Process Evaluation of a Comprehensive Intervention for the Early Detection and Prevention of Oral Cancer: A Mixed Methods Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
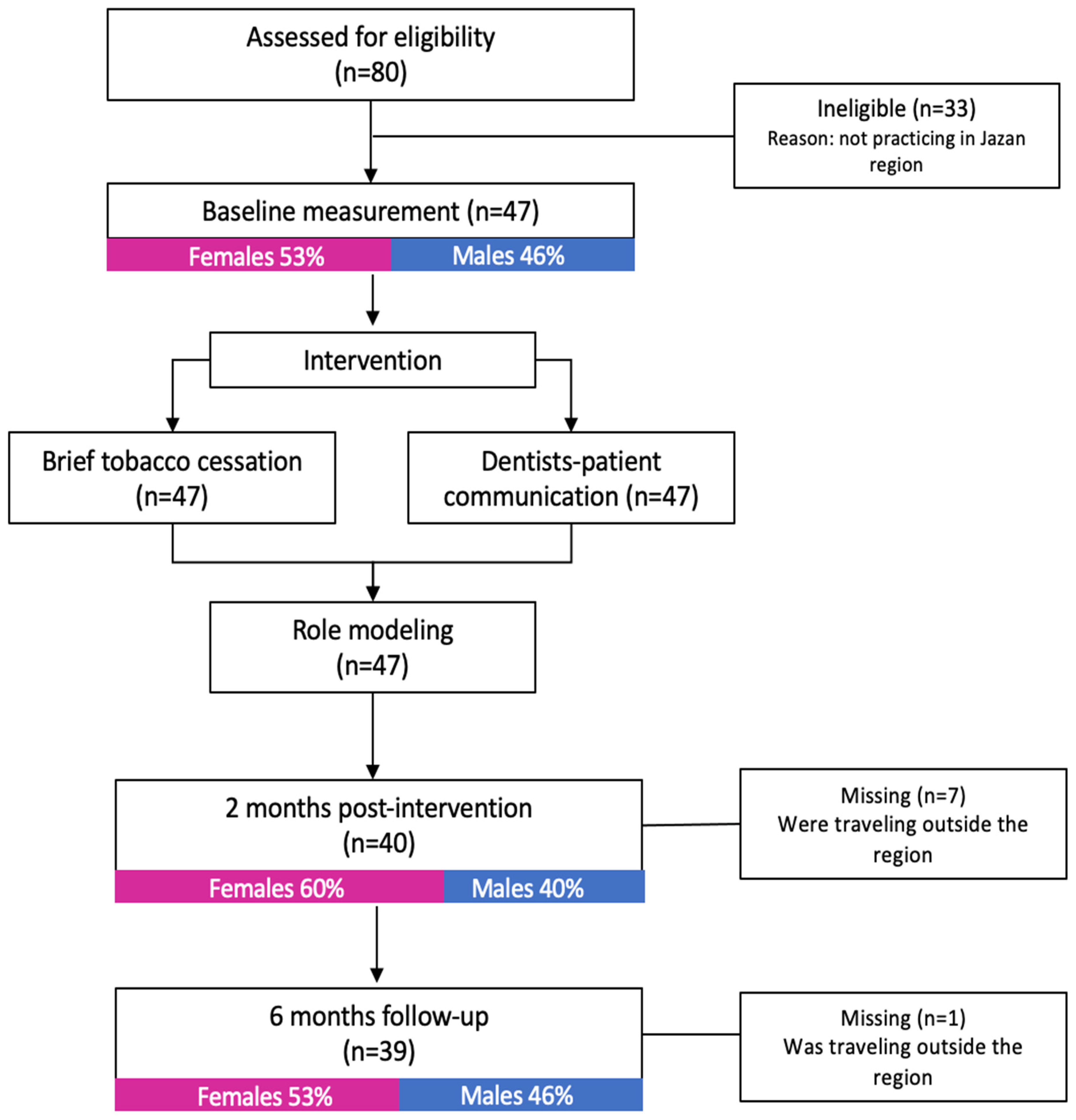
2.2. Setting and Participants
2.3. The ISAC Intervention
2.4. Data Collection for the Process Components
2.5. Data Analysis
3. Results
3.1. Reach
3.2. Dose Delivered
3.3. Dose Received
3.4. Recruitment
3.5. Fidelity
3.6. Satisfaction
“I have already recommended the ISAC to all my colleagues, as they have seen how the ISAC has greatly improved my confidence and skills”.
3.7. Context
“I hope all dental clinics focus on implementing oral-cancer examinations as much as they care about their financial profits”.
“I think the ISAC would be easier to follow by all dentists if the ISAC was integrated into the clinical software”.
“If I practice in a rural area, where I have no assistant, I think it will be challenging for me. Maybe it would be useful if the ISAC was somehow modified to account for this”, “…I would prefer to have a supporting tool that can help me when I practice alone”.
“If it’s implemented at a national level, definitely everybody would practice it”.
“We really need the ISAC to be part of the university’s continuous education course”, “we hope that Jazan University and the Ministry of Health continuously offer this intervention to every dentist in Saudi Arabia”.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miranda-Filho, A.; Bray, F. Global patterns and trends in cancers of the lip, tongue and mouth. Oral Oncol. 2020, 102, 104551. [Google Scholar] [CrossRef]
- Warnakulasuriya, S.; Kerr, A.R. Oral Cancer Screening: Past, Present, and Future. J. Dent. Res. 2021, 100, 1313–1320. [Google Scholar] [CrossRef] [PubMed]
- Alshehri, B.M. Trends in the incidence of oral cancer in Saudi Arabia from 1994 to 2015. World J. Surg. Onc. 2020, 18, 1–6. [Google Scholar] [CrossRef]
- Bakdash, A. Shammah (Smokeless Tobacco) and Public Health. Asian Pac. J. Cancer Prev. 2017, 18, 1183. [Google Scholar] [CrossRef]
- Brocklehurst, P.; Kujan, O.; O’Malley, L.A.; Ogden, G.; Shepherd, S.; Glenny, A.M. Screening programmes for the early detection and prevention of oral cancer. Cochrane Database Syst. Rev. 2013, 11, CD004150. [Google Scholar]
- Jafer, M.; Crutzen, R.; Halboub, E.; Moafa, I. Dentists Behavioral Factors Influencing Early Detection of Oral Cancer: Direct Clinical Observational Study. J. Canc Educ. 2020, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Jafer, M.; Crutzen, R.; Moafa, I.; van den Borne, B. What Do Dentists and Dental Students Think of Oral Cancer and Its Control and Prevention Strategies? A Qualitative Study in Jazan Dental School. J. Cancer Educ. 2021, 36, 134–142. [Google Scholar] [CrossRef] [Green Version]
- Jafer, M.; Crutzen, R.; Ibrahim, A.; Moafa, I.; Zaylaee, H.; Ajeely, M.; van den Borne, B.; Zanza, A.; Testarelli, L.; Patil, S. Using the Exploratory Sequential Mixed Methods Design to Investigate Dental Patients’ Perceptions and Needs Concerning Oral Cancer Information, Examination, Prevention and Behavior. Int. J. Environ. Res. Public Health 2021, 18, 7562. [Google Scholar] [CrossRef] [PubMed]
- Jafer, M.; Moafa, I.; Cruitzen, R.; Van Den Borne, B. Using Intervention Mapping to Develop ISAC, a Comprehensive Intervention for Early Detection and Prevention of Oral Cancer in Saudi Arabia. J. Cancer Educ. 2022, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.E.; Ruiter, R.A.C.; Markham, C.M.; Kok, G. Intervention Mapping: Theory- and Evidence-Based Health Promotion Program Planning: Perspective and Examples. Front. Public Health 2019, 7, 209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steckler, A.B.; Linnan, L. Process Evaluation for Public Health Interventions and Research; John Wiley: Hoboken, NJ, USA, 2014. [Google Scholar]
- Saunders, R.P.; Evans, M.H.; Joshi, P. Developing a process evaluation plan for assessing health promotion program implementation: A how to guide. Health Promot. Pract. 2005, 6, 134–147. [Google Scholar] [CrossRef] [PubMed]
- Moafa, I.; Hoving, C.; Van Den Borne, B.; Jafer, M. Dentists’ Perceptions and Usability Testing toward the Implementation of ISAC, a Comprehensive Oral Cancer Intervention in Dental Practices: A Qualitative Study in Jazan Region, Saudi Arabia. BMC Health Serv. Res. 2022, 22, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Toolkit for Oral Health Professional to Deliver Brief Tobacco Interventions in Primary Care. World Health Organization, 2017. Available online: https://www.who.int/publications-detail-redirect/toolkit-for-oral-health-professional-to-deliver-brief-tobacco-interventions-in-primary-care (accessed on 1 September 2020).
- Patient Communications: A Guide for Dentists—Canadian Dental Association. Available online: https://www.cda-adc.ca/_files/practice/practice_management/patient_communications/guides/dentalguide-ns.pdf (accessed on 1 September 2020).
- Oral Cancer Clinical Practice Guideline—CDSBC. Guideline for the Early Detection of Oral Cancer in British Columbia. 2008. Available online: https://www.cdsbc.org/CDSBCPublicLibrary/Oral-Cancer-Clinical-Practice-Guideline.pdf (accessed on 1 September 2020).
- Roberts, K.; Dowell, A.; Nie, J.B. Attempting rigour and replicability in thematic analysis of qualitative research data; a case study of codebook development. BMC Med. Res. Methodol. 2019, 19, 66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arora, A.K.; Rodriguez, C.; Carver, T.; Teper, M.H.; Rojas-Rozo, L.; Schuster, T. Evaluating Usability in Blended Learning Programs Within Health Professions Education: A Scoping Review. Med. Sci. Educ. 2021, 31, 1213–1246. [Google Scholar] [CrossRef]
- Whitelock, D.; Jelfs, A. Editorial for special issues on blended learning: Blending the issues and concerns of staff and students. J. Educ. Media 2003, 28, 99–100. [Google Scholar]
- Cappi, V.; Artioli, G.; Ninfa, E. The use of blended learning to improve health professionals’ communication skills: A literature review. Acta. Biomed. 2019, 90, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Al-Fodeh, R.S.; Alwahadni, A.M.; Abu Alhaija, E.S.; Bani-Hani, T.; Ali, K.; Daher, S.O.; Daher, H.O. Quality, effectiveness and outcome of blended learning in dental education during the Covid pandemic: Prospects of a post-pandemic implementation. Educ. Sci. 2021, 11, 810. [Google Scholar] [CrossRef]
- Hakanen, J.J.; Bakker, A.B.; Demerouti, E. How dentists cope with their job demands and stay engaged: The moderating role of job resources. Eur. J. Oral. Sci. 2005, 113, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Bird, M.; McGillion, M.; Chambers, E.M.; Dix, J.; Fajardo, C.J.; Gilmour, M.A.; Levesque, K.; Lim, A.; Mierdel, S.; Quellette, C.; et al. generative co-design framework for healthcare innovation: Development and application of an end-user engagement framework. Res. Involv. Engagem. 2021, 7, 12. [Google Scholar] [CrossRef] [PubMed]
- Larson, R.B. Controlling social desirability bias. J. Mark. Res. Soc. 2019, 61, 534–547. [Google Scholar] [CrossRef]
| Session Number | Session Name | Content |
|---|---|---|
|
Session 1.1 n = 47 | Tobacco-Cessation Counselling | Didactic: discussing the importance of tobacco counseling, the role of health professionals in general and dentists in particular, the uniqueness of dental setting in tobacco-cessation activities, and an overview of the common approaches used in tobacco-cessation counseling, as well as common theoretical and evidence-based models explaining the patient current stage in the decision-making process. |
|
Session 1.2 n = 47 | Practical: role modeling and training of the trainers (TOT) approach to providing encouragement and capacity-building assistance for tobacco-cessation counseling. | |
|
Session 2 n = 47 | Patient Communication | Role modeling and TOT by regional expert on patient-communications skills |
|
Session 3.1 n = 47 | The ISAC Modeling | Didactic: general and local OC epidemiology, general and local OC risk factors and their effects, full OC screening and referral to OC procedures (if needed), and biopsy taking, with an emphasis on patient education and practical examples, as well as introducing the ISAC method and tobacco-cessation services. |
|
Session 3.2 n = 47 | Practical: role modeling by the trainer (performing the ISAC), interns engaging in a role-play where they apply the ISAC on each other in two groups—the first group practices and the second group observes, and vice versa. This is followed by providing tailored feedback to each other, under the supervision of a trainer who will provide positive comments. |
| Intervention Component | Satisfaction Mean (SD) | Perceived Benefits Mean (SD) | Perceived Difficulty Mean (SD) |
|---|---|---|---|
| Tobacco-cessation counseling | 9.18 (0.91) | 9.92 (0.27) | 2.21 (1.80) |
| Patient communication | 9.28 (0.94) | 9.95 (0.22) | 0.79 (0.76) |
| The ISAC modeling | 9.77 (0.58) | 9.95 (0.22) | 0.51 (0.88) |
| Overall participation in the ISAC | 9.62 (0.54) | 9.72 (0.45) | 1.15 (1.26) |
| Participating in the ISAC Intervention Has Helped Me in: | Mean (SD) |
|---|---|
| Knowing more about oral cancer problems | 3.69 (0.47) |
| Better understanding my role in preventing and detecting oral cancer | 3.92 (0.27) |
| Feeling more confident in my ability to perform complete oral-cancer examinations | 3.95 (0.22) |
| Feeling more confident in my ability to perform patient education and in tobacco-cessation counseling | 3.72 (0.45) |
| Feeling more confident in my soft patient-communication skills | 3.64 (0.48) |
| Performing complete oral-cancer examinations | 3.95 (0.22) |
| Taking biopsies from a suspicious lesion | 3.38 (0.63) |
| Educating and training patients on oral cancer self-examination | 3.95 (0.22) |
| Providing brief tobacco-cessation counseling to my patients | 3.74 (0.44) |
| Know-how and where I can refer patients for specialized treatments | 3.79 (0.40) |
| Intervention Implementation | Main Findings |
|---|---|
| Reach |
|
| Dose received |
|
| Dose delivered |
|
| Fidelity |
|
| Satisfaction |
|
| Contamination |
|
| Context |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moafa, I.; Jafer, M.; Van Den Borne, B.; Hoving, C. Process Evaluation of a Comprehensive Intervention for the Early Detection and Prevention of Oral Cancer: A Mixed Methods Study. Int. J. Environ. Res. Public Health 2022, 19, 7120. https://doi.org/10.3390/ijerph19127120
Moafa I, Jafer M, Van Den Borne B, Hoving C. Process Evaluation of a Comprehensive Intervention for the Early Detection and Prevention of Oral Cancer: A Mixed Methods Study. International Journal of Environmental Research and Public Health. 2022; 19(12):7120. https://doi.org/10.3390/ijerph19127120
Chicago/Turabian StyleMoafa, Ibtisam, Mohammed Jafer, Bart Van Den Borne, and Ciska Hoving. 2022. "Process Evaluation of a Comprehensive Intervention for the Early Detection and Prevention of Oral Cancer: A Mixed Methods Study" International Journal of Environmental Research and Public Health 19, no. 12: 7120. https://doi.org/10.3390/ijerph19127120
APA StyleMoafa, I., Jafer, M., Van Den Borne, B., & Hoving, C. (2022). Process Evaluation of a Comprehensive Intervention for the Early Detection and Prevention of Oral Cancer: A Mixed Methods Study. International Journal of Environmental Research and Public Health, 19(12), 7120. https://doi.org/10.3390/ijerph19127120






