Combined Use of Transcutaneous Electrical Nerve Stimulation and Short Foot Exercise Improves Navicular Height, Muscle Size, Function Mobility, and Risk of Falls in Healthy Older Adults
Abstract
:1. Introduction
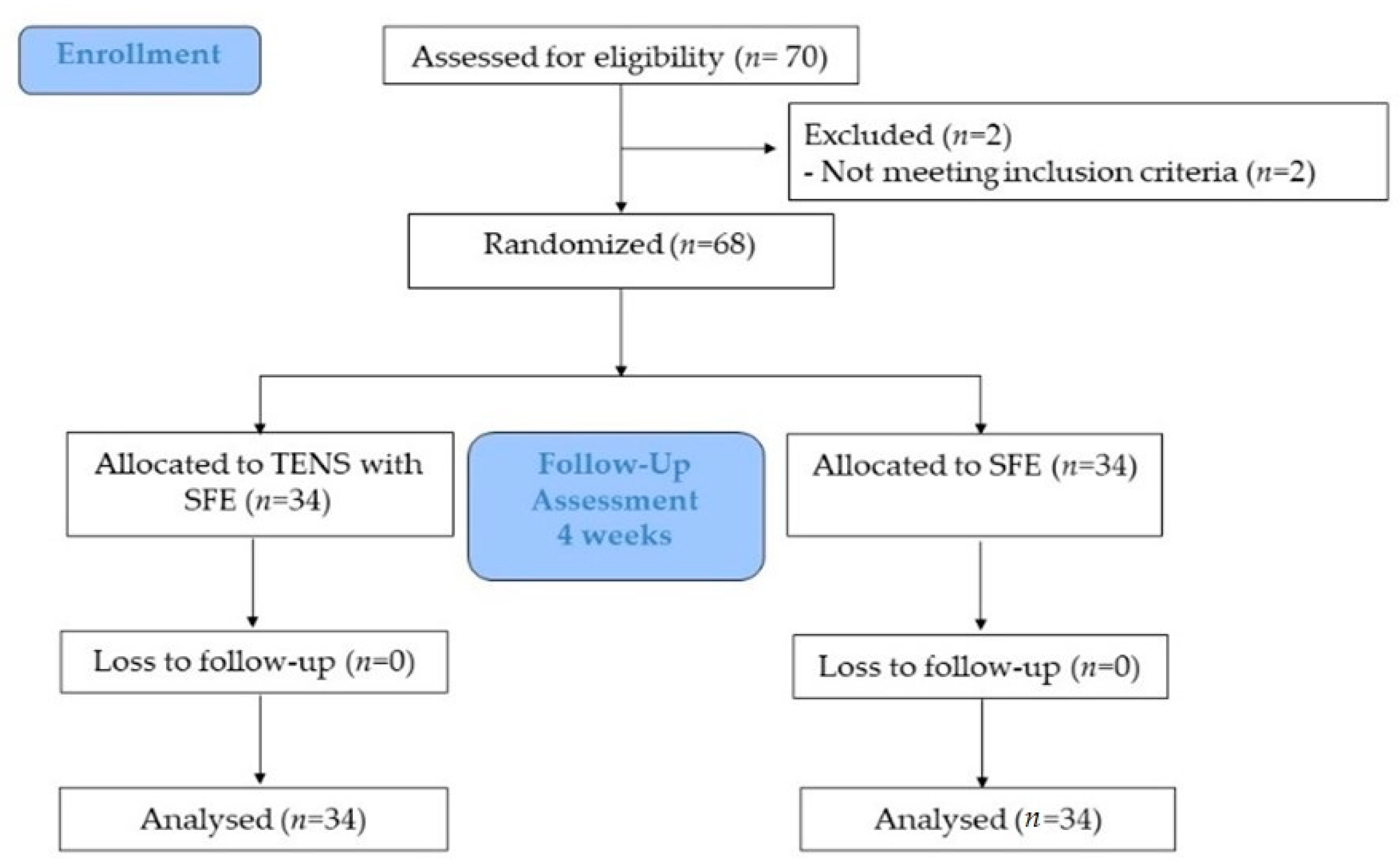
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Intervention
2.4. Outcome Measures
2.5. Statistical Analysis
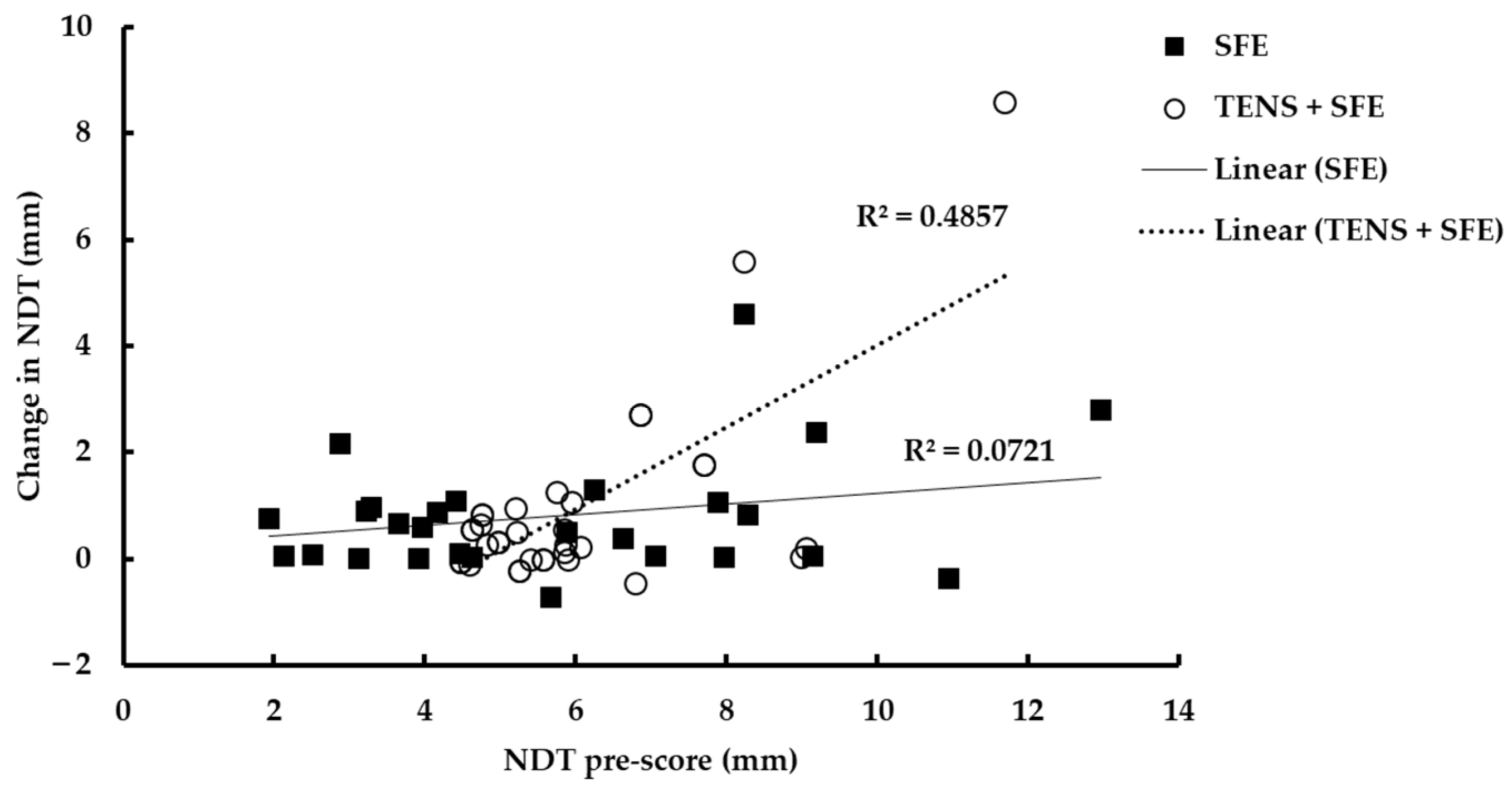
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pellicer-Garcia, B.; Anton-Solanas, I.; Ramon-Arbues, E.; Garcia-Moyano, L.; Gea-Caballero, V.; Juarez-Vela, R. Risk of Falling and Associated Factors in Older Adults with a Previous History of Falls. Int. J. Environ. Res. Public Health 2020, 17, 4085. [Google Scholar] [CrossRef] [PubMed]
- Lai, Z.; Pang, H.; Hu, X.; Dong, K.; Wang, L. Effects of intrinsic-foot-muscle exercise combined with the lower extremity resistance training on postural stability in older adults with fall risk: Study protocol for a randomised controlled trial. Trials 2021, 22, 587. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.J.; Yang, P.Y.; Yang, Y.C.; Lin, M.R.; Wang, Y.W. Prevalence and risk factors of falls among community-dwelling older people: Results from three consecutive waves of the national health interview survey in Taiwan. BMC Geriatr. 2020, 20, 529. [Google Scholar] [CrossRef] [PubMed]
- Birhanie, G.; Melese, H.; Solomon, G.; Fissha, B.; Teferi, M. Fear of falling and associated factors among older people living in Bahir Dar City, Amhara, Ethiopia-a cross-sectional study. BMC Geriatr. 2021, 21, 586. [Google Scholar] [CrossRef]
- Moreland, J.D.; Richardson, J.A.; Goldsmith, C.H.; Clase, C.M. Muscle weakness and falls in older adults: A systematic review and meta-analysis. J. Am. Geriatr. Soc. 2004, 52, 1121–1129. [Google Scholar] [CrossRef]
- Mickle, K.J.; Munro, B.J.; Lord, S.R.; Menz, H.B.; Steele, J.R. ISB Clinical Biomechanics Award 2009: Toe weakness and deformity increase the risk of falls in older people. Clin. Biomech. 2009, 24, 787–791. [Google Scholar] [CrossRef]
- Willemse, L.; Wouters, E.J.M.; Bronts, H.M.; Pisters, M.F.; Vanwanseele, B. The effect of interventions anticipated to improve plantar intrinsic foot muscle strength on fall-related dynamic function in adults: A systematic review. J. Foot Ankle Res. 2022, 15, 3. [Google Scholar] [CrossRef]
- Namsawang, J.; Muanjai, P.; Luangpon, N.; Kiatkulanusorn, S. The Effects of Electrical Stimulation Program on Navicular Height, Balance, and Fear of Falling in Community-Dwelling Elderly. Int. J. Environ. Res. Public Health 2021, 18, 9351. [Google Scholar] [CrossRef]
- Kusagawa, Y.; Kurihara, T.; Imai, A.; Maeo, S.; Sugiyama, T.; Kanehisa, H.; Isaka, T. Toe flexor strength is associated with mobility in older adults with pronated and supinated feet but not with neutral feet. J. Foot Ankle Res. 2020, 13, 55. [Google Scholar] [CrossRef]
- Cobb, S.C.; Bazett-Jones, D.M.; Joshi, M.N.; Earl-Boehm, J.E.; James, C.R. The relationship among foot posture, core and lower extremity muscle function, and postural stability. J. Athl. Train. 2014, 49, 173–180. [Google Scholar] [CrossRef]
- Koyama, K.; Yamauchi, J. Altered postural sway following fatiguing foot muscle exercises. PLoS ONE 2017, 12, e0189184. [Google Scholar] [CrossRef] [PubMed]
- McKeon, P.O.; Hertel, J.; Bramble, D.; Davis, I. The foot core system: A new paradigm for understanding intrinsic foot muscle function. Br. J. Sports Med. 2015, 249, 290. [Google Scholar] [CrossRef] [PubMed]
- Fiolkowski, P.; Brunt, D.; Bishop, M.; Woo, R.; Horodyski, M. Intrinsic pedal musculature support of the medial longitudinal arch: An electromyography study. J. Foot Ankle Surg. 2003, 42, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Headlee, D.L.; Leonard, J.L.; Hart, J.M.; Ingersoll, C.D.; Hertel, J. Fatigue of the plantar intrinsic foot muscles increases navicular drop. J. Electromyogr. Kinesiol. 2008, 18, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Park, D.J.; Hwang, Y.I. Comparison of the Intrinsic Foot Muscle Activities between Therapeutic and Three-Dimensional Foot-Ankle Exercises in Healthy Adults: An Explanatory Study. Int. J. Environ. Res. Public Health 2020, 17, 7189. [Google Scholar] [CrossRef] [PubMed]
- Latey, P.J.; Burns, J.; Nightingale, E.J.; Clarke, J.L.; Hiller, C.E. Reliability and correlates of cross-sectional area of abductor hallucis and the medial belly of the flexor hallucis brevis measured by ultrasound. J. Foot Ankle Res. 2018, 11, 28. [Google Scholar] [CrossRef]
- Taşa, S.; Çetinb, A. Mechanical properties and morphologic features of intrinsic foot muscles and plantar fascia in individuals with hallux valgus. Acta Orthop. Traumatol. Turc. 2019, 54, 282–286. [Google Scholar] [CrossRef]
- Jandova, T.; Narici, M.V.; Steffl, M.; Bondi, D.; D’Amico, M.; Pavlu, D.; Verratti, V.; Fulle, S.; Pietrangelo, T. Muscle Hypertrophy and Architectural Changes in Response to Eight-Week Neuromuscular Electrical Stimulation Training in Healthy Older People. Life 2020, 10, 184. [Google Scholar] [CrossRef]
- Mickle, K.J.; Angin, S.; Crofts, G.; Nester, C.J. Effects of Age on Strength and Morphology of Toe Flexor Muscles. J. Orthop. Sports Phys. Ther. 2016, 46, 1065–1070. [Google Scholar] [CrossRef]
- Pietrangelo, T.; Doria, C.; Bondi, D.; Kinel, E.; Renda, G.; Neri, G.; Verratti, V. Effects of endurance, resistance and neuro-muscular electrical stimulation trainings to the anthropometric and functional mobility domains in elderly. J. Gerontol. Geriatr. 2019, 67, 148–155. [Google Scholar]
- Mulligan, E.P.; Cook, P.G. Effect of plantar intrinsic muscle training on medial longitudinal arch morphology and dynamic function. Man. Ther. 2013, 18, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Cho, J.; Lee, S. Short-Foot Exercise Promotes Quantitative Somatosensory Function in Ankle Instability: A Randomized Controlled Trial. Med. Sci. Monit. 2019, 25, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Lynn, S.K.; Padilla, R.A.; Tsang, K.K. Differences in static- and dynamic-balance task performance after 4 weeks of intrinsic-foot-muscle training: The short-foot exercise versus the towel-curl exercise. J. Sport Rehabil. 2012, 21, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Tyson, S.F.; Sadeghi-Demneh, E.; Nester, C.J. The effects of transcutaneous electrical nerve stimulation on strength, proprioception, balance and mobility in people with stroke: A randomized controlled cross-over trial. Clin. Rehabil. 2013, 27, 785–791. [Google Scholar] [CrossRef] [PubMed]
- Cheing, G.L.; Hui-Chan, C.W. Would the addition of TENS to exercise training produce better physical performance outcomes in people with knee osteoarthritis than either intervention alone? Clin. Rehabil. 2004, 18, 487–497. [Google Scholar] [CrossRef]
- Namsawang, J.; Eungpinichpong, W.; Vichiansiri, R.; Rattanathongkom, S. Effects of the Short Foot Exercise with Neuromuscular Electrical Stimulation on Navicular Height in Flexible Flatfoot in Thailand: A Randomized Controlled Trial. J. Prev. Med. Public Health 2019, 52, 250–257. [Google Scholar] [CrossRef]
- Maffiuletti, N.A.; Dugnani, S.; Folz, M.; Di Pierno, E.; Mauro, F. Effect of combined electrostimulation and plyometric training on vertical jump height. Med. Sci. Sports Exerc. 2002, 34, 1638–1644. [Google Scholar] [CrossRef]
- Cho, H.Y.; In, T.S.; Cho, K.H.; Song, C.H. A single trial of transcutaneous electrical nerve stimulation (TENS) improves spasticity and balance in patients with chronic stroke. Tohoku J. Exp. Med. 2013, 229, 187–193. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Bubela, D.J.; Magasi, S.R.; Wang, Y.C.; Gershon, R.C. Sit-to-stand test: Performance and determinants across the age-span. Isokinet. Exerc. Sci. 2010, 18, 235–240. [Google Scholar] [CrossRef]
- Munoz-Bermejo, L.; Adsuar, J.C.; Mendoza-Munoz, M.; Barrios-Fernandez, S.; Garcia-Gordillo, M.A.; Perez-Gomez, J.; Carlos-Vivas, J. Test-Retest Reliability of Five Times Sit to Stand Test (FTSST) in Adults: A Systematic Review and Meta-Analysis. Biology 2021, 10, 510. [Google Scholar] [CrossRef]
- Panel on Prevention of Falls in Older Persons; American Geriatrics Society and British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J. Am. Geriatr. Soc. 2011, 59, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Barry, E.; Galvin, R.; Keogh, C.; Horgan, F.; Fahey, T. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: A systematic review and meta-analysis. BMC Geriatr. 2014, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Jang, E.M.; Park, S.H. Effects of Neuromuscular Electrical Stimulation Combined with Exercises versus an Exercise Program on the Physical Characteristics and Functions of the Elderly: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 2463. [Google Scholar] [CrossRef]
- Thiamwong, L.; Suwanno, J. Fear of Falling and Related Factors in a Community-based Studyof People 60 Years and Older in Thailand. Int. J. Gerontol. 2017, 11, 80–84. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Wong, Y.S. Influence of the abductor hallucis muscle on the medial arch of the foot: A kinematic and anatomical cadaver study. Foot Ankle Int. 2007, 28, 617–620. [Google Scholar] [CrossRef]
- Hahm, S.-C.; Suh, H.R.; Cho, H.-Y. The effect of transcutaneous electrical nerve stimulation on pain, muscle strength, balance, and gait in individuals with dementia: A double blind, pilot randomized controlled trial. Eur. J. Integr. Med. 2019, 29, 100932. [Google Scholar] [CrossRef]
- Davis, L.A.; Carzoli, J.P.; Feka, K.; Nelson, C.; Enoka, R.M. Exercise with TENS does not augment gains in balance and strength for dancers. J. Electromyogr. Kinesiol. 2021, 56, 102507. [Google Scholar] [CrossRef]
- Kim, E.K.; Kim, J.S. The effects of short foot exercises and arch support insoles on improvement in the medial longitudinal arch and dynamic balance of flexible flatfoot patients. J. Phys. Ther. Sci. 2016, 28, 3136–3139. [Google Scholar] [CrossRef]
- Stewart, S.; Ellis, R.; Heath, M.; Rome, K. Ultrasonic evaluation of the abductor hallucis muscle in hallux valgus: A cross-sectional observational study. BMC Musculoskelet. Disord. 2013, 14, 45. [Google Scholar] [CrossRef]
- Franchi, M.V.; Longo, S.; Mallinson, J.; Quinlan, J.I.; Taylor, T.; Greenhaff, P.L.; Narici, M.V. Muscle thickness correlates to muscle cross-sectional area in the assessment of strength training-induced hypertrophy. Scand. J. Med. Sci. Sports 2018, 28, 846–853. [Google Scholar] [CrossRef] [PubMed]
- Gondin, J.; Guette, M.; Ballay, Y.; Martin, A. Electromyostimulation training effects on neural drive and muscle architecture. Med. Sci. Sports Exerc. 2005, 37, 1291–1299. [Google Scholar] [CrossRef] [PubMed]
- Onigbinde, A.T.; Adeloye, O.O.; Akindoyin, O.; Nesto, T. Effects of motor-level transcutaneous electrical nerve stimulation on ipsilateral and un-stimulated contralateral quadriceps femoris. Technol. Health Care 2014, 22, 759–766. [Google Scholar] [CrossRef]
- Nishikawa, Y.; Takahashi, T.; Kawade, S.; Maeda, N.; Maruyama, H.; Hyngstrom, A. The Effect of Electrical Muscle Stimulation on Muscle Mass and Balance in Older Adults with Dementia. Brain Sci. 2021, 11, 339. [Google Scholar] [CrossRef]
- Jung, J.Y.; Jung, J.H.; Hahm, S.C.; Jung, K.; Kim, S.J.; Suh, H.R.; Cho, H.Y. The effect of single trial transcutaneous electrical nerve stimulation on balance and gait function in elderly people with dementia: A pilot study. Phys. Ther. Rehabil. Sci. 2017, 6, 59–64. [Google Scholar] [CrossRef]
- Enoka, R.M.; Amiridis, I.G.; Duchateau, J. Electrical Stimulation of Muscle: Electrophysiology and Rehabilitation. Physiology 2020, 35, 40–56. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, A.; Chavis, M.; Watkins, J.; Wilson, T. The five-times-sit-to-stand test: Validity, reliability and detectable change in older females. Aging Clin. Exp. Res. 2012, 24, 339–344. [Google Scholar] [CrossRef]
- Melo, T.A.; Duarte, A.C.M.; Bezerra, T.S.; Franca, F.; Soares, N.S.; Brito, D. The Five Times Sit-to-Stand Test: Safety and reliability with older intensive care unit patients at discharge. Rev. Bras. Ter. Intensiv. 2019, 31, 27–33. [Google Scholar] [CrossRef]
- Menz, H.B.; Lord, S.R. Foot pain impairs balance and functional ability in community-dwelling older people. J. Am. Podiatr. Med. Assoc. 2001, 91, 222–229. [Google Scholar] [CrossRef]
- Pinheiro, H.A.; Vilaça, K.H.C.; Carvalho, G.A. Assessment of muscle mass, risk of falls and fear of falling in elderly people with diabetic neuropathy. Fisioter. Mov. 2015, 28, 677–683. [Google Scholar] [CrossRef]
- Mickle, K.J.; Caputi, P.; Potter, J.M.; Steele, J.R. Efficacy of a progressive resistance exercise program to increase toe flexor strength in older people. Clin. Biomech. 2016, 40, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, T.; Sakuraba, K. Strength training for the intrinsic flexor muscles of the foot: Effects on muscle strength, the foot arch, and dynamic parameters before and after the training. J. Phys. Ther. Sci. 2014, 26, 373–376. [Google Scholar] [CrossRef]
- Menz, H.B.; Morris, M.E.; Lord, S.R. Foot and ankle risk factors for falls in older people: A prospective study. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 866–870. [Google Scholar] [CrossRef] [PubMed]
| TENS + SFE (n = 34) | SFE Alone (n = 34) | |
|---|---|---|
| Age (years) | 68.6 ± 4.6 | 68.7 ± 4.0 |
| Sex | 6 Males, 28 females | 6 Males, 28 females |
| Weight (Kg) | 59.9 ± 11.3 | 60.7 ± 11.5 |
| Height (cm) | 158.6 ± 9.6 | 158.9 ± 8.2 |
| BMI (Kg∙m−2) | 23.8 ± 3.7 | 23.9 ± 3.1 |
| NDT (mm) | 6.01 ± 1.61 | 5.96 ± 3.03 |
| FES-I (points) | 27.7 ± 10.2 | 26.4 ± 7.1 |
| CSA of AbdH (cm2) | 1.93 ± 0.49 | 1.86 ± 0.50 |
| 5TSTS (s) | 6.58 ± 1.68 | 7.53 ± 1.78 |
| TUG (s) | 6.98 ± 1.53 | 7.77 ± 1.75 |
| TENS + SFE (n = 34) | SFE Alone (n = 34) | Between Groups | |||
|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||
| NDT (mm) | 5.57 (4.80, 6.81) | 4.71 (4.15, 5.61) * | 5.16 (3.56, 8.04) | 4.60 (2.98, 4.60) * | 0.64 |
| FES-I (points) | 27.0 (19.0, 36.3) | 19 (16.0, 22.3) * | 25.0 (20.8, 31.0) | 21.0 (17.0, 25.0) * | 0.83 |
| CSA of AbdH (cm2) | 1.86 (1.61, 2.31) | 2.05(1.76, 2.53) * | 1.79 (1.56, 2.20) | 2.16 (1.77, 2.50) * | 0.49 |
| 5TSTS (s) | 6.52 (5.50, 7.87) | 5.61 (4.99, 6.25) * | 7.53 (6.10, 8.40) | 6.10 (5.36, 7.84)* | 0.68 |
| TUG (s) | 6.62 (6.15, 7.67) | 5.88 (5.43, 6.49) * | 7.41 (6.47, 8.90) | 6.67 (6.03, 8.25) * | 0.008 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Namsawang, J.; Muanjai, P. Combined Use of Transcutaneous Electrical Nerve Stimulation and Short Foot Exercise Improves Navicular Height, Muscle Size, Function Mobility, and Risk of Falls in Healthy Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 7196. https://doi.org/10.3390/ijerph19127196
Namsawang J, Muanjai P. Combined Use of Transcutaneous Electrical Nerve Stimulation and Short Foot Exercise Improves Navicular Height, Muscle Size, Function Mobility, and Risk of Falls in Healthy Older Adults. International Journal of Environmental Research and Public Health. 2022; 19(12):7196. https://doi.org/10.3390/ijerph19127196
Chicago/Turabian StyleNamsawang, Juntip, and Pornpimol Muanjai. 2022. "Combined Use of Transcutaneous Electrical Nerve Stimulation and Short Foot Exercise Improves Navicular Height, Muscle Size, Function Mobility, and Risk of Falls in Healthy Older Adults" International Journal of Environmental Research and Public Health 19, no. 12: 7196. https://doi.org/10.3390/ijerph19127196
APA StyleNamsawang, J., & Muanjai, P. (2022). Combined Use of Transcutaneous Electrical Nerve Stimulation and Short Foot Exercise Improves Navicular Height, Muscle Size, Function Mobility, and Risk of Falls in Healthy Older Adults. International Journal of Environmental Research and Public Health, 19(12), 7196. https://doi.org/10.3390/ijerph19127196






