Determinants of Telehealth Service Use among Mental Health Patients: A Case of Rural Louisiana
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Region
2.2. Study Setting and Population
2.3. Empirical Model and Statistical Analysis
3. Results
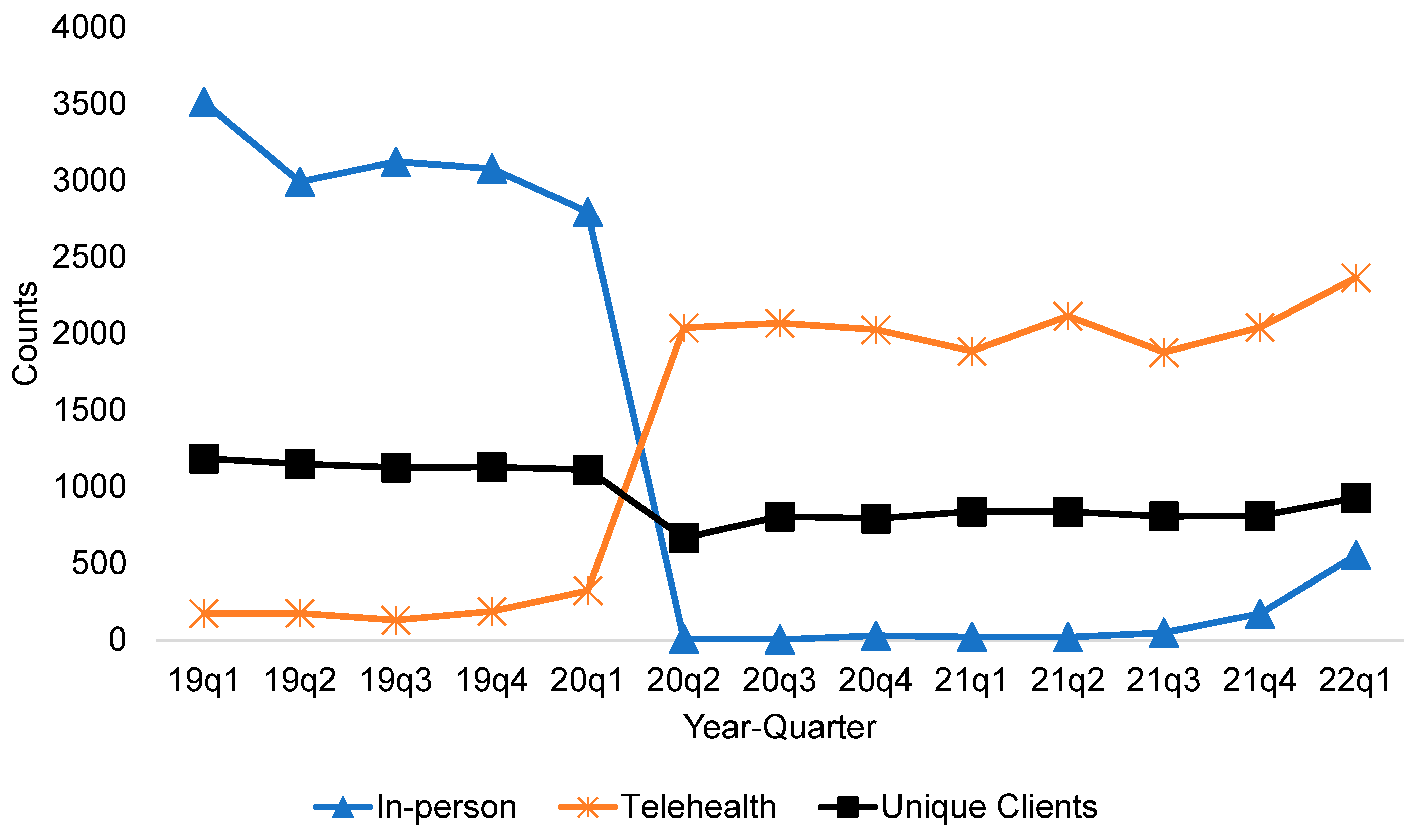
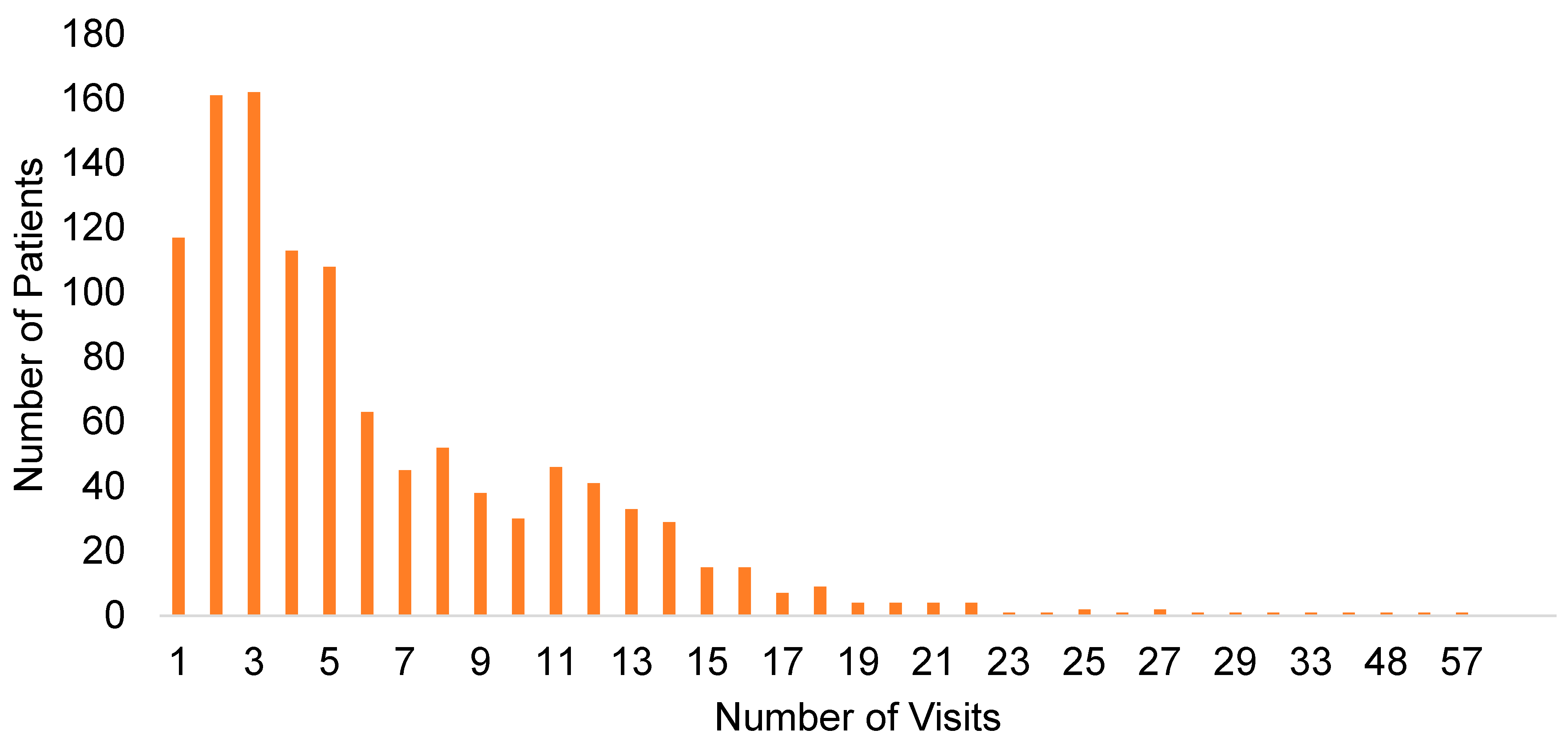
3.1. Telehealth Visit Trends
3.2. Descriptive Statistics
3.3. Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Whiteford, H.A.; Ferrari, A.J.; Degenhardt, L.; Feigin, V.; Vos, T. The global burden of mental, neurological and substance use disorders: An analysis from the Global Burden of Disease Study 2010. PLoS ONE 2015, 10, e0116820. [Google Scholar]
- Weisz, J.R.; Sandler, I.N.; Durlak, J.A.; Anton, B.S. Promoting and protecting youth mental health through evidence-based prevention and treatment. Am. Psychol. 2005, 60, 628. [Google Scholar] [CrossRef]
- Andrade, L.H.; Alonso, J.; Mneimneh, Z.; Wells, J.; Al-Hamzawi, A.; Borges, G.; Bromet, E.; Bruffaerts, R.; De Girolamo, G.; De Graaf, R. Barriers to mental health treatment: Results from the WHO World Mental Health surveys. Psychol. Med. 2014, 44, 1303–1317. [Google Scholar] [CrossRef] [Green Version]
- Hoare, E.; Callaly, E.; Berk, M. Can depression be prevented? If so, how? JAMA Psychiatry 2020, 77, 1095–1096. [Google Scholar] [CrossRef]
- Ahrnsbrak, R.; Bose, J.; Hedden, S.L.; Lipari, R.N.; Park-Lee, E. Key Substance Use and Mental Health Indicators in the United States: Results from the 2016 National Survey on Drug Use and Health; Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2017; p. 1572.
- Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55); Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2020. Available online: https://www.samhsa.gov/data/ (accessed on 15 April 2022).
- Fleury, M.-J.; Ngui, A.N.; Bamvita, J.-M.; Grenier, G.; Caron, J. Predictors of healthcare service utilization for mental health reasons. Int. J. Environ. Res. Public Health 2014, 11, 10559–10586. [Google Scholar] [CrossRef] [Green Version]
- Stewart, E.G. Sucide in rural areas. In Mental Health in Rural America: A field Guide; Stewart, E.G., Ed.; Routledge: New York, NY, USA, 2018. [Google Scholar]
- Federal Communications Commission. 2016 Broadband Progress Report; Federal Communications Commission: Washington, DC, USA, 2016.
- Kepley, H.O.; Streeter, R.A. Closing behavioral health workforce gaps: A HRSA program expanding direct mental health service access in underserved areas. Am. J. Prev. Med. 2018, 54, S190–S191. [Google Scholar] [CrossRef] [PubMed]
- SAMSHA. Rural Behavioral Health: Telehealth Challenges and Opportunities; SAMSHA: Rockville, MD, USA, 2016.
- Cantor, J.; Sood, N.; Bravata, D.M.; Pera, M.; Whaley, C. The impact of the COVID-19 pandemic and policy response on health care utilization: Evidence from county-level medical claims and cellphone data. J. Health Econ. 2022, 82, 102581. [Google Scholar] [CrossRef]
- Acharya, B.; Dhakal, C. Implementation of State Vaccine Incentive Lottery Programs and Uptake of COVID-19 Vaccinations in the United States. JAMA Netw. Open 2021, 4, e2138238. [Google Scholar] [CrossRef]
- Fortney, J.C.; Pyne, J.M.; Mouden, S.B.; Mittal, D.; Hudson, T.J.; Schroeder, G.W.; Williams, D.K.; Bynum, C.A.; Mattox, R.; Rost, K.M. Practice-based versus telemedicine-based collaborative care for depression in rural federally qualified health centers: A pragmatic randomized comparative effectiveness trial. Am. J. Psychiatry 2013, 170, 414–425. [Google Scholar] [CrossRef]
- Montoya, M.I.; Kogan, C.S.; Rebello, T.J.; Sadowska, K.; Garcia-Pacheco, J.A.; Khoury, B.; Kulygina, M.; Matsumoto, C.; Robles, R.; Huang, J. An international survey examining the impact of the COVID-19 pandemic on telehealth use among mental health professionals. J. Psychiatr. Res. 2022, 148, 188–196. [Google Scholar] [CrossRef]
- Drake, C.; Zhang, Y.; Chaiyachati, K.H.; Polsky, D. The limitations of poor broadband internet access for telemedicine use in rural America: An observational study. Ann. Intern. Med. 2019, 171, 382–384. [Google Scholar] [CrossRef]
- Zhu, J.M.; Myers, R.; McConnell, K.J.; Levander, X.; Lin, S.C. Trends in Outpatient Mental Health Services Use before and during The COVID-19 Pandemic: Study examines trends in outpatient mental health service using before and during the COVID-19 pandemic. Health Aff. 2022, 41, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Linden, M.; Horgas, A.L.; Gilberg, R.; Steinhagen-Thiessen, E. Predicting health care utilization in the very old: The role of physical health, mental health, attitudinal and social factors. J. Aging Health 1997, 9, 3–27. [Google Scholar] [CrossRef]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Andersen, R.; Newman, J.F. Societal and individual determinants of medical care utilization in the United States. Milbank Meml. Fund Q. Health Soc. 1973, 95–124. [Google Scholar] [CrossRef] [Green Version]
- Acharya, B.; Tabb, L. Spatiotemporal Analysis of Overall Health in the United States between 2010 and 2018. Cureus 2021, 13, c56. [Google Scholar]
- Elhai, J.D.; Ford, J.D. Correlates of mental health service use intensity in the National Comorbidity Survey and National Comorbidity Survey Replication. Psychiatr. Serv. 2007, 58, 1108–1115. [Google Scholar] [CrossRef]
- Shao, S.; Wang, M.; Jin, G.; Zhao, Y.; Lu, X.; Du, J. Analysis of health service utilization of migrants in Beijing using Anderson health service utilization model. BMC Health Serv. Res. 2018, 18, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Whitney, D.G.; Peterson, M.D. US national and state-level prevalence of mental health disorders and disparities of mental health care use in children. JAMA Pediatr. 2019, 173, 389–391. [Google Scholar] [CrossRef] [PubMed]
- Fleury, M.-J.; Grenier, G.; Bamvita, J.-M.; Perreault, M.; Kestens, Y.; Caron, J. Comprehensive determinants of health service utilisation for mental health reasons in a Canadian catchment area. Int. J. Equity Health 2012, 11, 20. [Google Scholar] [CrossRef] [Green Version]
- Sizer, M.A.; Bhatta, D. Mental Health and Food Insecurity Concerns in Northeast Louisiana; Northeast Delta Human Services Authority: Monroe, LA, USA, 2022. [Google Scholar]
- Winkelmann, R. Econometric Analysis of Count Data; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2008. [Google Scholar]
- Cameron, C.; Trivedi, P. Econometric Society Monographs: Regression Analysis of Count Data; Cambridge University Press: New York, NY, USA, 1998. [Google Scholar]
- Hilbe, J.M. Negative Binomial Regression; Cambridge University Press: New York, NY, USA, 2011. [Google Scholar]
- Elhai, J.D.; Calhoun, P.S.; Ford, J.D. Statistical procedures for analyzing mental health services data. Psychiatry Res. 2008, 160, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Calhoun, P.S.; Bosworth, H.B.; Grambow, S.C.; Dudley, T.K.; Beckham, J.C. Medical service utilization by veterans seeking help for posttraumatic stress disorder. Am. J. Psychiatry 2002, 159, 2081–2086. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Chakravarthy, B.; Yoon, J.; Snowden, L.; Bruckner, T.A. Psychiatric-related revisits to the emergency department following rapid expansion of community mental health services. Acad. Emerg. Med. 2019, 26, 1336–1345. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC.: College Station, TX, USA, 2021. [Google Scholar]
- Yuan, N.; Pevnick, J.M.; Botting, P.G.; Elad, Y.; Miller, S.J.; Cheng, S.; Ebinger, J.E. Patient use and clinical practice patterns of remote cardiology clinic visits in the era of COVID-19. JAMA Netw. Open 2021, 4, e214157. [Google Scholar] [CrossRef]
- Dixon, L.B.; Holoshitz, Y.; Nossel, I. Treatment engagement of individuals experiencing mental illness: Review and update. World Psychiatry 2016, 15, 13–20. [Google Scholar] [CrossRef] [Green Version]
- Saunders, S.M. Applicants’ experience of the process of seeking therapy. Psychother. Theory Res. Pract. Train. 1993, 30, 554. [Google Scholar] [CrossRef] [Green Version]
- Yokopenic, P.A.; Clark, V.A.; Aneshensel, C.S. Depression, problem recognition, and professional consultation. J. Nerv. Ment. Dis. 1983, 171, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Olfson, M.; Mojtabai, R.; Sampson, N.A.; Hwang, I.; Druss, B.; Wang, P.S.; Wells, K.B.; Pincus, H.A.; Kessler, R.C. Dropout from outpatient mental health care in the United States. Psychiatr. Serv. 2009, 60, 898–907. [Google Scholar] [CrossRef]
- Elhai, J.D.; Voorhees, S.; Ford, J.D.; Min, K.S.; Frueh, B.C. Sociodemographic, perceived and objective need indicators of mental health treatment use and treatment-seeking intentions among primary care medical patients. Psychiatry Res. 2009, 165, 145–153. [Google Scholar] [CrossRef]
- Lam, K.; Lu, A.D.; Shi, Y.; Covinsky, K.E. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern. Med. 2020, 180, 1389–1391. [Google Scholar] [CrossRef]
- Chunara, R.; Zhao, Y.; Chen, J.; Lawrence, K.; Testa, P.A.; Nov, O.; Mann, D.M. Telemedicine and healthcare disparities: A cohort study in a large healthcare system in New York City during COVID-19. J. Am. Med. Inform. Assoc. 2021, 28, 33–41. [Google Scholar] [CrossRef]
- Liddon, L.; Kingerlee, R.; Barry, J.A. Gender differences in preferences for psychological treatment, coping strategies, and triggers to help-seeking. Br. J. Clin. Psychol. 2018, 57, 42–58. [Google Scholar] [CrossRef]
- Evans-Lacko, S.; Aguilar-Gaxiola, S.; Al-Hamzawi, A.; Alonso, J.; Benjet, C.; Bruffaerts, R.; Chiu, W.; Florescu, S.; de Girolamo, G.; Gureje, O. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: Results from the WHO World Mental Health (WMH) surveys. Psychol. Med. 2018, 48, 1560–1571. [Google Scholar] [CrossRef] [Green Version]
- Nouri, S.; Khoong, E.C.; Lyles, C.R.; Karliner, L. Addressing equity in telemedicine for chronic disease management during the COVID-19 pandemic. NEJM Catal. Innov. Care Deliv. 2020, 1. [Google Scholar] [CrossRef]
- Roberts, T.; Miguel Esponda, G.; Krupchanka, D.; Shidhaye, R.; Patel, V.; Rathod, S. Factors associated with health service utilisation for common mental disorders: A systematic review. BMC Psychiatry 2018, 18, 262. [Google Scholar] [CrossRef] [Green Version]
- Fagiolini, A.; Kupfer, D.J.; Houck, P.R.; Novick, D.M.; Frank, E. Obesity as a correlate of outcome in patients with bipolar I disorder. Am. J. Psychiatry 2003, 160, 112–117. [Google Scholar] [CrossRef]
- Kilbourne, A.M.; Cornelius, J.R.; Han, X.; Haas, G.L.; Salloum, I.; Conigliaro, J.; Pincus, H.A. General-medical conditions in older patients with serious mental illness. Am. J. Geriatr. Psychiatry 2005, 13, 250–254. [Google Scholar] [CrossRef]
- Fisher, L.; Skaff, M.; Mullan, J.; Arean, P.; Glasgow, R.; Masharani, U. A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress in adults with type 2 diabetes. Diabet. Med. 2008, 25, 1096–1101. [Google Scholar] [CrossRef] [Green Version]
- Egede, L.E.; Dismuke, C.E. Serious psychological distress and diabetes: A review of the literature. Curr. Psychiatry Rep. 2012, 14, 15–22. [Google Scholar] [CrossRef]
- Lindsay Nour, B.M.; Elhai, J.D.; Ford, J.D.; Frueh, B.C. The role of physical health functioning, mental health, and sociodemographic factors in determining the intensity of mental health care use among primary care medical patients. Psychol. Serv. 2009, 6, 243. [Google Scholar] [CrossRef]
- Amini, B.; Kalankesh, L.R.; Ferdousi, R.; Farahbakhsh, M.; Fatehi, F. Willingness and preference for using telehealth services among patients with depression. Med. Sci. 2021, 25, 1133–1139. [Google Scholar]
- Palylyk-Colwell, E.; Argáez, C. Telehealth for the Assessment and Treatment of Depression, Post-Traumatic Stress Disorder, and Anxiety: Clinical Evidence; Canadian Agency for Drugs and Technologies in Health: Ottawa, ON, Canada, 2018. [Google Scholar]
- U.S. Census Bureau New Census Data Show Differences between Urban and Rural Populations. Available online: https://www.census.gov/newsroom/press-releases/2016/cb16-210.html (accessed on 15 April 2022).
| Variables | Parishes Included in the Study (N = 12) Mean (S.D.) | Rest of the Parishes in Louisiana (N = 52) Mean (S.D.) |
|---|---|---|
| Population size | 29,070 (41,132) | 82,995 (105,523) |
| Proportion of households with internet subscription | 0.62 (0.12) | 0.76 (0.08) |
| Median household income in the past 12 months | 37,371 (6360) | 48,549 (11,480) |
| Proportion of population without health insurance | 0.09 (0.02) | 0.09 (0.01) |
| Proportion of population aged 65 years and above | 0.18 (0.03) | 0.16 (0.02) |
| Proportion of Black population | 0.39 (0.17) | 0.30 (0.14) |
| Proportion of non-Hispanic White population | 0.57 (0.17) | 0.62 (0.13) |
| Proportion of ≥25 years population with a minimum of college education | 0.17 (0.07) | 0.18 (0.07) |
| Variable | Number (N) | Proportion (S.D.) | |
|---|---|---|---|
| Dependent variable | |||
| Number of visits (mean, S.D.) | 6.34 (5.635) | ||
| Independent variables | |||
| Predisposing factors | Age (years) | ||
| 18–30 | 255 | 0.229 | |
| 31–45 | 322 | 0.289 | |
| 46–60 | 368 | 0.330 | |
| 60 and above | 170 | 0.152 | |
| Gender (female) | 623 | 0.559 | |
| Education (years of school, mean, SD) | 11.50 (5.36) | ||
| Referral source (self) | 550 | 0.493 | |
| Race | |||
| African American | 615 | 0.552 | |
| White | 482 | 0.432 | |
| Others | 18 | 0.016 | |
| Enabling factor | Monthly income ($) (mean, SD) | 845 (887) | |
| Needs factors | Discharge (yes) | 69 | 0.062 |
| Chronic condition (yes) | 461 | 0.413 | |
| Number of diagnoses (mean, SD) | 1.722 (0.961) | ||
| Diagnosis type | |||
| Anxiety disorders | 44 | 0.039 | |
| Bipolar & related disorders | 158 | 0.142 | |
| Depressive disorders | 413 | 0.370 | |
| Other mental health challenges | 94 | 0.084 | |
| Schizophrenia spectrum & other psychotic disorders | 359 | 0.322 | |
| Trauma & stressor related disorders | 47 | 0.042 |
| Variable | Incidence Rate Ratio | Standard Error |
|---|---|---|
| Age in years (Ref: >60) | ||
| 18–30 | 1.164 * | 0.094 |
| 31–45 | 1.216 *** | 0.091 |
| 46–60 | 1.223 *** | 0.089 |
| Gender (female, Ref: Male) | 1.113 ** | 0.055 |
| Number of school years | 1.010 ** | 0.005 |
| Referral source (self, Ref: external sources) | 0.998 | 0.048 |
| Race (Ref: White) | ||
| African American | 0.991 | 0.049 |
| Others | 0.741 | 0.142 |
| Monthly income (in thousand USD) | 1.029 | 0.027 |
| Discharge (yes, Ref: No) | 0.550 *** | 0.058 |
| Chronic condition (yes, Ref: No) | 1.101 ** | 0.054 |
| Number of diagnoses | 1.067 *** | 0.027 |
| Primary diagnosis type (Ref: Depressive disorder) | ||
| Anxiety disorders | 0.959 | 0.117 |
| Bipolar and related disorders | 0.903 | 0.065 |
| Other mental health challenges | 0.928 | 0.084 |
| Schizophrenia spectrum and other psychotic disorders | 0.850 *** | 0.051 |
| Trauma and stressor-related disorders | 1.016 | 0.119 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sizer, M.A.; Bhatta, D.; Acharya, B.; Paudel, K.P. Determinants of Telehealth Service Use among Mental Health Patients: A Case of Rural Louisiana. Int. J. Environ. Res. Public Health 2022, 19, 6930. https://doi.org/10.3390/ijerph19116930
Sizer MA, Bhatta D, Acharya B, Paudel KP. Determinants of Telehealth Service Use among Mental Health Patients: A Case of Rural Louisiana. International Journal of Environmental Research and Public Health. 2022; 19(11):6930. https://doi.org/10.3390/ijerph19116930
Chicago/Turabian StyleSizer, Monteic A., Dependra Bhatta, Binod Acharya, and Krishna P. Paudel. 2022. "Determinants of Telehealth Service Use among Mental Health Patients: A Case of Rural Louisiana" International Journal of Environmental Research and Public Health 19, no. 11: 6930. https://doi.org/10.3390/ijerph19116930
APA StyleSizer, M. A., Bhatta, D., Acharya, B., & Paudel, K. P. (2022). Determinants of Telehealth Service Use among Mental Health Patients: A Case of Rural Louisiana. International Journal of Environmental Research and Public Health, 19(11), 6930. https://doi.org/10.3390/ijerph19116930






