Medical Photography Usage Amongst Doctors at a Portuguese Hospital
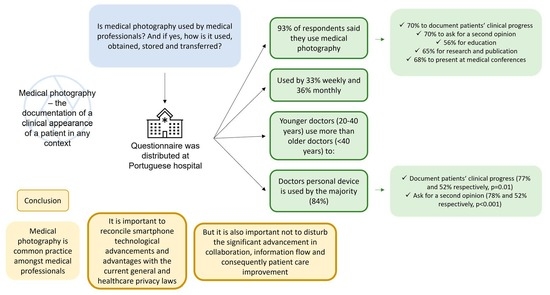
Abstract: Background
1. Background
2. Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Pasquali, P. (Ed.) History of Medical Photography. In Photography in Clinical Medicine, 1st ed.; Springer: Cham, Switzerland, 2020. [Google Scholar]
- Bhattacharya, S. Clinical photography and our responsibilities. Indian J. Plast. Surg. 2014, 47, 277–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freites-Martinez, A.; Hofmann-Wellenhof, R.; Eber, E.L. Smartphones in Medical Photography. In Photography in Clinical Medicine, 1st ed.; Pasquali, P., Ed.; Springer: Cham, Switzerland, 2020. [Google Scholar]
- Nettrour, J.F.; Burch, M.B.; Bal, B.S. Patients, pictures, and privacy: Managing clinical photographs in the smartphone era. Arthroplast. Today 2019, 5, 57–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, M.K.; Howard, D.P.; King, R. “A picture tells a thousand words” smartphone-based secure clinical image transfer improves compliance in open fracture management. Injury 2019, 50, 1284–1287. [Google Scholar] [CrossRef] [PubMed]
- Kameda-Smith, M.M.; Iorio-Morin, C.; Winkler-Schwartz, A.; Ahmed, U.S.; Bergeron, D.; Bigder, M.; Dakson, A.; Elliott, C.A.; Guha, D.; Lavergne, P.; et al. Smartphone Usage Patterns by Canadian Neurosurgery Residents: A National Cross-Sectional Survey. World Neurosurg. 2018, 111, e465–e470. [Google Scholar] [CrossRef]
- Chan, N.; Charette, J.; Dumestre, D.O.; Fraulin, F.O. Should ‘smart phones’ be used for patient photography? Plast. Surg. 2016, 24, 32–34. [Google Scholar] [CrossRef]
- Schaaf, H.; Malik, C.Y.; Howaldt, H.P.; Streckbein, P. Evolution of photography in maxillofacial surgery: From analog to 3D photography—An overview. Clin. Cosmet. Investig. Dent. 2009, 1, 39–45. [Google Scholar] [CrossRef] [Green Version]
- Uzun, M.; Bülbül, M.; Toker, S.; Beksaç, B.; Kara, A. Medical photography: Principles for orthopedics. J. Orthop. Surg. Res. 2014, 9, 23. [Google Scholar] [CrossRef] [Green Version]
- Buabbas, A.J.; Sharma, P.; Al-Abdulrazaq, A.; Shehab, H. Smartphone use by government dermatology practitioners in Kuwait: A self-reported questionnaire based cross-sectional study. BMC Med. Inform. Decis. Mak. 2019, 19, 155. [Google Scholar] [CrossRef] [Green Version]
- Abbott, L.M.; Magnusson, R.S.; Gibbs, E.; Smith, S.D. Smartphone use in dermatology for clinical photography and consultation: Current practice and the law. Australas. J. Dermatol. 2018, 59, 101–107. [Google Scholar] [CrossRef]
- Accetta, P.; Accetta, J.; Kostecki, J. The use of digital cameras by US dermatologists. J. Am. Acad. Dermatol. 2013, 69, 837–838. [Google Scholar] [CrossRef]
- Milam, E.C.; Leger, M.C. Use of medical photography among dermatologists: A nationwide online survey study. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 1804–1809. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.; Yun, D.; Bhatia, A.C.; Hsu, J.T.; Ruiz de Luzuriaga, A.M. Patient perception on the usage of smartphones for medical photography and for reference in dermatology. Dermatol. Surg. 2015, 41, 149–154. [Google Scholar] [CrossRef] [PubMed]
- British Society of Teledermatology tBAoDB; Scottish dermatologists, The British Dermatological Nursing Group (BDNG); The Primary Care Dermatology Society (PCDS). UK Guidance on the Use of Mobile Photographic Devices in Dermatology; The British Dermatological Nursing Group (BDNG): London, UK, 2017. [Google Scholar]
- Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/EC (General Data Protection Regulation) (Text with EEA Relevance); The European Parliament and the Council of the European Union: Brussels, Belgium, 2016.
- Jamil, F. Smartphone photography in oral and maxillofacial surgery. Br. J. Oral Maxillofac. Surg. 2016, 54, 104–105. [Google Scholar] [CrossRef] [PubMed]
- El Hadidy, T.S.; Alshafei, A.E.; Mortell, A.E.; Doherty, E.M. Smartphones in clinical practice: Doctors’ experience at two Dublin paediatric teaching hospitals. Ir. J. Med. Sci. 2018, 187, 565–573. [Google Scholar] [CrossRef]
- Illustrators IoM. Mobile Phone and Mobile Apps for Clinical Photography; Illustrators IoM: Grand-Saconnex, Switzerland, 2019. [Google Scholar]
- Lau, C.K.; Schumacher, H.H.; Irwin, M.S. Patients’ perception of medical photography. J. Plast. Reconstr. Aesthet. Surg. 2010, 63, e507–e511. [Google Scholar] [CrossRef]
- Hacard, F.; Maruani, A.; Delaplace, M.; Caille, A.; Machet, L.; Lorette, G.; Samimi, M. Patients’ acceptance of medical photography in a French adult and paediatric dermatology department: A questionnaire survey. Br. J. Dermatol. 2013, 169, 298–305. [Google Scholar] [CrossRef]
- Morris, C.; Scott, R.E.; Mars, M. WhatsApp in Clinical Practice-The Challenges of Record Keeping and Storage. A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 13426. [Google Scholar] [CrossRef]
- Nerminathan, A.; Harrison, A.; Phelps, M.; Scott, K.M.; Alexander, S. Doctors’ use of mobile devices in the clinical setting: A mixed methods study. Intern. Med. J. 2017, 47, 291–298. [Google Scholar] [CrossRef]
- Kornhaber, R.; Betihavas, V.; Baber, R.J. Ethical implications of digital images for teaching and learning purposes: An integrative review. J. Multidiscip. Healthc. 2015, 8, 299–305. [Google Scholar] [CrossRef] [Green Version]
- Wyatt, K.D.; Finley, A.; Uribe, R.; Pallagi, P.; Willaert, B.; Ommen, S.; Yiannias, J.; Hellmich, T. Patients’ Experiences and Attitudes of Using a Secure Mobile Phone App for Medical Photography: Qualitative Survey Study. J. Med. Internet Res. 2020, 22, e14412. [Google Scholar] [CrossRef]
- Houston, J.; Ashby, L.; Ogidi, J.; Lui, D.; Trompeter, A. A novel Caldicott-compliant hospital imaging protocol for open fracture photography. Br. J. Hosp. Med. 2020, 81, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Nabulyato, W.M.; Jeyaseelan, L.; Malagelada, F.; Heaton, S. Legal, ethical and practical considerations of smartphone use in orthopaedics. Bull. R. Coll. Surg. Engl. 2016, 98, 252–257. [Google Scholar] [CrossRef]
- Przybylo, J.A.; Wang, A.; Loftus, P.; Evans, K.H.; Chu, I.; Shieh, L. Smarter hospital communication: Secure smartphone text messaging improves provider satisfaction and perception of efficacy, workflow. J. Hosp. Med. 2014, 9, 573–578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chandawarkar, R.; Nadkarni, P. Safe clinical photography: Best practice guidelines for risk management and mitigation. Arch. Plast. Surg. 2021, 48, 295–304. [Google Scholar] [CrossRef]
- Mechanic, O.J.; Kurtzman, N.D.; Chiu, D.T.; Nathanson, L.A.; Berkowitz, S.J. Point of Care Image Capture with a Custom Smartphone Application: Experience with an Encounter-Based Workflow. J. Digit. Imaging 2020, 33, 83–87. [Google Scholar] [CrossRef]
| Total Sample (n = 257) | |
|---|---|
| n (%) | |
| Female Gender | 137 (53.3) |
| Age, years | |
| ≤40 | 177 (70.2) |
| >40 | 75 (29.8) |
| Practitioner level | |
| Resident | 116 (45.3) |
| Specialist | 140 (54.7) |
| Type of medical specialty * | |
| Medical field | 140 (55.8) |
| Medical-surgical | 72 (28.7) |
| Surgical | 39 (15.5) |
| Total Sample n (%) | Practitioner Level | Age | |||||
|---|---|---|---|---|---|---|---|
| Resident | Specialist | p-Value | ≤40 Years | >40 Years | p-Value | ||
| Why do you take photographs of patients? (Q 4) | |||||||
| I do not use it on any occasion (Q 4.1) | 18 (7.0) | 5 (4.3) | 13 (9.3) | 0.121 | 7 (4.0) | 11 (14.7) | 0.003 |
| To document the patient’s clinical progress (Q 4.2) | 180 (70.0) | 91 (78.4) | 89 (63.6) | 0.01 | 137 (77.4) | 39 (52.0) | <0.001 |
| To ask for a second opinion (Q 4.3) | 181 (70.4) | 95 (81.9) | 85 (60.7) | <0.001 | 138 (78.0) | 39 (52.0) | <0.001 |
| For educational purposes (Q 4.4) | 144 (56.0) | 62 (53.4) | 81 (57.9) | 0.479 | 101 (57.1) | 41 (54.7) | 0.726 |
| For research and publication (Q 4.5) | 166 (64.6) | 81 (69.8) | 85 (60.7) | 0.128 | 122 (68.9) | 39 (52.0) | 0.011 |
| To present at a medical conference (Q 4.6) | 175 (68.1) | 87 (75.0) | 87 (62.1) | 0.028 | 130 (73.4) | 40 (53.3) | 0.002 |
| How often do you take photographs of patients? (Q 5) | |||||||
| Weekly or more frequently | 105 (45.3) | 42 (38.2) | 63 (52.1) | 0.034 | 74 (44.0) | 29 (49.2) | 0.498 |
| Monthly of less frequently | 127 (54.7) | 68 (61.8) | 58 (47.9) | 94 (56.0) | 30 (50.8) | ||
| What kind of device do you use to take photographs? (Q 8) | |||||||
| Personal device | 191 (84.5) | 100 (91.7) | 90 (77.6) | 0.003 | 148 (89.2) | 40 (71.4) | 0.001 |
| Other (personal only for professional use/institutional) | 35 (15.5) | 9 (8.3) | 26 (22.4) | 18 (10.8) | 16 (28.6) | ||
| Where do you document oral/written consent? (Q 13) | |||||||
| I don’t document anywhere | 48 (20.2) | 21 (19.4) | 26 (20.2) | 0.902 | 36 (21.8) | 11 (15.9) | 0.466 |
| In personal documents | 24 (10.1) | 10 (9.3) | 14 (10.9) | 18 (10.9) | 6 (8.7) | ||
| Other (patient’s clinical record/with the photograph) | 166 (69.7) | 77 (71.3) | 89 (69.0) | 111 (67.3) | 52 (75.4) | ||
| I have received photographs for a second opinion (Q 23) | 198 (78.6) | 90 (78.3) | 107 (78.7) | 0.936 | 143 (82.2) | 53 (71.6) | 0.062 |
| Total Sample n (%) | Type of Specialty | ||||||
| Medical | Medical-Surgical | Surgical | p-Value | ||||
| Why do you take photographs of patients? (Q 4) | |||||||
| I do not use it on any occasion (Q 4.1) | 18 (7.0) | 14 (10.0) | 2 (2.8) | 1 (2.6) | 0.103 | ||
| To document the patient’s clinical progress (Q 4.2) | 180 (70.0) | 87 (62.1) | 58 (80.6) | 31 (79.5) | 0.008 | ||
| To ask for a second opinion (Q 4.3) | 181 (70.4) | 94 (67.1) | 52 (72.2) | 32 (82.1) | 0.185 | ||
| For educational purposes (Q 4.4) | 144 (56.0) | 77 (55.0) | 46 (63.9) | 18 (46.2) | 0.182 | ||
| For research and publication (Q 4.5) | 166 (64.6) | 90 (64.3) | 48 (66.7) | 25 (64.1) | 0.936 | ||
| To present at a medical conference (Q 4.6) | 175 (68.1) | 87 (62.1) | 54 (75.0) | 29 (74.4) | 0.104 | ||
| How often do you take photographs of patients? (Q 5) | |||||||
| Weekly or more frequently | 105 (45.3) | 41 (32.8) | 41 (62.1) | 21 (56.8) | <0.001 | ||
| Monthly of less frequently | 127 (54.7) | 84 (67.2) | 25 (37.9) | 16 (43.2) | |||
| What kind of device do you use to take photographs? (Q 8) | |||||||
| Personal device | 191 (84.5) | 102 (82.9) | 53 (84.1) | 32 (91.4) | 0.466 | ||
| Other (personal only for professional use/institutional) | 35 (15.5) | 21 (17.1) | 10 (15.9) | 3 (8.6) | |||
| Where do you document oral/written consent? (Q 13) | |||||||
| I don´t document anywhere | 48 (20.2) | 15 (11.5) | 20 (29.0) | 13 (38.2) | 0.002 | ||
| In personal documents | 24 (10.1) | 17 (13.0) | 4 (5.8) | 3 (8.8) | |||
| Other (patient’s clinical record/with the photograph) | 166 (69.7) | 99 (75.6) | 45 (65.2) | 18 (52.9) | |||
| I have received photographs for a second opinion (Q 23) | 198 (78.6) | 100 (73.0) | 61 (84.7) | 35 (92.1) | 0.015 | ||
| None | Only Verbal Consent | Only Written Consent | Both Verbal and Written Consent | |
|---|---|---|---|---|
| Why do you take photographs of patients? (Q 4) | ||||
| To document the patient’s clinical progress (Q 4.2) | 37 (20.6) | 120 (66.7) | 8 (4.4) | 15 (8.3) |
| To ask for a second opinion (Q 4.3) | 43 (23.8) | 126 (69.6) | 3 (1.7) | 9 (5.0) |
| For educational purposes (Q 4.4) | 39 (27.1) | 72 (50.0) | 9 (6.3) | 24 (16.7) |
| For research and publication (Q 4.5) | 20 (12.0) | 31 (18.7) | 21 (12.7) | 94 (56.6) |
| To present at a medical conference (Q 4.6) | 33 (18.9) | 49 (28.0) | 21 (12.0) | 72 (41.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cura, M.; Alves, H.; Andrade, J.P. Medical Photography Usage Amongst Doctors at a Portuguese Hospital. Int. J. Environ. Res. Public Health 2022, 19, 7304. https://doi.org/10.3390/ijerph19127304
Cura M, Alves H, Andrade JP. Medical Photography Usage Amongst Doctors at a Portuguese Hospital. International Journal of Environmental Research and Public Health. 2022; 19(12):7304. https://doi.org/10.3390/ijerph19127304
Chicago/Turabian StyleCura, Mariana, Hélio Alves, and José Paulo Andrade. 2022. "Medical Photography Usage Amongst Doctors at a Portuguese Hospital" International Journal of Environmental Research and Public Health 19, no. 12: 7304. https://doi.org/10.3390/ijerph19127304
APA StyleCura, M., Alves, H., & Andrade, J. P. (2022). Medical Photography Usage Amongst Doctors at a Portuguese Hospital. International Journal of Environmental Research and Public Health, 19(12), 7304. https://doi.org/10.3390/ijerph19127304