Association of Air Pollution and Weather Factors with Traffic Injury Severity: A Study in Taiwan
Abstract
:1. Introduction
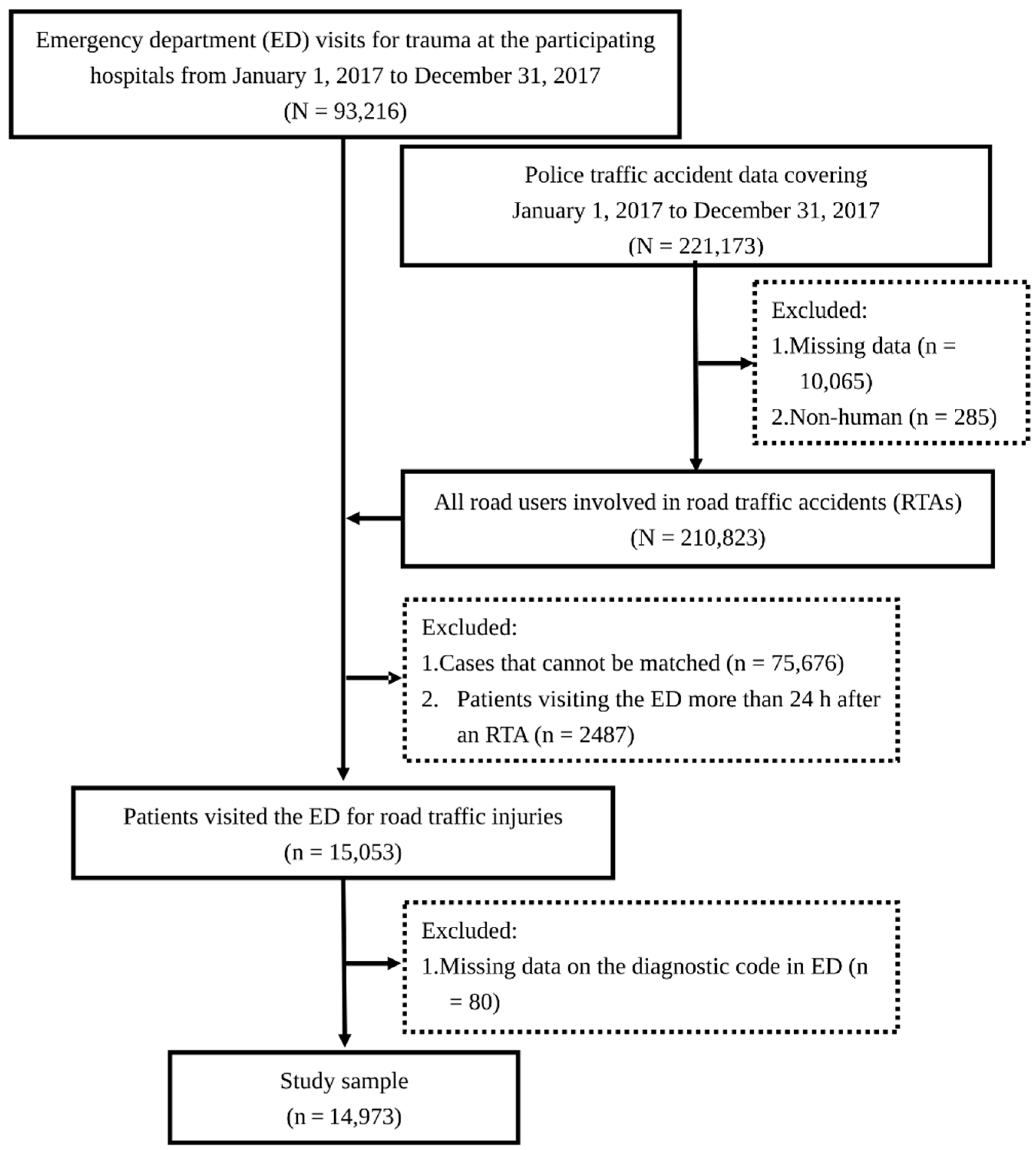
2. Materials and Methods
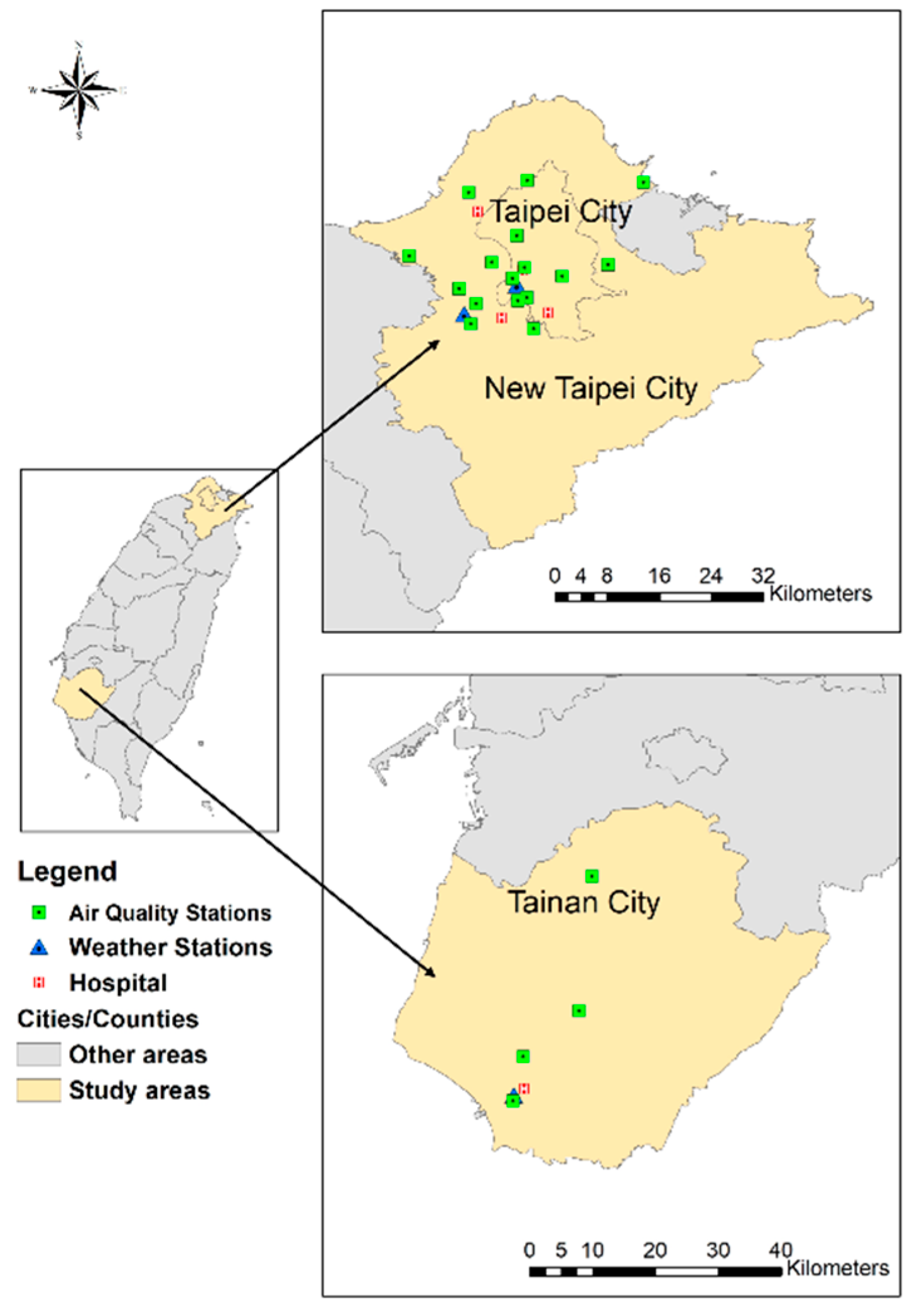
2.1. Study Design
2.2. Measurements
2.3. Outcome
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anderson, J.O.; Thundiyil, J.G.; Stolbach, A. Clearing the air: A review of the effects of particulate matter air pollution on human health. J. Med. Toxicol. 2012, 8, 166–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, S.; Zhang, J.; Zeng, X.; Zeng, Y.; Wang, S.; Chen, S. Association of traffic-related air pollution with children’s neurobehavioral functions in Quanzhou, China. Environ. Health Perspect. 2009, 117, 1612–1618. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lavy, V.; Ebenstein, A.; Roth, S. The Impact of Short Term Exposure to Ambient Air Pollution on Cognitive Performance and Human Capital Formation; NBER Working Paper No. 20648; National Bureau of Economic Research: Cambridge, MA, USA, 2014. [Google Scholar] [CrossRef]
- Amanzadeh, N.; Vesal, M.; Ardestani, S.F.F. The impact of short-term exposure to ambient air pollution on test scores in Iran. Popul. Environ. 2020, 41, 253–285. [Google Scholar] [CrossRef]
- Burkhardt, J.; Bayham, J.; Wilson, A.; Carter, E.; Berman, J.D.; O’Dell, K.; Ford, B.; Fischer, E.V.; Pierce, J.R. The effect of pollution on crime: Evidence from data on particulate matter and ozone. J. Environ. Econ. Manag. 2019, 98, 102267. [Google Scholar] [CrossRef]
- Berman, J.D.; Burkhardt, J.; Bayham, J.; Carter, E.; Wilson, A. Acute air pollution exposure and the risk of violent behavior in the United States. Epidemiology 2019, 30, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.R.; Schelegle, E.S.; Miller, L.A.; Hyde, D.M.; Van Winkle, L.S. Ozone exposure alters serotonin and serotonin receptor expression in the developing lung. Toxicol. Sci. 2013, 134, 168–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H.; Cai, J.; Chen, R.; Zhao, Z.; Ying, Z.; Wang, L.; Chen, J.; Hao, K.; Kinney, P.L.; Chen, H.; et al. Particulate matter exposure and stress hormone levels: A randomized, double-blind, crossover trial of air purification. Circulation 2017, 136, 618–627. [Google Scholar] [CrossRef]
- Hammad, H.M.; Ashraf, M.; Abbas, F.; Bakhat, H.F.; Qaisrani, S.A.; Mubeen, M.; Fahad, S.; Awais, M. Environmental factors affecting the frequency of road traffic accidents: A case study of sub-urban area of Pakistan. Environ. Sci. Pollut. Res. Int. 2019, 26, 11674–11685. [Google Scholar] [CrossRef]
- Global Status Report on Road Safety. 2018. Available online: https://www.who.int/violence_injury_prevention/road_safety_status/2018/en/ (accessed on 9 May 2022).
- Tamakloe, R.; Das, S.; Aidoo, E.N.; Park, D. Factors affecting motorcycle crash casualty severity at signalized and non-signalized intersections in Ghana: Insights from a data mining and binary logit regression approach. Accid. Anal. Prev. 2022, 165, 106517. [Google Scholar] [CrossRef]
- Zhang, W.; Wang, C.; Chen, Q.; Liu, J.; Feng, Z.; Wang, K.; Shen, Y. Lane-change behavior in low illumination: Research based on a questionnaire investigation. J. Transp. Saf. Secur. 2022, 14, 130–151. [Google Scholar] [CrossRef]
- Se, C.; Champahom, T.; Jomnonkwao, S.; Chaimuang, P.; Ratanavaraha, V. Empirical comparison of the effects of urban and rural crashes on motorcyclist injury severities: A correlated random parameters ordered probit approach with heterogeneity in means. Accid. Anal. Prev. 2021, 161, 106352. [Google Scholar] [CrossRef] [PubMed]
- Cheng, W.; Gill, G.S.; Sakrani, T.; Dasu, M.; Zhou, J. Predicting motorcycle crash injury severity using weather data and alternative Bayesian multivariate crash frequency models. Accid. Anal. Prev. 2017, 108, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Lio, C.F.; Cheong, H.H.; Un, C.H.; Lo, I.L.; Tsai, S.Y. The association between meteorological variables and road traffic injuries: A study from Macao. PeerJ 2019, 7, e6438. [Google Scholar] [CrossRef] [PubMed]
- Liang, M.; Zhao, D.; Wu, Y.; Ye, P.; Wang, Y.; Yao, Z.; Bi, P.; Duan, L.; Sun, Y. Short-term effects of ambient temperature and road traffic accident injuries in Dalian, Northern China: A distributed lag non-linear analysis. Accid. Anal. Prev. 2021, 153, 106057. [Google Scholar] [CrossRef]
- Ghada, W.; Estrella, N.; Ankerst, D.P.; Menzel, A. Universal thermal climate index associations with mortality, hospital admissions, and road accidents in Bavaria. PLoS ONE 2021, 16, e0259086. [Google Scholar] [CrossRef]
- Kim, Y.M.; Yu, G.G.; Shin, H.J.; Lee, S.W.; Park, J.; Kim, H. Effect of regional climatic conditions, air pollutants, and season on the occurrence and severity of injury in trauma patients. J. Korean Soc. Emerg. Med. 2018, 29, 603–615. [Google Scholar]
- Ha, K.H.; Cho, J.; Cho, S.K.; Kim, C.; Shin, D.C. Air pollution and unintentional injury deaths in South Korea. Environ. Sci. Pollut. Res. Int. 2015, 22, 7873–7881. [Google Scholar] [CrossRef]
- Sager, L. Estimating the effect of air pollution on road safety using atmospheric temperature inversions. J. Environ. Econ. Manag. 2019, 98, 102250. [Google Scholar] [CrossRef]
- Dastoorpoor, M.; Idani, E.; Khanjani, N.; Goudarzi, G.; Bahrampour, A. Relationship between air pollution, weather, traffic, and traffic-related mortality. Trauma Mon. 2016, 21, e37585. [Google Scholar] [CrossRef] [Green Version]
- Ahmadi, M.; Khorsandi, B.; Mesbah, M. The effect of air pollution on drivers’ safety performance. Environ. Sci. Pollut. Res. Int. 2021, 28, 15768–15781. [Google Scholar] [CrossRef]
- The Annual Report of Air Pollution Control in Taiwan (R.O.C.) in 2019. Available online: https://www.epa.gov.tw/ (accessed on 7 June 2022). (In Chinese)
- Motor Vehicle Registration. Available online: https://stat.thb.gov.tw/hb01/webMain.aspx?sys=100&funid=11100 (accessed on 7 June 2022). (In Chinese)
- Alonso, F.; Useche, S.A.; Faus, M.; Esteban, C. Does urban security modulate transportation choices and travel behavior of citizens? A national study in the Dominican Republic. Front. Sustain. Cities 2020, 2, 42. [Google Scholar] [CrossRef]
- Chang, H.L.; Lai, C.Y. Using travel socialization and underlying motivations to better understand motorcycle usage in Taiwan. Accid. Anal. Prev. 2015, 79, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Jing Chuan Child Safety Foundation. Available online: https://www.safe.org.tw/key_report/research_detail/90?key_id=648 (accessed on 7 June 2022). (In Chinese).
- Traffic Accidents (30 Days). Available online: https://stat.motc.gov.tw/mocdb/stmain.jsp?sys=100&funid=defjsp (accessed on 7 June 2022). (In Chinese)
- Rivas, I.; Basagaña, X.; Cirach, M.; López-Vicente, M.; Suades-González, E.; Garcia-Esteban, R.; Álvarez-Pedrerol, M.; Dadvand, P.; Sunyer, J. Association between early life exposure to air pollution and working memory and attention. Environ. Health Perspect. 2019, 127, 57002. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Guo, Y.; Zheng, Y.; Zhao, X.; Cao, Z.; Rigdon, S.E.; Xian, H.; Li, X.; Liu, T.; Xiao, J.; et al. Exposure to ambient PM2.5 associated with overall and domain-specific disability among adults in six low- and middle-income countries. Environ. Int. 2017, 104, 69–75. [Google Scholar] [CrossRef]
- Bilal, M.; Hassan, M.; Tahir, D.B.T.; Iqbal, M.S. Understanding the role of atmospheric circulations and dispersion of air pollution associated with extreme smog events over South Asian megacity. Environ. Monit. Assess 2022, 194, 82. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.; Li, Y.H.; Liu, H.C.; Li, Z. Is traffic accident related to air pollution? A case report from an island of Taihu Lake, China. Atmos. Pollut. Res. 2020, 11, 1028–1033. [Google Scholar] [CrossRef]
- Badach, J.; Dymnicka, M.; Baranowski, A. Urban vegetation in air quality management: A review and policy framework. Sustainability 2020, 12, 1258. [Google Scholar] [CrossRef] [Green Version]
- United Nations Development Programme. Available online: https://www.undp.org/sustainable-development-goals (accessed on 7 June 2022).
- Cheng, W.L.; Chen, Y.S.; Zhang, J.; Lyons, T.J.; Pai, J.L.; Chang, S.H. Comparison of the Revised Air Quality Index with the PSI and AQI indices. Sci. Total Environ. 2007, 382, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Taiwan Air Quality Monitoring Network. Available online: https://airtw.epa.gov.tw/cht/Information/Standard/AirQualityIndicator.aspx (accessed on 9 May 2022). (In Chinese)
- Google Maps Platform. Available online: https://cloud.google.com/maps-platform/ (accessed on 9 May 2022).
- Taiwan Geospatial One-Stop Portal. Available online: https://www.tgos.tw/TGOS/Web/TGOS_Home.aspx (accessed on 9 May 2022). (In Chinese).
- Environmental Information Open Platform. Available online: https://data.epa.gov.tw/ (accessed on 9 May 2022). (In Chinese)
- Open Weather Data. Available online: https://opendata.cwb.gov.tw/dataset/observation?page=1 (accessed on 9 May 2022). (In Chinese)
- Clark, D.E.; Black, A.W.; Skavdahl, D.H.; Hallagan, L.D. Open-access programs for injury categorization using ICD-9 or ICD-10. Inj. Epidemiol. 2018, 5, 11. [Google Scholar] [CrossRef] [Green Version]
- Establishment and Application of Traffic Accident Injury Data Collection System (2/2). Available online: https://www.iot.gov.tw/cp-78-12430-1759c-1.html (accessed on 9 May 2022). (In Chinese)
- Palmer, C. Major trauma and the injury severity score—Where should we set the bar? Annu. Proc. Assoc. Adv. Automot. Med. 2007, 51, 13–29. [Google Scholar] [CrossRef]
- Atkinson, T.; Gawarecki, L.; Tavakoli, M. Paired vehicle occupant analysis indicates age and crash severity moderate likelihood of higher severity injury in second row seated adults in frontal crashes. Accid. Anal. Prev. 2016, 89, 88–94. [Google Scholar] [CrossRef]
- Lam, C.; Pai, C.W.; Chuang, C.C.; Yen, Y.C.; Wu, C.C.; Yu, S.H.; Hung, K.S.; Chiu, W.T. Rider factors associated with severe injury after a light motorcycle crash: A multicentre study in an emerging economy setting. PLoS ONE 2019, 14, e0219132. [Google Scholar] [CrossRef] [PubMed]
- Mickey, R.M.; Greenland, S. The impact of confounder selection criteria on effect estimation. Am. J. Epidemiol. 1989, 129, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Olson, C.J.; Brand, D.; Mullins, R.J.; Harrahill, M.; Trunkey, D.D. Time to death of hospitalized injured patients as a measure of quality of care. J. Trauma 2003, 55, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Pal, J.; Brown, R.; Fleiszer, D. The value of the Glasgow Coma Scale and Injury Severity Score: Predicting outcome in multiple trauma patients with head injury. J. Trauma 1989, 29, 746–748. [Google Scholar] [CrossRef] [PubMed]
- Wiratama, B.S.; Chen, P.L.; Ma, S.T.; Chen, Y.H.; Saleh, W.; Lin, H.A.; Pai, C.W. Evaluating the combined effect of alcohol-involved and un-helmeted riding on motorcyclist fatalities in Taiwan. Accid. Anal. Prev. 2020, 143, 105594. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.L.; Pai, C.W. Evaluation of injuries sustained by motorcyclists in approach-turn crashes in Taiwan. Accid. Anal. Prev. 2019, 124, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Cepeda, M.; Schoufour, J.; Freak-Poli, R.; Koolhaas, C.M.; Dhana, K.; Bramer, W.M.; Franco, O.H. Levels of ambient air pollution according to mode of transport: A systematic review. Lancet Public Health 2017, 2, E23–E34. [Google Scholar] [CrossRef] [Green Version]
- Bourdrel, T.; Bind, M.A.; Béjot, Y.; Morel, O.; Argacha, J.F. Cardiovascular effects of air pollution. Arch. Cardiovasc. Dis. 2017, 110, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Block, M.L.; Elder, A.; Auten, R.L.; Bilbo, S.D.; Chen, H.; Chen, J.C.; Cory-Slechta, D.A.; Costa, D.; Diaz-Sanchez, D.; Dorman, D.C.; et al. The outdoor air pollution and brain health workshop. Neurotoxicology 2012, 33, 972–984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Han, S.; Bian, H.; Feng, Y.; Liu, A.; Li, X.; Zeng, F.; Zhang, X. Analysis of the relationship between O3, NO and NO2 in Tianjin, China. Aerosol. Air Qual. Res. 2011, 11, 128–139. [Google Scholar] [CrossRef] [Green Version]
- Diener, A.; Mudu, P. How can vegetation protect us from air pollution? A critical review on green spaces mitigation abilities for air-borne particles from a public health perspective—With implications for urban planning. Sci. Total Environ. 2021, 796, 148605. [Google Scholar] [CrossRef]
- Lei, Y.; Davies, G.M.; Jin, H.; Tian, G.; Kim, G. Scale-dependent effects of urban greenspace on particulate matter air pollution. Urban For. Urban Green. 2021, 61, 127089. [Google Scholar] [CrossRef]
- Pai, C.W.; Lin, H.Y.; Tsai, S.H.; Chen, P.L. Comparison of traffic-injury related hospitalization between bicyclists and motorcyclists in Taiwan. PLoS ONE 2018, 13, e0191221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Otte im Kampe, E.; Kovats, S.; Hajat, S. Impact of high ambient temperature on unintentional injuries in high-income countries: A narrative systematic literature review. BMJ Open 2016, 6, e010399. [Google Scholar] [CrossRef] [Green Version]
- Xing, F.; Huang, H.; Zhan, Z.Y.; Zhai, X.; Ou, C.; Sze, N.N.; Hon, K.K. Hourly associations between weather factors and traffic crashes: Non-linear and lag effects. Anal. Methods Accid. Res. 2019, 24, 100109. [Google Scholar] [CrossRef]
- Naik, B.; Tung, L.W.; Zhao, S.; Khattak, A.J. Weather impacts on single-vehicle truck crash injury severity. J. Saf. Res. 2016, 58, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Zhai, X.; Huang, H.; Sze, N.N.; Song, Z.Q.; Hon, K.K. Diagnostic analysis of the effects of weather condition on pedestrian crash severity. Accid. Anal. Prev. 2019, 122, 318–324. [Google Scholar] [CrossRef]
- Ackaah, W.; Apuseyine, B.A.; Afukaar, F.K. Road traffic crashes at nighttime: Characteristics and risk factors. Int. J. Inj. Contr. Saf. Promot. 2020, 27, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Plainis, S.; Murray, I.J.; Pallikaris, I.G. Road traffic casualties: Understanding the nighttime death toll. Inj. Prev. 2016, 12, 125–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roy, S.; Hawlader, M.D.H.; Nabi, M.H.; Chakraborty, P.A.; Zaman, S.; Alam, M.M. Patterns of injuries and injury severity among hospitalized road traffic injury (RTI) patients in Bangladesh. Heliyon 2021, 7, e06440. [Google Scholar] [CrossRef]
- Azami-Aghdash, S.; Aghaei, M.H.; Sadeghi-Bazarghani, H. Epidemiology of road traffic injuries among elderly people; A systematic review and meta-analysis. Bull. Emerg. Trauma 2018, 6, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Ang, B.H.; Chen, W.S.; Lee, S.W.H. Global burden of road traffic accidents in older adults: A systematic review and meta-regression analysis. Arch. Gerontol. Geriatr. 2017, 72, 32–38. [Google Scholar] [CrossRef] [PubMed]
| Variables | ISS < 9 (n = 12,120) | ISS ≥ 9 (n = 2853) | p Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Sex | 0.26 a | ||
| Male | 6591 (89.61) | 1585 (19.39) | |
| Female | 5529 (81.34) | 1268 (18.66) | |
| Age (year) median (IQR) | 30 (27) | 36 (34) | <0.001 b |
| Age group (year) | <0.001 c | ||
| <24 | 4541 (82.80) | 943 (17.20) | |
| 25–44 | 4037 (83.31) | 809 (16.69) | |
| 45–64 | 2596 (77.86) | 738 (22.14) | |
| >64 | 946 (72.27) | 363 (22.73) | |
| GCS median (IQR) | 15 (0) | 15 (0) | <0.001 b |
| Scene-to-hospital arrival time (min) median (IQR) | 35 (42) | 31 (18) | <0.001 b |
| Day of crash | 0.42 a | ||
| Weekday | 8910 (81.10) | 2076 (18.90) | |
| Weekend | 3210 (80.51) | 777 (19.49) | |
| Time of crash (time of day) | <0.001 a | ||
| Day (06:00–17:59) | 8040 (81.03) | 1882 (18.97) | |
| Evening (18:00–23:59) | 3364 (81.77) | 750 (18.23) | |
| Night (00:00–05:59) | 716 (76.41) | 221 (23.59) | |
| Time of crash (rush hour) | 0.93 a | ||
| 07:00–09:00 | 1741 (80.83) | 413 (19.17) | |
| 17:00–19:00 | 1647 (80.70) | 394 (19.30) | |
| Nonrush hours | 8732 (81.02) | 2046 (18.98) | |
| Type of road user | <0.001 a | ||
| Auto occupant | 866 (95.37) | 42 (4.63) | |
| Motorcyclist | 10,117 (80.95) | 2381 (19.05) | |
| Bicyclist | 364 (71.79) | 143 (28.21) | |
| Pedestrian | 771 (73.08) | 284 (26.92) | |
| Missing d | 2 (0.02) | 3 (0.11) | |
| Road width (m) median (IQR) | 10 (10) | 11 (11) | <0.001 b |
| Missing d | 9 (0.07) | 2 (0.07) | |
| 24-h accumulated precipitation (mm) Median (IQR) | 0 (2.5) | 0 (2) | 0.008 b |
| Heavy rain | 0.64 a | ||
| No (<80 mm) | 12,006 (80.97) | 2821 (19.03) | |
| Yes (≥80 mm) | 112 (79.43) | 29 (20.57) | |
| Missing data d | 2 (0.02) | 3 (0.11) | |
| Temperature (℃) median (IQR) | 25 (10) | 26 (10) | 0.006 b |
| Relative humidity (%) median (IQR) | 71 (15) | 71 (15) | 0.010 b |
| AQI median (IQR) | 51 (38) | 53.5 (43) | <0.001 b |
| AQI level | <0.001 c | ||
| Good (0–50) | 5698 (82.04) | 1247 (17.96) | |
| Moderate (51–100) | 4845 (81.10) | 1129 (18.90) | |
| Unhealthy (>100) | 1117 (75.83) | 356 (24.17) | |
| Missing data d | 460 (3.80) | 121 (4.24) | |
| PM2.5 (μg/m3) median (IQR) | 16 (15) | 16 (17) | 0.003 b |
| Missing data d | 653 (5.19) | 141 (4.94) | |
| PM10 (μg/m3) median (IQR) | 33 (26) | 35 (28) | <0.001 b |
| Missing data d | 482 (3.98) | 106 (3.79) | |
| NO2 (ppb) median (IQR) | 15 (14.4) | 14 (13.4) | <0.001 b |
| Missing data d | 588 (4.85) | 140 (4.91) | |
| NOx (ppb) median (IQR) | 19 (19) | 16 (18) | <0.001 b |
| Missing data d | 762 (6.29) | 188 (6.59) | |
| O3 (ppb) median (IQR) | 29 (25) | 29 (25.5) | 0.49 b |
| Missing data d | 512 (4.22) | 121 (4.24) |
| Variables | AQI Model | Best-Fit Multiple Air Pollutant Model | ||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Sex | ||||
| Female | Reference | Reference | ||
| Male | 1.102 (1.010–1.202) | 0.028 | 1.108 (1.013–1.211) | 0.025 |
| Age group (year) | ||||
| <24 | Reference | Reference | ||
| 25–44 | 1.023 (0.920–1.139) | 0.67 | 1.046 (0.937–1.168) | 0.42 |
| 45–64 | 1.398 (1.247–1.567) | <0.001 | 1.382 (1.228–1.555) | <0.001 |
| >64 | 1.767 (1.517–2.058) | <0.001 | 1.757 (1.502–2.055) | <0.001 |
| Time of crash | ||||
| Day (06:00–17:59) | Reference | Reference | ||
| Evening (18:00–23:59) | 0.975 (0.882–1.078) | 0.62 | 1.033 (0.932–1.144) | 0.54 |
| Night (00:00–05:59) | 1.491 (1.254–1.774) | <0.001 | 1.400 (1.166–1.680) | <0.001 |
| Scene-to-hospital arrival time (min) | 0.999 (0.998–0.999) | <0.001 | 0.998 (0.998–0.999) | <0.001 |
| Type of road user | ||||
| Motorcyclist | Reference | Reference | ||
| Bicyclist | 1.457 (1.183–1.795) | 0.001 | 1.429 (1.154–1.770) | 0.001 |
| Pedestrian | 1.379 (1.180–1.612) | <0.001 | 1.412 (1.202–1.660) | <0.001 |
| Auto occupant | 0.185 (0.133–0.256) | <0.001 | 0.180 (0.128–0.253) | <0.001 |
| Road width (m) | 1.014 (1.009–1.019) | <0.001 | 1.013 (1.008–1.019) | <0.001 |
| Temperature (°C, per IQR) | 1.238 (1.146–1.338) | <0.001 | 1.165 (1.077–1.262) | <0.001 |
| Relative humidity (%, per IQR) | 1.195 (1.117–1.278) | <0.001 | 1.136 (1.054–1.224) | <0.001 |
| AQI level | ||||
| Good (0–50) | Reference | |||
| Moderate (51–100) | 1.142 (1.040–1.253) | 0.005 | ||
| Unhealthy (>100) | 1.713 (1.486–1.975) | <0.001 | ||
| PM2.5 (μg/m3, per IQR) | 1.279 (1.209–1.353) | <0.001 | ||
| NOx (ppb, per IQR) | 0.743 (0.696–0.794) | <0.001 | ||
| O3 (ppb, per IQR) | 0.838 (0.774–0.906) | <0.001 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, T.-C.; Pai, C.-W.; Wu, C.-C.; Hsu, J.C.; Chen, R.-J.; Chiu, W.-T.; Lam, C. Association of Air Pollution and Weather Factors with Traffic Injury Severity: A Study in Taiwan. Int. J. Environ. Res. Public Health 2022, 19, 7442. https://doi.org/10.3390/ijerph19127442
Chan T-C, Pai C-W, Wu C-C, Hsu JC, Chen R-J, Chiu W-T, Lam C. Association of Air Pollution and Weather Factors with Traffic Injury Severity: A Study in Taiwan. International Journal of Environmental Research and Public Health. 2022; 19(12):7442. https://doi.org/10.3390/ijerph19127442
Chicago/Turabian StyleChan, Ta-Chien, Chih-Wei Pai, Chia-Chieh Wu, Jason C. Hsu, Ray-Jade Chen, Wen-Ta Chiu, and Carlos Lam. 2022. "Association of Air Pollution and Weather Factors with Traffic Injury Severity: A Study in Taiwan" International Journal of Environmental Research and Public Health 19, no. 12: 7442. https://doi.org/10.3390/ijerph19127442
APA StyleChan, T.-C., Pai, C.-W., Wu, C.-C., Hsu, J. C., Chen, R.-J., Chiu, W.-T., & Lam, C. (2022). Association of Air Pollution and Weather Factors with Traffic Injury Severity: A Study in Taiwan. International Journal of Environmental Research and Public Health, 19(12), 7442. https://doi.org/10.3390/ijerph19127442








