Psychological Intervention in Women Victims of Childhood Sexual Abuse: An Open Study—Protocol of a Randomized Controlled Clinical Trial Comparing EMDR Psychotherapy and Trauma-Based Cognitive Therapy
Abstract
:1. Introduction
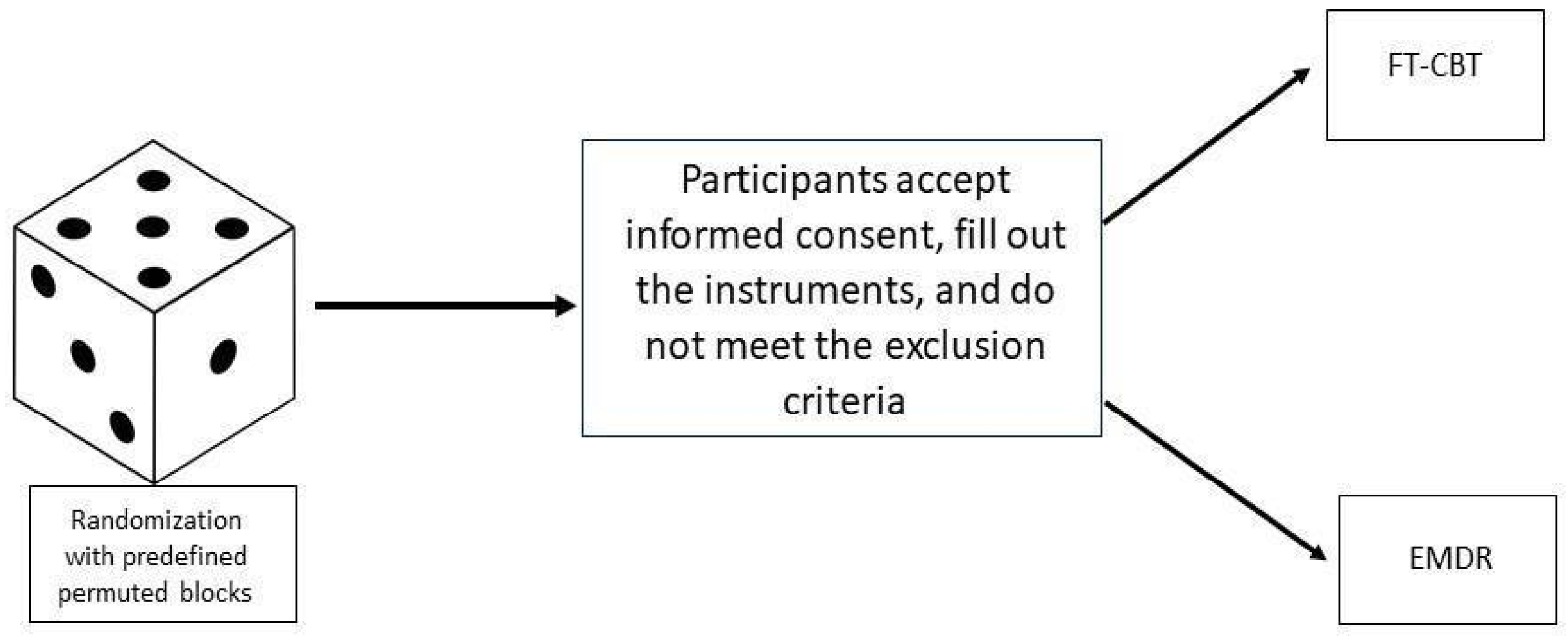
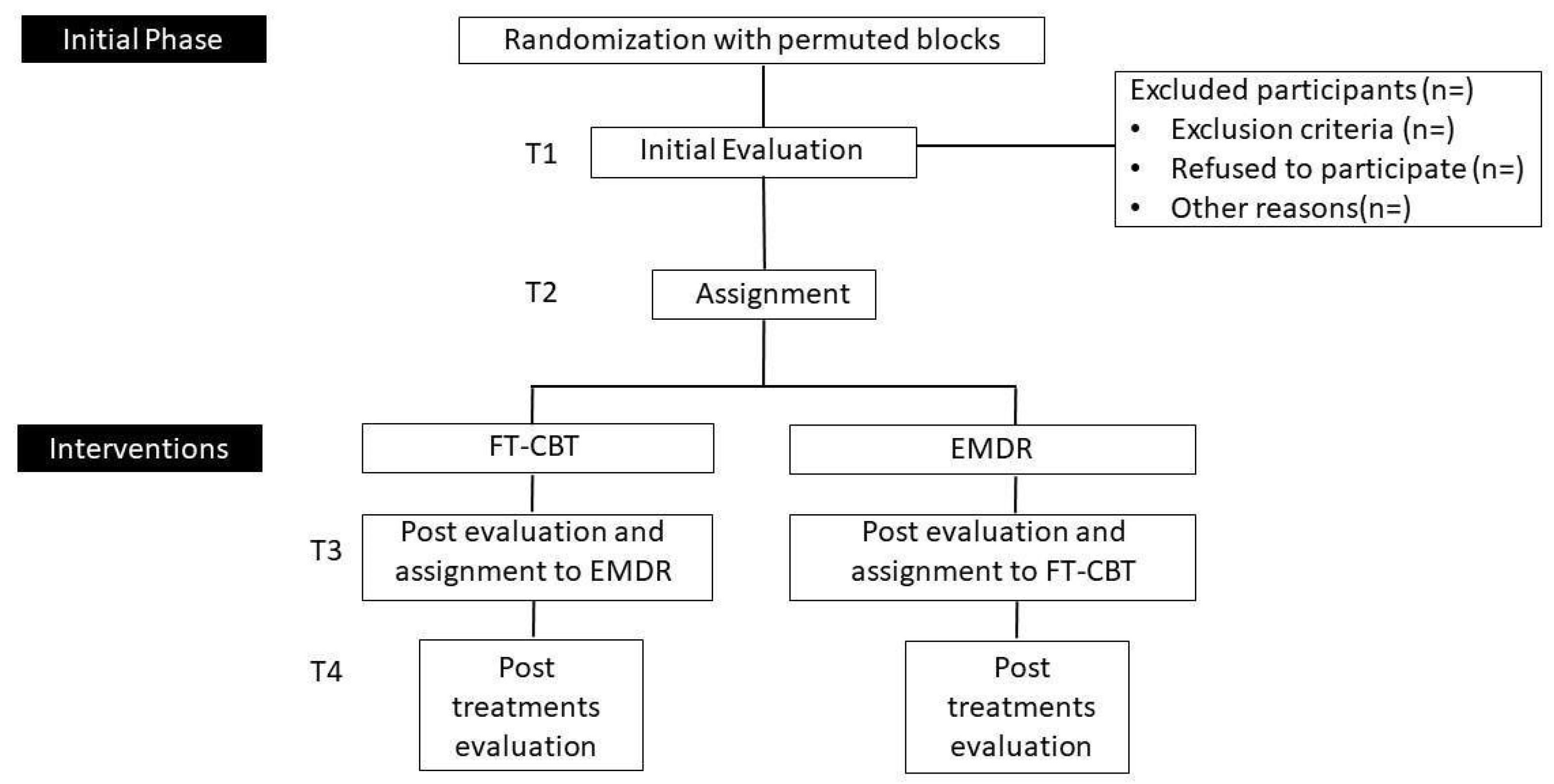
2. Method and Analysis
3. Procedure, Recruitment Process, and Participants
- Women over 18 years of age.
- Follow-up in the ACASI association or similar.
- Present symptoms related to the post-traumatic sequelae of having experienced sexual abuse as a child.
- The traumatic experience is accessible to the participant’s explicit memory.
- The participant has shared her experience in at least a containment context and can talk about it.
- Severe mental illness. Extreme scores in both the personality questionnaire and the psychopathology questionnaire in the indicators of global severity, paranoid ideation, and psychoticism.
- Any addiction problems with alcohol or other substances at the time of the assessment that may interfere with adherence to treatment and group dynamics.
- Being currently in treatment for the traumatic abuse experience.
- Presenting severe dissociative symptoms beyond those typical of a PTSD diagnosis. Extreme scores on the DES dissociation scale on pathological ideation items.
Study Schedule
4. Statistical Analysis
Ethics and Dissemination
5. Measurements
5.1. Satisfaction with Life Scale (SWLS)
5.2. Rosenberg Self-Esteem Scale (RSE)
5.3. Symptom Checklist-90-Revised (SCL-R)
5.4. Post-traumatic Stress Disorder Symptom Severity Scale according to the DSM-5 (EGS-R)
5.5. DSM-5 Personality Inventory—Brief Version (PID-5-BF) Adults
5.6. Scale of Emotional Regulation Difficulties (DERS)
5.7. Dissociative Symptom Scale (DSS)
5.8. Scale of Satisfaction with the TREATMENT received. (CRES-4): Spanish Version
5.9. Ad Hoc Registry for General Sociodemographic and Clinical Variables
6. Protocols of Treatment
7. Trauma-Focused CBT-Based Treatment
7.1. Phase 1: TF-CBT Coping Skills for Complex Traumas
7.2. Phase 2: Trauma Narration and Complicated Trauma Processing
7.3. Phase 3: Treatment Consolidation and Closure
8. Trauma-Focused EMDR-Based Treatment
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Clinical Trial
Provenance and Peer Review
References
- Whitelock, C.F.; Lamb, M.E.; Rentfrow, P.J. Overcoming Trauma: Psychological and Demographic Characteristics of Child Sexual Abuse Survivors in Adulthood. Clin. Psychol. Sci. 2013, 1, 359–362. [Google Scholar] [CrossRef]
- Gardner, M.J.; Thomas, H.J.; Erskine, H.E. The association between five forms of child maltreatment and depressive and anxiety disorders: A systematic review and meta-analysis. Child Abus. Negl. 2019, 96, 104082. [Google Scholar] [CrossRef]
- Scott, K.M.; Koenen, K.C.; King, A.; Petukhova, M.V.; Alonso, J.; Bromet, E.J.; Bruffaerts, R.; Bunting, B.; de Jonge, P.; Haro, J.M.; et al. Post-traumatic stress disorder associated with sexual assault among women in the WHO World Mental Health Surveys. Psychol. Med. 2018, 48, 155–167. [Google Scholar] [CrossRef] [Green Version]
- Sullivan, C.P.; Smith, A.J.; Lewis, M.; Jones, R.T. Network analysis of PTSDsymptoms following mass violence. Psychol. Trauma Theory Res. Pract. Policy 2018, 10, 58–66. [Google Scholar] [CrossRef]
- Weindl, D.; Knefel, M.; Glu, T.; Lueger-Schuster, B. Emotion regulation strategies, self-esteem, and anger in adult survivors of childhood maltreatment in foster care settings. Eur. J. Trauma Dissociation 2020, 4, 100163. [Google Scholar] [CrossRef]
- Gewirtz, A. The relationship between child sexual abuse, self-concept and psychopathology: The moderating role of social support and perceived parental quality. Child. Youth Serv. Rev. 2020, 113, 104938. [Google Scholar] [CrossRef]
- Villodas, M.T.; Morelli, N.M.; Hong, K.; Duong, J.; Evans, M.C.; Elson, D.; Rose, E.; Picci, G.; Fishbein, D. Differences in late adolescent psychopathology among youth with histories of co-occurring abuse and neglect experiences. Child Abus. Negl. 2021, 120, 105189. [Google Scholar] [CrossRef]
- Briere, J.; Runtz, M. Post Sexual Abuse Trauma: Data and Implications for Clinical Practice. J. Interpers. Violence 1987, 2, 367–379. [Google Scholar] [CrossRef]
- Hébert, M.; Langevin, R.; Oussaïd, E. Cumulative childhood trauma, emotion, regulation, dissociation, and behavior problems in school-aged sexual abuse victims. J. Affect. Disord. 2018, 225, 306–312. [Google Scholar] [CrossRef] [Green Version]
- Pereda, N. Short-Term Psychological consequences of child sexual abuse. Papeles del Psicólogo 2009, 30, 135–144. Available online: http://www.cop.es/papeles (accessed on 30 March 2022).
- Brewin, C.R.; Andrews, B.; Valentine, J.D. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J. Consult. Clin. Psychol. 2000, 68, 748–766. [Google Scholar] [CrossRef] [PubMed]
- Hornor, G. Child Sexual Abuse: Consequences and Implications. J. Pediatr. Health Care 2010, 24, 358–364. [Google Scholar] [CrossRef] [PubMed]
- López, S.; Faro, C.; Lopetegui, L.; Pujol-Ribera, E.; Monteagudo, M.; Cobo, J.; Fernández, M.I. Impact of childhood sexual abuse on the sexual and affective relationships of adult women|[Impacto del abuso sexual durante la infancia-adolescencia en las relaciones sexuales y afectivas de mujeres adultas]. Gaceta Sanit. 2017, 31, 210–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarasua, B.; Zubizarreta, I.; de Corral, P.; Echeburúa, E. Psychological treatment of adult female survivors of childhood sexual abuse: Long term results|[Tratamiento psicológico de mujeres adultas víctimas de abuso sexual en la infancia: Resultados a largo plazo]. Anales De Psicologia 2013, 29, 29–37. [Google Scholar]
- Mannarino, A.P.; Cohen, J.A.; Deblinger, E.; Runyon, M.K.; Steer, R.A. Trauma-Focused Cognitive-Behavioral Therapy for Children: Sustained Impact of Treatment 6 and 12 Months Later. Child Maltreat. 2012, 17, 231–241. [Google Scholar] [CrossRef] [Green Version]
- Cary, C.E.; McMillen, J.C. The data behind the dissemination: A systematic review of trauma-focused cognitive behavioral therapy for use with children and youth. Child Youth Serv. Rev. 2012, 34, 748–757. [Google Scholar] [CrossRef]
- Keeshin, B.R.; Strawn, J.R. Psychological and Pharmacologic Treatment of Youth with Posttraumatic Stress Disorder: An Evidence-based Review. Child Adolesc. Psychiatr. Clin. N. Am. 2014, 23, 399–411. [Google Scholar] [CrossRef]
- Leenarts, L.E.W.; Diehle, J.; Doreleijers, T.A.H.; Jansma, E.P.; Lindauer, R.J.L. Evidence-based treatments for children with trauma-related psychopathology as a result of childhood maltreatment: A systematic review. Eur. Child Adolesc. Psychiatry 2013, 22, 269–283. [Google Scholar] [CrossRef]
- Brown, E.J.; Cohen, J.A.; Mannarino, A. Trauma-Focused Cognitive-Behavioral Therapy: The role of caregivers. J. Affect. Disord. 2020, 277, 39–45. [Google Scholar] [CrossRef]
- Jensen, T.K.; Holt, T.; Ormhaug, S.M.; Egeland, K.; Granly, L.; Hoaas, L.C.; Hukkelberg, S.S.; Indregard, T.; Stormyren, S.D.; Wentzel-Larsen, T. A randomized effectiveness study comparing trauma-focused cognitive behavioral therapy with therapy as usual for youth. J. Clin. Child Adolesc. Psychol. 2014, 43, 356–369. [Google Scholar] [CrossRef] [Green Version]
- Rosner, R.; Rimane, E.; Frick, U.; Gutermann, J.; Hagl, M.; Renneberg, B.; Schreiber, F.; Vogel, A.; Steil, R. Effect of Developmentally Adapted Cognitive Processing Therapy for Youth with Symptoms of Posttraumatic Stress Disorder After Childhood Sexual and Physical Abuse: A Randomized Clinical Trial. JAMA Psychiatry 2019, 76, 484–491. [Google Scholar] [CrossRef] [PubMed]
- Thomas, F.C.; Puente-Duran, S.; Mutschler, C.; Monson, C.M. Trauma-focused cognitive behavioral therapy for children and youth in low and middle-income countries: A systematic review. Child Adolesc. Ment. Health 2022, 27, 146–160. [Google Scholar] [CrossRef] [PubMed]
- Konanur, S.; Muller, R.T.; Cinamon, J.S.; Thornback, K.; Zorzella, K.P. Effectiveness of Trauma-Focused Cognitive Behavioral Therapy in a community-based program. Child Abus. Negl. 2015, 50, 159–170. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.L.; Sharma-Patel, K.; Brown, E.J.; Huntt, J.S.; Chaplin, W.F. Complex trauma and Trauma-Focused Cognitive-Behavioral Therapy: How do trauma chronicity and PTSD presentation affect treatment outcome? Child Abus. Negl. 2021, 111, 104734. [Google Scholar] [CrossRef]
- Shapiro, F. Efficacy of the eye movement desensitization procedure in the treatment of traumatic memories. J. Trauma Stress 1989, 2, 199–223. [Google Scholar] [CrossRef]
- Shapiro, F. Eye Movement Desensitization and Reprocessing: Basic Principles, Protocols and Procedures, 2nd ed.; Guilford Press: New York, NY, USA, 2001. [Google Scholar]
- WHO. Guidelines for the Managements of Conditions Specifically Rellated to Stress; WHO: Ginebra, Switzerland, 2013. [Google Scholar]
- Nijdam, M.J.; van der Meer, C.A.I.; van Zuiden, M.; Dashtgard, P.; Medema, D.; Olff, M.Q. Turning wounds into wisdom: Posttraumatic growth over the course of two types of trauma-focused psychotherapy in patients with PTSD. J. Affect. Disord. 2018, 227, 424–431. [Google Scholar] [CrossRef]
- De Roos, C.; van der Oord, S.; Zijlstra, B.; Lucassen, S.; Perrin, S.; Emmelkamp, P.; de Jongh, A. Comparison of eye movement desensitization and reprocessing therapy, cognitive behavioral writing therapy, and wait-list in pediatric posttraumatic stress disorder following single-incident trauma: A multicenter randomized clinical trial. J. Child Psychol. Psychiatry Allied Discip. 2017, 58, 1219–1228. [Google Scholar] [CrossRef]
- Hase, M.; Plagge, J.; Hase, A.; Braas, R.; Ostacoli, L.; Hofmann, A.; Huchzermeier, C. Eye movement desensitization and reprocessing versus treatment as usual in the treatment of depression: A randomized-controlled trial. Front. Psychol. 2018, 9, 1384. [Google Scholar] [CrossRef] [Green Version]
- Edmond, T.; Rubin, A.; Wambach, K. The effectiveness of EMDR with adult female survivors of childhood sexual abuse. Soc. Work. Res. 1999, 23, 103–116. [Google Scholar] [CrossRef]
- Edmond, T.; Rubin, A. Assessing the Long-Term Effects of EMDR: Results from an 18-Month Follow-Up Study with Adult Female Survivors of CSA. J. Child Sex Abus. 2004, 13, 69–86. [Google Scholar] [CrossRef]
- Van Vliet, N.I.; Huntjens, R.J.; Van DIjk, M.K.; Bachrach, N.; Meewisse, M.L.; De Jongh, A. Phase-based treatment versus immediate trauma-focused treatment for post-traumatic stress disorder due to childhood abuse: Randomised clinical trial. BJPsych Open 2021, 7, e211. [Google Scholar] [CrossRef]
- Landin-Romero, R.; Moreno-Alcazar, A.; Pagani, M.; Amann, B.L. How does eye movement desensitization and reprocessing therapy work? A systematic review on suggested mechanisms of action. Front. Psychol. 2018, 9, 1395. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.W.; Cuijpers, P. A meta-analysis of the contribution of eye movements in processing emotional memories. J. Behav. Ther. Exp. Psychiatry 2013, 44, 231–239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Navarro, P.N.; Landin-Romero, R.; Guardiola-Wanden-Berghe, R.; Moreno-Alcázar, A.; Valiente-Gómez, A.; Lupo, W.; García, F.; Fernández, I.; Perez, V.; Amann, B.L. 25 years of Eye Movement Desensitization and Reprocessing (EMDR): The EMDR therapy protocol, hypotheses of its mechanism of action and a systematic review of its efficacy in the treatment of post-traumatic stress disorder. Revista de Psiquiatría y Salud Mental 2018, 11, 101–114. [Google Scholar] [CrossRef]
- Ehring, T.; Welboren, R.; Morina, N.; Wicherts, J.M.; Freitag, J.; Emmelkamp, P.M.G. Meta-analysis of psychological treatments for posttraumatic stress disorder in adult survivors of childhood abuse. Clin. Psychol. Rev. 2014, 34, 645–657. [Google Scholar] [CrossRef] [Green Version]
- Ostacoli, L.; Carletto, S.; Cavallo, M.; Baldomir-Gago, P.; Di Lorenzo, G.; Fernandez, I.; Hase, M.; Justo-Alonso, A.; Lehnung, M.; Migliaretti, G.; et al. Comparison of eye movement desensitization reprocessing and cognitive behavioral therapy as adjunctive treatments for recurrent depression: The European Depression EMDR Network (EDEN) randomized controlled trial. Front. Psychol. 2018, 9, 150–162. [Google Scholar] [CrossRef]
- Khan, A.M.; Dar, S.; Ahmed, R.; Bachu, R.; Adnan, M.; Kotapati, V.P. Cognitive Behavioral Therapy versus Eye Movement Desensitization and Reprocessing in Patients with Post-traumatic Stress Disorder: Systematic Review and Meta-analysis of Randomized Clinical Trials. Cureus 2018, 10, e3250. [Google Scholar] [CrossRef] [Green Version]
- Pierce, B.S.; Perrin, P.B.; Tyler, C.M.; McKee, G.B.; Watson, J.D. The COVID-19 telepsychology revolution: A national study of pandemic-based changes in U.S. mental health care delivery. Am. Psychol. 2021, 76, 14–25. [Google Scholar] [CrossRef]
- Robillard, R.; Daros, A.R.; Phillips, J.L.; Porteous, M.; Saad, M.; Pennestri, M.H.; Kendzerska, T.; Edwards, J.D.; Solomonova, E.; Bhatla, R.; et al. Emerging New Psychiatric Symptoms and the Worsening of Pre-existing Mental Disorders during the COVID-19 Pandemic: A Canadian Multisite Study: Nouveaux symptômes psychiatriques émergents et détérioration des troubles mentaux préexistants pendanturant la pandémie de la COVID-19: Une étude canadienne multisite. Can. J. Psychiatry 2021, 66, 815–826. [Google Scholar]
- META (mHealth: Ethical, Legal and Social Aspects in the Technological Age.) AI. Available online: https://about-mhealth.net/about-mhealth/what-is-mhealth/ (accessed on 10 April 2021).
- Engel, S.; Schumacher, S.; Niemeyer, H.; Kuester, A.; Burchert, S.; Klusmann, H.; Rau, H.; Willmund, G.-D.; Knaevelsrud, C. Associations between oxytocin and vasopressin concentrations, traumatic event exposure and posttraumatic stress disorder symptoms: Group comparisons, correlations, and courses during an internet-based cognitive-behavioural treatment. Eur. J. Psychotraumatol. 2021, 12. [Google Scholar] [CrossRef]
- Spence, J.; Titov, N.; Johnston, L.; Dear, B.F.; Wootton, B.; Terides, M.; Zou, J. Internet-delivered eye movement desensitization and reprocessing (iEMDR): An open trial. F1000Research 2013, 2, 79. [Google Scholar] [CrossRef] [PubMed]
- Lenferink, L.I.M.; Meyerbröker, K.; Boelen, P.A. PTSD treatment in times of COVID-19: A systematic review of the effects of online EMDR. Psychiatry Res. 2020, 293, 113438. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Kilpatrick, D.G.; Calhoun, K.S. Early behavorial treatment for rape trauma: Efficacy or artifact? Behav. Ther. 1988, 19, 421–427. [Google Scholar] [CrossRef]
- Echeburúa, E.; Corral, P.; Zubizarreta, I.; Sarasua, B. Tratamiento Psicológico del Estrés Postraumático Crónico en Víctimas de Agresiones Sexuales; Fundación Paidela: La Coruña, Spain, 1995. [Google Scholar]
- Diener, E.; Emmons, R.A.; Larsem, R.J.; Griffin, S. The Satisfaction with Life Scale. J. Pers. Assess 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Pavot, W.; Diener, E. Review of the Satisfaction with Life Scale. In Assessing Well-Being; Social Indicators Research Series; Diener, E., Ed.; Springer: Dordrecht, Spain, 2009; Volume 39. [Google Scholar] [CrossRef]
- Rosenberg, M. La Autoimagen del Adolescente y la Sociedad; traducción de 1973; Paidós: Buenos Aires, Argentina, 1965. [Google Scholar]
- Atienza, F.L.; Pons, D.; Balaguer, I.; García-Merita, M. Psychometric properties of the satisfaction with life scale in adolescents|[Propiedades Psicométricas de la Escala de Satisfacción con la VIDA en Adolescentes]. Psicothema 2000, 12, 314–319. [Google Scholar]
- Arboleda, M.; Cantón-Cortés, D.; Cantón, J. Consecuencias a largo plazo del abuso sexual infantil: Papel de la naturaleza y continuidad del abuso y del ambiente familiar. Psicol. Conduct. 2011, 10, 41–56. Available online: https://www.proquest.com/scholarly-journals/consecuencias-largo-plazo-del-abuso-sexual/docview/927743565/se-2?accountid=14777 (accessed on 30 March 2022).
- Supple, A.J.; Su, J.; Plunkett, S.W.; Peterson, G.W.; Bush, K.R. Factor Structure of the Rosenberg Self-Esteem Scale. J. Cross-Cult. Psychol. 2013, 44, 748–764. [Google Scholar] [CrossRef]
- Cong, C.W.; Cheong, J.Y. Validation of Rosenberg self-esteem scale for Malaysian adolescents. Curr. Psychol. 2022. [Google Scholar] [CrossRef]
- Mayordomo, T.; Gutierrez, M.; Sales, A. Adapting and validating the Rosenberg Self-Esteem Scale for elderly Spanish population. Int. Psychogeriatr. 2019, 32, 183–190. [Google Scholar] [CrossRef]
- Fernández-Montalvo, A.; Echeburúa, E. Manual práctico del juego patológico. In Ayuda Para el Paciente y Guía Para el Terapeuta; Pirámide: Madrid, Spain, 1997. [Google Scholar]
- Morejón, A.J.V.; García-Bóveda, R.J.; Jiménez, R.V.-M. Escala de autoestima de Rosenberg: Fiabilidad y validez en población clínica española. Apuntes de psicología 2012, 22, 247–255. Available online: https://www.apuntesdepsicologia.es/index.php/revista/article/view/53 (accessed on 30 March 2022).
- Derogatis, L.R.; Yevzeroff, H.; Wittelsberger, B. Social class, psychological disorder, and the nature of the psychopathologic indicator. J. Consult. Clin. Psychol. 1975, 43, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Hildenbrand, A.K.; Nicholls, E.G.; Aggarwal, R.; Brody-Bizar, E.; Daly, B.P. Symptom Checklist-90-Revised (SCL-90-R). Corsini Encycl. Psychol. 2015. [Google Scholar]
- Fernández, I.G.; de Miguel, C.L.; Pérez, C.G.; Fernández, C.G.; Fernández, J.G. Diagnósticos psiquiátricos prevalentes a consecuencia del abuso sexual durante la infancia y la adolescencia. Rev. Enferm. Salud Ment. 2019, 12, 13–20. [Google Scholar]
- de Rivera, J.L.G.; De las Cuevas, C.; Rodríguez, M.; Rodríguez, F. Cuestionario de 90 Síntomas SCL-90-R de Derogatis, L. Adaptación Española; TEA Ediciones: Madrid, Spain, 2002. [Google Scholar]
- Echeburúa, E.; Amor, P.J.; Sarasua, B.; Zubizarreta, I.; Holgado-Tello, F.P.; Muñoz, J.M. Posttraumatic stress disorder symptom severity scale-revised (EGS-R) according to DSM-5 criteria: Psychometric properties. Ter. Psicol. 2016, 34, 111–128. [Google Scholar] [CrossRef] [Green Version]
- Robinaugh, D.J.; McNally, R.J. Trauma centrality and PTSD symptom severity in adult survivors of childhood sexual abuse. J. Trauma. Stress 2011, 24, 483–486. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Fillol, C.; Perez-Garcia, M.; Karatzias, T.; Hidalgo, N. Concordance between Two PTSD Instruments in a Spanish Sample of Women Survivors of Intimate Partner Violence. In Proceedings of the 2nd International Trauma Informed Care Online Conference: Interventions to Reduce Core and Comorbid Trauma Symptoms, Online, 9 November 2021. [Google Scholar] [CrossRef]
- Krueger, R.F.; Derringer, J.; Markon, K.E.; Watson, D.; Skodol, A.E. Erratum: Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychol. Med. 2012, 42, 1891. [Google Scholar] [CrossRef] [Green Version]
- Tong, L.; Oates, K.; McDowell, M. Personality development following sexual abuse. Child Abus. Negl. 1987, 11, 371–383. [Google Scholar] [CrossRef]
- Walker, H.E.; Freud, J.S.; Ellis, R.A.; Fraine, S.M.; Wilson, L.C. The prevalence of sexual revictimization: A meta-analytic review. Trauma Violence Abus. 2017, 20, 67–80. [Google Scholar] [CrossRef]
- Gutiérrez, F.; Aluja, A.; Peri, J.M.; Calvo, N.; Ferrer, M.; Baillés, E.; Gutiérrez-Zotes, J.A.; Gárriz, M.; Caseras, X.; Markon, K.E.; et al. Psychometric Properties of the Spanish PID-5 in a Clinical and a Community Sample. Assessment 2017, 24, 326–336. [Google Scholar] [CrossRef]
- Gratz, K.L.; Roemer, L. Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Tull, M.; Vidaña, A.; Betts, J. Emotion regulation difficulties in PTSD. In Emotion in Posttraumatic Stress Disorder; Tull, M.T., Kimbrel, N.A., Eds.; Academic Press: Cambridge, MA, USA, 2020; pp. 295–310. [Google Scholar]
- Hervás, G.; Jódar, R. Adaptación al castellano de la Escala de Dificultades en la Regulación Emocional. Clínica y Salud 2008, 19, 139–156. Available online: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1130-52742008000200001&lng=es (accessed on 30 March 2022).
- Bernstein, E.M.; Putnam, F.W. Development, reliability, and validity of a dissociation scale. J. Nerv. Ment. Dis. 1986, 174, 727–735. [Google Scholar] [CrossRef]
- Messman-Moore, T.L.; Long, P.J. The role of childhood sexual abuse sequelae in the sexual revictimization of women: An empirical review and theoretical reformulation. Clin. Psychol. Rev. 2013, 23, 537–557. [Google Scholar] [CrossRef]
- Icaran, E.; Colom, R.; Orengo-Garcia, F. Validation study of the dissociative experiences scale with a Spanish population sample.|[Estudio de validación de la escala de experiencias disociativas con muestra de población española]. Actas Esp. Psiquiatr. 1996, 24, 7–10. [Google Scholar]
- Feixas, G.; Pucurull, O.; Roca, C.; Paz, C.; García, E.; Bados, A. Escala de satisfacción con el tratamiento recibido (CRES-4): La versión en español. Revista de Psicoterapia 2012, 23, 51–58. [Google Scholar] [CrossRef]
- Nielsen, S.L.; Smart, D.W.; Isakson, R.L.; Worthen, V.E.; Gregersen, A.T.; Lambert, M.J. The consumer reports effectiveness score: What did consumers report? J. Couns. Psychol. 2004, 51, 25–37. [Google Scholar] [CrossRef]
- Cohen, J.A.; Mannarino, A.P.; Kliethermes, M.; Murray, L.A. Trauma-focused CBT for youth with complex trauma. Child Abus. Negl. 2012, 36, 528–541. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J.; Mannarino, A.; Deblinger, E. Treating Trauma and Traumatic Grief in Children and Adolescents; Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- Artigas, L.; Jarero, I.; Mauer, M.; Cano, T.L.; Alcalá, N. EMDR and traumatic stress after natural disasters: Integrative Treatment protocol and the Butterfly Hug. In Proceedings of the conference EMDRIA, Toronto, ON, Canada; 2000. [Google Scholar]
- Jarero, I.; Artigas, L. The EMDR integrative group treatment protocol: EMDR group treatment for early intervention following critical incidents. Rev. Eur. Psychol. Appl. 2012, 62, 219–222. [Google Scholar] [CrossRef]
- Shapiro, E. The Group Traumatic Episode Protocol (G-TEP) for Early EMDR Intervention (EEI). In Proceedings of the EMDR Symposium, Istanbul, Turkey, 28 November 2013. Unpublished Conference Paper. [Google Scholar]
- Jarero, I.; Artigas, L.; Protocolo para Estabilización en Síndrome de Estrés Agudo (PESEA). Individual, Grupal y a Distancia. In Proceedings of the National EMDR Association Conference, Madrid, Spain, 21 April 2018. [Google Scholar]
- Haoa, F.; Tanb, W.; Jianga, L.; Zhanga, L.; Zhaoa, X.; Zoua, Y.; Hua, Y.; Luoa, X.; Jiangd, X.; McIntyree, R.S.; et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020, 87, 100–106. [Google Scholar] [CrossRef]
- Naslund, J.A.; Habc, M.P.; Aschbrenner, K.A.; Araya, R.; Marsch, L.; Unützer, J.; Pate, V.; Stephen, S.; Bartels, J.; Dabd, M. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: A narrative review of the literature. Lancet Psychiatry 2017, 4, 486–500. [Google Scholar] [CrossRef] [Green Version]
| STUDY PERIOD | |||||||
|---|---|---|---|---|---|---|---|
| Enrolment | Allocation | Post-Allocation | Close-Out | ||||
| TIMEPOINT * | −t1 | 0 | t1 | t2 | t3 | t4 | |
| ENROLMENT: | X | ||||||
| Eligibilityscreen | X | ||||||
| Informedconsent | X | ||||||
| Filling thequestionnaires | |||||||
| Allocation | X | ||||||
| INTERVENTIONS: | |||||||
| EMDR + TF-CBT |  | X | X | ||||
| TF-CBT + EMDR |  | X | X | ||||
| ASSESSMENTS: | |||||||
| Satisfaction with life scale (SWLS) | X | X | X | X | |||
| Rosenberg Self-Esteem Scale(RSE) | X | X | X | X | |||
| Symptom Checklist-90-Revised (SCL-R) | X | X | X | X | |||
| Post-traumatic Stress Disorder Symptom Severity Scale according totheDSM-5(EGS-R) | X | X | X | X | |||
| DSM-5 Personality Inventory—Brief Version (PID-5-BF)Adults | X | X | |||||
| Scale of emotional regulation difficulties (DERS) | X | X | X | X | |||
| Dissociative Symptom Scale (DES) | X | X | X | X | |||
| Scale of satisfaction with the treatment received. (CRES-4) | X | X | |||||
| Ad-hoc registry for general sociodemographic and clinicalvariables | X | ||||||
| Treatment Protocols | |
|---|---|
| Trauma-Focused CBT-based treatment Adaptation of the protocol of Cohen for complex trauma. TF-CBT is an evidence-based therapeutic approach for treating traumatized patients. Generate an improvement of symptoms of PTSD, dissociative, affective, or cognitive and behavioral problems. Eight weekly one-hour online group sessions per week Three phases of 2–3 sessions each. Phase 1: TF-CBT Coping Skills for Complex Traumas. Objectives: Establishing a trusting relationship and self-regulation skills; reinforcing safety; psychoeducation; relaxation skills, mindfulness affective and cognitive coping. Phase 2: Trauma Narration and Complicated Trauma Processing. Objectives: The development of the trauma narrative; identify and examine the impact of core beliefs; development of a hierarchy of feared stimuli and a gradual exposure schedule. Live exposure to trauma memories. Phase 3: Consolidation and completion of treatment. Objectives: After processing the trauma, share the individual progress achieved with others; follow-up sessions; ensure safety and develop appropriate relationships in real-life situations. | Trauma-Focused EMDR treatment Adaptation of Jarero and Artigas’s EMDR group therapy protocol (EMDR-IGTP) and Elan Shapiro’s Traumatic Event Protocol (G-TEP) for complex trauma. EMDR is an evidence-based therapeutic approach for treating traumatized patients. Generate an improvement in PTSD symptoms, dissociative, affective, or cognitive and behavioral problems. Eight weekly one-hour online group sessions per week Eight-phase EMDR protocol. Phases 3 to 7 will be conducted during sessions 3 to 8. Phase 1: Objective: Client history before session 1. Phase 2: Objectives: Preparation for the treatment of the traumatic event, with psychoeducation and regulation strategies, calming place, and setting up positive feelings with EBL. Phases 3–6: Objectives: performed following the G-TEP worksheet. Sense of security (safe place, past resource, desired future-PC, timeline) control structure, order, differentiation of past and present. Phase 7: Closing of the session. Objectives: A group debriefing of the experience and conducting some of the stabilization exercises. Phase 8: Objectives: Re-evaluation. After the group intervention, assess any need for individual attention. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Molero-Zafra, M.; Mitjans-Lafont, M.T.; Hernández-Jiménez, M.J.; Pérez-Marín, M. Psychological Intervention in Women Victims of Childhood Sexual Abuse: An Open Study—Protocol of a Randomized Controlled Clinical Trial Comparing EMDR Psychotherapy and Trauma-Based Cognitive Therapy. Int. J. Environ. Res. Public Health 2022, 19, 7468. https://doi.org/10.3390/ijerph19127468
Molero-Zafra M, Mitjans-Lafont MT, Hernández-Jiménez MJ, Pérez-Marín M. Psychological Intervention in Women Victims of Childhood Sexual Abuse: An Open Study—Protocol of a Randomized Controlled Clinical Trial Comparing EMDR Psychotherapy and Trauma-Based Cognitive Therapy. International Journal of Environmental Research and Public Health. 2022; 19(12):7468. https://doi.org/10.3390/ijerph19127468
Chicago/Turabian StyleMolero-Zafra, Milagros, María Teresa Mitjans-Lafont, María Jesús Hernández-Jiménez, and Marián Pérez-Marín. 2022. "Psychological Intervention in Women Victims of Childhood Sexual Abuse: An Open Study—Protocol of a Randomized Controlled Clinical Trial Comparing EMDR Psychotherapy and Trauma-Based Cognitive Therapy" International Journal of Environmental Research and Public Health 19, no. 12: 7468. https://doi.org/10.3390/ijerph19127468
APA StyleMolero-Zafra, M., Mitjans-Lafont, M. T., Hernández-Jiménez, M. J., & Pérez-Marín, M. (2022). Psychological Intervention in Women Victims of Childhood Sexual Abuse: An Open Study—Protocol of a Randomized Controlled Clinical Trial Comparing EMDR Psychotherapy and Trauma-Based Cognitive Therapy. International Journal of Environmental Research and Public Health, 19(12), 7468. https://doi.org/10.3390/ijerph19127468







