Modifiable Resources and Resilience in Racially and Ethnically Diverse Older Women: Implications for Health Outcomes and Interventions
Abstract
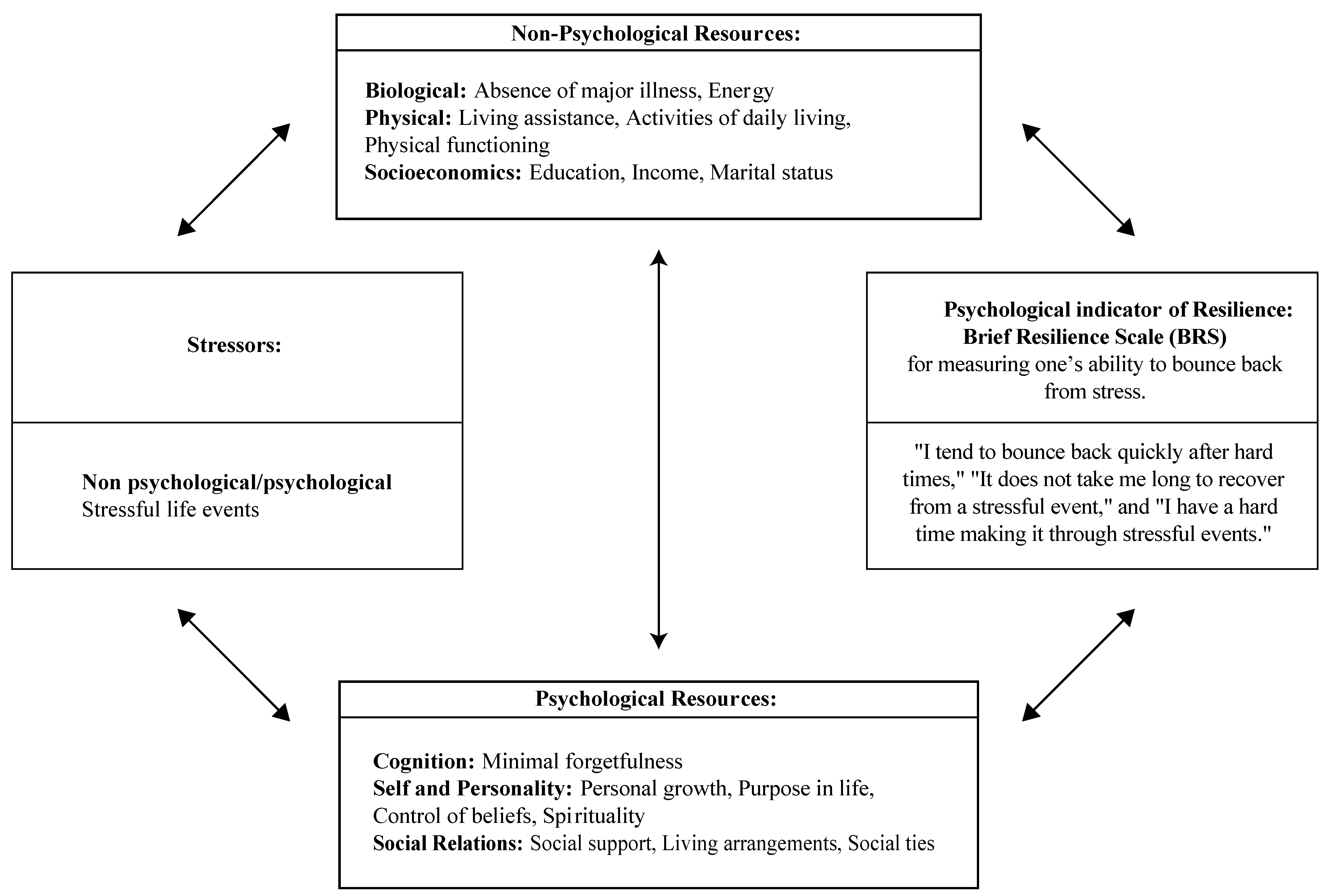
:1. Introduction
2. Methods
2.1. Design and Study Population
2.2. Measures
2.3. Statistical Analysis
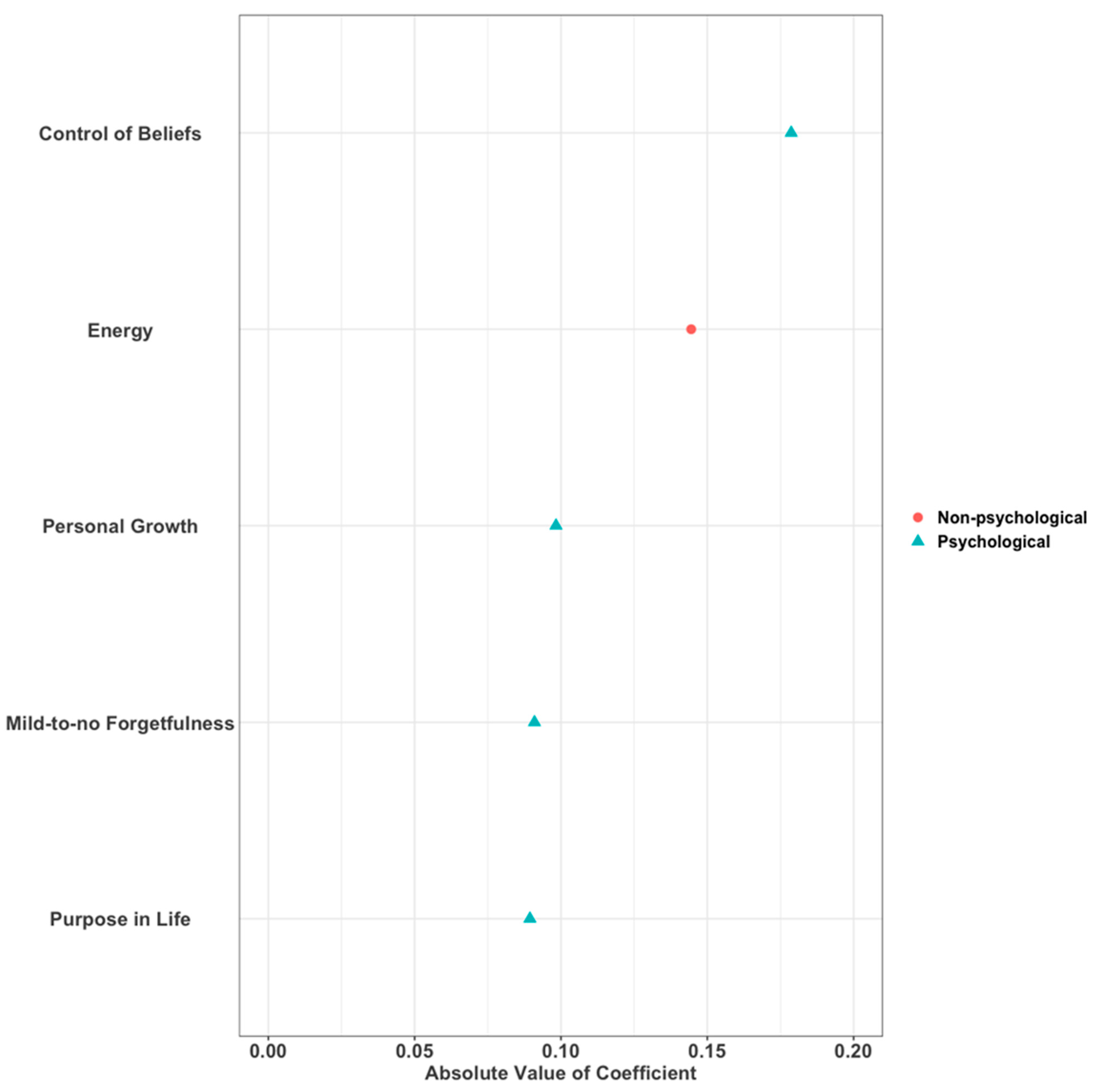
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Masten, A.S. Ordinary magic: Resilience processes in development. Am. Psychol. 2001, 56, 227–238. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S.; Garmezy, N. Risk, vulnerability, and protective factors in developmental psychopathology. In Advances in Clinical Child Psychology; Springer: Berlin/Heidelberg, Germany, 1985; pp. 1–52. [Google Scholar]
- Staudinger, U.M.; Greve, W. Resilience and Aging. Encyclopedia of Geropsychology; Springer: New York, NY, USA, 2015; pp. 1–9. [Google Scholar]
- Rutter, M. Resilience as a dynamic concept. Dev. Psychopathol. 2012, 24, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Woods, N.F.; Rillamas-Sun, E.; Cochrane, B.B.; La Croix, A.Z.; Seeman, T.E.; Tindle, H.A.; Zaslavsky, O.; Bird, C.E.; Johnson, K.C.; Manson, J.E. Aging well: Observations from the Women’s Health Initiative study. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2016, 71 (Suppl. 1), S3–S12. [Google Scholar] [CrossRef] [PubMed]
- Hildon, Z.; Montgomery, S.M.; Blane, D.; Wiggins, R.D.; Netuveli, G. Examining resilience of quality of life in the face of health-related and psychosocial adversity at older ages: What is “right” about the way we age? Gerontologist 2009, 50, 36–47. [Google Scholar] [CrossRef] [PubMed]
- Nygren, B.; Aléx, L.; Jonsén, E.; Gustafson, Y.; Norberg, A.; Lundman, B. Resilience, sense of coherence, purpose in life and self-transcendence in relation to perceived physical and mental health among the oldest old. Aging Ment. Health 2005, 9, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Council, N.R. Preparing for an Aging World: The Case for cross-National Research; National Academies Press (US): Washington, DC, USA, 2001. [Google Scholar]
- National Research Council; Committee on Population. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life; National Academies Press: Washington, DC, USA, 2004. [Google Scholar]
- Lutz, L.J.; Gaffney-Stomberg, E.; Williams, K.W.; McGraw, S.M.; Niro, P.J.; Karl, J.P.; Cable, S.J.; Cropper, T.L.; McClung, J.P. Adherence to the dietary guidelines for americans is associated with psychological resilience in young adults: A cross-sectional study. J. Acad. Nutr. Diet. 2017, 117, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, A.L.; Faulkner, B.; Wekerle, C. The relationship among internal resilience, smoking, alcohol use, and depression symptoms in emerging adults transitioning out of child welfare. Child Abus. Negl. 2013, 37, 22–32. [Google Scholar] [CrossRef]
- Tsourtos, G.; Ward, P.R.; Miller, E.R.; Hill, K.; Barton, C.; Wilson, C.J.; Woodman, R. Does Resilience Moderate the Relationship Between Stress and Smoking Status? Subst. Use Misuse 2019, 54, 412–425. [Google Scholar] [CrossRef]
- Hegberg, N.J.; Tone, E.B. Physical activity and stress resilience: Considering those at-risk for developing mental health problems. Ment. Health Phys. Act. 2015, 8, 1–7. [Google Scholar] [CrossRef]
- Springfield, S.; Qin, F.; Hedlin, H.; Eaton, C.B.; Rosal, M.C.; Taylor, H.; Staudinger, U.M.; Stefanick, M.L. Resilience and CVD-protective Health Behaviors in Older Women: Examining Racial and Ethnic Differences in a Cross-Sectional Analysis of the Women’s Health Initiative. Nutrients 2020, 12, 2107. [Google Scholar] [CrossRef]
- McCuistion, T.S. The Relationship Between Resilience and Sleep Quality. Master’s Thesis, Abilene Christian University, Abilene, TX, USA, 2016. [Google Scholar]
- Hughes, J.M.; Ulmer, C.S.; Hastings, S.N.; Gierisch, J.M.; Workgroup, M.-A.V.M.; Howard, M.O. Sleep, resilience, and psychological distress in United States military Veterans. Mil. Psychol. 2018, 30, 404–414. [Google Scholar] [CrossRef] [PubMed]
- Coronado, P.; Oliva, A.; Fasero, M.; Piñel, C.; Herraiz, M.; Pérez-López, F. Resilience and related factors in urban, mid-aged Spanish women. Climacteric 2015, 18, 867–872. [Google Scholar] [CrossRef] [PubMed]
- DeNisco, S. Exploring the relationship between resilience and diabetes outcomes in African Americans. J. Am. Acad. Nurse Pract. 2011, 23, 602–610. [Google Scholar] [CrossRef] [PubMed]
- Arrebola-Moreno, A.L.; Garcia-Retamero, R.; Catena, A.; Marfil-Álvarez, R.; Melgares-Moreno, R.; Ramírez-Hernández, J.A. On the protective effect of resilience in patients with acute coronary syndrome. Int. J. Clin. Health Psychol. 2014, 14, 111–119. [Google Scholar] [CrossRef]
- Brondolo, E. Racial and ethnic disparities in health: Examining the contexts that shape resilience and risk. Psychosom. Med. 2015, 77, 2–5. [Google Scholar] [CrossRef]
- Geronimus, A.T.; Hicken, M.T.; Pearson, J.A.; Seashols, S.J.; Brown, K.L.; Cruz, T.D. Do US black women experience stress-related accelerated biological aging? Hum. Nat. 2010, 21, 19–38. [Google Scholar] [CrossRef]
- Sternthal, M.J.; Slopen, N.; Williams, D.R. Racial disparities in health: How much does stress really matter? Du Bois Rev. 2011, 8, 95–113. [Google Scholar] [CrossRef]
- Chyu, L.; Upchurch, D.M. Racial and ethnic patterns of allostatic load among adult women in the United States: Findings from the National Health and Nutrition Examination Survey 1999–2004. J. Women’s Health 2011, 20, 575–583. [Google Scholar] [CrossRef]
- Upchurch, D.M.; Stein, J.; Greendale, G.A.; Chyu, L.; Tseng, C.-H.; Huang, M.-H.; Lewis, T.T.; Kravitz, H.M.; Seeman, T. A longitudinal investigation of race, socioeconomic status, and psychosocial mediators of allostatic load in midlife women: Findings from the study of women’s health across the nation. Psychosom. Med. 2015, 77, 402–412. [Google Scholar] [CrossRef]
- O’Rourke, N. Psychological resilience and the well-being of widowed women. Ageing Int. 2004, 29, 267–280. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Galea, S.; Bucciarelli, A.; Vlahov, D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J. Consult. Clin. Psychol. 2007, 75, 671–682. [Google Scholar] [CrossRef] [PubMed]
- Lamond, A.J.; Depp, C.A.; Allison, M.; Langer, R.; Reichstadt, J.; Moore, D.J.; Golshan, S.; Ganiats, T.G.; Jeste, D.V. Measurement and predictors of resilience among community-dwelling older women. J. Psychiatr. Res. 2008, 43, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Finan, P.H.; Garland, E.L. The role of positive affect in pain and its treatment. Clin. J. Pain 2015, 31, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Sabayan, B.; Oleksik, A.M.; Maier, A.B.; Buchem, M.A.; Poortvliet, R.K.; Ruijter, W.; Gussekloo, J.; Craen, A.J.; Westendorp, R.G. High blood pressure and resilience to physical and cognitive decline in the oldest old: The Leiden 85-plus study. J. Am. Geriatr. Soc. 2012, 60, 2014–2019. [Google Scholar] [CrossRef] [PubMed]
- Clauss-Ehlers, C.S.; Yang, Y.-T.T.; Chen, W.-C.J. Resilience from childhood stressors: The role of cultural resilience, ethnic identity, and gender identity. J. Infant Child Adolesc. Psychother. 2006, 5, 124–138. [Google Scholar]
- Follins, L.D.; Walker, J.N.J.; Lewis, M.K. Resilience in Black lesbian, gay, bisexual, and transgender individuals: A critical review of the literature. J. Gay Lesbian Ment. Health 2014, 18, 190–212. [Google Scholar] [CrossRef]
- Davis, S.M. The “Strong Black Woman Collective”: A developing theoretical framework for understanding collective communication practices of Black women. Women’s Stud. Commun. 2015, 38, 20–35. [Google Scholar] [CrossRef]
- Van Wormer, K.; Sudduth, C.; Jackson, D.W., III. What we can learn of resilience from older African-American women: Interviews with women who worked as maids in the deep south. J. Hum. Behav. Soc. Environ. 2011, 21, 410–422. [Google Scholar] [CrossRef]
- Lavretsky, H. Resilience and Aging: Research and Practice; JHU Press: Baltimore, MD, USA, 2014. [Google Scholar]
- Windle, G. What is resilience? A review and concept analysis. Rev. Clin. Gerontol. 2011, 21, 152–169. [Google Scholar] [CrossRef]
- MacLeod, S.; Musich, S.; Hawkins, K.; Alsgaard, K.; Wicker, E.R. The impact of resilience among older adults. Geriatr. Nurs. 2016, 37, 266–272. [Google Scholar] [CrossRef]
- Assari, S. Unequal gain of equal resources across racial groups. Int. J. Health Policy Manag. 2018, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Staudinger, U.M. The positive plasticity of adult development: Potential for the 21st century. Am. Psychol. 2020, 75, 540–553. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Ruberman, W.; Weinblatt, E.; Goldberg, J.D.; Chaudhary, B.S. Psychosocial influences on mortality after myocardial infarction. N. Engl. J. Med. 1984, 311, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Berkman, L.F. Assessing the physical health effects of social networks and social support. Annu. Rev. Public Health 1984, 5, 413–432. [Google Scholar] [CrossRef]
- Berkman, L.F. Social networks, support, and health: Taking the next step forward. Am. J. Epidemiol. 1986, 123, 559–562. [Google Scholar] [CrossRef]
- Ryff, C.D. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Pers. Soc. Psychol. 1989, 57, 1069. [Google Scholar] [CrossRef]
- Ryff, C.D.; Keyes, C.L.M. The structure of psychological well-being revisited. J. Pers. Soc. Psychol. 1995, 69, 719. [Google Scholar] [CrossRef]
- Smith, B.W.; Epstein, E.M.; Ortiz, J.A.; Christopher, P.J.; Tooley, E.M. The foundations of resilience: What are the critical resources for bouncing back from stress? In Resilience in Children, Adolescents, and Adults; Springer: Berlin/Heidelberg, Germany, 2013; pp. 167–187. [Google Scholar]
- Zou, H.; Hastie, T. Regularization and variable selection via the elastic net. J. R. Stat. Soc. Ser. B Stat. Methodol. 2005, 67, 301–320. [Google Scholar] [CrossRef]
- Harrell, F.E., Jr. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis; Springer: Berlin/Heidelberg, Germany, 2015. [Google Scholar]
- Amireault, S.; Godin, G. The Godin-Shephard leisure-time physical activity questionnaire: Validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Percept. Mot. Ski. 2015, 120, 604–622. [Google Scholar] [CrossRef] [PubMed]
- Richardson, G.E. The metatheory of resilience and resiliency. J. Clin. Psychol. 2002, 58, 307–321. [Google Scholar] [CrossRef] [PubMed]
- Szymanski, D.M.; Stewart, D.N. Racism and sexism as correlates of African American women’s psychological distress. Sex Roles 2010, 63, 226–238. [Google Scholar] [CrossRef]
- Beal, F.M. Double jeopardy: To be Black and female. Meridians 2008, 8, 166–176. [Google Scholar] [CrossRef]
- Geronimus, A.T. Understanding and eliminating racial inequalities in women’s health in the United States: The role of the weathering conceptual framework. J. Am. Med. Women’s Assoc. (1972) 2001, 56, 133–136, 149–150. [Google Scholar]
- Beaulac, J.; Kristjansson, E.; Cummins, S. Peer reviewed: A systematic review of food deserts, 1966–2007. Prev. Chronic Dis. 2009, 6, A105. [Google Scholar]
- Feagin, J.; Bennefield, Z. Systemic racism and US health care. Soc. Sci. Med. 2014, 103, 7–14. [Google Scholar] [CrossRef]
- Nuru-Jeter, A.; Dominguez, T.P.; Hammond, W.P.; Leu, J.; Skaff, M.; Egerter, S.; Jones, C.P.; Braveman, P. “It’s the skin you’re in”: African-American women talk about their experiences of racism. An exploratory study to develop measures of racism for birth outcome studies. Matern. Child Health J. 2009, 13, 29. [Google Scholar] [CrossRef]
- Noonan, A.S.; Velasco-Mondragon, H.E.; Wagner, F.A. Improving the health of African Americans in the USA: An overdue opportunity for social justice. Public Health Rev. 2016, 37, 12. [Google Scholar] [CrossRef]
- Shorter-Gooden, K. Multiple resistance strategies: How African American women cope with racism and sexism. J. Black Psychol. 2004, 30, 406–425. [Google Scholar] [CrossRef]
- Woods-Giscombé, C.L.; Lobel, M. Race and gender matter: A multidimensional approach to conceptualizing and measuring stress in African American women. Cult. Divers. Ethn. Minority Psychol. 2008, 14, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Goodkind, J.R.; Hess, J.M.; Gorman, B.; Parker, D.P. “We’re Still in a Struggle” Diné Resilience, Survival, Historical Trauma, and Healing. Qual. Health Res. 2012, 22, 1019–1036. [Google Scholar] [CrossRef] [PubMed]
- Taylor, H.A., Jr.; Washington-Plaskett, T.; Quyyumi, A.A. Black Resilience-Broadening the Narrative and the Science on Cardiovascular Health and Disease Disparities. Ethn. Dis. 2020, 30, 365–368. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.M.; Spencer, Z.; Wilson, S.K. I am not your felon: Decoding the trauma, resilience, and recovering mothering of formerly incarcerated Black women. Crime Delinq. 2021, 67, 1103–1136. [Google Scholar] [CrossRef]
- Larun, L.; Brurberg, K.G.; Odgaard-Jensen, J.; Price, J.R. Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst. Rev. 2016, 10, CD003200. [Google Scholar]
- Bolier, L.; Haverman, M.; Westerhof, G.J.; Riper, H.; Smit, F.; Bohlmeijer, E. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health 2013, 13, 119. [Google Scholar] [CrossRef]
- Reijnders, J.; van Heugten, C.; van Boxtel, M. Cognitive interventions in healthy older adults and people with mild cognitive impairment: A systematic review. Ageing Res. Rev. 2013, 12, 263–275. [Google Scholar] [CrossRef]
- Goodman, F.R.; Disabato, D.J.; Kashdan, T.B.; Machell, K.A. Personality strengths as resilience: A one-year multiwave study. J. Personal. 2017, 85, 423–434. [Google Scholar] [CrossRef]
- Theeboom, T.; Beersma, B.; van Vianen, A.E. Does coaching work? A meta-analysis on the effects of coaching on individual level outcomes in an organizational context. J. Posit. Psychol. 2014, 9, 1–18. [Google Scholar] [CrossRef]
- Lachman, M.E.; Neupert, S.D.; Agrigoroaei, S. The relevance of control beliefs for health and aging. In Handbook of the Psychology of Aging; Elsevier: Amsterdam, The Netherlands, 2011; pp. 175–190. [Google Scholar]
- Tomlinson, D.; Diorio, C.; Beyene, J.; Sung, L. Effect of exercise on cancer-related fatigue: A meta-analysis. Am. J. Phys. Med. Rehabil. 2014, 93, 675–686. [Google Scholar] [CrossRef]
- Werneburg, B.L.; Jenkins, S.M.; Friend, J.L.; Berkland, B.E.; Clark, M.M.; Rosedahl, J.K.; Preston, H.R.; Daniels, D.C.; Riley, B.A.; Olsen, K.D. Improving resiliency in healthcare employees. Am. J. Health Behav. 2018, 42, 39–50. [Google Scholar] [CrossRef] [PubMed]
- Morning, A. Does genomics challenge the social construction of race? Sociol. Theory 2014, 32, 189–207. [Google Scholar] [CrossRef]
- Ford, C.L.; Airhihenbuwa, C.O. The public health critical race methodology: Praxis for antiracism research. Soc. Sci. Med. 2010, 71, 1390–1398. [Google Scholar] [CrossRef] [PubMed]

| Covariates | Crude | Model 1 Age-Adjusted | Model 2 Age and Race/Ethnicity Adjusted | Model 3 Age, Race/Ethnicity and Stressor Adjusted |
|---|---|---|---|---|
| Estimate (95% CI) | Estimate (95% CI) | Estimate (95% CI) | ||
| POTENTIAL MODIFIERS | ||||
| Age (per year) | −0.0099 (−0.011, −0.0090); p < 0.0001 | |||
| Race/ethnicity | Joint p-value = 0.0056 | Joint p-value = 0.0008 | ||
| non-Hispanic White | −0.031 (−0.056, −0.0064) | −0.011 (−0.036, 0.013) | ||
| Asian or Pacific Islander | −0.039 (−0.086, 0.0081) | −0.032 (−0.079, 0.014) | ||
| Black or African American | Reference | Reference | ||
| Hispanic/Latina | −0.077 (−0.12, −0.033) | −0.084 (−0.13, −0.041) | ||
| STRESSORS | ||||
| Stressful life events | −0.047 (−0.049, −0.045); p < 0.0001 | −0.049 (−0.051, −0.047); p < 0.0001 | −0.049 (−0.051, −0.047); p < 0.0001 | |
| RESOURCES | ||||
| non-psychological | ||||
| Physical | ||||
| Absence of major illness (y/n) | −0.13 (−0.14, −0.11); p < 0.0001 | −0.11 (−0.13, −0.093); p < 0.0001 | −0.11 (−0.13, −0.093); p < 0.0001 | −0.089 (−0.11, −0.072); p < 0.0001 |
| Energy score | 0.015 (0.014, 0.015); p < 0.0001 | 0.015 (0.0143, 0.0151); p < 0.0001 | 0.015 (0.014, 0.015); p < 0.0001 | 0.014 (0.013, 0.014); p < 0.0001 |
| Living Assistance (y/n) | −0.24 (−0.27, −0.22); p < 0.0001 | −0.20 (−0.22, −0.17); p < 0.0001 | −0.20 (−0.22, −0.18); p < 0.0001 | −0.18 (−0.20, −0.15); p < 0.0001 |
| Activities of Daily Living score | 0.071 (0.064, 0.077); p < 0.0001 | 0.062 (0.056, 0.069); p < 0.0001 | 0.062 (0.056, 0.069); p < 0.0001 | 0.060 (0.054, 0.066); p < 0.0001 |
| Physical Functioning score | 0.0061 (0.0058, 0.0063); p < 0.0001 | 0.0060 (0.0057, 0.0062); p < 0.0001 | 0.0060 (0.0057, 0.0063); p < 0.0001 | 0.0055 (0.0052, 0.0057); p < 0.0001 |
| Socio-economic status | ||||
| Education | Joint p-value < 0.0001 | Joint p-value < 0.0001 | Joint p-value < 0.0001 | Joint p-value < 0.0001 |
| ≤HS | Reference | Reference | Reference | Reference |
| HS or GED | 0.13 (0.084, 0.18) | 0.13 (0.080, 0.17) | 0.13 (0.078, 0.17) | 0.11 (0.065, 0.15) |
| Vocational or training school/some college orassociate degree | 0.22 (0.17, 0.27); | 0.21 (0.16, 0.25) | 0.20 (0.16, 0.25) | 0.19 (0.15, 0.23) |
| ≥College degree | 0.30 (0.25, 0.34) | 0.28 (0.23, 0.32) | 0.28 (0.23, 0.32) | 0.24 (0.20, 0.29) |
| Annual Family Income | Joint p-value < 0.0001 | Joint p-value < 0.0001 | Joint p-value < 0.0001 | Joint p-value < 0.0001 |
| <20,000 | Reference | Reference | Reference | Reference |
| 20,000–34,999 | 0.085 (0.063, 0.11); | 0.081 (0.059, 0.10) | 0.082 (0.059, 0.10) | 0.072 (0.050, 0.094) |
| 35,000–49,999 | 0.14 (0.12, 0.16); | 0.13 (0.10, 0.15) | 0.13 (0.10, 0.15) | 0.11 (0.086, 0.13) |
| 50,000–74,999 | 0.19 (0.17, 0.22); | 0.17 (0.14, 0.20) | 0.17 (0.15, 0.20) | 0.15 (0.13, 0.18) |
| 75,000+ | 0.26 (0.24, 0.29); | 0.23 (0.20, 0.25) | 0.23 (0.21, 0.26) | 0.20 (0.18, 0.23) |
| Married or living with partner, (y/n) | −0.0015 (−0.014, 0.011); p = 0.82 | −0.015 (−0.028, −0.0027); p = 0.017 | −0.015 (−0.027, −0.0025); p = 0.019 | −0.0015 (−0.014, 0.011); p = 0.81 |
| Psychological | ||||
| Cognition | ||||
| Mild-to-no Forgetfulness, (y/n) | 0.49 (0.47, 0.50); p < 0.0001 | 0.47 (0.46, 0.49); p < 0.0001 | 0.47 (0.46, 0.49); p < 0.0001 | 0.42 (0.41, 0.44); p < 0.0001 |
| Self and Personality | ||||
| Personal Growth score | 0.056 (0.047, 0.066); p < 0.0001 | 0.056 (0.046, 0.066); p < 0.0001 | 0.056 (0.048, 0.065); p < 0.0001 | 0.054 (0.046, 0.062); p < 0.0001 |
| Purpose in Life score | 0.061 (0.050, 0.072); p < 0.0001 | 0.061 (0.050, 0.073); p = 0.0001 | 0.061 (0.051, 0.072); p < 0.0001 | 0.059 (0.048, 0.069); p < 0.0001 |
| Control of Beliefs score | 0.17 (0.167, 0.173); p < 0.0001 | 0.168 (0.165, 0.171); p < 0.0001 | 0.168 (0.165, 0.171); p < 0.0001 | 0.16 (0.15, 0.16); p < 0.0001 |
| Spirituality score | 0.042 (0.040, 0.044); p < 0.0001 | 0.042 (0.040, 0.044); p < 0.0001 | 0.043 (0.041, 0.045); p < 0.0001 | 0.043 (0.041, 0.045); p < 0.0001 |
| Social Relations | ||||
| Social Support score | 0.028 (0.025, 0.030); p < 0.0001 | 0.027 (0.025, 0.029); p < 0.0001 | 0.027 (0.025, 0.029); p < 0.0001 | 0.025 (0.023, 0.027); p < 0.0001 |
| Living Arrangements score | −0.021 (−0.035, 0.0069); p = 0.006 | −0.038 (−0.050, −0.026); p < 0.0001 | −0.037 (−0.050, −0.025); p < 0.0001 | −0.025 (−0.036, −0.015); p < 0.0001 |
| Social ties score | 0.039 (0.036, 0.042); p < 0.0001 | 0.037 (0.034, 0.040); p < 0.0001 | 0.037 (0.034, 0.040); p < 0.0001 | 0.035 (0.032, 0.038); p < 0.0001 |
| Total | Low (BRS 1.0–2.9) | Medium (BRS 3.0–4.2) | High (BRS 4.3–5.0) | |
|---|---|---|---|---|
| CHARACTERISTICS | n = 77,395 | n = 5496 (7.1%) | n = 36,638 (47.3%) | n = 35,261 (45.6%) |
| POTENTIAL MODIFIERS | ||||
| Age at data collection on resilience in years (mean (sd)) | 76.99 (6.41) | 77.67 (6.69) | 77.37 (6.44) | 76.49 (6.29) |
| Race/ethnicity (%) | ||||
| Black or African American | 4475 (5.8) | 387 (7.0) | 1914 (5.2) | 2174 (6.2) |
| non-Hispanic White | 69,448 (89.7) | 4840 (88.1) | 33,024 (90.1) | 31,584 (89.6) |
| Hispanic/Latina | 1891 (2.4) | 177 (3.2) | 895 (2.4) | 819 (2.3) |
| Asian or Pacific Islander | 1581 (2.0) | 92 (1.7) | 805 (2.2) | 684 (1.9) |
| STRESSORS | ||||
| non-psychological | ||||
| Have had stressful life events over the past year (%) | Missing n = 293 | Missing n = 46 | Missing n = 144 | Missing n = 103 |
| No | 18,597 (23.8) | 1108 (19.9) | 7610 (20.6) | 9879 (27.7) |
| Yes | 59,638 (76.2) | 4450 (80.1) | 29,421 (79.5) | 25,767 (72.3) |
| Mean number of stressful life events out of total 12 (mean (sd)) | Missing n = 287 | Missing n = 45 | Missing n = 140 | Missing n = 102 |
| 1.57 (1.37) | 1.89 (1.58) | 1.72 (1.43) | 1.36 (1.24) | |
| How much stressful life events upset participants 1 = not too much; 3 = very much) (mean (sd)) | Missing n = 293 | Missing n = 46 | Missing n = 144 | Missing n = 103 |
| 1.57 (1.38) | 1.90 (1.58) | 1.73 (1.44) | 1.36 (1.24) | |
| Stressful life events (Perceived stress) (mean (sd)) | Missing n = 287 | Missing n = 45 | Missing n = 140 | Missing n = 102 |
| Scale 0–36 | 3.2 (3.13) | 4.14 (3.80) | 3.57 (3.31) | 2.67 (2.72) |
| RESOURCES | ||||
| non-psychological | ||||
| Biological | ||||
| Absence of major illness (%) | ||||
| No | 66,949 (86.5) | 4581 (83.4) | 31,277 (85.4) | 31,091 (88.2) |
| Yes | 10,446 (13.5) | 915 (16.6) | 5361 (14.6) | 4170 (11.8) |
| Energy (mean (sd)) | Missing n = 2415 | Missing n = 251 | Missing n = 1263 | Missing n = 901 |
| Scale 0–24 (higher score indicates more energy) | 59.99 (19.88) | 48.47 (22.18) | 54.95 (18.84) | 66.95 (18.09) |
| Physical | ||||
| Living assistance (%) | Missing n = 7654 | Missing n = 613 | Missing n = 3633 | Missing n = 3408 |
| No | 65,564 (94.0) | 4415 (90.4) | 30,718 (93.1) | 30,431 (95.5) |
| Yes | 4177 (6.0) | 468 (9.6) | 2287 (6.9) | 1422 (4.5) |
| Activities of daily living (mean (sd)) | Missing n = 1265 | Missing n = 111 | Missing n = 641 | Missing n = 513 |
| Scale 1–18 (higher indicates more independence in performing activities) | 17.72 (1.13) | 17.44 (1.64) | 17.67 (1.22) | 17.82 (0.92) |
| Physical functioning construct (mean (sd)) | Missing n = 4113 | Missing n = 407 | Missing n = 2132 | Missing n = 1574 |
| Scale 0–100 (higher score indicates higher health state) | 68.33 (26.42) | 59.63 (29.15) | 64.70 (26.69) | 73.36 (24.70) |
| Socio-economic status | ||||
| Education level (%) | Missing n = 502 | Missing n = 47 | Missing n = 223 | Missing n = 232 |
| ≤HS | 1930 (2.5) | 228 (4.2) | 1037 (2.9) | 665 (1.9) |
| HS or GED | 11,573 (15.1) | 943 (17.3) | 6077 (16.7) | 4553 (13.0) |
| Vocational or training school/some college or associate degree | 27,716 (36.0) | 2052 (37.7) | 13,290 (36.5) | 12,374 (35.3) |
| ≥College degree | 35,674 (46.4) | 2226 (40.9) | 16,011 (44.0) | 17,437 (49.8) |
| Annual Family Income (%) | Missing n = 3982 | Missing n = 308 | Missing n = 1972 | Missing n = 1702 |
| <20,000 | 7305 (10.0) | 735 (14.2) | 3839 (11.1) | 2731 (8.1) |
| 20,000–34,999 | 15,742 (21.4) | 1278 (24.6) | 7896 (22.8) | 6568 (19.6) |
| 35,000–49,999 | 15,650 (21.3) | 1123 (21.7) | 7569 (21.8) | 6958 (20.7) |
| 50,000–74,999 | 16,955 (23.1) | 1085 (20.9) | 7761 (22.4) | 8109 (24.2) |
| 75,000+ | 17,761 (24.2) | 967 (18.6) | 7601 (21.9) | 9193 (2.4) |
| Marital Status (%) | Missing n = 262 | Missing n = 19 | Missing n = 124 | Missing n = 119 |
| Never married | 3142 (4.1) | 246 (4.5) | 1472 (4.0) | 1424 (4.1) |
| Divorced or separated | 11,386 (14.8) | 855 (15.6) | 5137 (14.1) | 5394 (15.3) |
| Widowed | 9824 (12.7) | 737 (13.5) | 4699 (12.9) | 4388 (12.5) |
| Presently married/married-like relationship | 52,781 (68.4) | 3639 (66.4) | 25,206 (69.0) | 23,936 (68.1) |
| Psychological | ||||
| Cognition | ||||
| Minimal Forgetfulness, (% Y) | Missing n = 1089 | Missing n = 117 | Missing n = 597 | Missing n = 375 |
| No | 10,078 (13.2) | 1442 (26.8) | 6154 (17.1) | 2482 (7.1) |
| Yes | 66,228 (86.8) | 3937 (73.2) | 29,887 (82.9) | 32,404 (92.9) |
| Self and Personality | ||||
| Personal growth construct (mean (sd)) | Missing n = 5845 | Missing n = 547 | Missing n = 2856 | Missing n = 2442 |
| Scale 0–28 (higher score indicates higher sense of continued growth and development) | 21.20 (4.96) | 18.27 (5.18) | 19.88 (4.80) | 23.00 (4.43) |
| Purpose in life construct (mean (sd)) | Missing n = 6433 | Missing n = 612 | Missing n = 3203 | Missing n = 2618 |
| Scale 0–28 (higher score indicates higher sense of purpose) | 19.82 (4.78) | 16.88 (4.99) | 18.51 (4.51) | 21.61 (4.35) |
| Control of beliefs (mean (sd)) | Missing n = 117 | Missing n = 12 | Missing n = 61 | Missing n = 44 |
| Scale 0–8 (higher score indicates more internal control) | 5.83 (1.81) | 4.60 (1.61) | 5.39 (1.67) | 6.46 (1.73) |
| Spirituality (mean (sd)) | Missing n = 3150 | Missing n = 301 | Missing n = 1506 | Missing n = 1343 |
| Scale 0–8 (higher indicates more religious ties) | 5.68 (2.79) | 5.00 (2.96) | 5.41 (2.81) | 6.07 (2.69) |
| Social Relations | ||||
| Social support construct (mean (sd)) | Missing n = 4698 | Missing n = 506 | Missing n = 2343 | Missing n = 1849 |
| Scale 9–45 (higher score indicates more social support) | 37.77 (7.59) | 34.38 (9.12) | 36.36 (7.77) | 39.72 (6.58) |
| Living arrangements | Missing n = 4098 | Missing n = 385 | Missing n = 2078 | Missing n = 1635 |
| Scale 0–5 (high score indicates living with more people) | 0.62 (0.54) | 0.62 (0.55) | 0.63 (0.55) | 0.62 (0.54) |
| Social ties (subset of social integration) (mean (sd)) | Missing n = 2453 | Missing n = 242 | Missing n = 1205 | Missing n = 1006 |
| Scale 1–24 (higher indicates more social ties) | 18.78 (3.21) | 17.70 (3.67) | 18.51 (3.26) | 19.24 (3.01) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Springfield, S.; Qin, F.; Hedlin, H.; Eaton, C.B.; Rosal, M.C.; Taylor, H.; Staudinger, U.M.; Stefanick, M.L. Modifiable Resources and Resilience in Racially and Ethnically Diverse Older Women: Implications for Health Outcomes and Interventions. Int. J. Environ. Res. Public Health 2022, 19, 7089. https://doi.org/10.3390/ijerph19127089
Springfield S, Qin F, Hedlin H, Eaton CB, Rosal MC, Taylor H, Staudinger UM, Stefanick ML. Modifiable Resources and Resilience in Racially and Ethnically Diverse Older Women: Implications for Health Outcomes and Interventions. International Journal of Environmental Research and Public Health. 2022; 19(12):7089. https://doi.org/10.3390/ijerph19127089
Chicago/Turabian StyleSpringfield, Sparkle, Feifei Qin, Haley Hedlin, Charles B. Eaton, Milagros C. Rosal, Herman Taylor, Ursula M. Staudinger, and Marcia L. Stefanick. 2022. "Modifiable Resources and Resilience in Racially and Ethnically Diverse Older Women: Implications for Health Outcomes and Interventions" International Journal of Environmental Research and Public Health 19, no. 12: 7089. https://doi.org/10.3390/ijerph19127089
APA StyleSpringfield, S., Qin, F., Hedlin, H., Eaton, C. B., Rosal, M. C., Taylor, H., Staudinger, U. M., & Stefanick, M. L. (2022). Modifiable Resources and Resilience in Racially and Ethnically Diverse Older Women: Implications for Health Outcomes and Interventions. International Journal of Environmental Research and Public Health, 19(12), 7089. https://doi.org/10.3390/ijerph19127089






