Improving Access to Cancer Treatment Services in Australia’s Northern Territory—History and Progress
Abstract
1. Introduction
2. Methods
3. Results
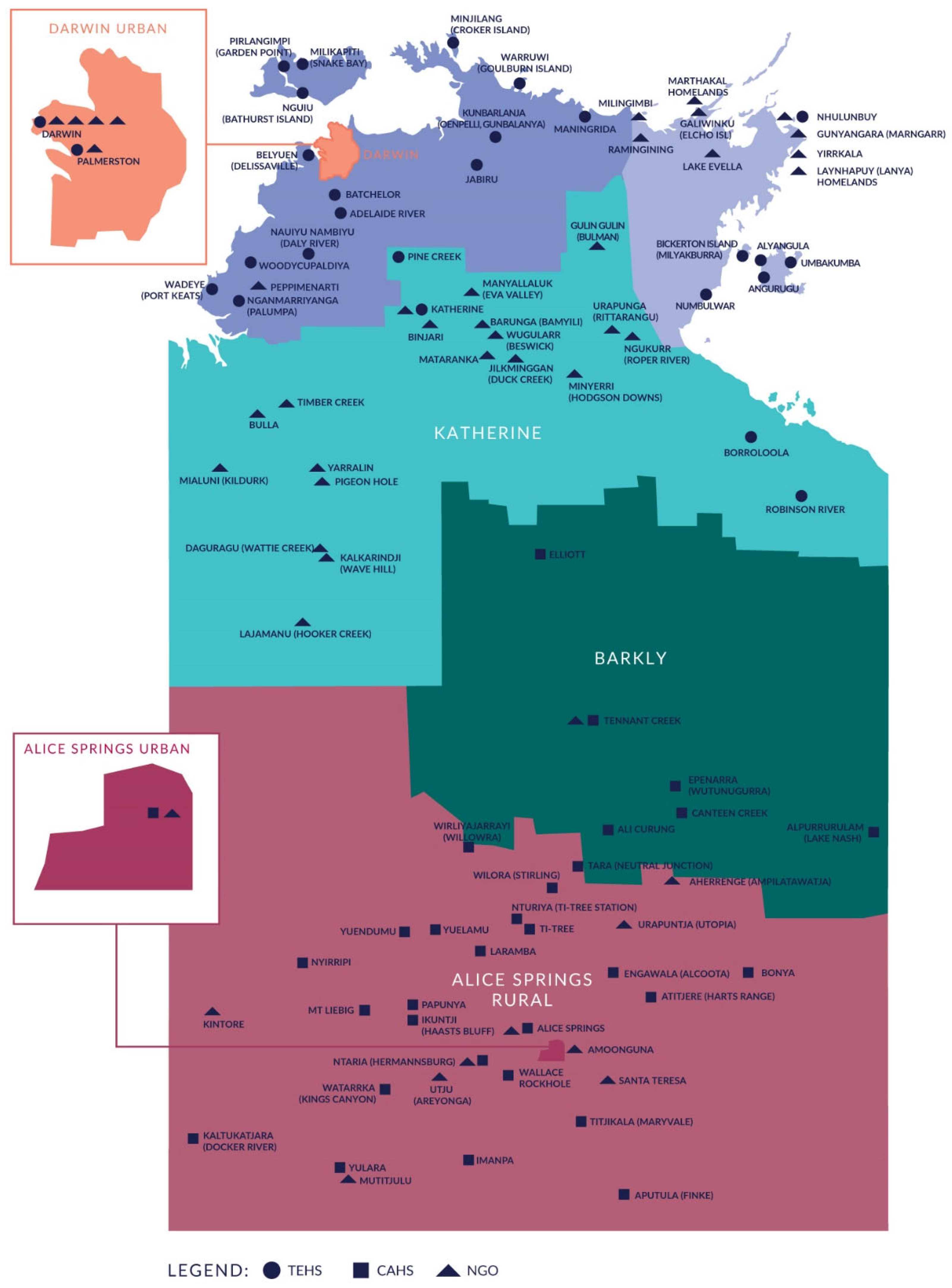
3.1. Description of Overall Service Delivery
3.2. Top End Cancer Services
3.3. Central Australian Health Service
3.4. Workforce
3.5. Screening
3.6. Telehealth
3.7. Assisting Patients with Travel and Accommodation
3.8. Palliative Care
4. Discussion
4.1. Limitations
4.2. Implications
- Improve travel assistance and support, including review of the 200 km eligibility limit for the PATS.
- Increase the availability of appropriate accommodation for patients travelling for cancer treatment, including in Alice Springs and Katherine.
- Develop additional strategies to recruit and retain the cancer workforce and remote workforce:
- Non-Indigenous health workforce: training to work in a remote setting, additional management and clinical support, professional development opportunities and community programs to help health professionals build social connections.
- Indigenous health workforce: providing additional opportunities for career progression and professional development, strategies to address heavy workloads and burnout, support for balancing work and community responsibilities, provide additional clinical and cultural mentoring and build supportive and culturally safe workplaces.
- Develop further localised strategies to increase participation in screening programs—including increased education for remote health professionals. Localised screening programs should be collaboratively designed with the community to make them acceptable to Indigenous people and people in remote areas.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kou, K.; Dasgupta, P.; Cramb, S.M.; Yu, X.Q.; Baade, P.D. Temporal trends in population-level cure of cancer: The Australian context. Cancer Epidemiol. Biomark. Prev. 2020, 29, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Rutherford, M.J.; Bardot, A.; Ferlay, J.; Andersson, T.M.L.; Myklebust, T.Å.; Tervonen, H.; Thursfield, V.; Ransom, D.; Shack, L.; et al. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995–2014 (ICBP SURVMARK-2): A population-based study. Lancet Oncol. 2019, 20, 1493–1505. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA A Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Williams, S.; Siahpush, M.; Mulhollen, A. Socioeconomic, Rural-Urban, and Racial Inequalities in US Cancer Mortality: Part I—All Cancers and Lung Cancer and Part II—Colorectal, Prostate, Breast, and Cervical Cancers. J. Cancer Epidemiol. 2011, 2011, 107497. [Google Scholar] [CrossRef] [PubMed]
- Afshar, N.; English, D.R.; Milne, R.L. Rural–urban residence and cancer survival in high-income countries: A systematic review. Cancer 2019, 125, 2172–2184. [Google Scholar] [CrossRef] [PubMed]
- Gurney, J.; Stanley, J.; McLeod, M.; Koea, J.; Jackson, C.; Sarfati, D. Disparities in Cancer-Specific Survival Between Māori and Non-Māori New Zealanders, 2007–2016. JCO Glob. Oncol. 2020, 6, 766–774. [Google Scholar] [CrossRef]
- Withrow, D.R.; Pole, J.D.; Nishri, E.D.; Tjepkema, M.; Marrett, L.D. Cancer Survival Disparities Between First Nation and Non-Aboriginal Adults in Canada: Follow-up of the 1991 Census Mortality Cohort. Cancer Epidemiol. Biomark. Prev. 2017, 26, 145–151. [Google Scholar] [CrossRef]
- Condon, J.R.; Zhang, X.; Baade, P.; Griffiths, K.; Cunningham, J.; Roder, D.M.; Coory, M.; Jelfs, P.L.; Threlfall, T. Cancer survival for Aboriginal and Torres Strait Islander Australians: A national study of survival rates and excess mortality. Popul. Health Metr. 2014, 12, 1. [Google Scholar] [CrossRef]
- Butler, J.; Foot, C.; Bomb, M.; Hiom, S.; Coleman, M.; Bryant, H.; Vedsted, P.; Hanson, J.; Richards, M. The International Cancer Benchmarking Partnership: An international collaboration to inform cancer policy in Australia, Canada, Denmark, Norway, Sweden and the United Kingdom. Health Policy 2013, 112, 148–155. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Cancer in Australia 2019. Available online: https://www.aihw.gov.au/reports/cancer/cancer-in-australia-2019/summary (accessed on 2 September 2021).
- Fox, P.; Boyce, A. Cancer health inequality persists in regional and remote Australia. Med. J. Aust. 2014, 201, 445–446. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Estimates of Aboriginal and Torres Strait Islander Australians. 2016. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/mf/3238.0.55.001 (accessed on 2 September 2021).
- Department of the Prime Minister and Cabinet. Closing the Gap Prime Minister’s Report 2020. Available online: https://ctgreport.niaa.gov.au/content/closing-gap-2020 (accessed on 2 September 2021).
- Australian Institute of Health and Welfare. Aboriginal and Torres Strait Islander Health Performance Framework 2020 Summary Report. Available online: https://www.indigenoushpf.gov.au/ (accessed on 2 September 2021).
- Australian Institute of Health and Welfare. Rural & Remote Health. Available online: https://www.aihw.gov.au/reports/rural-remote-australians/rural-remote-health/contents/profile-of-rural-and-remote-australians (accessed on 9 December 2021).
- Gruen, R.L.; Weeramanthri, T.S.; Bailie, R.S. Outreach and improved access to specialist services for Indigenous people in remote Australia: The requirements for sustainability. J. Epidemiol. Community Health 2002, 56, 517–521. [Google Scholar] [CrossRef] [PubMed]
- McBain-Rigg, K.E.; Veitch, C. Cultural barriers to health care for Aboriginal and Torres Strait Islanders in Mount Isa. Aust. J. Rural. Health 2011, 19, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Diaz, A.; Whop, L.J.; Valery, P.C.; Moore, S.P.; Cunningham, J.; Garvey, G.; Condon, J.R. Cancer outcomes for Aboriginal and Torres Strait Islander Australians in rural and remote areas. Aust. J. Rural. Health 2015, 23, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.; Dwyer, J.; Willis, E.; Pekarsky, B. Travelling to the city for hospital care: Access factors in country Aboriginal patient journeys. Aust. J. Rural. Health 2014, 22, 109–113. [Google Scholar] [CrossRef]
- Banham, D.; Roder, D.; Keefe, D.; Farshid, G.; Eckert, M.; Cargo, M.; Brown, A. Disparities in cancer stage at diagnosis and survival of Aboriginal and non-Aboriginal South Australians. Cancer Epidemiol. 2017, 48, 131–139. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Aboriginal and Torres Strait Islander Health Performance Framework: 1.08 Cancer. Available online: https://www.indigenoushpf.gov.au/measures/1-08-cancer#.YTBO9nBDMu0.mailto (accessed on 2 September 2021).
- Migiro, G. The World’s Largest Country Subdivisions. Available online: https://www.worldatlas.com/articles/the-world-s-largest-country-subdivisions.html (accessed on 2 September 2021).
- Northern Territory Government. Northern Territory Population Growth Strategy 2018–2028. Available online: https://population.nt.gov.au/__data/assets/pdf_file/0007/559384/Population-Strategy.pdf (accessed on 16 September 2021).
- Australian Bureau of Statistics. Regional Population Growth, Australia, 2017–2018. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Previousproducts/3218.0Main%20Features602017-18?opendocument&tabname=Summary&prodno=3218.0&issue=2017-18&num=&view= (accessed on 2 September 2021).
- Northern Territory Department of Health. Annual Report 2019–2020. Available online: https://health.nt.gov.au/__data/assets/pdf_file/0005/948632/NT-Department-of-Health-Annual-Report-2019-20.PDF (accessed on 2 September 2021).
- Australian Bureau of Statistics. Census of Population and Housing—Counts of Aboriginal and Torres Strait Islander Australians. Available online: https://www.abs.gov.au/statistics/people/aboriginal-and-torres-strait-islander-peoples/census-population-and-housing-counts-aboriginal-and-torres-strait-islander-australians/latest-release (accessed on 2 September 2021).
- Australian Bureau of Statistics. 2016 Census QuickStats: Northern Territory. Available online: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/7?opendocument (accessed on 18 January 2022).
- De Vincentiis, B.; Guthridge, S.; Spargo, J.; Su, J.-Y.; Nandakumara, S. Story of Our Children and Young People. Available online: https://cmc.nt.gov.au/__data/assets/pdf_file/0006/760254/story-of-our-children-and-young-people.pdf (accessed on 9 September 2021).
- Australian Bureau of Statistics. 2016 Census Reveals the Changing Face of the Northern Territory. Available online: https://www.abs.gov.au/Ausstats/abs@.nsf/dd0ca10eed681f12ca2570ce0082655d/c73d7cc81ca1fd2fca258148000a4067!OpenDocument (accessed on 2 September 2021).
- Zhang, X.; Dugdale, S.; Warton, L.; Li, S.Q. Cancer in the Northern Territory 1991–2015: Incidence and Mortality. Available online: https://health.nt.gov.au/__data/assets/pdf_file/0006/956211/Cancer-in-the-Northern-Territory-1991-2015-incidence-and-mortality.pdf (accessed on 14 September 2021).
- Hunter, J.; Smith, C.; Delaney, G.P.; Templeman, K.; Grant, S.; Ussher, J.M. Coverage of cancer services in Australia and providers’ views on service gaps: Findings from a national cross-sectional survey. BMC Cancer 2019, 19, 570. [Google Scholar] [CrossRef]
- Chondur, R.; Coffey, P.; Guthridge, S. Smoking Prevalence Northern Territory—1994 to 2013. Available online: https://digitallibrary.health.nt.gov.au/prodjspui/bitstream/10137/603/1/Smoking%20prevalence%20factsheet%2021May2014_FINAL.pdf (accessed on 14 September 2021).
- Australian Institute of Health and Welfare. Alcohol, Tobacco & Other Drugs in Australia. Available online: https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/about (accessed on 14 September 2021).
- Carruthers, S.; Pennefather, M.; Ward, L.; Giam, K.; Penniment, M. Measuring (and narrowing) the gap: The experience with attendance of Indigenous cancer patients for Radiation Therapy in the Northern Territory. J. Med. Imaging Radiat. Oncol. 2019, 63, 510–516. [Google Scholar] [CrossRef]
- Condon, J.R.; Zhang, X.; Dempsey, K.; Garling, L.; Guthridge, S. Trends in cancer incidence and survival for Indigenous and non-Indigenous people in the Northern Territory. Med. J. Aust. 2016, 205, 454–458. [Google Scholar] [CrossRef]
- Condon, J.R.; Warman, G.; Arnold, L. (Eds.) The Health and Welfare of Territorians; Territory Health Services: Casuarina, NT, Australia, 2001.
- Kettle, E.; The Australian National University, North Australia Research Unit. Health Services in the Northern Territory: A History 1824–1970; The Australian National University, North Australia Research Unit (NARU): Brinkin, NT, Australia, 1991. [Google Scholar]
- Northern Territory Government. Aerial Medical Services. Available online: https://nt.gov.au/wellbeing/hospitals-health-services/aerial-medical-services (accessed on 16 September 2021).
- Australian Bureau of Statistics. Population Projections, Northern Territory, 1999 to 2021; Australian Bureau of Statistics: Canberra, Australia, 1999.
- Australian Bureau of Statistics. National, State and Territory Population. Available online: https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/dec-2019 (accessed on 2 September 2021).
- Department of Health. Northern Territory Cancer Care Strategy 2018–2022. Available online: https://digitallibrary.health.nt.gov.au/prodjspui/bitstream/10137/7486/1/NT%20Health%20Cancer%20Care%20Strategy%202018-2022.pdf (accessed on 16 November 2021).
- Darwin Private Hospital. Patient Information Directory. Available online: https://darwinprivatehospital.com.au/application/files/5715/9347/6341/Darwin_Private_Hospital_2020_002-compressed.pdf#:~:text=The%20Darwin%20Private%20Hospital%20Infusion,other%20infusions%20as%20an%20outpatient (accessed on 16 November 2021).
- Osman, H. NT Receives Advanced Medical Imaging Tech. Available online: https://www.healthcareitnews.com/news/anz/nt-receives-advanced-medical-imaging-tech (accessed on 9 December 2021).
- Australian Bureau of Statistics. 2016 Census QuickStats: Katherine. Available online: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/UCL714001 (accessed on 18 January 2022).
- Keane, L. Local cancer patients praise latest addition to Katherine Hospital. Katherine Times, 18 November 2015. [Google Scholar]
- Frenk, J.; Chen, L.; Bhutta, Z.A.; Cohen, J.; Crisp, N.; Evans, T.; Fineberg, H.; Garcia, P.; Ke, Y.; Kelley, P.; et al. Health professionals for a new century: Transforming education to strengthen health systems in an interdependent world. Lancet 2010, 376, 1923–1958. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Health Workforce. Available online: https://www.aihw.gov.au/reports/australias-health/health-workforce (accessed on 15 December 2021).
- Australian Bureau of Statistics. Australian Social Trends, April 2013. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/lookup/4102.0main+features20april+2013 (accessed on 21 December 2021).
- Northern Territory PHN. Northern Territory PHN Primary Health Care Workforce Needs Assessment: Year 2: Allied Primary Health Workforce. Available online: https://www.ntphn.org.au/wp-content/uploads/2021/06/HWNA_Allied-Health-Final-22012020.pdf (accessed on 21 December 2021).
- Northern Territory PHN. Northern Territory Primary Health Care Workforce Needs Assessment: Year 1: Remote Primary Health Care and General Practitioners. Available online: https://www.ntphn.org.au/wp-content/uploads/2021/06/NT-PHN-HWNA-2018.pdf (accessed on 21 December 2021).
- Wakerman, J.; Humphreys, J.; Russell, D.; Guthridge, S.; Bourke, L.; Dunbar, T.; Zhao, Y.; Ramjan, M.; Murakami-Gold, L.; Jones, M.P. Remote health workforce turnover and retention: What are the policy and practice priorities? Hum. Resour. Health 2019, 17, 99. [Google Scholar] [CrossRef]
- Zhao, Y.; Russell, D.J.; Guthridge, S.; Ramjan, M.; Jones, M.P.; Humphreys, J.S.; Carey, T.A.; Wakerman, J. Long-term trends in supply and sustainability of the health workforce in remote Aboriginal communities in the Northern Territory of Australia. BMC Health Serv. Res. 2017, 17, 836. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. National Health Workforce Data Sets. Available online: https://hwd.health.gov.au/ (accessed on 5 April 2022).
- Northern Territory PHN. Regional Health Profiles. Available online: https://www.ntphn.org.au/about/publications/regional-profiles/ (accessed on 5 April 2022).
- Department of Health. The Aboriginal and Torres Strait Islander Allied Health Workforce. Available online: https://hwd.health.gov.au/resources/publications/factsheet-alld-atsi-allied-health-2019.pdf (accessed on 5 April 2022).
- Zhang, X.; Condon, J. Cancer Screening in the Northern Territory 2019. Available online: https://digitallibrary.health.nt.gov.au/prodjspui/bitstream/10137/7938/1/Cancer%20screening%20in%20the%20Northern%20Territory%202019.pdf (accessed on 18 November 2021).
- Department of Health. NT Health Virtual Care Strategy. Available online: https://digitallibrary.health.nt.gov.au/prodjspui/bitstream/10137/11840/2/NTHealthVirtualCareStrategy.pdf (accessed on 23 November 2021).
- Department of Health. Technical Appendix—Data Development—The Northern Territory (NT). Available online: https://www1.health.gov.au/internet/publications/publishing.nsf/Content/oatsih-hpf-2012-toc~tech-app~data~nt (accessed on 23 November 2021).
- Dods, S.; Freyne, J.; Alem, L.; Nepal, S.; Li, J.; Jang-Jaccard, J. Caring for the Last 3%: Telehealth Potential and Broadband Implications for Remote Australia. Available online: https://publications.csiro.au/rpr/download?pid=csiro:EP129516&dsid=DS3 (accessed on 30 November 2021).
- Department of Health. Evaluation of the PATS-Telehealth Project. Available online: http://www.amsant.org.au/wp-content/uploads/2016/03/PATS-Telehealth-Report-FINAL.pdf (accessed on 23 November 2021).
- Olver, I.N.; Selva-Nayagam, S. Evaluation of a telemedicine link between Darwin and Adelaide to facilitate cancer management. Telemed. J. 2000, 6, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Northern Territory PHN. NT PHN Program Needs Assessment 2019. Available online: https://www.ntphn.org.au/wp-content/uploads/2021/06/2019-NEEDS-ASSESSMENT-FINAL-UNLINKED.pdf (accessed on 21 December 2021).
- Bonney, A.; Knight-Billington, P.; Mullan, J.; Moscova, M.; Barnett, S.; Iverson, D.; Saffioti, D.; Eastland, E.; Guppy, M.; Weston, K.; et al. The telehealth skills, training, and implementation project: An evaluation protocol. JMIR Res. Protoc. 2015, 4, e2. [Google Scholar] [CrossRef] [PubMed]
- Shahid, S.; Teng, T.K.; Bessarab, D.; Aoun, S.; Baxi, S.; Thompson, S.C. Factors contributing to delayed diagnosis of cancer among Aboriginal people in Australia: A qualitative study. BMJ Open 2016, 6, e010909. [Google Scholar] [CrossRef]
- Northern Territory Health. Patient Assistance Travel Scheme. Available online: https://nt.gov.au/wellbeing/health-subsidies-support-and-home-visits/patient-assistance-travel-scheme (accessed on 9 December 2021).
- NT Radiation Oncology. Barbara James House. Available online: http://ntro.com.au/barbara-james-hostel/ (accessed on 9 December 2021).
- Northern Territory Department of Health. Northern Territory Cancer Plan 2013–2016. Available online: https://digitallibrary.health.nt.gov.au/prodjspui/bitstream/10137/1152/1/Northern%20Territory%20Cancer%20Plan%202013%20-%202016.pdf (accessed on 9 December 2021).
- Waran, E.; Zubair, M.Y.; O’Connor, N. The gap reversed: A review of site of death in the Top End. MJA 2017, 207, 39. [Google Scholar] [CrossRef][Green Version]
- Royal Darwin Hospital Management Board. Royal Darwin Hospital Management Board Annual Report 2004/2005. Available online: https://hdl.handle.net/10137/7458 (accessed on 15 December 2021).
- PEPA Education. Territory Palliative Care—Top End Service Royal Darwin Hospital. Available online: https://pepaeducation.com/host-sites/territory-palliative-care-top-end-service-royal-darwin-hospital/ (accessed on 15 December 2021).
- Waran, E.; O’Connor, N.; Zubair, M.Y.; May, P. “Finishing up” on country: Challenges and compromises. Intern. Med. J. 2016, 46, 1108–1111. [Google Scholar] [CrossRef]
- McGrath, P. “I don’t want to be in that big city; this is my country here”: Research findings on Aboriginal peoples’ preference to die at home. Aust. N. Z. J. Public Health 2007, 15, 264–268. [Google Scholar] [CrossRef]
- Thompson, S.C.; Cheetham, S.; Baxi, S. The enablers, barriers and preferences of accessing radiation therapy facilities in the rural developed world—A systematic review. BMC Cancer 2017, 17, 794. [Google Scholar] [CrossRef]
- Ambroggi, M.; Biasini, C.; Del Giovane, C.; Fornari, F.; Cavanna, L. Distance as a Barrier to Cancer Diagnosis and Treatment: Review of the Literature. Oncologist 2015, 20, 1378–1385. [Google Scholar] [CrossRef]
- Thompson, S.C.; Shahid, S.; Bessarab, D.; Durey, A.; Davidson, P.M. Not just bricks and mortar: Planning hospital cancer services for Aboriginal people. BMC Res. Notes 2011, 4, 62. [Google Scholar] [CrossRef]
- Shahid, S.; Finn, L.D.; Thompson, S.C. Barriers to participation of Aboriginal people in cancer care: Communication in the hospital setting. Med. J. Aust. 2009, 190, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Marcusson-Rababi, B.; Anderson, K.; Whop, L.J.; Butler, T.; Whitson, N.; Garvey, G. Does gynaecological cancer care meet the needs of Indigenous Australian women? Qualitative interviews with patients and care providers. BMC Health Serv. Res. 2019, 19, 606. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.; Diaz, A.; Parikh, D.R.; Garvey, G. Accessibility of cancer treatment services for Indigenous Australians in the Northern Territory: Perspectives of patients and care providers. BMC Health Serv. Res. 2021, 21, 95. [Google Scholar] [CrossRef] [PubMed]
- Vass, A.; Mitchell, A.; Dhurrkay, Y. Health literacy and Australian Indigenous peoples: An analysis of the role of language and worldview. Health Promot. J. Aust. 2011, 22, 33–37. [Google Scholar] [CrossRef]
- Shahid, S.; Thompson, S.C. An overview of cancer and beliefs about the disease in Indigenous people of Australia, Canada, New Zealand and the US. Aust. N. Z. J. Public Health 2009, 33, 109–118. [Google Scholar] [CrossRef]
- McGrath, P.; Phillips, E. Western Notions of Informed Consent and Indigenous Cultures: Australian Findings at the Interface. J. Bioethical Inq. 2008, 5, 21–31. [Google Scholar] [CrossRef]
- Green, M.; Anderson, K.; Griffiths, K.; Garvey, G.; Cunningham, J. Understanding Indigenous Australians’ experiences of cancer care: Stakeholders’ views on what to measure and how to measure it. BMC Health Serv. Res. 2018, 18, 982. [Google Scholar] [CrossRef]
- Taylor, E.V.; Haigh, M.M.; Shahid, S.; Garvey, G.; Cunningham, J.; Thompson, S.C. Cancer services and their initiatives to improve the care of Indigenous Australians. Int. J. Environ. Res. Public Health 2018, 15, 717. [Google Scholar] [CrossRef]
- Taylor, E.V.; Lyford, M.; Holloway, M.; Parsons, L.; Mason, T.; Sabesan, S.; Thompson, S.C. “The support has been brilliant”: Experiences of Aboriginal and Torres Strait Islander patients attending two high performing cancer services. BMC Health Serv. Res. 2021, 21, 493. [Google Scholar] [CrossRef]
- Zhao, Y.; Russell, D.J.; Guthridge, S.; Ramjan, M.; Jones, M.P.; Humphreys, J.S.; Wakerman, J. Costs and effects of higher turnover of nurses and Aboriginal health practitioners and higher use of short-term nurses in remote Australian primary care services: An observational cohort study. BMJ Open 2019, 9, e023906. [Google Scholar] [CrossRef]
- Russell, D.J.; Zhao, Y.; Guthridge, S.; Ramjan, M.; Jones, M.P.; Humphreys, J.S.; Wakerman, J. Patterns of resident health workforce turnover and retention in remote communities of the Northern Territory of Australia, 2013–2015. Hum. Resour. Health 2017, 15, 52. [Google Scholar] [CrossRef] [PubMed]
- Cosgrave, C. The Whole-of-Person Retention Improvement Framework: A Guide for Addressing Health Workforce Challenges in the Rural Context. Int. J. Environ. Res. Public Health 2020, 17, 2698. [Google Scholar] [CrossRef]
- Lai, G.C.; Taylor, E.V.; Haigh, M.M.; Thompson, S.C. Factors Affecting the Retention of Indigenous Australians in the Health Workforce: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 914. [Google Scholar] [CrossRef] [PubMed]
- Zucca, A.; Boyes, A.; Newling, G.; Hall, A.; Girgis, A. Travelling all over the countryside: Travel-related burden and financial difficulties reported by cancer patients in New South Wales and Victoria. Aust. J. Rural. Health 2011, 19, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Gordon, L.G.; Ferguson, M.; Chambers, S.K.; Dunn, J. Fuel, Beds, Meals and Meds: Out-of-Pocket Expenses for Patients with Cancer in Rural Queensland. Cancer Forum 2009, 33, 204–210. [Google Scholar]
- Shahid, S.; Finn, L.; Bessarab, D.; Thompson, S.C. ‘Nowhere to room … nobody told them’: Logistical and cultural impediments to Aboriginal peoples’ participation in cancer treatment. Aust. Health Rev. 2011, 35, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Queensland Health. Patient Travel Subsidy Scheme Health Service Directive. Available online: https://www.health.qld.gov.au/__data/assets/pdf_file/0033/848706/qh-hsdgdl-050-2.pdf (accessed on 9 December 2021).
- WA Country Health Service. Am I Eligible for PATS? Available online: https://www.wacountry.health.wa.gov.au/Our-patients/Patient-Assisted-Travel-Scheme-PATS/Am-I-eligible-for-PATS (accessed on 9 December 2021).
- Standing Committee on Community Affairs. Reforming Patient Assisted Travel Schemes. Available online: https://www.aph.gov.au/parliamentary_business/committees/senate/community_affairs/completed_inquiries/2004-07/pats/report/c07 (accessed on 9 December 2021).
- Thaker, D.; Monypenny, R.; Olver, I.; Sabesan, S. Cost savings from a telemedicine model of care in northern Queensland, Australia. Med. J. Aust. 2013, 199, 414–417. [Google Scholar] [CrossRef]
- NT Health. Telehealth. Available online: https://health.nt.gov.au/professionals/ehealth/telehealth (accessed on 18 January 2022).
- Roberts, S.; Spain, B.; Hicks, C.; London, J.; Tay, S. Telemedicine in the Northern Territory: An assessment of patient perceptions in the preoperative anaesthetic clinic. Aust. J. Rural. Health 2015, 23, 136–141. [Google Scholar] [CrossRef]
- Sabesan, S.; Kelly, J.; Evans, R.; Larkins, S. A tele-oncology model replacing face-to-face specialist cancer care: Perspectives of patients in North Queensland. J. Telemed. Telecare 2014, 20, 207–211. [Google Scholar] [CrossRef]
- Caffery, L.J.; Bradford, N.K.; Wickramasinghe, S.I.; Hayman, N.; Smith, A.C. Outcomes of using telehealth for the provision of healthcare to Aboriginal and Torres Strait Islander people: A systematic review. Aust. N. Z. J. Public Health 2017, 41, 48–53. [Google Scholar] [CrossRef]
- Mooi, J.; Whop, L.; Valery, P.C.; Sabesan, S.S. Teleoncology for Indigenous patients: The responses of patients and health workers. Aust. J. Rural. Health 2012, 20, 5. [Google Scholar] [CrossRef] [PubMed]
- Christou, A.; Katzenellenbogen, J.; Thompson, S.C. Australia’s National Bowel Cancer Screening Program: Does it work for Indigenous Australians? BMC Public Health 2010, 10, 373. [Google Scholar] [CrossRef] [PubMed]
- Christou, A.; Thompson, S.C. How Could the National Bowel Cancer Screening Program for Aboriginal People in Western Australia Be Improved? Western Australian Department of Health: Perth, Australia, 2010.
- Christou, A.; Thompson, S.C. Colorectal cancer screening knowledge, attitudes and behavioural intention among Indigenous Western Australians. BMC Public Health 2012, 12, 528. [Google Scholar] [CrossRef] [PubMed]
- Christou, A.; Thompson, S.C. Missed opportunities in educating Aboriginal Australians about bowel cancer screening: Whose job is it anyway? Contemp. Nurse 2013, 46, 59–69. [Google Scholar] [CrossRef]
- Department of Health. National Bowel Cancer Screening Program: Primary Health Care Engagement Strategy 2016–2020. Available online: https://www.health.gov.au/resources/publications/national-bowel-cancer-screening-program-primary-health-care-engagement-strategy (accessed on 18 January 2022).
- Smith, M.; Hammond, I.; Saville, M. Lessons from the renewal of the National Cervical Screening Program in Australia. Public Health Res. Pract. 2019, 29, e292191420. [Google Scholar] [CrossRef]
- Lee, S.; Obamiro, K.; Cooper, A.; Barnett, T. General practitioner perspectives on barriers and enablers to bowel cancer screening in rural Tasmania: A thematic analysis of face-to-face interviews. Aust. J. Gen. Pract. 2021, 50, 158–163. [Google Scholar] [CrossRef]
- Department of Health and Aging; KPMG. Review of the National Bowel Cancer Screening Program (Phase 2): Final Report, Part One. Available online: https://www.health.gov.au/sites/default/files/documents/2020/01/review-of-the-national-bowel-cancer-screening-program-phase-2-review-of-the-national-bowel-cancer-screening-program-phase-2-final-report-part-one.pdf (accessed on 18 January 2022).
- Australian Institute of Health and Welfare. Aboriginal and Torres Strait Islander Health Performance Framework 2017 Report: Northern Territory. Available online: https://www.aihw.gov.au/reports/ihw/186/health-performance-framework-2017-nt/contents/table-of-contents (accessed on 9 December 2021).
- Hill, T.; Cass, B.; Newton, B.; Valentine, K. Indigenous carers. In Social Policy Research Paper No 45; Department of Social Services, Australian Government: Canberra, Australia, 2012. [Google Scholar]
- Australian Bureau of Statistics. Australian Aboriginal and Torres Strait Islander Health Survey: First Results, Australia, 2012–2013: Table 7 [Data Cube]; Australian Bureau of Statistics: Canberra, Australia, 2013.
- Australian Bureau of Statistics (Ed.) National Aboriginal and Torres Strait Islander Social Survey, 2014–2015: Table 14. Stressors, by Sex and Remoteness [Data Cube]; Australian Bureau of Statistics: Canberra, Australia, 2016.
- Cancer Australia. National Aboriginal and Torres Strait Islander Cancer Framework. 2015. Available online: https://canceraustralia.gov.au/publications-and-resources/cancer-australia-publications/national-aboriginal-and-torres-strait-islander-cancer-framework (accessed on 14 June 2022).
- Cancer Australia. Aboriginal and Torres Strait Islander Cancer Control Indicators. Available online: https://ncci.canceraustralia.gov.au/aboriginal-and-torres-strait-islander-cancer-control-indicators (accessed on 14 June 2022).
| Regional Government Health Services | Hospitals | Estimated Population | Hospital Beds | Surgery | Radiotherapy | Chemotherapy | Palliative Care | Allied Health | Pastoral Care |
|---|---|---|---|---|---|---|---|---|---|
| Top End Health Service (TEHS) | Royal Darwin Hospital | 139,000 | 360 | ✓ | ✓ +PET +Cyclotron | ✓ (16 chairs increasing to 20) | ✓ (12 bed) | ✓ | ✓ |
| Palmerston Regional Hospital | 37,000 | 116 | Limited | × | × | ✓ | ✓ | ✓ | |
| Katherine Hospital | 24,000 region (10,000 Katherine) | 60 | × | × | ✓ (4 chairs) | ✓ | ✓ | ✓ | |
| Gove Hospital | 16,000 region | 30 | × | × | × | × | ✓ | ✓ | |
| Darwin Private Hospital | 104 | ✓ | × | ✓ (4 chairs) | ✓ | ✓ | ✓ | ||
| Central Australian Health Service (CAHS) | Alice Springs Hospital | 25,000 Alice Springs | 181 | ✓ | × | ✓ (6 chairs) | ✓ (10 bed) | ✓ | ✓ |
| Tennant Creek Hospital | 8500 region (3500 Tennant Creek) | 20 | × | × | × | ✓ | ✓ | ✓ | |
| Profession | Darwin | Central Australia | Katherine Region | Northern Territory | Australia |
|---|---|---|---|---|---|
| Aboriginal Health Practitioners | 2.1 | 11.7 | 16.3 | 5.8 | 0.8 |
| Medical Practitioners | 92.8 | 69.7 | 29.3 | 48 | 205.3 |
| Nurses and Midwives | 277.3 | 260.9 | 115.8 | 149.6 | 674.5 |
| Oral Health Practitioners | 7.5 | 5.8 | 3.4 | 5.9 | 44.6 |
| Occupational Therapists | 11.9 | 8.4 | 1.9 | 6.5 | 33.3 |
| Optometrists | 1.6 | 1.5 | np | 1.3 | 10.6 |
| Pharmacists | 11.1 | 6.9 | 2.8 | 7.1 | 49.5 |
| Physiotherapists | 8.4 | 7.1 | 5.8 | 6.6 | 52.7 |
| Podiatrists | 1.4 | 2 | np | 1.1 | 9.7 |
| Psychologists | 7.2 | 8.4 | np | 6.3 | 53 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taylor, E.V.; Thackrah, R.D.; Thompson, S.C. Improving Access to Cancer Treatment Services in Australia’s Northern Territory—History and Progress. Int. J. Environ. Res. Public Health 2022, 19, 7705. https://doi.org/10.3390/ijerph19137705
Taylor EV, Thackrah RD, Thompson SC. Improving Access to Cancer Treatment Services in Australia’s Northern Territory—History and Progress. International Journal of Environmental Research and Public Health. 2022; 19(13):7705. https://doi.org/10.3390/ijerph19137705
Chicago/Turabian StyleTaylor, Emma V., Rosalie D. Thackrah, and Sandra C. Thompson. 2022. "Improving Access to Cancer Treatment Services in Australia’s Northern Territory—History and Progress" International Journal of Environmental Research and Public Health 19, no. 13: 7705. https://doi.org/10.3390/ijerph19137705
APA StyleTaylor, E. V., Thackrah, R. D., & Thompson, S. C. (2022). Improving Access to Cancer Treatment Services in Australia’s Northern Territory—History and Progress. International Journal of Environmental Research and Public Health, 19(13), 7705. https://doi.org/10.3390/ijerph19137705






