Medication Knowledge and Adherence in Type 2 Diabetes Mellitus Patients in Brunei Darussalam: A Pioneer Study in Brunei Darussalam
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Settings
2.2. Study Population
2.3. Questionnaire and Score Measurement
2.4. Pilot Study
2.5. Data Analysis
2.6. Ethical Approval
3. Results
3.1. Demographic Data
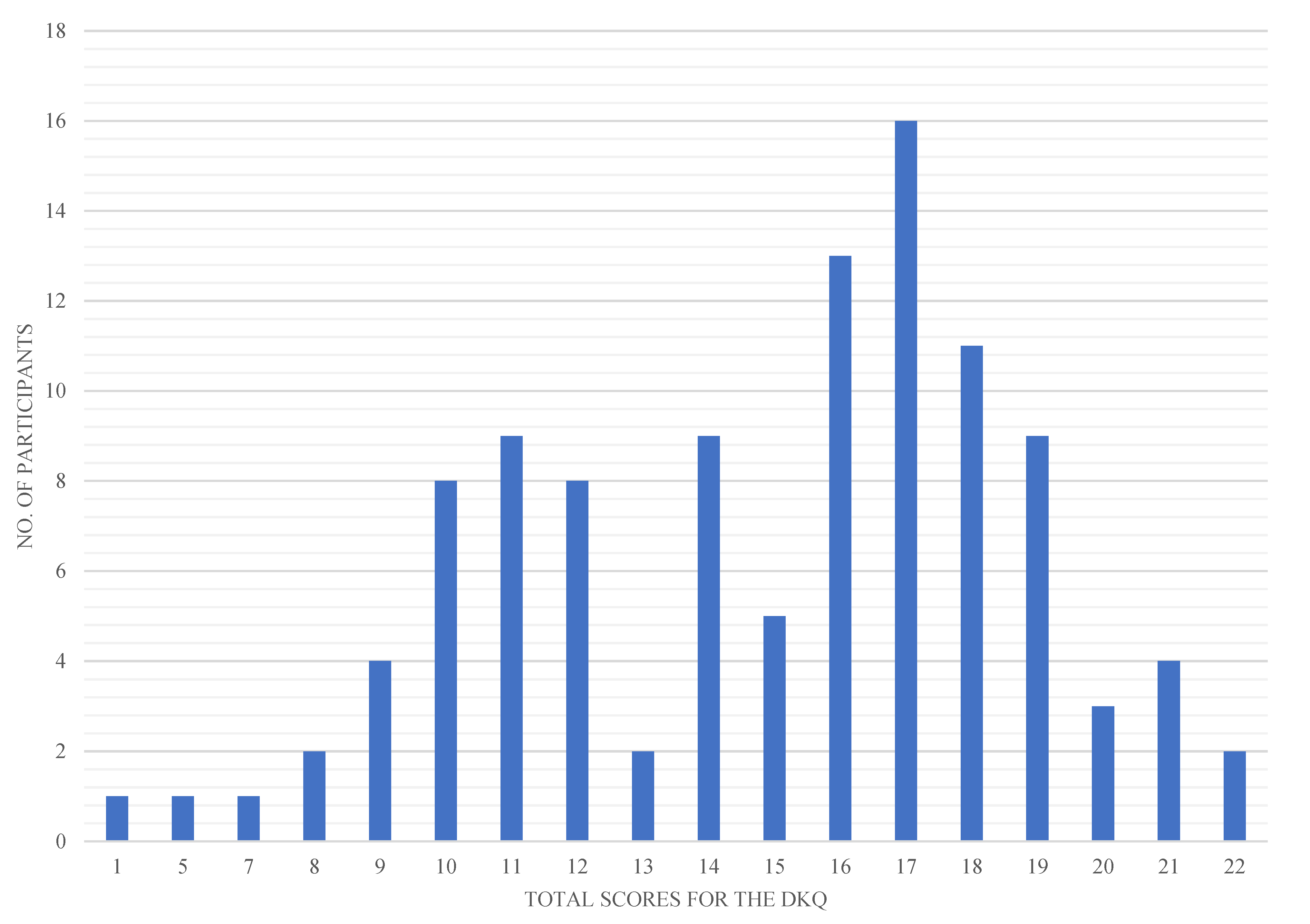
3.2. Diabetes Knowledge Questionnaire
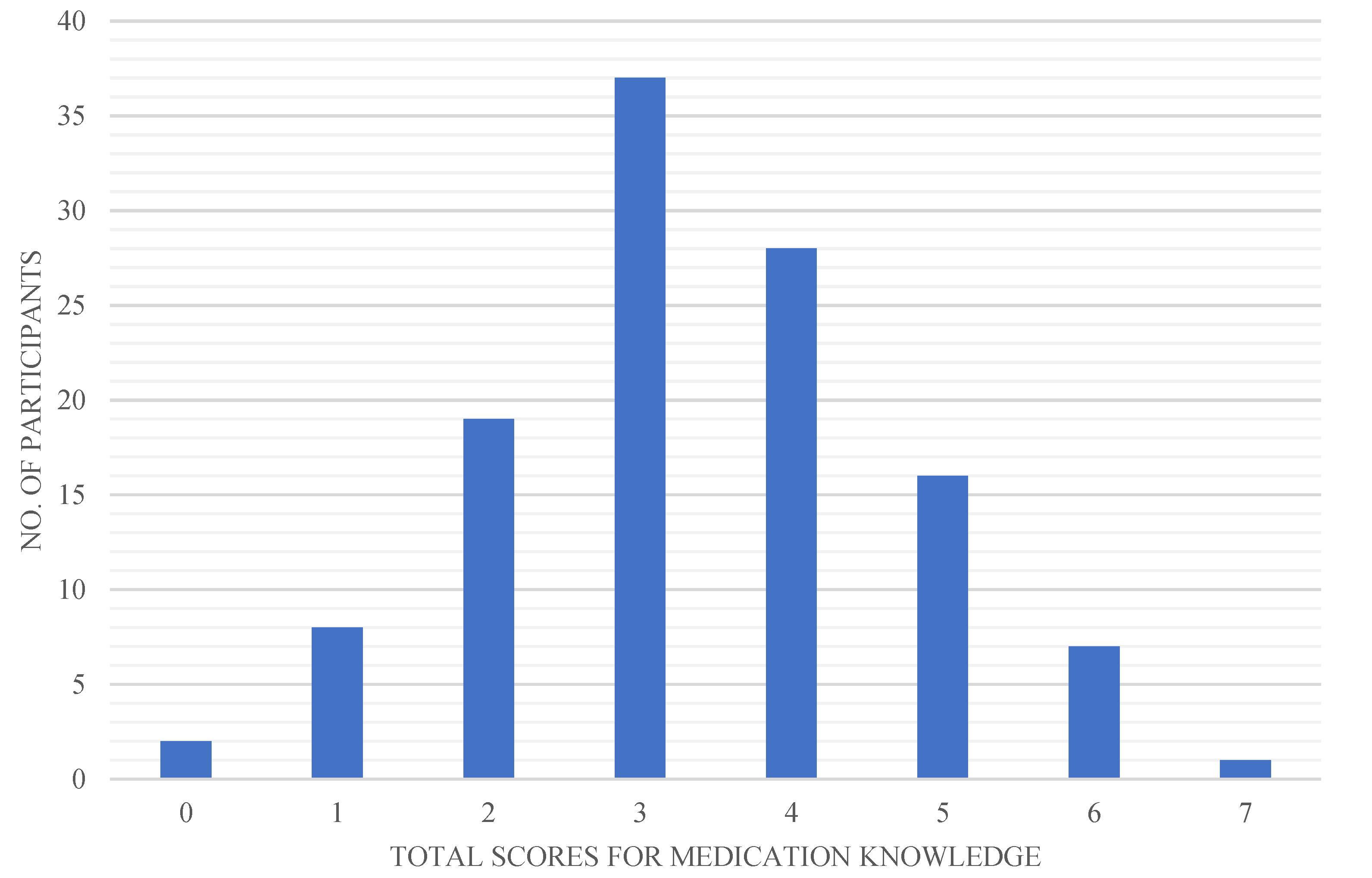
3.3. Medication Knowledge
3.4. Medication Adherence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Kharroubi, A.T. Diabetes mellitus: The epidemic of the century. World J. Diabetes 2015, 6, 850. [Google Scholar] [CrossRef] [PubMed]
- Diabetes, D.O.F. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010, 33 (Suppl. 1), S81–S90. [Google Scholar]
- Olokoba, A.B.; Obateru, O.A.; Olokoba, L.B. Type 2 diabetes mellitus: A review of current trends. Oman Med. J. 2012, 27, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.K.; Lai, D.T.C.; Wong, J.Y.Y.; Si-Ramlee, K.A.; Razak, L.; Kassim, N.; Kamis, Z.; Koh, D. Cross-sectional STEPwise Approach to Surveillance (STEPS) Population Survey of Noncommunicable Diseases (NCDs) and Risk Factors in Brunei Darussalam 2016. Asia Pac. J. Public Health 2017, 29, 635–648. [Google Scholar] [CrossRef]
- 2016 World Health Day Focuses on Beating Diabetes|Brunei’s No.1 News Website. Available online: https://www.brudirect.com/news.php?id=1428 (accessed on 9 May 2022).
- Paola de Carvalho, T.I.; Fernanda Pinto Okuno, M.I.; Regina Vancini Campanharo, C.I.; Carolina Barbosa Teixeira Lopes, M.I.; Ester Assayag Batista, R.I. Patients’ Knowledge about Medication Prescription in the Emergency Service. Rev. Bras. Enferm. 2018, 71, 329–335. [Google Scholar] [CrossRef] [Green Version]
- Gudeta, T.; Mechal, D. Patient Knowledge of Correct Dosage Regimen; The Need for Good Dispensing Practice. J. Prim. Care Community Health 2019, 10, 2150132719876522. [Google Scholar] [CrossRef] [Green Version]
- Rubio, J.S.; García-Delgado, P.; Iglésias-Ferreira, P.; Mateus-Santos, H.; Martínez-Martínez, F. Measurement of patients’ knowledge of their medication in community pharmacies in Portugal. Cienc Saude Coletiva 2015, 20, 219–228. [Google Scholar] [CrossRef]
- Cumbler, E.; Wald, H.; Kutner, J. Lack of patient knowledge regarding hospital medications. J. Hosp. Med. 2010, 5, 83–86. [Google Scholar] [CrossRef]
- Ramia, E.; Zeenny, R.M.; Hallit, S.; Salameh, P. Assessment of patients’ knowledge and practices regarding their medication use and risks in Lebanon. Int. J. Clin. Pharm. 2017, 39, 1084–1094. [Google Scholar] [CrossRef]
- Sample Size Calculator by Raosoft, Inc. Raosoft. 2020. Available online: http://www.raosoft.com/samplesize.html (accessed on 10 May 2022).
- Omar, N.; Wong, J.; Thu, K.; Alikhan, F.; Chaw, L. International Journal of Infectious Diseases Prevalence and associated factors of diabetes mellitus among tuberculosis patients in Brunei Darussalam: A 6-year retrospective cohort study. Int. J. Infect. Dis. 2021, 105, 267–273. [Google Scholar] [CrossRef]
- Garcia, A.A.; Villagomez, E.T.; Brown, S.A.; Kouzekanani, K.; Hanis, C.L. The Starr County Diabetes Education Study: Development of the Spanish-language diabetes knowledge questionnaire. Diabetes Care 2001, 24, 16–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McPherson, M.L.; Smith, S.W.; Powers, A.; Zuckerman, I.H. Association between diabetes patients’ knowledge about medications and their blood glucose control. Res. Soc. Adm. Pharm. 2008, 4, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Okuyan, B.; Sancar, M.; Izzetin, F.V. Assessment of medication knowledge and adherence among patients under oral chronic medication treatment in community pharmacy settings. Pharmacoepidemiol. Drug Saf. 2013, 22, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Mekonnen, G.B.; Gelayee, D.A. Low Medication Knowledge and Adherence to Oral Chronic Medications among Patients Attending Community Pharmacies: A Cross-Sectional Study in a Low-Income Country. BioMed Res. Int. 2020, 2020, 4392058. [Google Scholar] [CrossRef] [PubMed]
- Arifulla, M.; John, L.J.; Sreedharan, J.; Muttappallymyalil, J.; Basha, A. Patients’ Adherence to Anti-Diabetic Medications in a Hospital at Ajman, UAE. Malays. J. Med. Sci. 2014, 21, 44–49. [Google Scholar] [PubMed]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’ s alpha. Int. J. Med. Educ. 2011, 2, 53. [Google Scholar] [CrossRef]
- Watkins, M.W. A Step-by-Step Guide to Exploratory Factor Analysis with R and RStudio; Routledge: London, UK, 2020. [Google Scholar]
- Bujang, M.A.; Omar, E.D.; Baharum, N.A. A Review on Sample Size Determination for Cronbach’s Alpha Test: A Simple Guide for Researchers. Malays J. Med. Sci. 2018, 25, 85–99. [Google Scholar] [CrossRef]
- Mirahmadizadeh, A.; Khorshidsavar, H.; Seif, M.; Sharifi, M.H. Adherence to Medication, Diet and Physical Activity and the Associated Factors Amongst Patients with Type 2 Diabetes. Diabetes Ther. 2020, 11, 479–494. [Google Scholar] [CrossRef] [Green Version]
- Tan, S.Y.; Shazli, A.A.H.; Abd Wahab, A.; Rahman, A.A.; Idris, F. Diabetes awareness in Kampong Kapok, Brunei Maura district, Brunei Darussalam. Brunei Int. Med. J. 2015, 11, 247–250. [Google Scholar]
- Pecoits-Filho, R.; Abensur, H.; Betônico, C.C.R.; Machado, A.D.; Parente, E.B.; Queiroz, M.; Salles, J.E.N.; Titan, S.; Vencio, S. Interactions between kidney disease and diabetes: Dangerous liaisons. Diabetol. Metab. Syndr. 2016, 8, 50. [Google Scholar] [CrossRef]
- Watson, S. Foamy Urine: Symptoms, Causes, and More. 2017. Available online: https://www.healthline.com/health/foamy-urine (accessed on 10 May 2022).
- Hyperglycemia and Hypoglycemia in Type 2 Diabetes-InformedHealth.org-NCBI Bookshelf. Available online: https://www.ncbi.nlm.nih.gov/books/NBK279510/ (accessed on 10 May 2022).
- Bukhsh, A.; Khan, T.M.; Nawaz, M.S.; Ahmed, H.S.; Chan, K.G.; Goh, B.H. Association of diabetes knowledge with glycemic control and self-care practices among pakistani people with type 2 diabetes mellitus. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 1409–1417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abbasi, Y.F.; See, O.G.; Ping, N.Y.; Balasubramanian, G.P.; Hoon, Y.C.; Paruchuri, S. Diabetes knowledge, attitude, and practice among type 2 diabetes mellitus patients in Kuala Muda District, Malaysia—A cross-sectional study. Diabetes Metab. Syndr. Clin. Res. Rev. 2018, 12, 1057–1063. [Google Scholar] [CrossRef] [PubMed]
- Lim, P.C.; Rajah, R.; Lee, C.Y.; Wong, T.Y.; Tan, S.S.A.; Karim, S.A. Systematic Review and Meta-Analysis of Diabetes Knowledge among Type 2 Diabetes Patients in Southeast Asia. Rev. Diabet. Stud. 2021, 17, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Cryer, P.E. Minimizing hypoglycemia in diabetes. Diabetes Care 2015, 38, 1583–1591. [Google Scholar]
- Romero-Sanchez, J.; Garcia-Cardenas, V.; Abaurre, R.; Martínez-Martínez, F.; Garcia-Delgado, P. Prevalence and predictors of inadequate patient medication knowledge. J. Eval. Clin. Pract. 2016, 22, 808–815. [Google Scholar] [CrossRef] [Green Version]
- Hargis, M.B.; Castel, A.D. Improving Medication Understanding and Adherence Using Principles of Memory and Metacognition: In Press-Policy Insights from Behavioral and Brain Sciences. Policy Insights Behav Brain Sci. 2018, 5, 147–154. [Google Scholar] [CrossRef]
- Karaoui, L.R.; Deeb, M.E.; Nasser, L.; Hallit, S. Knowledge and practice of patients with diabetes mellitus in Lebanon: A cross-sectional study. BMC Public Health 2018, 18, 525. [Google Scholar] [CrossRef] [Green Version]
- Alshayban, D.M.; Naqvi, A.A.; Alhumaid, O.; Alqahtani, A.S.; Islam, A.; Ghori, S.A.; Haseeb, A.; Ali, M.; Iqbal, M.S.; Elrggal, M.E.; et al. Association of Disease Knowledge and Medication Adherence Among Out-Patients With Type 2 Diabetes Mellitus in Khobar, Saudi Arabia. Front. Pharmacol. 2020, 11, 60. [Google Scholar] [CrossRef] [Green Version]
- Al-Qazaz, H.K.; Sulaiman, S.A.; Hassali, M.A.; Shafie, A.A.; Sundram, S.; Al-Nuri, R.; Saleem, F. Diabetes knowledge, medication adherence and glycemic control among patients with type 2 diabetes. Int. J. Clin. Pharm. 2011, 33, 1028–1035. [Google Scholar] [CrossRef]
- Manan, M.M.; Husin, A.R.; Alkhoshaiban, A.S.; Al-Worafi, Y.M.A.; Ming, L.C. Interplay between Oral Hypoglycemic Medication Adherence and Quality of Life among Elderly Type 2 Diabetes Mellitus Patients. J. Clin. Diagn. Res. 2014, 8, JC05. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4316278/ (accessed on 15 May 2022). [CrossRef]
- Review, C. Interventions to Improve Medication Adherence A Review. JAMA 2020, 320, 2461–2473. [Google Scholar]
- Izahar, S.; Lean, Q.Y.; Hameed, M.A.; Murugiah, M.K.; Patel, R.P.; Al-Worafi, Y.M.; Wong, T.W.; Ming, L.C. Content analysis of Mobile health applications on Diabetes Mellitus. Front. Endocrinol. 2017, 8, 318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milosavljevic, A.; Aspden, T.; Harrison, J. Community pharmacist-led interventions and their impact on patients’ medication adherence and other health outcomes: A systematic review. Int. J. Pharm. Pract. 2018, 26, 387–397. [Google Scholar] [CrossRef] [PubMed]
| Details | n (%) |
|---|---|
| Age (year) | |
| <40 | 12 (10.20) |
| 40–60 | 61 (51.70) |
| >60 | 45 (38.10) |
| Gender | |
| Male | 62 (52.50) |
| Female | 56 (47.50) |
| Race | |
| Malay | 101 (85.60) |
| Non-malay | 17 (14.40) |
| Education level | |
| No formal education | 2 (1.70) |
| Primary school | 13 (11.00) |
| Secondary school | 80 (67.80) |
| Higher education | 23 (19.50) |
| Occupation | |
| Retired | 45 (38.14) |
| Unemployed | 23 (19.49) |
| Private sector | 23 (19.49) |
| Government sector | 21 (17.80) |
| Self-employed | 5 (4.24) |
| Student | 1 (0.85) |
| Family history | |
| Yes | 88 (74.58) |
| No | 24 (20.34) |
| Not sure | 6 (5.08) |
| Duration since diagnosed with T2DM | |
| 6–11 months | 2 (1.69) |
| 1–4 years | 25 (21.19) |
| 5–9 years | 16 (13.56) |
| ≥10 | 75 (63.56) |
| Participants’ antidiabetic therapy | |
| Insulin only | 2 (1.69) |
| Insulin combined with oral medication | 29 (24.58) |
| Oral medication only | 87 (73.73) |
| Abbreviation: | |
| T2DM–Type 2 diabetes mellitus |
| Questions | n (%) |
|---|---|
| 1. Eating too much sugar and other sweet foods is a cause of diabetes. | 5 (4.24) |
| 2. The usual cause of diabetes is lack of effective insulin in the body. | 77 (65.25) |
| 3. Diabetes is caused by failure of the kidneys to keep sugar out of the urine. | 39 (33.05) |
| 4. Kidneys produce insulin. | 33 (28.21) |
| 5. In untreated diabetes, the amount of sugar in the blood usually increases. | 114 (96.61) |
| 6. If I am diabetic, my children have a higher chance of being diabetic. | 83 (70.34) |
| 7. Diabetes can be cured. | 41 (34.75) |
| 8. A fasting blood sugar level of 11.7 mmol/L is too high. | 109 (92.37) |
| 9. The best way to check my diabetes is by testing my urine. | 47 (39.83) |
| 10. Regular exercise will increase the need for insulin or other diabetic medication. | 80 (67.80) |
| 11. There are two main types of diabetes: Type 1 (insulin-dependent) and Type 2 (non-insulin-dependent). | 71 (60.17) |
| 12. An insulin reaction (severe hypoglycemia) is caused by too much food. | 97 (82.20) |
| 13. Medication is more important than diet and exercise to control my diabetes. | 58 (49.15) |
| 14. Diabetes often causes poor circulation. | 69 (58.47) |
| 15. Cuts and abrasions on diabetics heal more slowly. | 98 (83.05) |
| 16. Diabetics should take extra care when cutting their toenails. | 105 (88.98) |
| 17. A person with diabetes should cleanse a cut with iodine and alcohol. | 29 (24.58) |
| 18. The way I prepare my food is as important as the foods I eat. | 92 (77.97) |
| 19. Diabetes can damage my kidneys. | 109 (92.37) |
| 20. Diabetes can cause loss of feelings in my hands, fingers, and feet. | 90 (76.27) |
| 21. Shaking and sweating are signs of high blood sugar. | 71 (60.17) |
| 22. Frequent urination and thirst are signs of low blood sugar. | 77 (65.25) |
| 23. Tight elastic hose or socks are not bad for diabetics. | 65 (55.08) |
| 24. A diabetic diet consists mostly of special foods. | 75 (63.56) |
| p-Value and CI | Correlation Coefficient | |
|---|---|---|
| Diabetes knowledge with: | ||
| Education level | <0.05 (95% CI: 0.002, 0.352) | 0.183 |
| Family history | <0.05 (95% CI: −0.381, −0.036) | −0.215 |
| Total medications taken | <0.05 (95% CI: 0.004, 0.354) | 0.185 |
| Medication knowledge with: | ||
| Gender | <0.05 (95% CI: 0.031, 0.377) | 0.211 |
| Family history | <0.05 (95% CI: −0.227, 0.133) | −0.215 |
| Total medications taken | <0.05 (95% CI: −0.469, −0.143) | −0.315 |
| Medication adherence with: | ||
| Race | <0.05 (95% CI: −0.397, −0.05) | −0.233 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muhammad Haskani, N.H.; Goh, H.P.; Wee, D.V.T.; Hermansyah, A.; Goh, K.W.; Ming, L.C. Medication Knowledge and Adherence in Type 2 Diabetes Mellitus Patients in Brunei Darussalam: A Pioneer Study in Brunei Darussalam. Int. J. Environ. Res. Public Health 2022, 19, 7470. https://doi.org/10.3390/ijerph19127470
Muhammad Haskani NH, Goh HP, Wee DVT, Hermansyah A, Goh KW, Ming LC. Medication Knowledge and Adherence in Type 2 Diabetes Mellitus Patients in Brunei Darussalam: A Pioneer Study in Brunei Darussalam. International Journal of Environmental Research and Public Health. 2022; 19(12):7470. https://doi.org/10.3390/ijerph19127470
Chicago/Turabian StyleMuhammad Haskani, Najwa Hazwani, Hui Poh Goh, Daniel Vui Teck Wee, Andi Hermansyah, Khang Wen Goh, and Long Chiau Ming. 2022. "Medication Knowledge and Adherence in Type 2 Diabetes Mellitus Patients in Brunei Darussalam: A Pioneer Study in Brunei Darussalam" International Journal of Environmental Research and Public Health 19, no. 12: 7470. https://doi.org/10.3390/ijerph19127470
APA StyleMuhammad Haskani, N. H., Goh, H. P., Wee, D. V. T., Hermansyah, A., Goh, K. W., & Ming, L. C. (2022). Medication Knowledge and Adherence in Type 2 Diabetes Mellitus Patients in Brunei Darussalam: A Pioneer Study in Brunei Darussalam. International Journal of Environmental Research and Public Health, 19(12), 7470. https://doi.org/10.3390/ijerph19127470







