Research-Driven Guidelines for Delivering Group Exercise Programs via Videoconferencing to Older Adults
Abstract
1. Introduction
Objectives
2. Methods
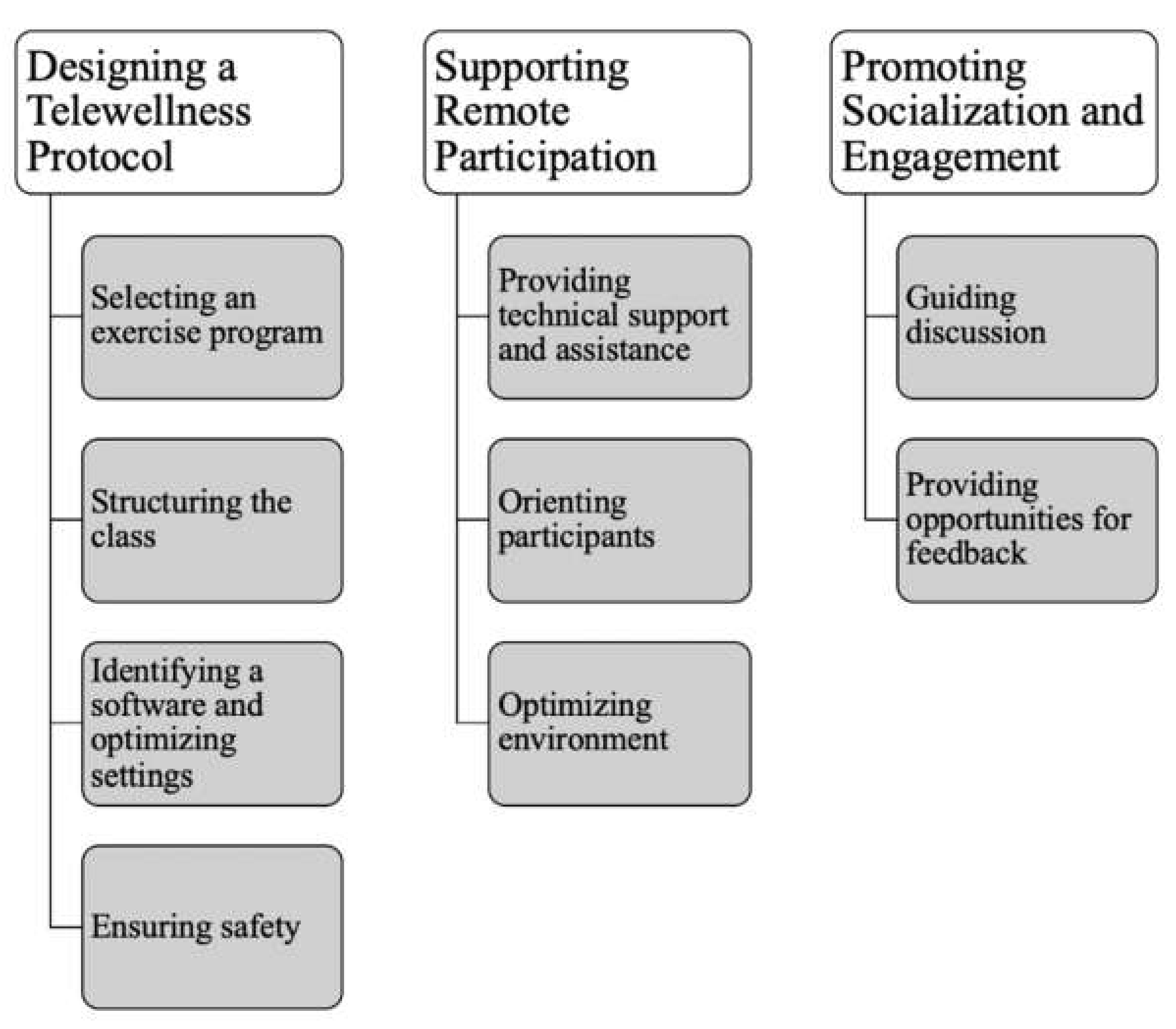
3. Results
3.1. Designing a Telewellness Program
3.1.1. Selecting an Exercise Program
3.1.2. Structuring the Class
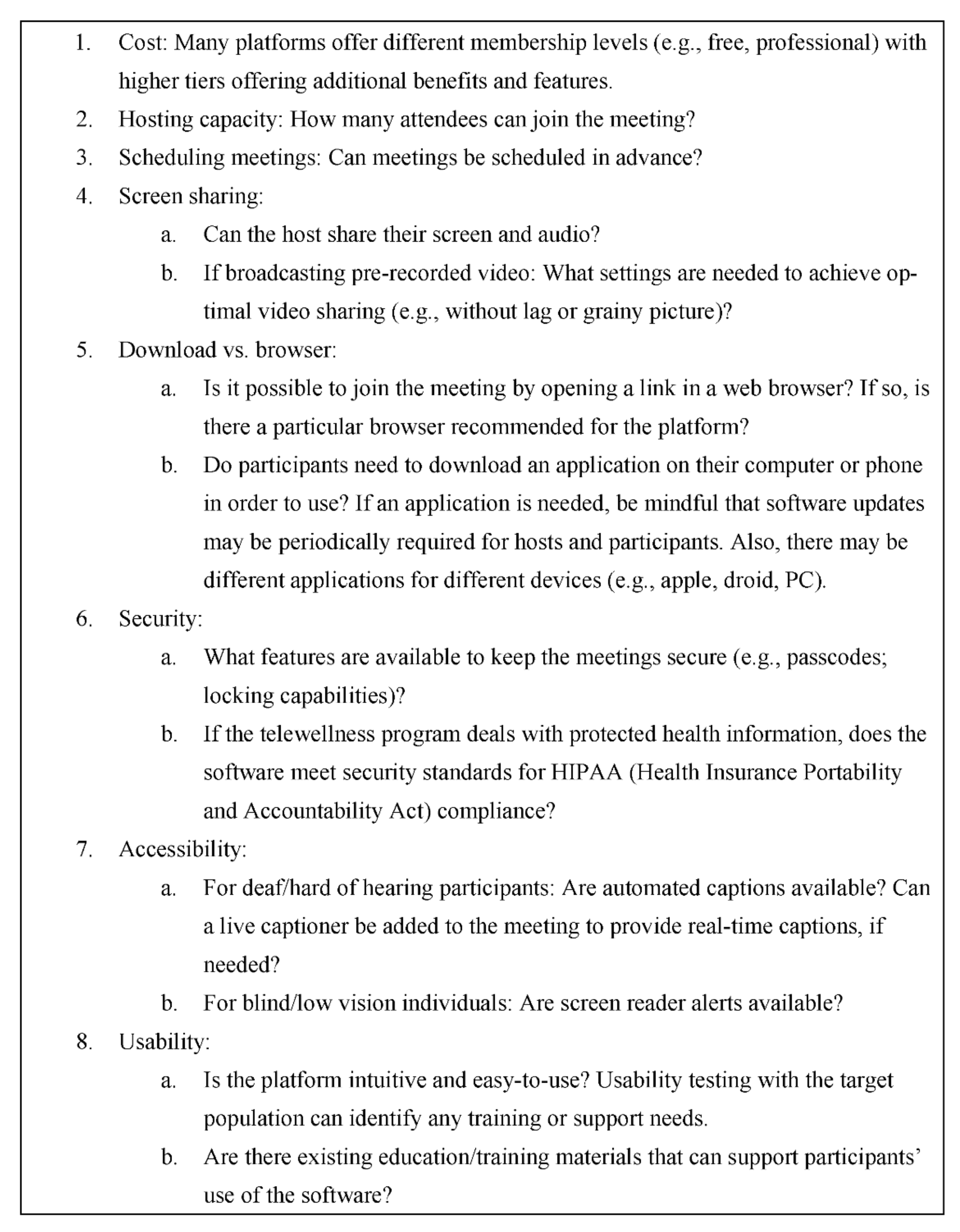
3.1.3. Identifying a Software and Optimizing Settings
3.1.4. Ensuring Safety
3.2. Supporting Remote Participation
3.2.1. Providing Technical Support and Assistance
3.2.2. Orienting Participants
3.2.3. Optimizing Environment
3.3. Promoting Socialization and Engagement
3.3.1. Guiding Discussion
3.3.2. Providing Opportunities for Feedback
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beer, J.M.; Mitzner, T.L.; Rogers, W.A. Design considerations for technology interventions to support social and physical wellness for older adults with disability. Int. J. Autom. Smart Technol. 2015, 5, 249–264. [Google Scholar] [CrossRef]
- Administration for Community Living. 2020 Profile of Older Americans; Administration for Community Living: Washington, DC, USA, 2020.
- Erickson, W.; Lee, C.; Von Schrader, S. Disability Statistics from the American Community Survey (ACS); Cornell University Yang-Tan Institute (YTI): Ithaca, NY, USA, 2017; Available online: www.disabilitystatistics.org (accessed on 12 January 2022).
- Centers for Disease Control (CDC). Healthy People 2010; Centers for Disease Control (CDC): Atlanta, GA, USA, 2010.
- Anderson, L.; Oldridge, N.; Thompson, D.R.; Zwisler, A.-D.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J. Am. Coll. Cardiol. 2016, 67, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Giardini, M.; Nardone, A.; Godi, M.; Guglielmetti, S.; Arcolin, I.; Pisano, F.; Schieppati, M. Instrumental or physical-exercise rehabilitation of balance improves both balance and gait in Parkinson’s disease. Neural Plast. 2018, 2018, 5614242. [Google Scholar] [CrossRef]
- Macko, R.F.; Ivey, F.M.; Forrester, L.W.; Hanley, D.; Sorkin, J.D.; Katzel, L.I.; Silver, K.H.; Goldberg, A.P. Treadmill exercise rehabilitation improves ambulatory function and cardiovascular fitness in patients with chronic stroke. Stroke 2005, 36, 2206–2211. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.S.; Walker, S.; Smart, N.A.; Piepoli, M.F.; Warren, F.C.; Ciani, O.; Whellan, D.; O’Connor, C.; Keteyian, S.J.; Coats, A.; et al. Impact of exercise rehabilitation on exercise capacity and quality-of-life in heart failure: Individual participant meta-analysis. J. Am. Coll. Cardiol. 2019, 73, 1430–1443. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.C.; Maher, C.G.; Briffa, T.; Sherrington, C.; Bennell, K.; Alison, J.; Singh, M.F.; Glasziou, P.P. Prescribing exercise interventions for patients with chronic conditions. Can. Med. Assoc. J. 2016, 188, 510–518. [Google Scholar] [CrossRef]
- Chodzko-Zajko, W.; Schwingel, A.; Chae Hee, P. Successful aging: The role of physical activity. Am. J. Lifestyle Med. 2009, 3, 20–28. [Google Scholar] [CrossRef]
- Moore, S.C.; Patel, A.V.; Matthews, C.E.; Berrington de Gonzalez, A.; Park, Y.; Katki, H.A.; Linet, M.S.; Weiderpass, E.; Visvanathan, K.; Helzlsouer, K.J.; et al. Leisure Ttme physical activity of moderate to vigorous intensity and mortality: A large pooled cohort analysis. PLOS Med. 2012, 9, e1001335. [Google Scholar] [CrossRef]
- United States Office of Disease Prevention and Health Promotion. 2008 Physical Activity Guidelines for Americans; United States Office of Disease Prevention and Health Promotion: Washington, DC, USA, 2008.
- Bixter, M.T.; Blocker, K.A.; Rogers, W.A. Enhancing social engagement of older adults through technology. In Aging, Technology and Health; Pak, R., McLaughlin, A.C., Eds.; Academic Press: San Diego, CA, USA, 2018; pp. 179–214. [Google Scholar]
- Lydon, E.A.; Nguyen, L.T.; Nie, Q.; Rogers, W.A.; Mudar, R.A. An integrative framework to guide social engagement interventions and technology design for persons with mild cognitive impairment. Front. Public Health 2022, 9, 750340. [Google Scholar] [CrossRef]
- Lee, R.M.; Robbins, S.B. The relationship between social connectedness and anxiety, self-esteem, and social identity. J. Couns. Psychol. 1998, 45, 338–345. [Google Scholar] [CrossRef]
- Cornwell, B.; Laumann, E.O.; Schumm, L.P. The social connectedness of older adults: A national profile. Am. Sociol. Rev. 2008, 73, 185–203. [Google Scholar] [CrossRef] [PubMed]
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social relationships and mortality risk: A meta-analytic review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, J.R.H.; Kellezi, B.; Stevenson, C.; McNamara, N.; Bowe, M.; Wilson, I.; Halder, M.M.; Mair, E. Social prescribing as ‘Social Cure’: A longitudinal study of the health benefits of social connectedness within a social prescribing pathway. J. Health Psychol. 2022, 27, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef]
- The National Academies of Sciences, Engineering, and Medicine; Division of Behavioral and Social Sciences and Education; Health and Medicine Division; Board on Behavioral, Cognitive, and Sensory Sciences; Board on Health Sciences Policy; Committee on the Health and Medical Dimensions of Social Isolation and Loneliness in Older Adults. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System; National Academies Press (US): Washington, DC, USA, 2020.
- Bennell, K.L.; Lawford, B.J.; Keating, C.; Brown, C.; Kasza, J.; Mackenzie, D.; Metcalf, B.; Kimp, A.J.; Egerton, T.; Spiers, L.; et al. Comparing video-based, telehealth-delivered exercise and weight loss programs with online education on outcomes of knee osteoarthritis. Ann. Intern. Med. 2021, 175, 198–209. [Google Scholar] [CrossRef]
- Ellis, T.D.; Cavanaugh, J.T.; Deangelis, T.; Hendron, K.; Thomas, C.A.; Saint-Hilaire, M.; Pencina, K.; Latham, N.K. Comparative effectiveness of mHealth-supported exercise compared with exercise alone for people with Parkinson disease: Randomized controlled pilot study. Phys. Ther. 2019, 99, 203–216. [Google Scholar] [CrossRef]
- Quinn, L.; Macpherson, C.; Long, K.; Shah, H. Promoting physical activity via telehealth in people with Parkinson disease: The path forward after the COVID-19 pandemic? Phys. Ther. 2020, 100, 1730–1736. [Google Scholar] [CrossRef]
- Howland, C.; Wakefield, B. Assessing telehealth interventions for physical activity and sedentary behavior self-management in adults with type 2 diabetes mellitus: An integrative review. Res. Nurs. Health 2021, 44, 92–110. [Google Scholar] [CrossRef]
- Lafaro, K.J.; Raz, D.J.; Kim, J.Y.; Hite, S.; Ruel, N.; Varatkar, G.; Erhunmwunsee, L.; Melstrom, L.; Lee, B.; Singh, G.; et al. Pilot study of a telehealth perioperative physical activity intervention for older adults with cancer and their caregivers. Support. Care Cancer 2019, 28, 3867–3876. [Google Scholar] [CrossRef]
- Wilroy, J.; Herbey, I.; Ivankova, N.; Rimmer, J. Grounded theory model for adherence to home exercise among people with a mobility disability. J. Clin. Transl. Sci. 2021, 5, 66. [Google Scholar] [CrossRef]
- Tsai, H.-H.; Tsai, Y.-F. Changes in depressive symptoms, social support, and loneliness over 1 Year after a minimum 3-month videoconference program for older nursing home residents. J. Med. Internet Res. 2011, 13, 373–384. [Google Scholar] [CrossRef] [PubMed]
- Talmage, C.A.; Coon, D.W.; Dugger, B.N.; Knopf, R.C.; O’Connor, K.A.; Schofield, S.A. Social leisure activity, physical activity, and valuation of life: Findings from a longevity study. Act. Adapt. Aging 2019, 44, 61–84. [Google Scholar] [CrossRef]
- Collado-Mateo, D.; Lavín-Pérez, A.M.; Peñacoba, C.; Del Coso, J.; Leyton-Román, M.; Luque-Casado, A.; Gasque, P.; Fernández-Del-Olmo, M.Á.; Amado-Alonso, D. Key factors associated with adherence to physical exercise in patients with chronic diseases and older adults: An umbrella review. Int. J. Environ. Res. Public Health 2021, 18, 2023. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, R.E.; Martin, A.D.; Taunton, J.E.; Rhodes, E.C.; Donnelly, M.; Elliot, J. Factors associated with exercise adherence among older adults. Sports Med. 1999, 28, 397–411. [Google Scholar] [CrossRef]
- Tallner, A.; Pfeifer, K.; Mäurer, M. Web-based interventions in multiple sclerosis: The potential of tele-rehabilitation. Ther. Adv. Neurol. Disord. 2016, 9, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Pardasani, M. Senior centers: Characteristics of participants and nonparticipants. Act. Adapt. Aging 2010, 34, 48–70. [Google Scholar] [CrossRef]
- Czaja, S.J.; Boot, W.R.; Charness, N.; Rogers, W.A. Designing for Older Adults; CRC Press: Boca Raton, FL, USA, 2019. [Google Scholar] [CrossRef]
- Nie, Q.; Nguyen, L.; Myers, D.; Gibson, A.; Kerssens, C.; Mudar, R.; Rogers, W. Design guidance for video chat system to support social engagement for older adults with and without mild cognitive impairment. Gerontechnology 2020, 20, 1–15. [Google Scholar] [CrossRef]
- Fraser, J.; Gutwin, C. A framework of assistive pointers for low vision users. In Proceedings of the Fourth International ACM Conference on Assistive Technologies, Arlington, VA, USA, 13–15 November 2000. [Google Scholar]
- Smith, A. Older Adults and Technology Use. 2014. Available online: https://www.pewresearch.org/internet/2014/04/03/older-adults-and-technology-use/ (accessed on 12 January 2022).
- Vaportzis, E.; Giatsi Clausen, M.; Gow, A.J. Older adults perceptions of technology and barriers to interacting with tablet computers: A focus group study. Front. Psychol. 2017, 8, 1687. [Google Scholar] [CrossRef]
- Anderson, M.; Perrin, A. Tech Adoption Climbs among Older Adults: Technology Use Among Seniors. 2017. Available online: https://www.pewresearch.org/internet/2017/05/17/tech-adoption-climbs-among-older-adults/ (accessed on 12 January 2022).
- Seifert, A.; Cotten, S.R.; Xie, B. A double burden of exclusion? Digital and social exclusion of older adults in times of COVID-19. J. Gerontol. Ser. B 2021, 76, e99–e103. [Google Scholar] [CrossRef]
- Kakulla, B. Tech Trends and Adults 50-Plus; AARP Research: Washington, DC, USA, 2022. [Google Scholar]
- Turgoose, D.; Ashwick, R.; Murphy, D. Systematic review of lessons learned from delivering tele-therapy to veterans with post-traumatic stress disorder. J. Telemed. Telecare 2018, 24, 575–585. [Google Scholar] [CrossRef]
- Morrison, K.S.; Paterson, C.; Toohey, K. The Feasibility of Exercise Interventions Delivered via Telehealth for People Affected by Cancer: A Rapid Review of the Literature. In Seminars in Oncology Nursing; WB Saunders: Philadelphia, PA, USA, 2020; Volume 36, p. 151092. [Google Scholar]
- National Council on Aging. About Evidence-Based Programs. 2022. Available online: https://www.ncoa.org/article/about-evidence-based-programs (accessed on 15 March 2022).
- Stuck, R.; Mitzner, T.L. Designing successful exercise classes for older adults with mobility disabilities. Certif. Sr. Advis. J. 2021, 83, 3–9. [Google Scholar]
- Mitzner, T.L.; Stuck, R.; Hartley, J.Q.; Beer, J.M.; Rogers, W.A. Acceptance of televideo technology by adults aging with a mobility impairment for health and wellness interventions. J. Rehabil. Assist. Technol. Eng. 2017, 4, 2055668317692755. [Google Scholar] [CrossRef] [PubMed]
- Beer, J.; Mackin, T.; Mois, G.; Koon, L.; Datta, A.; Mitzner, T.; Rogers, W. User attitudes and implementation requirements of a tele-exercise intervention for people aging with lower body mobility impairment. Gerontechnology 2021, 20, 1–12. [Google Scholar] [CrossRef]
- Mitzner, T.L.; Remillard, E.T.; Cohen, K.; Cochran, L. TechSAge Tool: Guidelines for Delivering Telewellness Programs to Older Adults with Disabilities; Rehabilitation Engineering Research Center on Technologies to Support Aging-in-Place for People with Long-Term Disabilities, Atlanta, GA, USA. 2021. Available online: https://techsage.gatech.edu/sites/default/files/2021-08/TechSAge%20Tool_Telewellness%20Guidelines_V1_Final.pdf (accessed on 12 January 2022).
- Klempel, N.; Blackburn, N.E.; McMullan, I.L.; Wilson, J.J.; Smith, L.; Cunningham, C.; O’Sullivan, R.; Caserotti, P.; Tully, M.A. The effect of chair-based exercise on physical function in older adults: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 1902. [Google Scholar] [CrossRef]
- Marusic, U.; Grosprêtre, S.; Paravlic, A.; Kovač, S.; Pišot, R.; Taube, W. Motor Imagery during Action Observation of Locomotor Tasks Improves Rehabilitation Outcome in Older Adults after Total Hip Arthroplasty. Neural Plast. 2018, 2018, 5651391. [Google Scholar] [CrossRef]
- Guillot, A.; Collet, C.; Nguyen, V.A.; Malouin, F.; Richards, C.; Doyon, J. Brain activity during visual versus kinesthetic imagery: An fMRI study. Hum. Brain Mapp. 2009, 30, 2157–2172. [Google Scholar] [CrossRef]
- Adams, R. Revised Physical Activity Readiness Questionnaire. Can. Fam. Physician Med. Fam. Can. 1999, 45, 992–1005. [Google Scholar]
- Waite, L.J. The demographic faces of the elderly. Popul. Dev. Rev. 2004, 30, 3–16. [Google Scholar]
- Data.ai. State of Mobile. Available online: https://go.appannie.com/State-of-Mobile-2021-PreRegister.html (accessed on 12 January 2022).
- Callahan, L.F.; Cleveland, R.J.; Altpeter, M.; Hackney, B. Evaluation of tai chi program effectiveness for people with arthritis in the community: A randomized controlled trial. J. Aging Phys. Act. 2016, 24, 101–110. [Google Scholar] [CrossRef]
- Voukelatos, A.; Cumming, R.G.; Lord, S.R.; Rissel, C. A randomized, controlled trial of tai chi for the prevention of falls: The central Sydney tai chi trial. J. Am. Geriatr. Soc. 2007, 55, 1185–1191. [Google Scholar] [CrossRef]
- Fransen, M.; Nairn, L.; Winstanley, J.; Lam, P.; Edmonds, J. Physical activity for osteoarthritis management: A randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Care Res. 2007, 57, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Gardiner, C.; Geldenhuys, G.; Gott, M. Interventions to reduce social isolation and loneliness among older people: An integrative review. Health Soc. Care Community 2018, 26, 147–157. [Google Scholar] [CrossRef] [PubMed]
- O’Rourke, H.M.; Collins, L.; Sidani, S. Interventions to address social connectedness and loneliness for older adults: A scoping review. BMC Geriatr. 2018, 18, 214. [Google Scholar] [CrossRef]
- Collins, C.C.; Benedict, J. Evaluation of a community-based health promotion program for the elderly: Lessons from seniors CAN. Am. J. Health Promot. 2006, 21, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Cox, E.O.; Green, K.E.; Hobart, K.; Jang, L.-J.; Seo, H. Strengthening the late-life care process: Effects of two forms of a care-receiver efficacy intervention. Gerontologist 2007, 47, 388–397. [Google Scholar] [CrossRef][Green Version]
- Martina, C.M.S.; Stevens, N.L. Breaking the cycle of loneliness? Psychological effects of a friendship enrichment program for older women. Aging Ment. Health 2006, 10, 467–475. [Google Scholar] [CrossRef]
- Ollonqvist, K.; Palkeinen, H.; Aaltonen, T.; Pohjolainen, T.; Puukka, P.; Hinkka, K.; Pöntinen, S. Alleviating loneliness among frail older people—Findings from a randomised controlled trial. Int. J. Ment. Health Promot. 2008, 10, 26–34. [Google Scholar] [CrossRef]
- Stewart, M.; Craig, D.; MacPherson, K.; Alexander, S. Promoting positive affect and diminishing loneliness of widowed seniors through a support intervention. Public Health Nurs. 2001, 18, 54–63. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitzner, T.L.; Remillard, E.T.; Mumma, K.T. Research-Driven Guidelines for Delivering Group Exercise Programs via Videoconferencing to Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 7562. https://doi.org/10.3390/ijerph19137562
Mitzner TL, Remillard ET, Mumma KT. Research-Driven Guidelines for Delivering Group Exercise Programs via Videoconferencing to Older Adults. International Journal of Environmental Research and Public Health. 2022; 19(13):7562. https://doi.org/10.3390/ijerph19137562
Chicago/Turabian StyleMitzner, Tracy L., Elena T. Remillard, and Kara T. Mumma. 2022. "Research-Driven Guidelines for Delivering Group Exercise Programs via Videoconferencing to Older Adults" International Journal of Environmental Research and Public Health 19, no. 13: 7562. https://doi.org/10.3390/ijerph19137562
APA StyleMitzner, T. L., Remillard, E. T., & Mumma, K. T. (2022). Research-Driven Guidelines for Delivering Group Exercise Programs via Videoconferencing to Older Adults. International Journal of Environmental Research and Public Health, 19(13), 7562. https://doi.org/10.3390/ijerph19137562




