Dry Heat as a Potential Decontamination Method on the Filtration Efficiency of Filtering Facepiece Respirators
Abstract
:1. Introduction
2. Materials and Methods
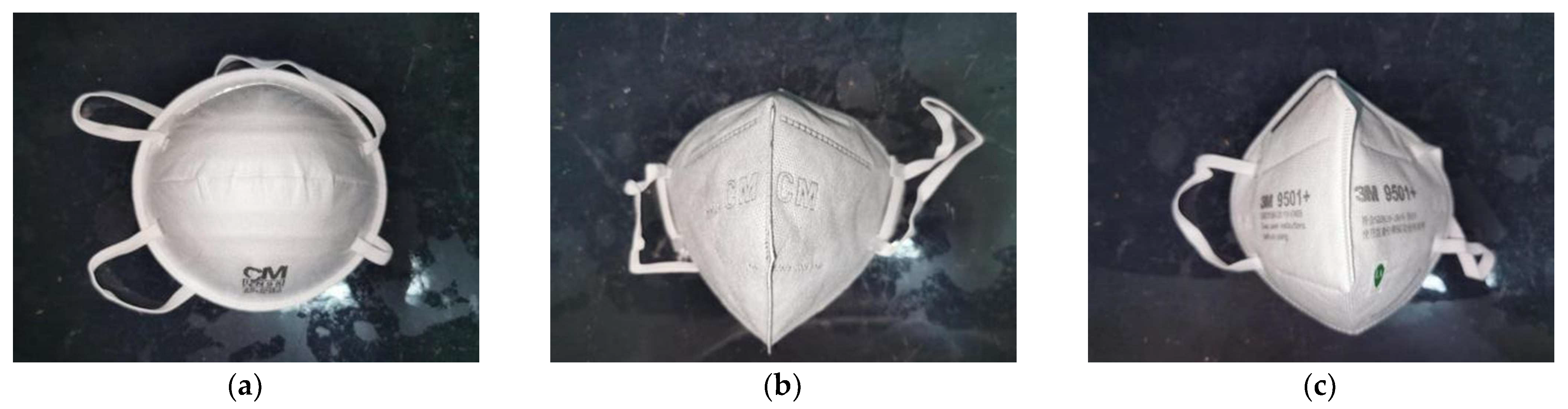
2.1. Filtering Facepiece Respirator Description
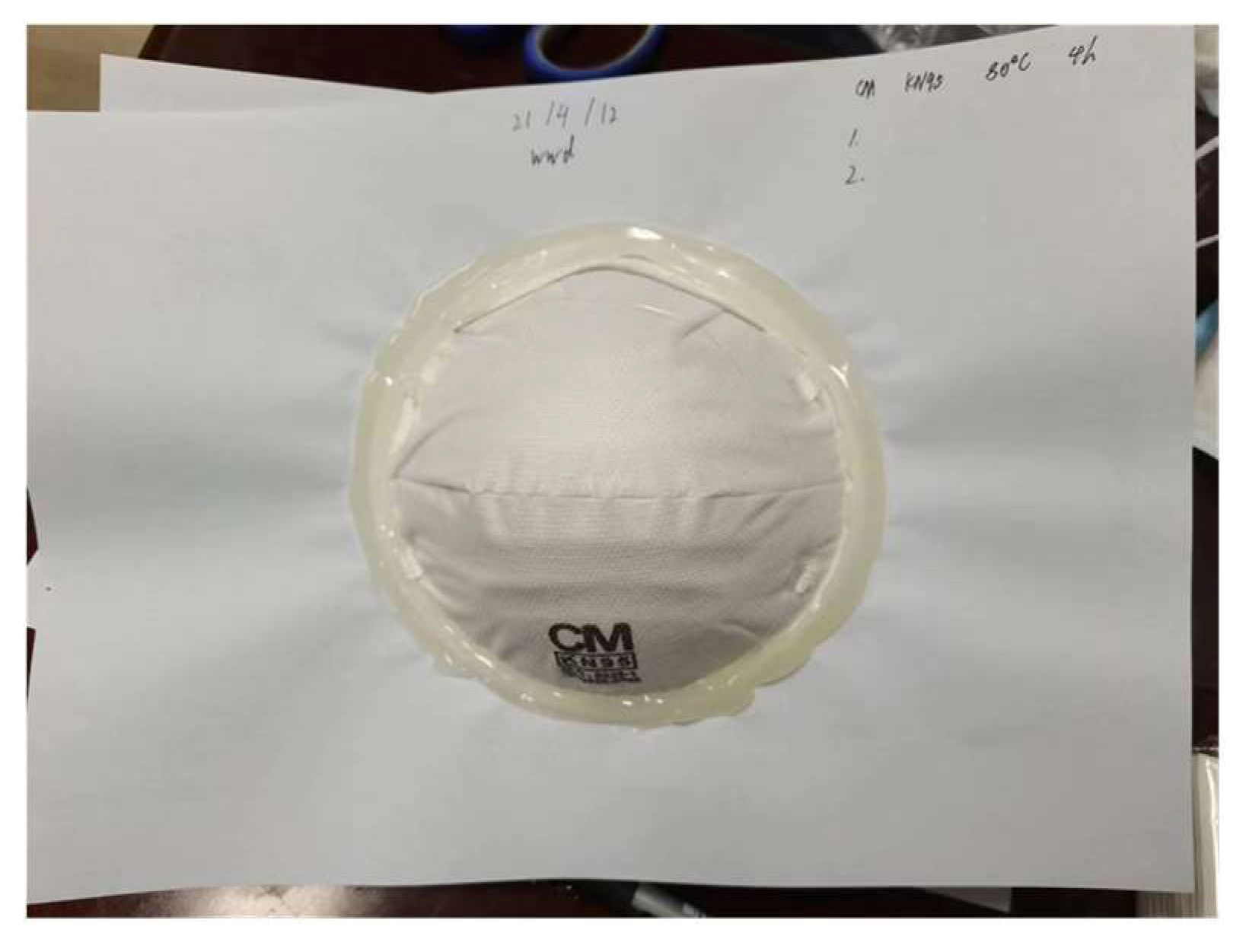
2.2. Heat Pretreatment
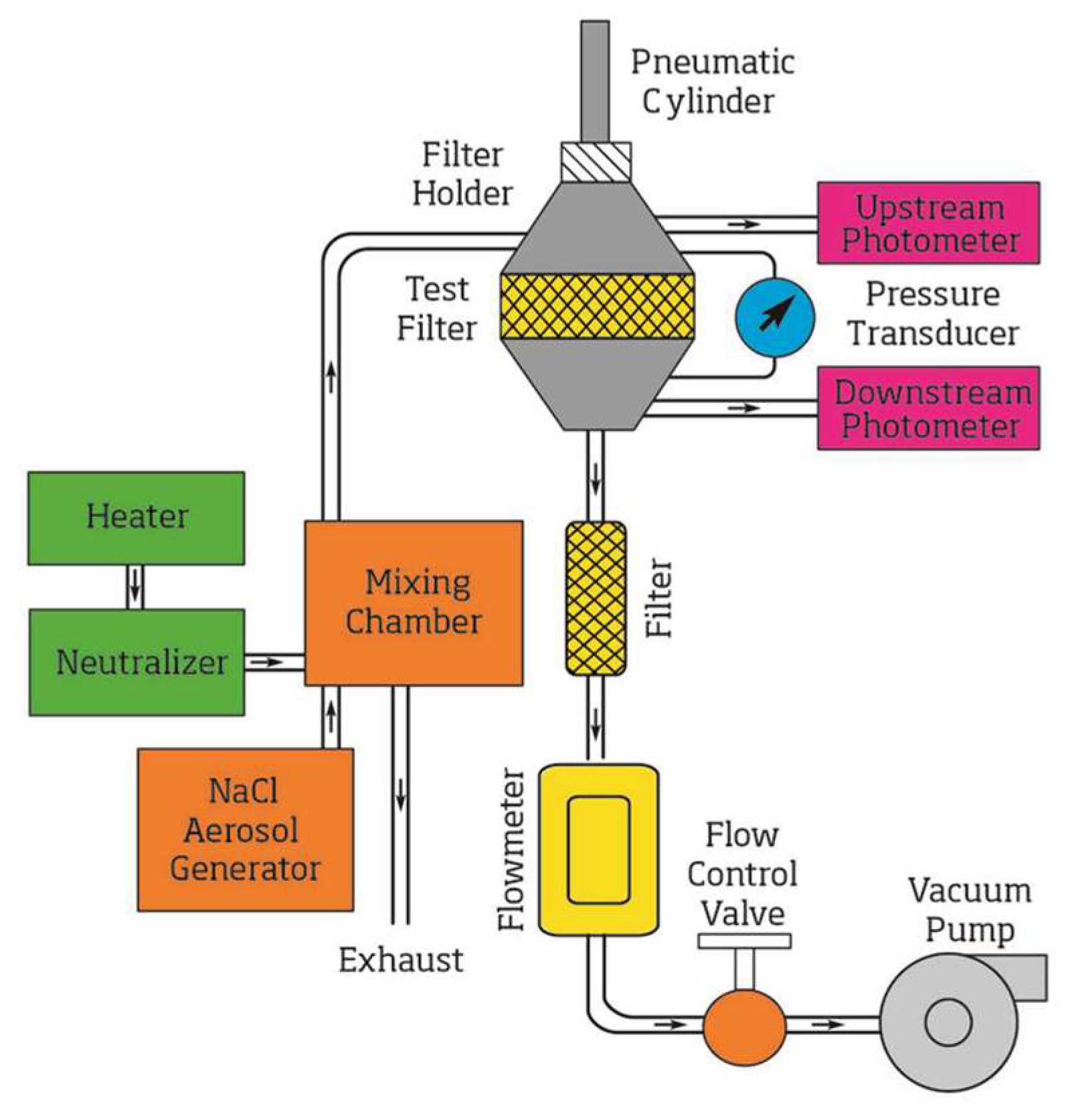
2.3. Filtration Efficiency Measurement
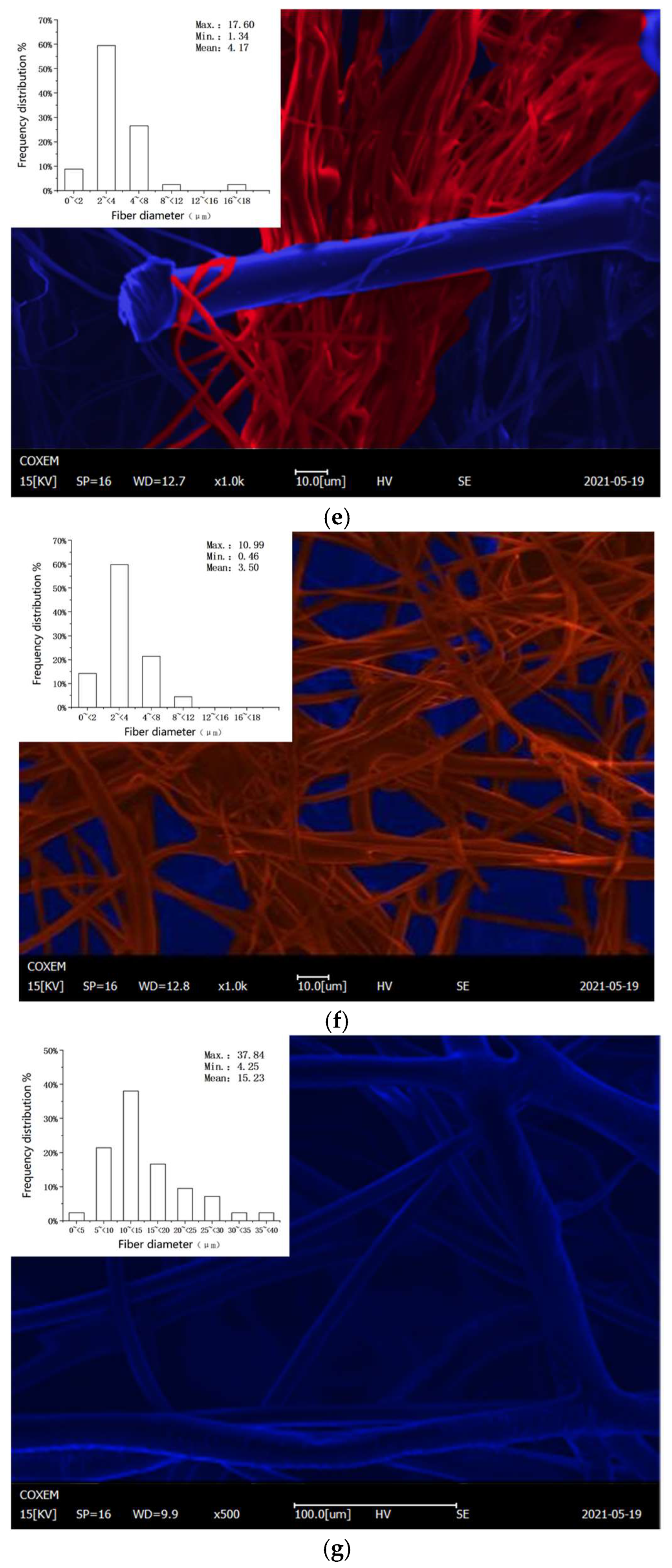
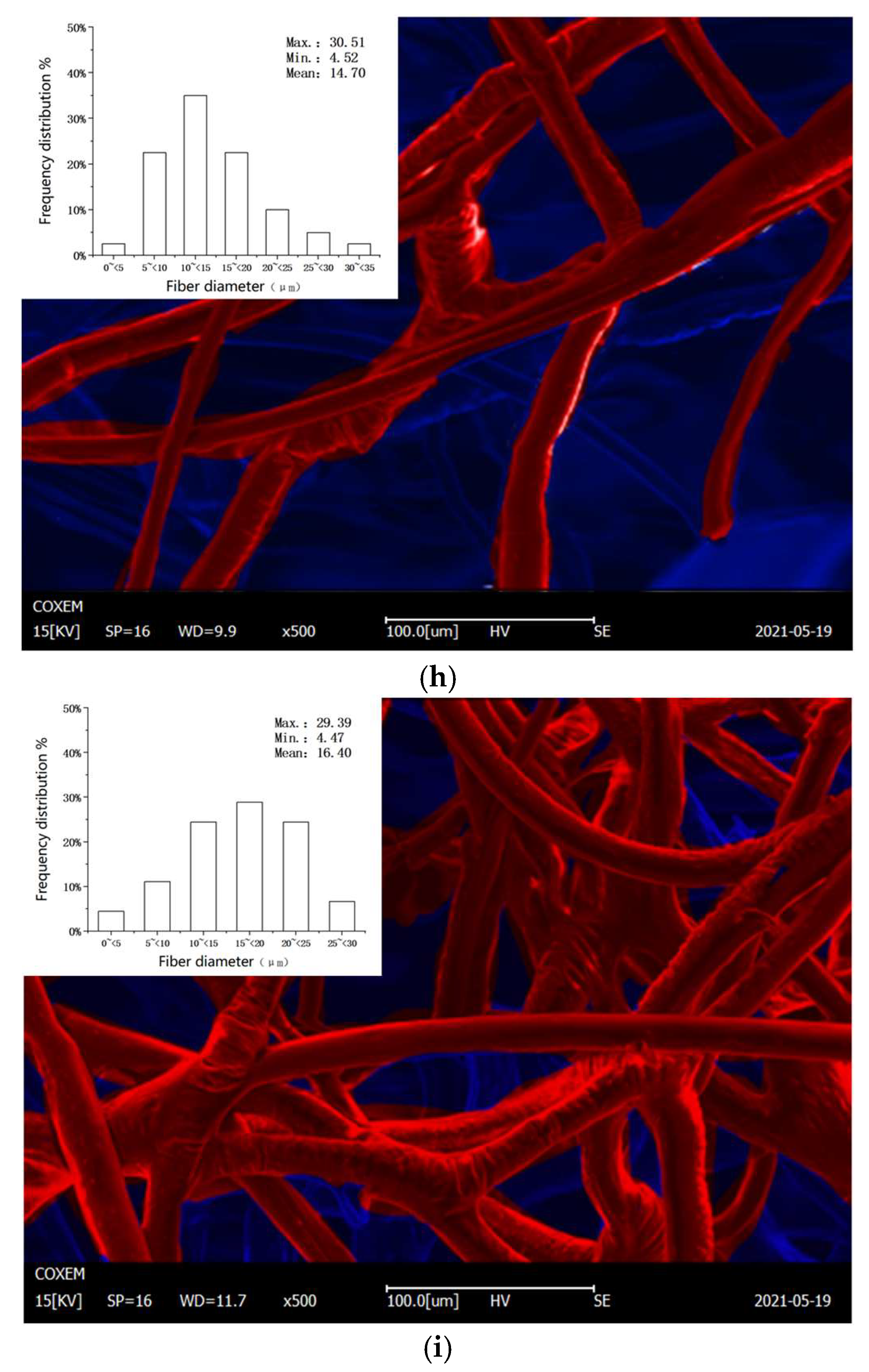
2.4. Microstructure of the Respirator Filter
2.5. Experimental Data Processing
2.5.1. Filtration Efficiency
2.5.2. Microstructure
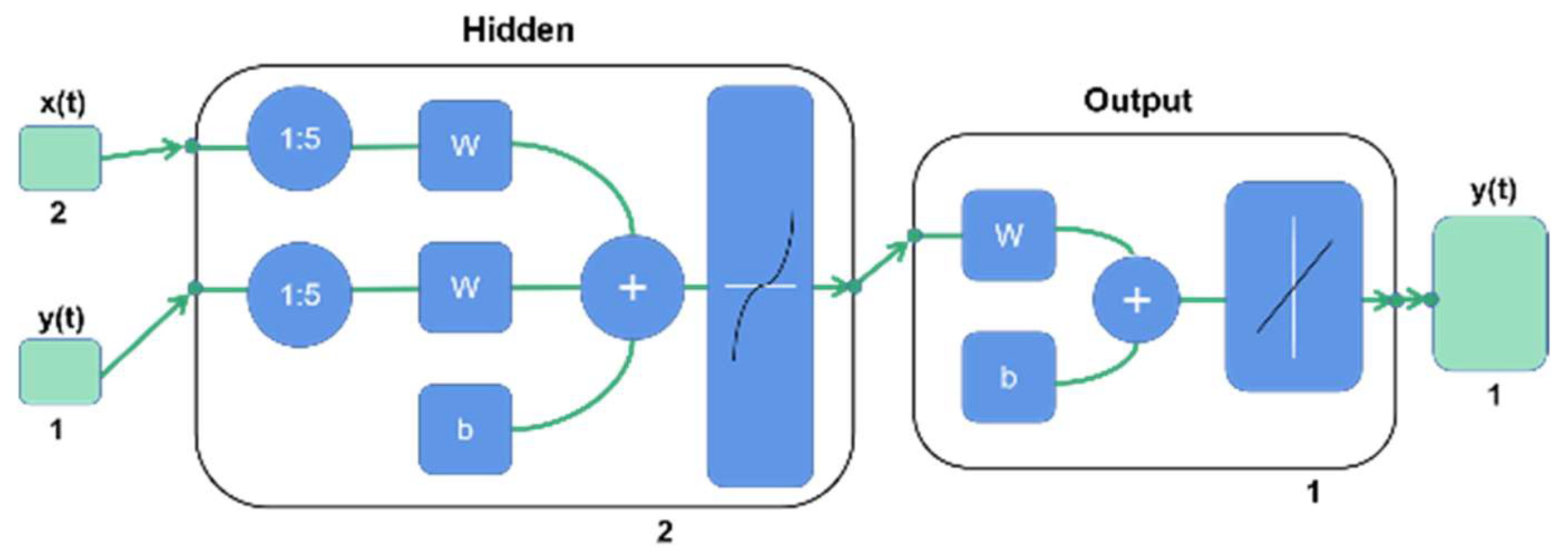
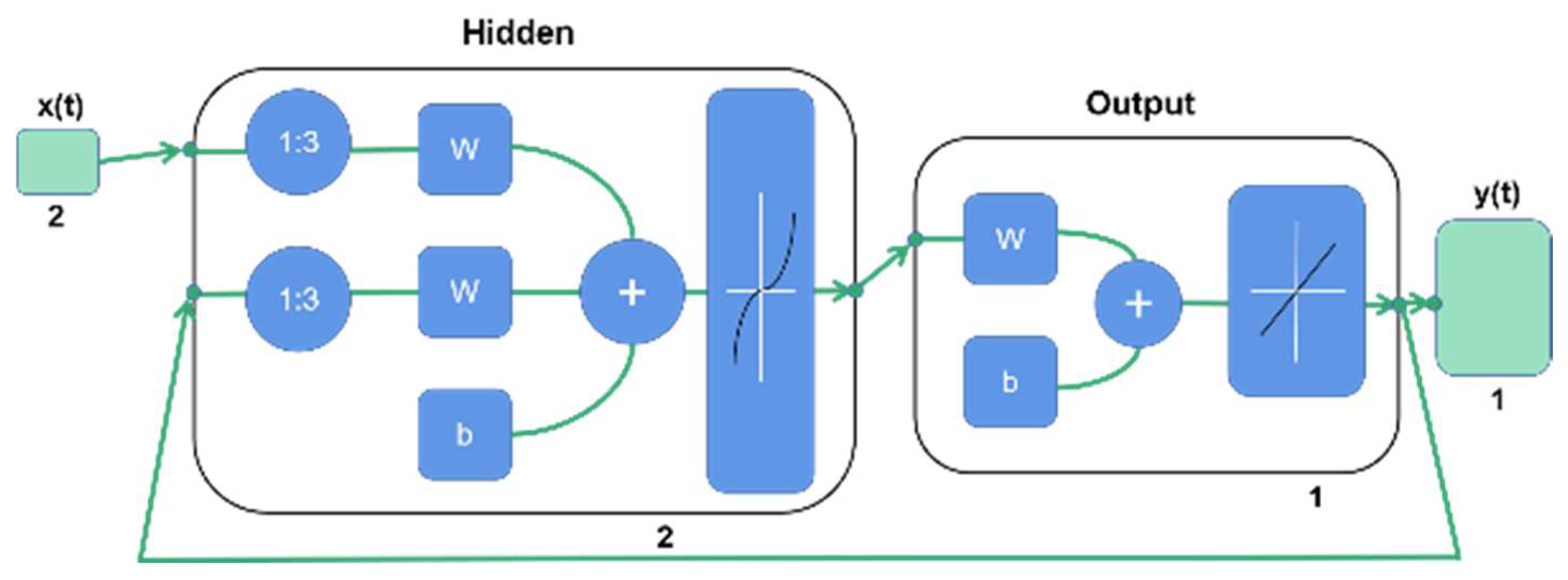
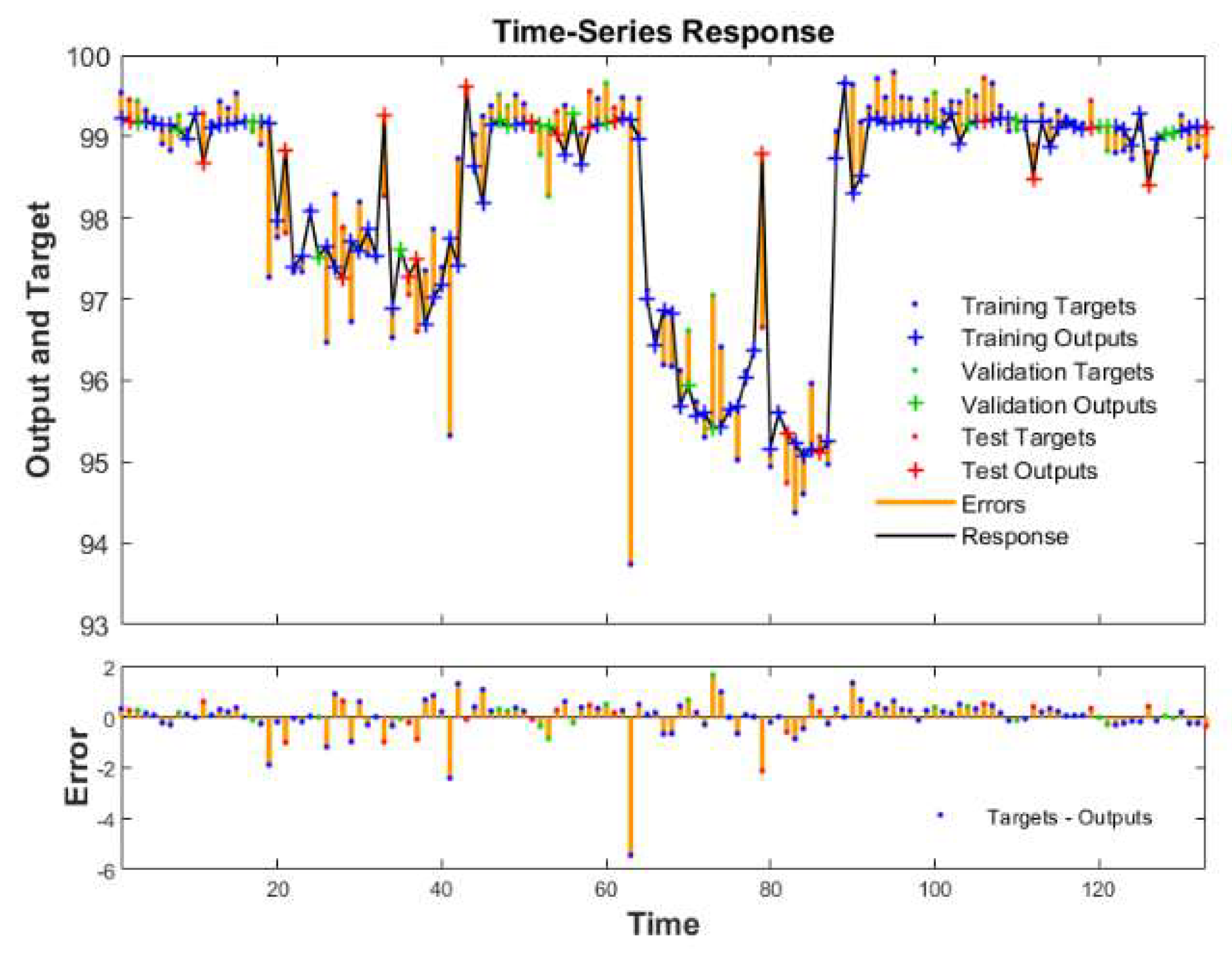
2.5.3. Establishment of a Neural Network Model
3. Results
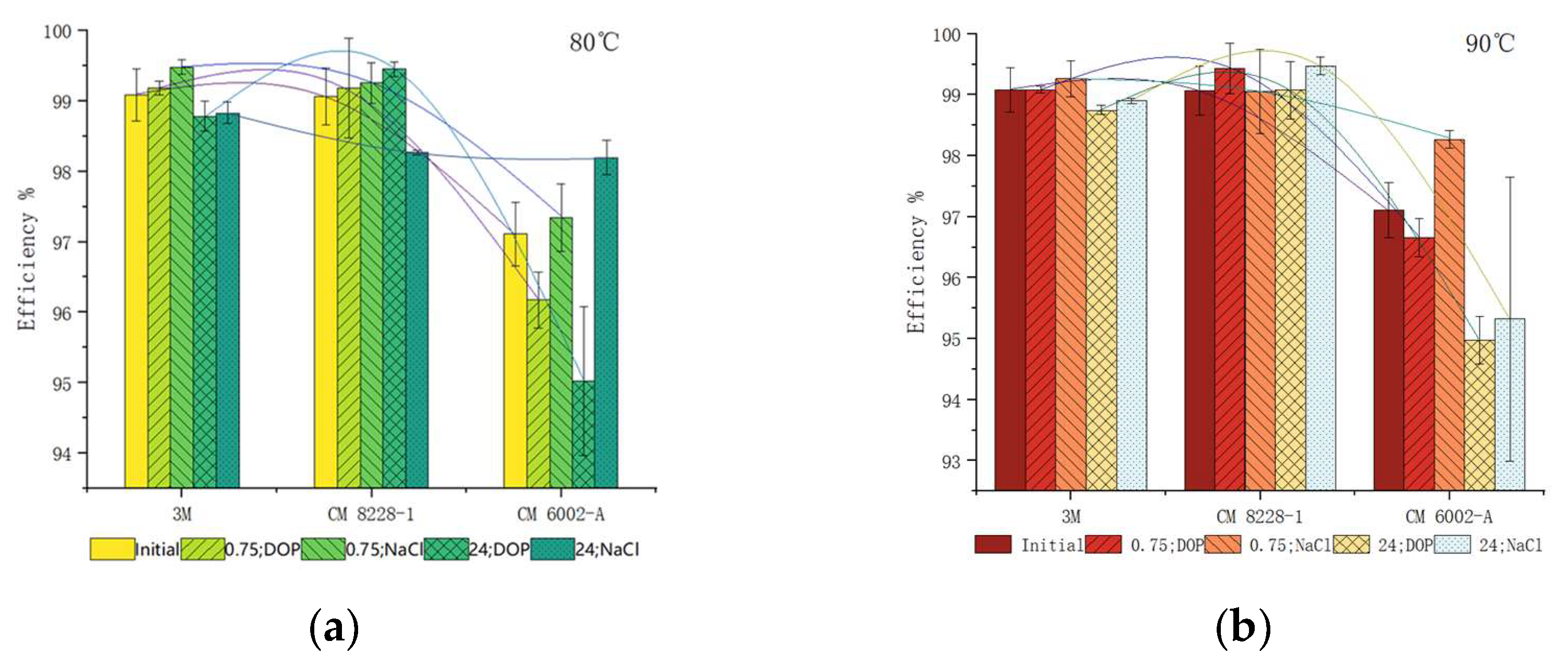
3.1. Filtration Efficiency
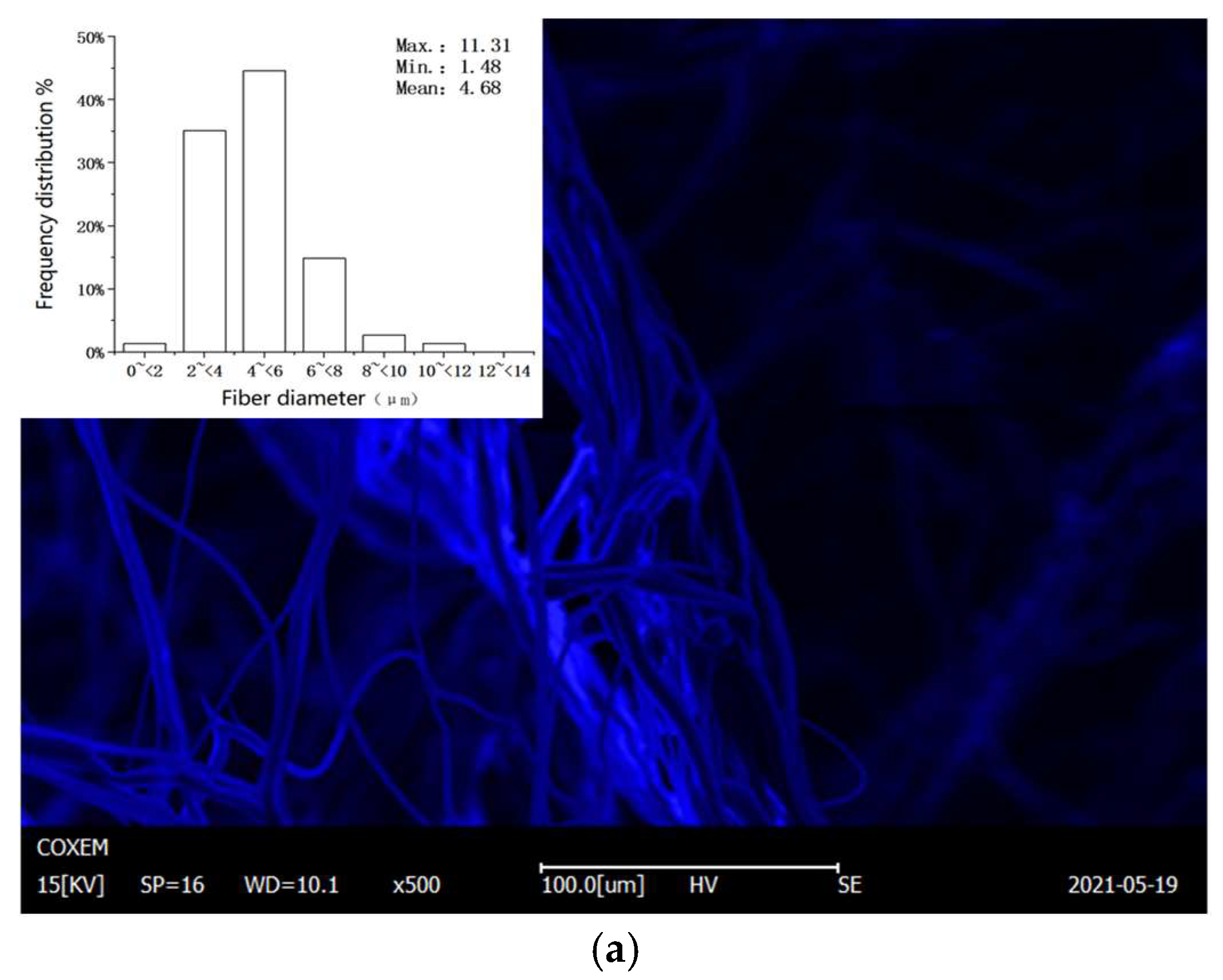
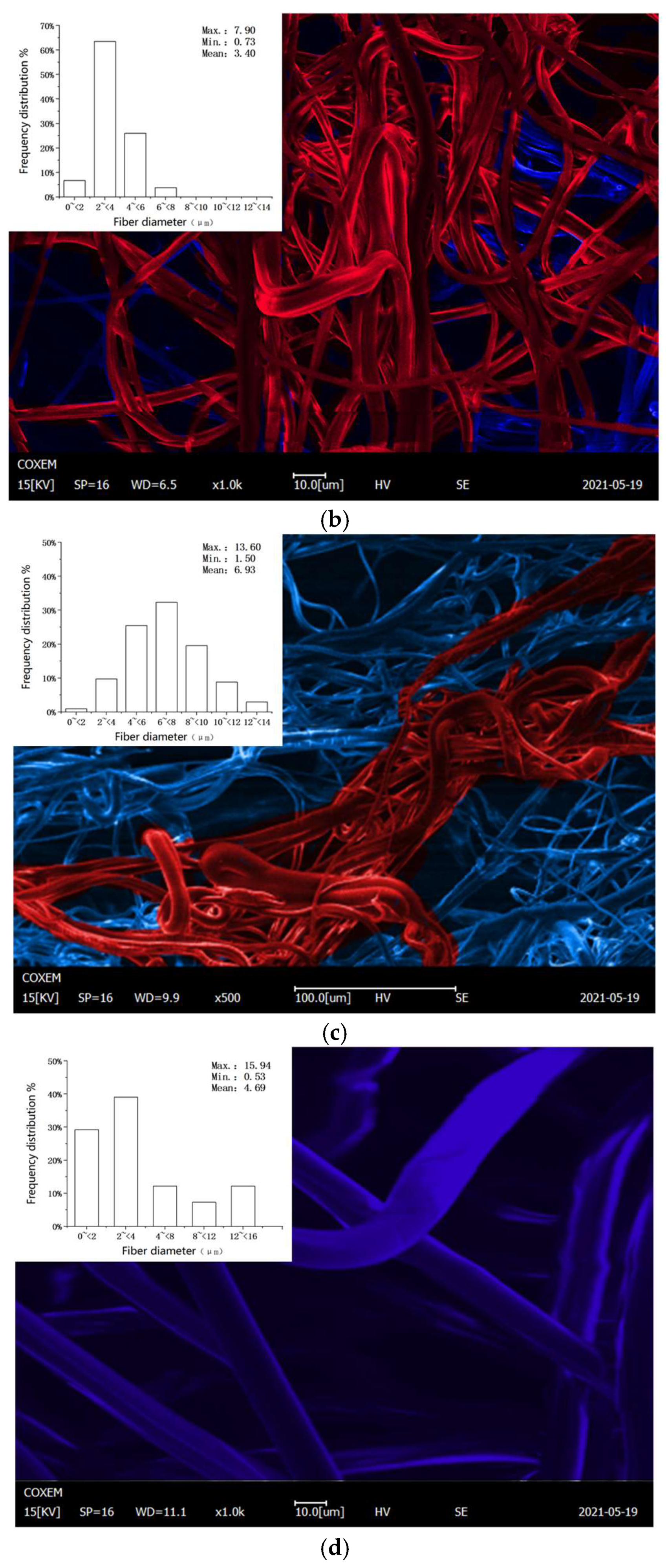
3.2. Microstructure
3.3. Model Building
4. Discussion
4.1. Variation of Filtration Efficiency
4.2. Changes in Microstructure
4.3. Feasibility of Neural Network Method Application
4.4. Feasibility of Dry Heat Disinfection
5. Conclusions
- (1)
- Heating temperature and duration will affect the respirator filtration efficiency. As the temperature and time increased, the decline in respirator filtration efficiency became more obvious.
- (2)
- Through the SEM images, it is clear that excessive temperature led to the increase in the fiber distribution inhomogeneity and the pore distribution range, reducing the filtration efficiency of the respirator.
- (3)
- The NARX neural network model exhibited an ideal fit. The model showed that the effect of dry heat treatment at 80 °C and 90 °C on the filtration efficiency of the respirator was limited when other factors were not considered. The respirator may have a surplus of filtration efficiency in the production process, therefore, the respirator may continue to be used after thermal disinfection at a certain temperature and duration. According to the predicted data of the neural network, it can be inferred that at 100 °C for 0.25 h, and above, the filtration efficiency of the respirator will no longer meet the requirement of GB 2626-2019.
- (4)
- The initial filtration efficiencies of different respirators are inconsistent, which will lead to different reductions in the filtration efficiency caused by dry heating. According to our experimental results, the heating disinfection temperature can be between 70 °C and 90 °C, and the heating time can be between 30 min and 2 h.
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Department of Planning Development; Informatization Health Commission. Statistical Bulletin of China Health Development. Available online: http://www.nhc.gov.cn/guihuaxxs/s10743/202107/af8a9c98453c4d9593e07895ae0493c8.shtml (accessed on 20 May 2022).
- Xiaobin, Y.; Jun, C.; Xin, Z. Particle size conversion for mask filter efficiency test and comparability of different standards. J. Text. Res. 2020, 41, 152–157, 171. [Google Scholar]
- Hongjie, P.; Xiaobin, Y.; Chuan, Z.; Shouxing, Z.; Suqin, C.; Hongseng, L. Comparison of filtration efficiency standards for COVID-19 protective masks. J. Text. Res. 2021, 42, 97–105. [Google Scholar]
- Jin, T.; Yiming, S. Effect of working dust on the protective performance of self-priming filter anti-particulate respirator. In Proceedings of the Collection of the 25th Cross-Strait and Hong Kong, Macau Occupational Safety and Health Academic Research Association and China Occupational Safety and Health Association Academic Annual Conference and Science and Technology Award Conference 2017, Urumqi, China, 20 September–22 September 2017. [Google Scholar]
- Asbach, C.; Held, A.; Kiendler-Scharr, A.; Scheuch, G.; Schmid, H.-J. Position Paper of the Gesellschaft für Aerosolforschung on Understanding the Role of Aerosol Particles in SARS-CoV-2 Infection; Gesellschaft für Aerosolforschung e. V.: Cologne, Germany, 2021. [Google Scholar]
- Zhou, S.S.; Lukula, S.; Chiossone, C.; Nims, R.W.; Suchmann, D.B.; Ijaz, M.K. Assessment of a respiratory face mask for capturing air pollutants and pathogens including human influenza and rhinoviruses. J. Thorac. Dis. 2018, 10, 2059–2069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abboah-Offei, M.; Salifu, Y.; Adewale, B.; Bayuo, J.; Ofosu-Poku, R.; Opare-Lokko, E.B.A. A rapid review of the use of face mask in preventing the spread of COVID-19. Int. J. Nurs. Stud. Adv. 2021, 3, 100013. [Google Scholar] [CrossRef] [PubMed]
- Tabatabaeizadeh, S. Airborne transmission of COVID-19 and the role of face mask to prevent it: A systematic review and meta-analysis. Eur. J. Med. Res. 2021, 26, 1. [Google Scholar] [CrossRef]
- Bo, Y.; Guo, C.; Lin, C.; Zeng, Y.; BiLi, H.; Zhang, Y. Effectiveness of non-pharmaceutical interventions on COVID-19 transmission in 190 countries from 23 January to 13 April 2020. Int. J. Infect. Dis. 2021, 102, 247–253. [Google Scholar] [CrossRef]
- Li, Y.; Liang, M.; Gao, L.; Ahmed, M.A.; Patrick, J.; Cheng, C.; Zhou, Q.; Sun, C. Face masks to prevent transmission of COVID-19: A systematic review and meta-analysis. Am. J. Infect. Control 2021, 49, 900–906. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Huang, A.; Li, Z.; Rimoin, A.W. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef] [PubMed]
- GB 2626-2019. Respiratory Protection—Non-Powered Air-Purifying Particle Respirator. State Administration for Market Regulation, National Standardization Administration: China, Beijing, 2019.
- China News Service. Nearly 800 People Were Infected in 9 Days, and There Is a Shortage of Masks, Protective Clothing, and Other Materials Here. Available online: https://m.gmw.cn/2022-05/18/content_1302953011.htm (accessed on 22 May 2022).
- Dharmaraj, S.; Ashokkumar, V.; Hariharan, S.; Manibharathi, A.; LokeShow, P.; Chong, C.T.; Ngamcharussrivichai, C. The COVID-19 pandemic face mask waste: A blooming threat to the marine environment. Chemosphere 2022, 287, 132411. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Lawson, J.; Hervé, R.; Jakob, H. Development of a rapid plasma decontamination system for decontamination and reuse of filtering facepiece respirators. AIP Adv. 2021, 11, 105311. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, D. Reuse of N95 masks. Engineering 2020, 6, 593. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Ikram, A.; Savul, S.; Lalani, F. Decontamination and Reuse of N95 Masks: A Narrative Review. Can. J. Infect. Dis. Med. Microbiol. 2020, 2020, 8869472. [Google Scholar] [CrossRef] [PubMed]
- Rutala, W.; Weber, D. Guideline for Disinfection and Sterilization in Healthcare Facilities. Available online: https://Stacks.cdc.gov (accessed on 22 May 2022).
- Pascoe, M.J.; Robertson, A.; Crayford, A.; Durand, E.; Steer, J.; Castelli, A.; Wesgate, R.; Evans, S.L.; Porch, A.; Maillard, J.-Y. Dry heat and microwave-generated steam protocols for the rapid decontamination of respiratory personal protective equipment in response to COVID-19-related shortages. J. Hosp. Infect. 2020, 106, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Joshi, S.; Venkatesan, S. A detailed investigation of N95 respirator sterilization with dry heat, hydrogen peroxide, and ionizing radiation. J. Ind. Text. 2022, 15280837221090663. [Google Scholar] [CrossRef]
- Wielick, C.; Ludwig-Begall, L.F.; Dams, L.; Razafimahefa, R.M.; Demeuldre, P.F.; Napp, A.; Laperre, J.; Jolois, O.; Farnire, F.; Haubruge, E.; et al. The use of germicidal ultraviolet light, vaporised hydrogen peroxide and dry heat to decontaminate face masks and filtering respirators contaminated with an infectious norovirus. Infect. Prev. Pract. 2021, 3, 100111. [Google Scholar] [CrossRef] [PubMed]
- Yim, W.; Cheng, D.; Patel, S.H.; Kou, R.; Meng, Y.S.; Jokerst, J.V. KN95, and N95 Respirators Retain Filtration Efficiency despite a Loss of Dipole Charge during Decontamination. ACS Appl. Mater. Interfaces 2020, 12, 54473–54480. [Google Scholar] [CrossRef]
- Seresirikachorn, K.; Phoophiboon, V.; Chobarporn, T.; Tiankanon, K.; Aeumjaturapat, S.; Chusakul, S.; Snidvongs, K. Decontamination and reuse of surgical masks and N95 filtering facepiece respirators during the COVID-19 pandemic: A systematic review. Infect. Control Hosp. Epidemiol. 2021, 42, 25–30. [Google Scholar] [CrossRef]
- Liao, L.; Xiao, W.; Zhao, M.; Yu, X.; Wang, H.; Wang, Q.; Chu, S.; Cui, Y. Can N95 respirators be reused after disinfection? How many times? ACS Nano 2020, 14, 6348–6356. [Google Scholar] [CrossRef]
- Doshi, S.; Banavar, S.P.; Flaum, E.; Kulkarni, S.; Vaidya, U.; Kumar, S.; Chen, T.; Bhattacharya, A.; Prakash, M. Applying heat and humidity using stove boiled water for decontamination of N95 respirators in low resource settings. PLoS ONE 2021, 16, e0255338. [Google Scholar] [CrossRef]
- Kumar, A.; Kasloff, S.; Leung, T.C.A.; Strong, J. Decontamination of N95 masks for re-use employing 7 widely available sterilization methods. PLoS ONE 2020, 15, e0243965. [Google Scholar] [CrossRef]
- Schwartz, A.; Stiege, M. Decontamination and reuse of N95 respirators with hydrogen peroxide vapor to address worldwide personal protective equipment shortages during the SARS-CoV-2 (COVID-19) pandemic. Appl. Biosaf. 2020, 25, 67–70. [Google Scholar] [CrossRef]
- Kenney, P.A.; Chan, B.K.; Kortright, K.E.; Cintron, M.; Russi, M.; Epright, J.; Lee, L.; Balcezak, T.J.; Havill, N.L.; Martinello, R.A. Hydrogen peroxide vapor decontamination of N95 respirators for reuse. Infect Control Hosp. Epidemiol. 2022, 43, 45–47. [Google Scholar] [CrossRef] [PubMed]
- Rosales, V.; Iglesias, C.; Viana, A.; Lorenzo, C.; Ghazanfari, S.; Magariños, B.; González, C.A.G. Supercritical CO2 sterilization: An effective treatment to reprocess FFP3 face masks and to reduce waste during COVID-19 pandemic. Sci. Total Environ. 2022, 826, 154089. [Google Scholar] [CrossRef] [PubMed]
- DeAngelis, H.; Grillet, A.; Nemer, M.; Wasiolek, M. Gamma radiation sterilization of N95 respirators leads to decreased respirator performance. PLoS ONE 2021, 16, e0248859. [Google Scholar] [CrossRef] [PubMed]
- Cramer, A.; Tian, E.; Sherry, H.; Galanek, M.; Lamere, E. Assessment of the qualitative fit test and quantitative single-pass filtration efficiency of disposable N95 masks following gamma irradiation. JAMA Netw. Open 2020, 3, e209961. [Google Scholar] [CrossRef]
- Golladay, G.J.; Leslie, K.A.; Zuelzer, W.A.; Cassano, A.D.; Plauny, J.J.; Daniels, F.E.; Bearman, G.; Kates, S.L. Rationale and process for N95 respirator sanitation and reuse in the coronavirus disease 2019 (COVID-19) pandemic. Infect. Control Hosp. Epidemiol. 2022, 43, 40–44. [Google Scholar] [CrossRef]
- Smith, J.S.; Hanseler, H.; Welle, J.; Rattray, R.; Campbell, M.; Brotherton, T.; Moudgil, T.; Pack, T.F.; Wegmann, K.; Jensen, S. Effect of various decontamination procedures on disposable N95 mask integrity and SARS-CoV-2 infectivity. J. Clin. Transl. Sci. 2021, 5, E10. [Google Scholar] [CrossRef]
- Kampf, G.; Todt, D.; Pfaender, S.; Steinmann, E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020, 104, 246–251. [Google Scholar] [CrossRef] [Green Version]
- Onofre, R.; CarmoBorges, R.; Demarco, G.; Dotto, L.; Schwendicke, F.; FernandoDemarco, F. Decontamination of N95 respirators against SARS-CoV-2: A scoping review. J. Dent. 2021, 104, 103534. [Google Scholar] [CrossRef]
- Cinquemani, C.; Boyle, C.; Bach, E.; Schollmeyer, E. Inactivation of microbes using compressed carbon dioxide—An environmentally sound disinfection process for medical fabrics. J. Supercrit. Fluids 2007, 42, 392–397. [Google Scholar] [CrossRef]
- Oh, C.; Araud, E.; Puthussery, J.V.; Bai, H.; Clark, G.G.; Wang, L.; Verma, V.; Nguyen, T.H. Dry heat as a decontamination method for N95 respirator reuse. Environ. Sci. Technol. Lett. 2020, 7, 677–682. [Google Scholar] [CrossRef]
- Kobayashi, L.M.; Marins, B.R.; dos Santos Costa, P.C.; Perazzo, H.; Castro, R. Extended use or reuse of N95 respirators during COVID-19 pandemic: An overview of national regulatory authority recommendations. Infect. Control Hosp. Epidemiol. 2020, 41, 1364–1366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, W.; Pan, B.; Kan, H. Evaluation of heat inactivation of virus contamination on medical mask. J. Microbes Infect. 2020, 15, 31–35. (In Chinese) [Google Scholar]
- Office of the National HealthCommission; Office of the State Administration of Traditional Chinese. Medicine Diagnosis and Treatment Scheme for Novel Coronavirus Pneumonia (Trial Version 5). Available online: http://www.nhc.gov.cn/yzygj/s7653p/202002/3b09b894ac9b4204a79db5b8912d4440.shtml (accessed on 5 May 2022).
- Chan, K.H.; Peiris, J.S.M.; Lam, S.Y.; Poon, L.L.M.; Yuen, K.Y.; Seto, W.H. The Effects of Temperature and Relative Humidity on the Viability of the SARS Coronavirus. Adv. Virus Res. 2011, 2011, 734690. [Google Scholar] [CrossRef] [PubMed]
- Martinez, E.; Crèvecoeur, S.; Dams, L.; Rabecki, F.; Habraken, S.; Daube, E.H.G. Effect of five decontamination methods on face masks and filtering facepiece respirators contaminated with Staphylococcus aureus and Pseudomonas aeruginosa. Access Microbiol. 2022, 4, 000342. [Google Scholar] [CrossRef]
- Casanova, L.M.; Jeon, S.; Rutala, W.A.; Weber, D.J.; Sobsey, M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010, 76, 2712–2717. [Google Scholar] [CrossRef] [Green Version]
- Sales, E.; Mulatier, N.; Wittmann, L.; Fernandes, A.; Vacher, B.; Penuelas, J. Effect of dry heat treatment between room temperature and 160 °C on surgical masks. Mater. Lett. 2022, 308, 131270. [Google Scholar] [CrossRef]
- Viscusi, D.J.; King, W.P.; Shaffer, R.E. Effect of decontamination on the filtration efficiency of two filtering facepiece respirator models. J. Int. Soc. Respir. Prot. 2007, 24, 93. [Google Scholar]
- Application Note AFT-008 Rev.A-(A4). TSI® Instrumentation for measuring submicron particle filtration of barrier face coverings to ASTM F3502. TSI Incorporated: Shoreview, MN, USA, 2021.
- Qi, S.; Hongzhan, L. Research on Magnetorheological Damper Model Based on NARX Neural Network. Modul. Mach. Tool Autom. Manuf. Tech. 2021, 2, 9–13. (In Chinese) [Google Scholar]
- Longhui, Z.; Zhengfeng, L.; Naxin, W.; Xiaofeng, K.; Yali, F. Computation for motion on truncated point of mooring line based on Narx network. Ship Mech. 2019, 23, 936–947. (In Chinese) [Google Scholar]
- Si, C. Study on Structure and Filtration Properties of Polypropylene Melt-blown Nonwoven; Zhejiang Sci-Tech University: Hangzhou, China, 2020. [Google Scholar]
- Cheng, S.; Muhaiminul, A.S.M.; Yue, Z.; Wang, Y.; Xiao, Y.; Militky, J.; Prasad, M.; Zhu, G. Effect of Temperature on the Structure and Filtration Performance of Polypropylene Melt-Blown Nonwovens. Autex Res. J. 2021, 21, 207–217. [Google Scholar] [CrossRef]
- Liu, C.; Dai, Z.; He, B.; Ke, Q. -F. The Effect of Temperature and Humidity on the Filtration Performance of Electret Melt-Blown Nonwovens. Materials 2020, 13, 4774. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.H., M.; Liu, L.; Liu, Y.; Tsai, P.; Chen, Z. Protective effect of masks on COVID-19 and methods of sterilization for the purpose of reuse. Melliand China 2020, 48, 42–46+52. (In Chinese) [Google Scholar]




| Particle | Concentration | MMD * | NMD * |
|---|---|---|---|
| DOP | 50–200 mg/m3 | 0.33 μm | 0.20 μm |
| NaCl | 12–20 mg/m3 | 0.26 μm | 0.075 μm |
| Training Regression (R) | Validation Regression (R) | Test Regression (R) | All Regression (R) |
|---|---|---|---|
| 0.86 | 0.90 | 0.88 | 0.87 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jin, Z.; Sun, C.; Wu, W.; Yang, X. Dry Heat as a Potential Decontamination Method on the Filtration Efficiency of Filtering Facepiece Respirators. Int. J. Environ. Res. Public Health 2022, 19, 7167. https://doi.org/10.3390/ijerph19127167
Jin Z, Sun C, Wu W, Yang X. Dry Heat as a Potential Decontamination Method on the Filtration Efficiency of Filtering Facepiece Respirators. International Journal of Environmental Research and Public Health. 2022; 19(12):7167. https://doi.org/10.3390/ijerph19127167
Chicago/Turabian StyleJin, Zhixu, Chenchen Sun, Wending Wu, and Xiaobing Yang. 2022. "Dry Heat as a Potential Decontamination Method on the Filtration Efficiency of Filtering Facepiece Respirators" International Journal of Environmental Research and Public Health 19, no. 12: 7167. https://doi.org/10.3390/ijerph19127167
APA StyleJin, Z., Sun, C., Wu, W., & Yang, X. (2022). Dry Heat as a Potential Decontamination Method on the Filtration Efficiency of Filtering Facepiece Respirators. International Journal of Environmental Research and Public Health, 19(12), 7167. https://doi.org/10.3390/ijerph19127167





