Determinants of Lack of Access to Treatment for Women Diagnosed with Breast Cancer in Brazil
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
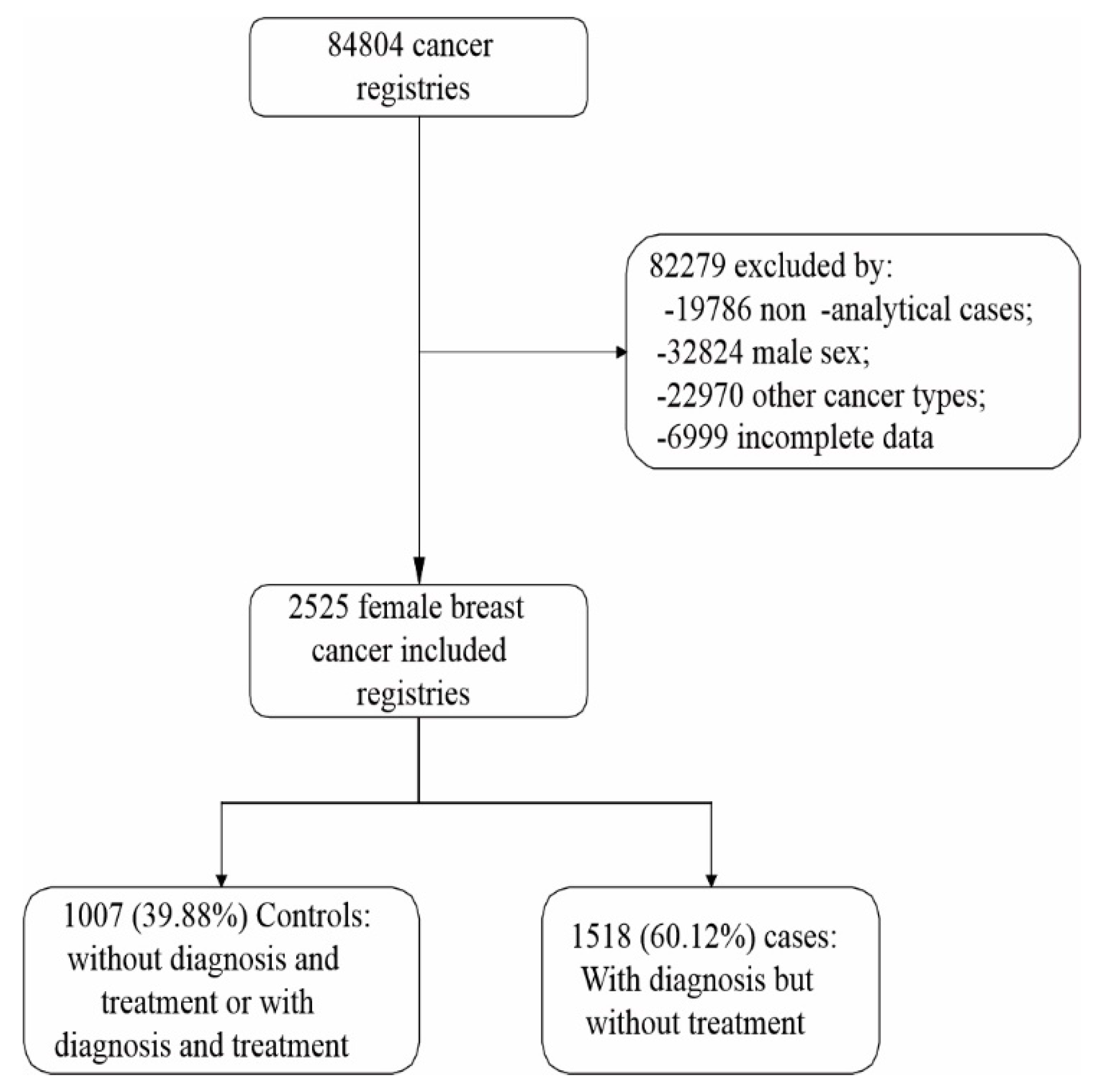
2.2. Participants
2.3. Data Source
2.4. Variables
2.5. Ethical Aspects
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Instituto Nacional de Câncer (INCA). Estimativa 2020: Incidência de Câncer No Brasil; Instituto Nacional de Câncer: Rio de Janeiro, Brazil, 2019; ISBN 978-85-7318-389-4.
- Paolucci, T.; Bernetti, A.; Bai, A.V.; Capobianco, S.V.; Bonifacino, A.; Maggi, G.; Ippolitoni, G.; Tinelli, L.; Santilli, V.; Agostini, F. The Recovery of Reaching Movement in Breast Cancer Survivors: Two Different Rehabilitative Protocols in Comparison. Eur. J. Phys. Rehabil. Med. 2020, 57, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Paolucci, T.; Bernetti, A.; Bai, A.V.; Segatori, L.; Monti, M.; Maggi, G.; Ippolitoni, G.; Tinelli, L.; Santilli, V.; Paoloni, M. The Sequelae of Mastectomy and Quadrantectomy with Respect to the Reaching Movement in Breast Cancer Survivors: Evidence for an Integrated Rehabilitation Protocol during Oncological Care. Support. Care Cancer 2021, 29, 899–908. [Google Scholar] [CrossRef] [PubMed]
- Ministério da Saúde (MS). Lei No 8080. Dispõe Sobre as Condições Para a Promoção, Proteção e Recuperação Da Saúde, a Organização e o Funcionamento Dos Serviços Correspondentes e Dá Outras Providências; Diário Oficial da União: Brasilia, Brazil, 1990.
- Ministério da Saúde (MS). Portaria No 1.220, de 3 de Junho de 2014. Dispõe Sobre a Aplicação Da Lei No 12.732, de 22 de Novembro de 2012, Que Versa a Respeito Do Primeiro Tratamento Do Paciente Com Neoplasia Maligna Comprovada, No Âmbito Do Sistema Único de Saúde (SUS); Diário Oficial da União: Brasilia, Brazil, 2014.
- Sousa, S.M.M.T.; Carvalho, M.D.G.F.D.M.; Santos, L.A.; Mariano, S.B.C. Acesso Ao Tratamento da Mulher Com Câncer de Mama. Saúde Debate 2019, 43, 727–741. [Google Scholar] [CrossRef]
- Ferreira, N.A.S.; Schoueri, J.H.M.; Sorpreso, I.C.E.; Adami, F.; Figueiredo, F.W.D.S. Waiting Time between Breast Cancer Diagnosis and Treatment in Brazilian Women: An Analysis of Cases from 1998 to 2012. Int. J. Environ. Res. Public Health 2020, 17, 4030. [Google Scholar] [CrossRef]
- Ferreira, N.A.S.; de Carvalho, S.M.F.; Valenti, V.E.; Bezerra, I.M.P.; Batista, H.M.T.; de Abreu, L.C.; Matos, L.L.; Adami, F. Treatment Delays among Women with Breast Cancer in a Low Socio-Economic Status Region in Brazil. BMC Women’s Health 2017, 17, 13. [Google Scholar]
- Inumaru, L.E.; Irineu Gomes Duarte Quintanilha, M.; Aparecida Da Silveira, É.; Veloso Naves, M.M. Risk and Protective Factors for Breast Cancer in Midwest of Brazil. J. Environ. Public Health 2012, 2012, 356851. [Google Scholar] [CrossRef]
- Dos-Santos-Silva, I. Políticas de Controle Do Câncer de Mama No Brasil: Quais São Os Próximos Passos? Cad. Saúde Pública 2018, 34, e00097018. [Google Scholar] [CrossRef]
- Ministério da Saúde (MS). Portaria No 741, de 19 de Dezembro de 2005. Define Unidades de Assistência de Alta Complexidade Em Oncologia, Centros de Assistência de Alta Complexidade Em Oncologia e Centros de Referência Em Alta Complexidade Em Oncologia; Diário Oficial da União: Brasilia, Brazil, 2005.
- Guerriero, I.C.Z. Resolução No 510 de 7 de Abril de 2016 Que Trata Das Especificidades Éticas Das Pesquisas Nas Ciências Humanas e Sociais e de Outras Que Utilizam Metodologias Próprias Dessas Áreas. Ciênc. Saúde Coletiva 2016, 21, 2619–2629. [Google Scholar] [CrossRef]
- de Oliveira, R.R.A.; Martins, A.A.G.; dos Santos Medeiros, W.A.; Souto Nóbrega, W.F.; dos Santos Andrade, L.S.; Gomes, K.A.L. Fatores Determinantes Para O Retardo No Diagnóstico e Tratamento Do Câncer de Mama: Revisão Integrativa. Rev. Interdiscip. Saúde 2021, 8, 209–225. [Google Scholar] [CrossRef]
- Renna Junior, N.L.; Silva, G.D.A. Diagnóstico de Câncer de Mama em Estado Avançado No Brasil: Análise de Dados Dos Registros Hospitalares de Câncer (2000–2012). Rev. Bras. Ginecol. Obstet. 2018, 40, 127–136. [Google Scholar]
- de Fátima Vasques Monteiro, M.; Barbosa, C.P.; Vertamatti, M.A.F.; Tavares, M.N.A.; de Oliveira Carvalho, A.C.; Alencar, A.P.A. Access to Public Health Services and Integral Care for Women during the Puerperal Gravid Period Period in Ceará, Brazil. BMC Health Serv. Res. 2019, 19, 851. [Google Scholar] [CrossRef]
- Costa, L.D.L.N.; de Lima Sardinha, A.H.; Verzaro, P.M.; Lisbôa, L.L.C.; Batista, R.F.L. Mortalidade Por Câncer de Mama e Condições de Desenvolvimento Humano No Brasil. Rev. Bras. Cancerol. 2019, 65, 1. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Soares, L.R.; Gonzaga, C.M.R.; Branquinho, L.W.; Sousa, A.-L.L.; Souza, M.R.; Freitas-Junior, R. Mortalidade Por Câncer de Mama Feminino No Brasil de Acordo Com a Cor. Rev. Bras. Ginecol. Obstet. 2015, 37, 388–392. [Google Scholar] [CrossRef][Green Version]
- de Medeiros, G.C.; Teodózio, C.G.C.; Fabro, E.A.N.; de Aguiar, S.S.; Lopes, A.H.M.; de Conte, B.C.; da Silva, E.V.; Coelho, L.L.P.; Muniz, N.F.; de Carvalho Schuab, S.I.P. Fatores Associados Ao Atraso Entre o Diagnóstico e o Início Do Tratamento de Câncer de Mama: Um Estudo de Coorte Com 204.130 Casos No Brasil. Rev. Bras. Cancerol. 2020, 66, 3. [Google Scholar] [CrossRef]
- Azevedo e Silva, G.; Bustamante-Teixeira, M.T.; Aquino, E.M.L.; Tomazelli, J.G.; dos-Santos-Silva, I. Acesso à Detecção Precoce Do Câncer de Mama No Sistema Único de Saúde: Uma Análise a Partir Dos Dados Do Sistema de Informações em Saúde. Cad. Saude Publica 2014, 30, 1537–1550. [Google Scholar] [CrossRef] [PubMed]
- Buranello, M.C.; Meirelles, M.C.C.C.; de Walsh, I.A.P.; Pereira, G.D.A.; de Castro, S.S. Breast Cancer Screening Practice and Associated Factors: Women’s Health Survey in Uberaba MG Brazil, 2014. Cienc. Saude Coletiva 2018, 23, 2661–2670. [Google Scholar] [CrossRef]
- de Paula Silva, R.; Gigante, D.P.; Amorim, M.H.C.; Leite, F.M.C. Fatores Associados à Realização de Mamografia Em Usuárias Da Atenção Primária à Saúde Em Vitória, Espírito Santo. Epidemiol. Serv. Saúde 2019, 28, e2018048. [Google Scholar]
- Schäfer, A.A.; Santos, L.P.; Miranda, V.I.A.; Tomasi, C.D.; Soratto, J.; Quadra, M.R.; Meller, F.O. Desigualdades Regionais e Sociais Na Realização de Mamografia e Exame Citopatológico Nas Capitais Brasileiras em 2019: Estudo Transversal. Epidemiol. Serv. Saúde 2021, 30, e2021172. [Google Scholar] [CrossRef]
- McLaughlin, J.M.; Anderson, R.T.; Ferketich, A.K.; Seiber, E.E.; Balkrishnan, R.; Paskett, E.D. Effect on Survival of Longer Intervals between Confirmed Diagnosis and Treatment Initiation among Low-Income Women with Breast Cancer. J. Clin. Oncol. 2012, 30, 4493. [Google Scholar] [CrossRef]
- Shin, D.W.; Cho, J.; Kim, S.Y.; Guallar, E.; Hwang, S.S.; Cho, B.; Oh, J.H.; Jung, K.W.; Seo, H.G.; Park, J.H. Delay to Curative Surgery Greater than 12 Weeks Is Associated with Increased Mortality in Patients with Colorectal and Breast Cancer but Not Lung or Thyroid Cancer. Ann. Surg. Oncol. 2013, 20, 2468–2476. [Google Scholar] [CrossRef] [PubMed]
- Finger, B.A.; Limberger, T. Acesso Ao Tratamento Oncológico No SUS: A Responsabilidade Civil Do Estado Pela Perda Da Chance de Cura Ou de Sobrevida das Pacientes Com Câncer de Mama No Rio Grande Do Sul. Rev. Direitos Garantias Fundam. 2019, 20, 155. [Google Scholar] [CrossRef]
- Cabral, A.L.L.V.; Giatti, L.; Casale, C.; Cherchiglia, M.L. Vulnerabilidade Social e Câncer de Mama: Diferenciais No Intervalo Entre o Diagnóstico e o Tratamento Em Mulheres de Diferentes Perfis Sociodemográficos. Cienc. Saude Coletiva 2019, 24, 613–622. [Google Scholar] [CrossRef]
- De Oliveira, E.X.G.; Pinheiro, R.S.; Melo, E.C.P.; Carvalho, M.S. Condicionantes Socioeconômicos e Geográficos Do Acesso à Mamografia No Brasil, 2003–2008. Cienc. Saude Colet. 2011, 16, 3649–3664. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total n (%) | Control 1007 (39.9%) | Cases 1.518 (60.1%) | p-Value 1 |
|---|---|---|---|---|
| Age Range (Years) | ||||
| 18–39 | 284 (11.25) | 89 (31.34) | 195 (68.66) | 0.001 |
| 40–49 | 558 (22.10) | 217 (38.89) | 341 (61.11) | |
| 50–69 | 1273 (50.42) | 511 (40.14) | 762 (59.86) | |
| 70+ | 410 (16.24) | 190 (46.34) | 220 (53.66) | |
| Ethnicity | <0.001 | |||
| White | 1180 (46.73) | 544 (46.10) | 636 (53.90) | |
| No White | 1345 (53.27) | 463 (34.42) | 882 (65.58) | |
| Educational level | 0.003 | |||
| None | 148 (5.86) | 65 (43.92) | 83 (56.08) | |
| Elementary School | 1429 (56.59) | 598 (41.85) | 831 (58.15) | |
| High school | 649 (25.70) | 252 (38.83) | 397 (61.17) | |
| Higher Education | 299 (11.84) | 92 (30.77) | 207 (69.23) | |
| Marital status | 0.660 | |||
| Single | 559 (22.14) | 214 (38.28) | 345 (61.72) | |
| Married | 1402 (55.52) | 568 (40.51) | 834 (59.49) | |
| Widow/Separate | 564 (22.34) | 225 (39.89) | 339 (60.11) | |
| Smoking | 0.564 | |||
| Never | 1646 (71.60) | 647 (39.31) | 999 (60.69) | |
| Former smoker | 379 (16.49) | 142 (37.47) | 237 (62.53) | |
| Current smoker | 274 (11.92) | 114 (41.61) | 160 (58.39) | |
| Alcohol consumption | 0.065 | |||
| Never | 1726 (77.16) | 671 (38.88) | 1055 (61.12) | |
| Former | 134 (5.99) | 42 (31.34) | 92 (68.66) | |
| Current | 377 (16.85) | 161 (42.71) | 216 (57.29) | |
| Region | <0.001 | |||
| Central-West | 83 (3.32) | 29 (34.94) | 54 (65.06) | |
| Northeast | 311 (12.43) | 104 (33.44) | 207 (66.56) | |
| South | 385 (15.38) | 223 (57.92) | 162 (42.08) | |
| Southeast | 1603 (64.04) | 612 (38.18) | 991 (61.82) | |
| North | 121 (4.83) | 28 (23.14) | 93 (76.86) | |
| Cancer family history | 0.270 | |||
| No | 871 (37.80) | 352 (40.41) | 519 (59.59) | |
| yes | 1433 (62.20) | 546 (38.10) | 887 (61.90) | |
| Health service reference | 0.234 | |||
| SUS | 2175 (86.14) | 855 (39.31) | 1320 (60.69) | |
| No SUS | 340 (13.47) | 149 (43.82) | 191 (56.18) | |
| Private | 10 (0.40) | 3 (30.00) | 7 (70.00) | |
| Diagnostic stage | 0.001 | |||
| I | 627 (24.83) | 285(45.45) | 342(54.55) | |
| II | 894 (35.41) | 367(41.05) | 527(58.95) | |
| III | 708 (28.04) | 252(35.59) | 456(64.41) | |
| IV | 296 (11.72) | 103(34.80) | 193(65.20) |
| Variable | Treatment Barrier OR (CI 95%) | p-Value 1 |
|---|---|---|
| Age Range (Years) | ||
| 18–39 | Ref | Ref |
| 40–49 | 0.90 (0.82; 1.003) | 0.059 |
| 50–69 | 0.93 (0.85; 1.02) | 0.124 |
| 70+ | 0.56 (0.76; 0.97) | 0.016 |
| Ethnicity | ||
| White | Ref | Ref |
| No White | 1.12 (1.04; 1.20) | 0.002 |
| Educational level | ||
| None | Ref | Ref |
| Elementary School | 1.09 (0.94; 1.26) | 0.254 |
| High School | 1.13 (0.97; 1.32) | 0.123 |
| Higher Education | 1.33 (1.13; 1.57) | 0.001 |
| Region | ||
| Central-West | Ref | Ref |
| Northeast | 1.07 (0.89; 1.27) | 0.467 |
| South | 0.73 (0.59; 0.89) | 0.002 |
| Southeast | 1.02 (0.86; 1.20) | 0.848 |
| North | 1.19 (0.99; 1.43) | 0.067 |
| Diagnostic stage | ||
| I | Ref | Ref |
| II | 1.07 (0.98; 1.17) | 0.119 |
| III | 1.12 (1.02; 1.23) | 0.013 |
| IV | 1.19 (1.07; 1.33) | 0.001 |
| Variable | OR (CI 95%) | p-Value 1 |
|---|---|---|
| Ethnicity | ||
| White | Ref | Ref |
| No White | 1.71 (1.44; 2.01) | <0.001 |
| Educational level | ||
| None | Ref | Ref |
| Elementary School | 1.23 (0.87; 1.74) | 0.238 |
| High School | 1.46 (1.01; 2.12) | 0.041 |
| Higher education | 2.36 (1.56; 3.60) | <0.001 |
| Diagnostic stage | ||
| I | Ref | Ref |
| II | 1.20 (0.98; 1.49) | 0.077 |
| III | 1.44 (1.15; 1.80) | 0.001 |
| IV | 1.58 (1.18; 2.11) | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alves, M.N.T.; Monteiro, M.d.F.V.; Alves, F.T.; dos Santos Figueiredo, F.W. Determinants of Lack of Access to Treatment for Women Diagnosed with Breast Cancer in Brazil. Int. J. Environ. Res. Public Health 2022, 19, 7635. https://doi.org/10.3390/ijerph19137635
Alves MNT, Monteiro MdFV, Alves FT, dos Santos Figueiredo FW. Determinants of Lack of Access to Treatment for Women Diagnosed with Breast Cancer in Brazil. International Journal of Environmental Research and Public Health. 2022; 19(13):7635. https://doi.org/10.3390/ijerph19137635
Chicago/Turabian StyleAlves, Maria Nizete Tavares, Maria de Fátima Vasques Monteiro, Fernanda Tavares Alves, and Francisco Winter dos Santos Figueiredo. 2022. "Determinants of Lack of Access to Treatment for Women Diagnosed with Breast Cancer in Brazil" International Journal of Environmental Research and Public Health 19, no. 13: 7635. https://doi.org/10.3390/ijerph19137635
APA StyleAlves, M. N. T., Monteiro, M. d. F. V., Alves, F. T., & dos Santos Figueiredo, F. W. (2022). Determinants of Lack of Access to Treatment for Women Diagnosed with Breast Cancer in Brazil. International Journal of Environmental Research and Public Health, 19(13), 7635. https://doi.org/10.3390/ijerph19137635






