Occupational Health and Safety Receptivity towards Clinical Innovations That Can Benefit Workplace Mental Health Programs: Anxiety and Hypnotherapy Trends
Abstract
1. Introduction
1.1. Anxiety Is a Normal Everyday Condition: Diagnosis Not Required
1.2. Anxiety in the Workplace: It Comes to Work and Can Be Exacerbated at Work
1.3. Productivity Impact
1.4. Occupational Health and Safety (OHS) Responsibility
1.5. Leaders in the Field
1.6. Hypnotherapy—What It Is, and Isn’t
1.7. Hypnotherapy Inclusion in OHS Services
2. Research Aims
- Hypnotherapy is considered an effective cognitive behavioural therapy (CBT) to deal with anxiety in clinical practice,
- has a place in workplace OHS programs to manage anxiety; and
- what barriers towards receptivity may need to be overcome by OHS before being considered a workplace service?
3. Methods and Results
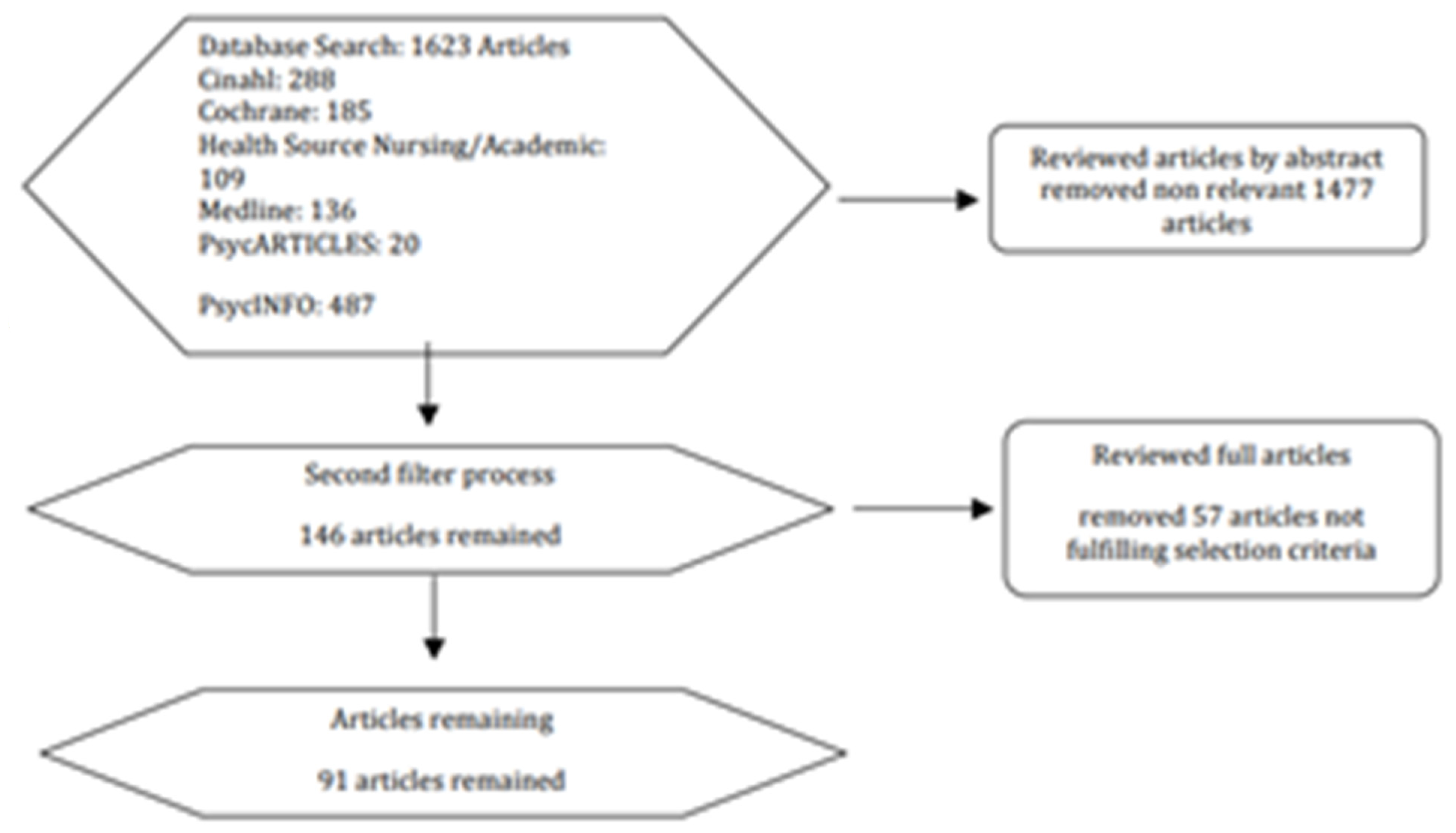
3.1. Literature Review
- Meta-analysis of randomised controlled trials
- Randomised controlled trials
- Controlled studies without randomisation
- Descriptive studies such as comparative studies, correlation-based studies, or case control studies, expert committee reports or opinions, clinical experience, or respected authority, or both.
Literature Review Findings around Clinical Trends
3.2. Quantitative Survey
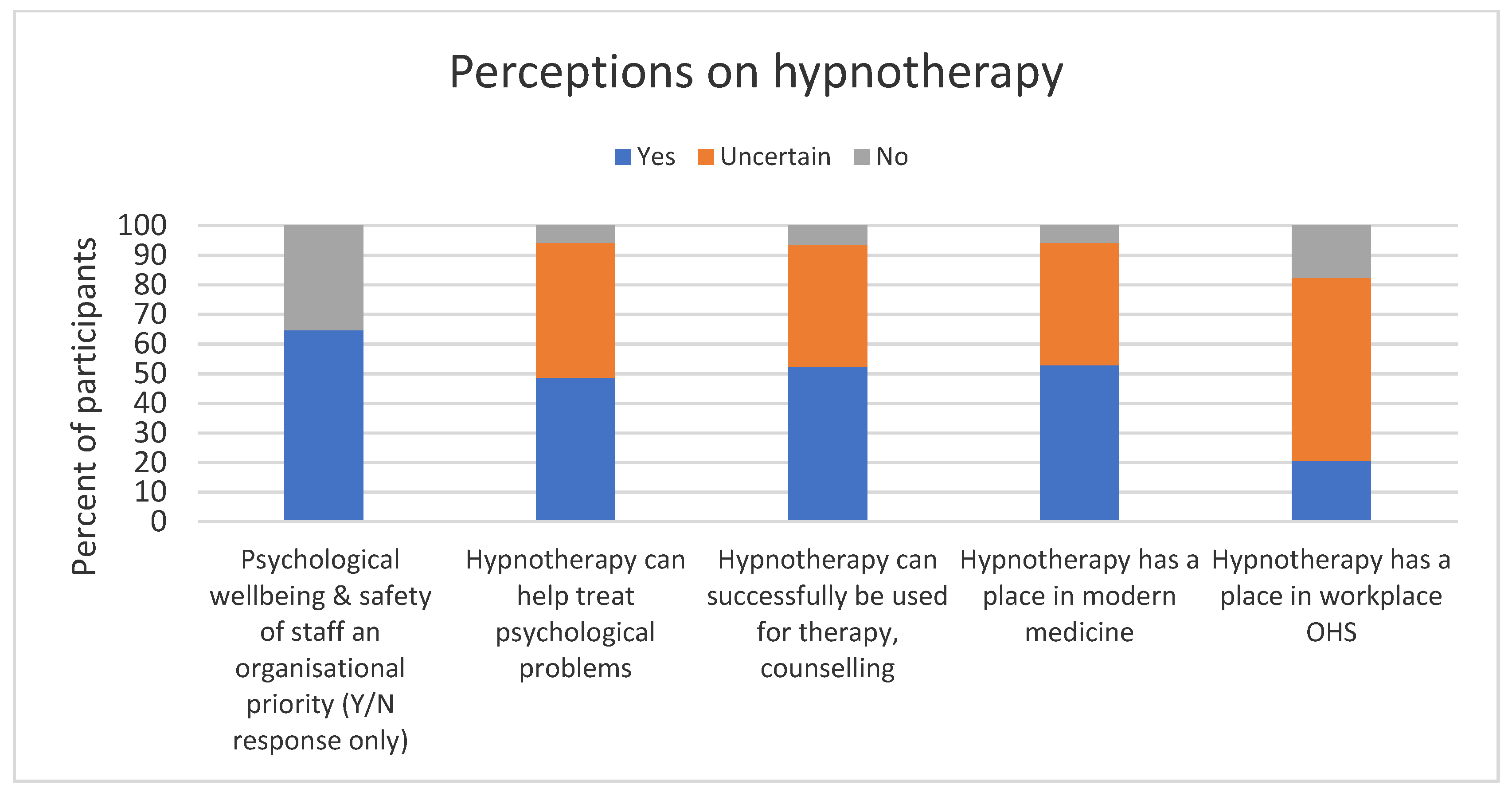
OHS Perceptions Regarding Hypnotherapy for Anxiety Management
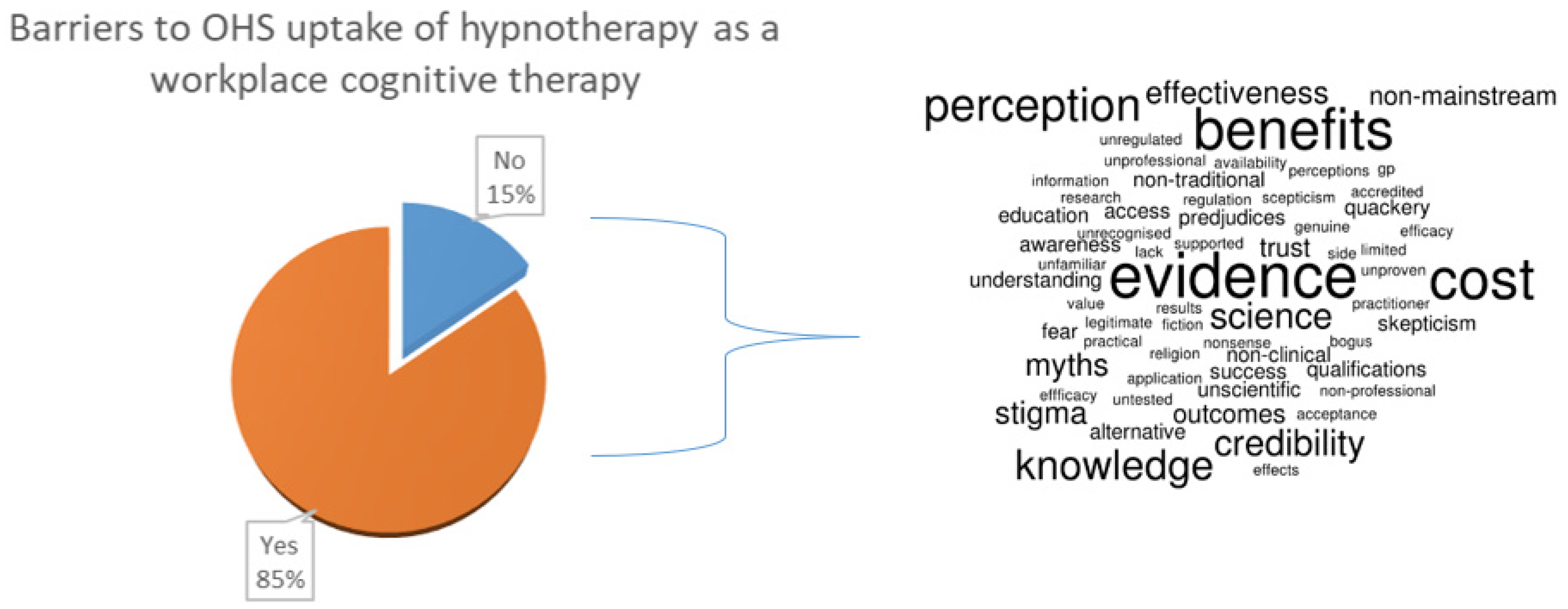
3.3. Barriers to Adoption of Hypnotherapy
4. Qualitative Focus Groups
4.1. Triangulation of the Data
“Senior staff are less likely to recognise a day needed for mental well-being over a day off for personal care. It is like they don’t understand the relationship my anxiety has with my output”.
“I think a lot of people just consider anxiety to be on the same level as stress. Stress is more temporary, and I would like others to know more about anxiety and accepted its place in our life”.
“COVID-19 really changed how I viewed anxiety. I guess I always thought of it as something weak people had or something that people needed to just get over. My workplace really hasn’t embraced how it impacted our daily lives and how to alleviate some of the issues”.
“I wouldn’t dare tell the people around me at work anything about my personal life. You don’t know who will share what story with who and what will end up happening”.
4.2. Other Considerations
“Is a hypnotherapist truly qualified? I am not sure how they are certified, and I really don’t know much about how they would actually provide a solution for staff with anxiety”.
“Perhaps if someone had provided me with an understanding of hypnosis and how it all worked, I might have had included it in my toolbag”.
4.3. Opportunities
4.4. Limitations
5. Discussion
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- WHO. Mental health atlas. Bull. World Health Organ. 2015, 93, 516. [Google Scholar]
- Robertson, D.J. The practice of cognitive-behavioural hypnotherapy. In A Manual for Evidence-Based Clinical Hypnosis; Karnac Books: London, UK, 2013. [Google Scholar]
- Negrón-Oyarzo, I.; Pérez, M.Á.; Terreros, G.; Muñoz, P.; Dagnino-Subiabre, A. Effects of chronic stress in adolescence on learned fear, anxiety, and synaptic transmission in the rat prelimbic cortex. Behav. Brain Res. 2014, 259, 342. [Google Scholar] [CrossRef]
- Rolls, E.T. Limbic systems for emotion and for memory, but no single limbic system. Cortex 2015, 62, 119–157. [Google Scholar] [CrossRef]
- Lopes, L.; Campos, P.F. SCAH!RF: A Novel Wearable as a Subconscious Approach for Mitigating Anxiety Symptoms; Springer: Berlin/Heidelberg, Germany, 2019; pp. 664–667. [Google Scholar]
- Salario, A. The Fear & Anxiety Solution: A Breakthrough Process for Healing and Empowerment with Your Subconscious Mind. Spirituality & Health Magazine, 1 November 2012; 90. [Google Scholar]
- Bertrams, A.; Englert, C.; Dickhäuser, O.; Baumeister, R.F. Role of self-control strength in the relation between anxiety and cognitive performance. Emotion 2013, 13, 668–680. [Google Scholar] [CrossRef]
- Eysenck, M.W.; Calvo, M.G. Anxiety and performance: The processing efficiency theory. Cogn. Emot. 1992, 6, 409–434. [Google Scholar] [CrossRef]
- Philippi, C.L.; Koenigs, M. The neuropsychology of self-reflection in psychiatric illness. J. Psychiatr. Res. 2014, 54, 55–63. [Google Scholar] [CrossRef]
- Beijer, S.E. HR Practices at Work: Their Conceptualization and Measurement in HRM Research; Gildeprint: Enschede, The Netherlands, 2014. [Google Scholar]
- Wilson, M. From processing efficiency to attentional control: A mechanistic account of the anxiety–performance relationship. Int. Rev. Sport Exerc. Psychol. 2008, 1, 184–201. [Google Scholar] [CrossRef]
- Boxall, P.; Guthrie, J.P.; Paauwe, J. Editorial introduction: Progressing our understanding of the mediating variables linking HRM, employee well-being and organisational performance. Hum. Resour. Manag. J. 2016, 26, 103–111. [Google Scholar] [CrossRef]
- Levett, K.M.; Coughlan, S.; Longridge, S.; Roumeliotis, V.; Adams, J. Be well: A systems-based wellness intervention using mindfulness in the workplace—A case study. J. Manag. Organ. 2019, 25, 613–634. [Google Scholar] [CrossRef]
- Giorgi, G. Findings in the area of anxiety disorders reported from Baylor University (Effect of hypnosis on anxiety: Results from a randomized controlled trial with women in postmenopause). Health Med. Week 2021, 2698. [Google Scholar]
- Giorgi, G.; Lecca, L.I.; Alessio, F.; Finstad, G.L.; Bondanini, G.; Lulli, L.G.; Arcangeli, G.; Mucci, N. COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 7857. [Google Scholar] [CrossRef]
- Alladin, A. Integrative CBT for Anxiety Disorders: An Evidence-Based Approach to Enhancing Cognitive Behavioral Therapy with Mindfulness and Hypnotherapy; Wiley Blackwell: Chichester, UK, 2016. [Google Scholar]
- Beard, C. Cognitive bias modification for anxiety: Current evidence and future directions. Exp. Rev. Neurotherap. 2011, 11, 299–311. [Google Scholar] [CrossRef]
- Harder, H.G.; Wagner, S.; Rash, J.A. Mental Illness in the Workplace: Psychological Disability Management; Gower Publishing: Farnham, UK, 2014. [Google Scholar]
- Marciniak, M.; Lage, M.J.; Landbloom, R.P.; Dunayevich, E.; Bowman, L. Medical and productivity costs of anxiety disorders: Case control study. Depress. Anxiety 2004, 19, 112–120. [Google Scholar] [CrossRef]
- ADAA. Anxiety Disorders: Anxiety Disorders Association of America survey finds Americans report stress, anxiety. Ment. Health Bus. Week 2006, 9. [Google Scholar]
- Riba, M.B.; Parikh, S.V.; Greden, J.F. Mental Health in the Workplace Strategies and Tools to Optimize Outcomes; Springer International Publishing: Cham, Switzerland, 2019. [Google Scholar]
- Geisler, M.; Berthelsen, H.; Muhonen, T. Retaining social workers: The role of quality of work and psychosocial safety climate for work engagement, job satisfaction, and organizational commitment. Hum. Serv. Organ. Manag. Leadersh. Gov. 2019, 43, 1–15. [Google Scholar] [CrossRef]
- Goss, J.R. Health Expenditure Data, Analysis and Policy Relevance in Australia, 1967 to 2020. Int. J. Environ. Res. Public Health 2022, 19, 2143. [Google Scholar] [CrossRef]
- Gallagher, C.; Underhill, E.; Rimmer, M. Occupational safety and health management systems in Australia: Barriers to success. Policy Pract. Health Saf. 2003, 1, 67–81. [Google Scholar] [CrossRef][Green Version]
- Spence, G.B. Workplace wellbeing programs: If you build it they may NOT come… because it’s not what they really need! Int. J. Wellbeing 2015, 5, 109–124. [Google Scholar] [CrossRef]
- Baicker, K.; Cutler, D.; Song, Z. Workplace wellness programs can generate savings. Health Aff. (Proj. Hope) 2010, 29, 304. [Google Scholar] [CrossRef]
- Goldenhar, L.M.; Schulte, P.A. Intervention research in occupational health and safety. J. Occup. Med. 1994, 36, 763. [Google Scholar]
- Okpaku, S.O. Innovations in Global Mental Health; Springer International Publishing: Cham, Switzerland, 2020. [Google Scholar]
- Bryant, R.A.; Moulds, M.L.; Nixon, R.D.; Mastrodomenico, J.; Felmingham, K.; Hopwood, S. Hypnotherapy and cognitive behaviour therapy of acute stress disorder: A 3-year follow-up. Behav. Res. Ther. 2006, 44, 1331–1335. [Google Scholar] [CrossRef] [PubMed]
- Fuhr, K.; Meisner, C.; Broch, A.; Cyrny, B.; Hinkel, J.; Jaberg, J.; Petrasch, M.; Schweizer, C.; Stiegler, A.; Zeep, C.; et al. Efficacy of hypnotherapy compared to cognitive behavioral therapy for mild to moderate depression—Results of a randomized controlled rater-blind clinical trial. J. Aff. Disord. 2021, 286, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Alladin, A. Cognitive hypnotherapy for accessing and healing emotional injuries for anxiety disorders. Am. J. Clin. Hypn. 2016, 59, 24–46. [Google Scholar] [CrossRef] [PubMed]
- Alladin, A. The wounded self: New approach to understanding and treating anxiety disorders. Am. J. Clin. Hypn. 2014, 56, 368–388. [Google Scholar] [CrossRef]
- Fisch, S.; Brinkhaus, B.; Teut, M. Hypnosis in patients with perceived stress—A systematic review. BMC Comp. Alt. Med. 2017, 17, 323. [Google Scholar] [CrossRef]
- Golden, W.L. Cognitive hypnotherapy for anxiety disorders. Am. J. Clin. Hypn. 2012, 54, 263–274. [Google Scholar] [CrossRef]
- Hartman, D.; Zimberoff, D. Hypnotic trance in Heart-Centered therapies. J. Heart Center. Ther. 2003, 6, 105. [Google Scholar]
- Papadakis, D. Exploring the subconscious with hypnosis to alleviate insomnia. Aust. J. Clin. Hypnother. Hypn. 2013, 35, 4–19. [Google Scholar]
- Halligan, P.W.; Oakley, D.A. Hypnosis and cognitive neuroscience: Bridging the gap. Cortex 2013, 49, 359–364. [Google Scholar] [CrossRef]
- Oakley, D.A.; Halligan, P.W. Hypnotic suggestion and cognitive neuroscience. Trends Cogn. Sci. 2009, 13, 264–270. [Google Scholar] [CrossRef]
- Jensen, M.P.; Jamieson, G.A.; Lutz, A.; Mazzoni, G.; McGeown, W.J.; Santarcangelo, E.L.; Demertzi, A.; De Pascalis, V.; Banyai, E.I.; Rominger, C.; et al. New directions in hypnosis research: Strategies for advancing the cognitive and clinical neuroscience of hypnosis. Neurosci. Conscious. 2017, 2017, nix004. [Google Scholar] [CrossRef] [PubMed]
- Erpelding, N.; Borsook, D. Capturing brain metrics of neuropathic pain using nuclear magnetic resonance (Report). Pain Manag. 2013, 3, 395. [Google Scholar] [CrossRef] [PubMed]
- Yapko, M.D. Hypnosis with Children and Adolescents, 5th ed.; Routledge: London, UK, 1984; pp. 487–509. [Google Scholar]
- Dhanani, N.M.; Caruso, J.J.; Carinci, A.J. Complementary and alternative medicine for pain: An evidence-based review. Curr. Pain Headache Rep. 2010, 15, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Lynn, S.J.; Malakataris, A.; Condon, L.; Maxwell, R.; Cleere, C. Post-traumatic Stress Disorder: Cognitive hypnotherapy, mindfulness, and acceptance-based treatment approaches. Am. J. Clin. Hypn. 2012, 54, 311–330. [Google Scholar] [CrossRef] [PubMed]
- Faucher, J.; Koszycki, D.; Bradwejn, J.; Merali, Z.; Bielajew, C. Effects of CBT versus MBSR treatment on social stress reactions in social anxiety disorder. Mindfulness 2016, 7, 514–526. [Google Scholar] [CrossRef]
- Fan, D.; Zhu, C.J.; Timming, A.R.; Su, Y.; Huang, X.; Lu, Y. Using the past to map out the future of occupational health and safety research: Where do we go from here? Int. J. Hum. Res. Manag. 2020, 31, 90–127. [Google Scholar] [CrossRef]
- Dollard, M.F.; Bakker, A.B. Psychosocial safety climate as a precursor to conducive work environments, psychological health problems, and employee engagement. J. Occup. Organ. Psychol. 2010, 83, 579–599. [Google Scholar] [CrossRef]
- Woock, C. Earnings losses of injured men: Reported and unreported injuries. Ind. Relat. J. Econ. Soc. 2009, 48, 610–628. [Google Scholar] [CrossRef]
- Schatzberg, A.F.; Nemeroff, C.B. The American Psychiatric Association Publishing Textbook of Psychopharmacology, 15th ed.; Textbook of Psychopharmacology; American Psychiatric Association Publishing: Washington, DC, USA, 2017. [Google Scholar]
- Morley, S.; Eccleston, C.; Williams, A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain 1999, 80, 1–13. [Google Scholar] [CrossRef]
- Brooker, E. Music performance anxiety: A clinical outcome study into the effects of cognitive hypnotherapy and eye movement desensitisation and reprocessing in advanced pianists. Psychol. Music 2018, 46, 107–124. [Google Scholar] [CrossRef]
- Mohaghegh Toosi, F.; Sharbaf, H.A.; Fathi, M.; Kareshki, H. The effectiveness of cognitive developmental hypnotherapy on differentiation of self, meaning in life and marital conflicts in married women. Am. J. Clin. Hypn. 2022, 64, 248–262. [Google Scholar] [CrossRef] [PubMed]
- Adachi, T.; Fujino, H.; Nakae, A.; Mashimo, T.; Sasaki1, J. A meta-analysis of hypnosis for chronic pain problems: A comparison between hypnosis, standard care, and other psychological interventions. Int. J. Clin. Exp. Hypn. 2014, 62, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Hammond, D.C. Hypnosis in the treatment of anxiety- and stress-related disorders. Expert Rev. Neurother. 2010, 10, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Valentine, K.E.; Milling, L.S.; Clark, L.J.; Moriarty, C.L. The efficacy of hypnosis as a treatment for anxiety: A meta-analysis. Int. J. Clin. Exp. Hypn. 2019, 67, 336–363. [Google Scholar] [CrossRef]
- McConkey, K.M.; Jupp, J.J. Opinions about the forensic use of hypnosis. Aust. Psychol. 1985, 20, 83–291. [Google Scholar] [CrossRef]
- Yu, C. Fostering positive attitudes towards hypnosis through a measure of mental imagery ability. Aust. J. Clin. Exp. Hypn. 2007, 35, 134–149. [Google Scholar]
- Coe, W.C.; Ryken, K. Hypnosis and risks to human subjects. Am. Psychol. 1979, 34, 673–681. [Google Scholar] [CrossRef]
- Cowen, L. Eeny Meeny Miny Moe: Who Can Practice I Don’t Know? Aust. J. Clin. Hypnother. Hypnosis 2016, 38, 26–39. [Google Scholar]
- De Lucchi, D.A.; Barling, N. Knowledge, attitudes, and beliefs about clinical hypnosis. Aust. J. Clin. Exp. Hypn. 2004, 32, 36–52. [Google Scholar]
- Raz, A.; Shapiro, T. Hypnosis and Neuroscience: A Cross Talk between Clinical and Cognitive Research. Arch. Gen. Psychiatry 2002, 59, 85–90. [Google Scholar] [CrossRef]
- Terhune, D.B.; Cleeremans, A.; Raz, A.; Lynn, S.J. Hypnosis and top-down regulation of consciousness. Neurosci. Biobehav. Rev. 2017, 81 Pt A, 59–74. [Google Scholar] [CrossRef]
- Terhune, D.B.; Polito, V.; Barnier, A.J.; Woody, E.Z. Variations in the Sense of Agency during Hypnotic Responding: Insights from Latent Profile Analysis. Psychol. Conscious. 2016, 3, 293–302. [Google Scholar] [CrossRef]
- Theorell, T. Handbook of Socioeconomic Determinants of Occupational Health From Macro-Level to Micro-Level Evidence, 1st ed.; Handbook Series in Occupational Health Sciences; Springer International Publishing: Cham, Switzerland, 2020. [Google Scholar]
- Winter, A. The rise and fall of forensic hypnosis. Stud. Hist. Philos. Biol. Biomed. Sci. 2013, 44, 26. [Google Scholar] [CrossRef] [PubMed]
- Birnbaum, H.G.; Kessler, R.C.; Kelley, D.; Ben-Hamadi, R.; Joish, V.N.; Greenberg, P.E. Employer burden of mild, moderate, and severe major depressive disorder: Mental health services utilization and costs, and work performance. Depress. Anxiety 2010, 27, 78–89. [Google Scholar] [CrossRef] [PubMed]
| Survey n (%) | Focus Group n | |
|---|---|---|
| N | 136 | 12 |
| Female: male | 60:76 (44.1:55.9) | 11:1 |
| Age group (years) | ||
| - 18–29 | 2 (1.5) | 1 |
| - 30–39 | 23 (16.9) | 6 |
| - 40–49 | 29 (21.3) | 4 |
| - 50–59 | 52 (38.2) | 1 |
| - 60+ | 30 (22.1) | 0 |
| Role in organisation | ||
| - Executive, administrator, or senior manager | 17 (12.5) | 1 |
| - Line manager with OHS responsibility | 11 (8.1) | 5 |
| - Qualified OHS provider | 108 (79.4) | 6 |
| Number of employees | ||
| - Less than 10 | 18 (13.2) | 3 |
| - 10–99 | 17 (12.5) | 8 |
| - Over 100 | 101 (74.3) | 1 |
| Time in organisation (years) | ||
| - Less than 5 | 75 (55.2) | 1 |
| - 5–10 | 26 (19.1) | 8 |
| - 10+ | 35 (25.7) | 3 |
| Place in the Workplace OHS p Value | Barriers to OHS Uptake p Value | |
|---|---|---|
| Sex (F:M) | 0.069 | 0.200 |
| Age group | 0.013 | 0.605 |
| Role in organisation | 0.301 | 0.327 |
| Number of employees | 0.142 | 0.066 |
| Time in organisation | 0.551 | 0.135 |
| Place in modern medicine | 0.001 | 0.469 |
| Myths | 0.321 | 0.069 |
| Place in workplace OHS | 0.207 | |
| Barriers to uptake | 0.207 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coventry, P. Occupational Health and Safety Receptivity towards Clinical Innovations That Can Benefit Workplace Mental Health Programs: Anxiety and Hypnotherapy Trends. Int. J. Environ. Res. Public Health 2022, 19, 7735. https://doi.org/10.3390/ijerph19137735
Coventry P. Occupational Health and Safety Receptivity towards Clinical Innovations That Can Benefit Workplace Mental Health Programs: Anxiety and Hypnotherapy Trends. International Journal of Environmental Research and Public Health. 2022; 19(13):7735. https://doi.org/10.3390/ijerph19137735
Chicago/Turabian StyleCoventry, Petrina. 2022. "Occupational Health and Safety Receptivity towards Clinical Innovations That Can Benefit Workplace Mental Health Programs: Anxiety and Hypnotherapy Trends" International Journal of Environmental Research and Public Health 19, no. 13: 7735. https://doi.org/10.3390/ijerph19137735
APA StyleCoventry, P. (2022). Occupational Health and Safety Receptivity towards Clinical Innovations That Can Benefit Workplace Mental Health Programs: Anxiety and Hypnotherapy Trends. International Journal of Environmental Research and Public Health, 19(13), 7735. https://doi.org/10.3390/ijerph19137735





