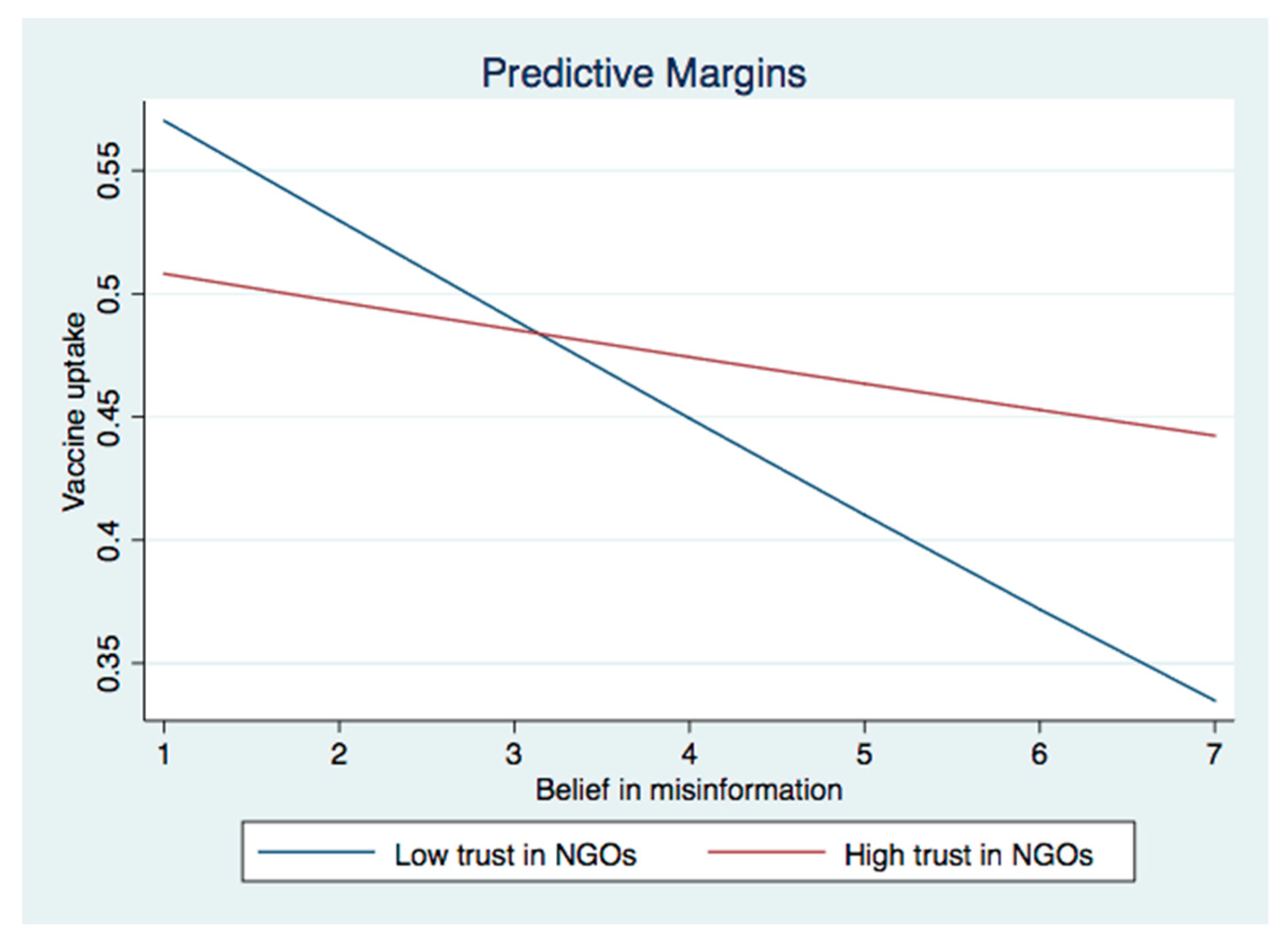
| MI × Trust in NGOs | 0.04 *** | 0.07 *** | ||||||
| [0.02, 0.05] | [0.04, 0.10] | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, X.; Lee, W.; Lin, F. Infodemic, Institutional Trust, and COVID-19 Vaccine Hesitancy: A Cross-National Survey. Int. J. Environ. Res. Public Health 2022, 19, 8033. https://doi.org/10.3390/ijerph19138033
Chen X, Lee W, Lin F. Infodemic, Institutional Trust, and COVID-19 Vaccine Hesitancy: A Cross-National Survey. International Journal of Environmental Research and Public Health. 2022; 19(13):8033. https://doi.org/10.3390/ijerph19138033
Chicago/Turabian StyleChen, Xi, Woohyung Lee, and Fen Lin. 2022. "Infodemic, Institutional Trust, and COVID-19 Vaccine Hesitancy: A Cross-National Survey" International Journal of Environmental Research and Public Health 19, no. 13: 8033. https://doi.org/10.3390/ijerph19138033
APA StyleChen, X., Lee, W., & Lin, F. (2022). Infodemic, Institutional Trust, and COVID-19 Vaccine Hesitancy: A Cross-National Survey. International Journal of Environmental Research and Public Health, 19(13), 8033. https://doi.org/10.3390/ijerph19138033






