Resilience Interventions Conducted in Western and Eastern Countries—A Systematic Review
Abstract
1. Introduction
Purpose of This Review
2. Materials and Methods
2.1. Inclusion Criteria
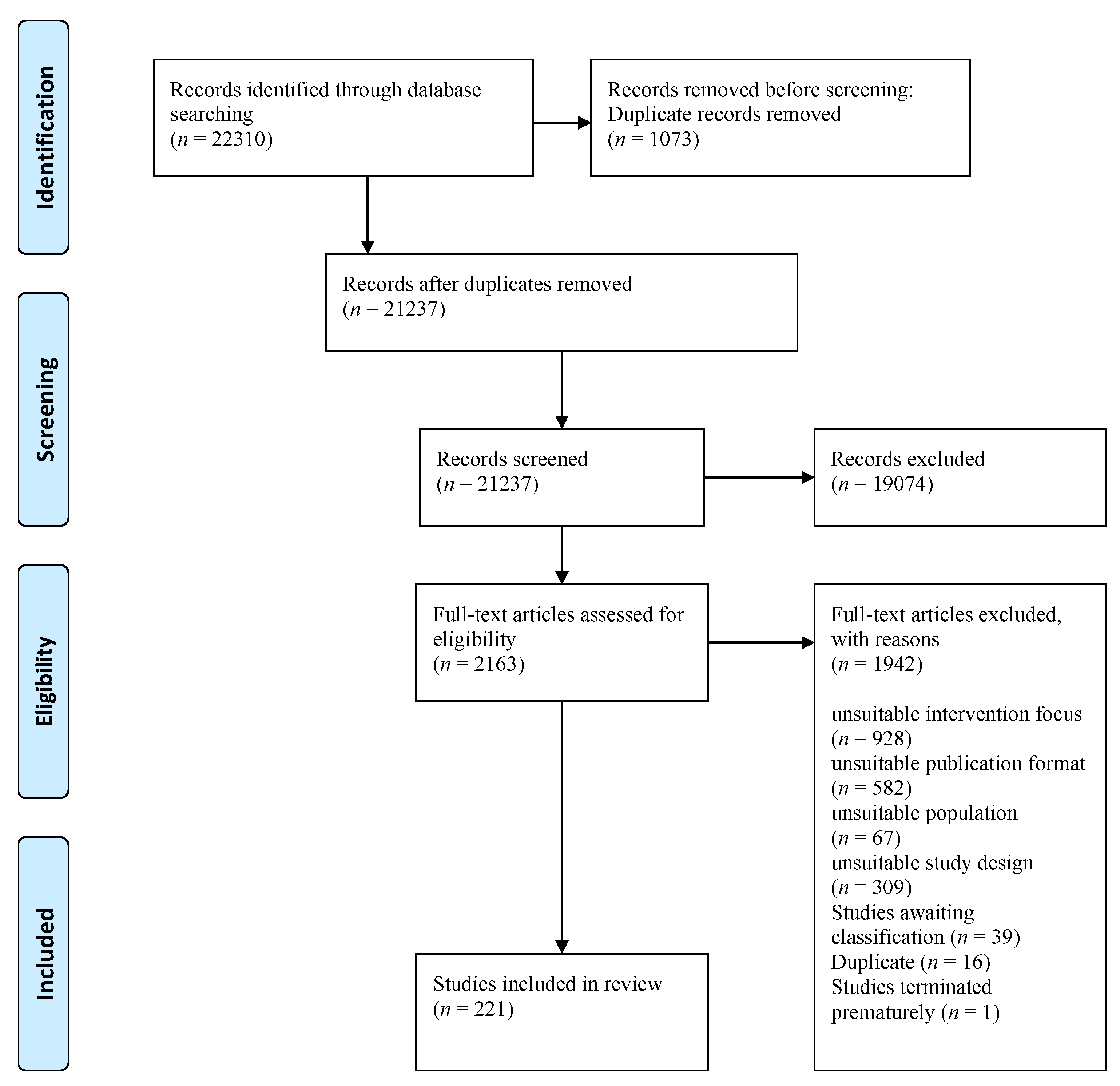
2.2. Study Selection
2.3. Data Analysis
2.4. Risk of Bias
3. Results
3.1. Characteristics of Included Studies
3.2. Risk of Bias
3.3. Differences in the Implementation of Interventions between Western and Eastern Populations
3.4. Differences between Western and Eastern Countries in Effect Sizes on Mental Health Outcomes
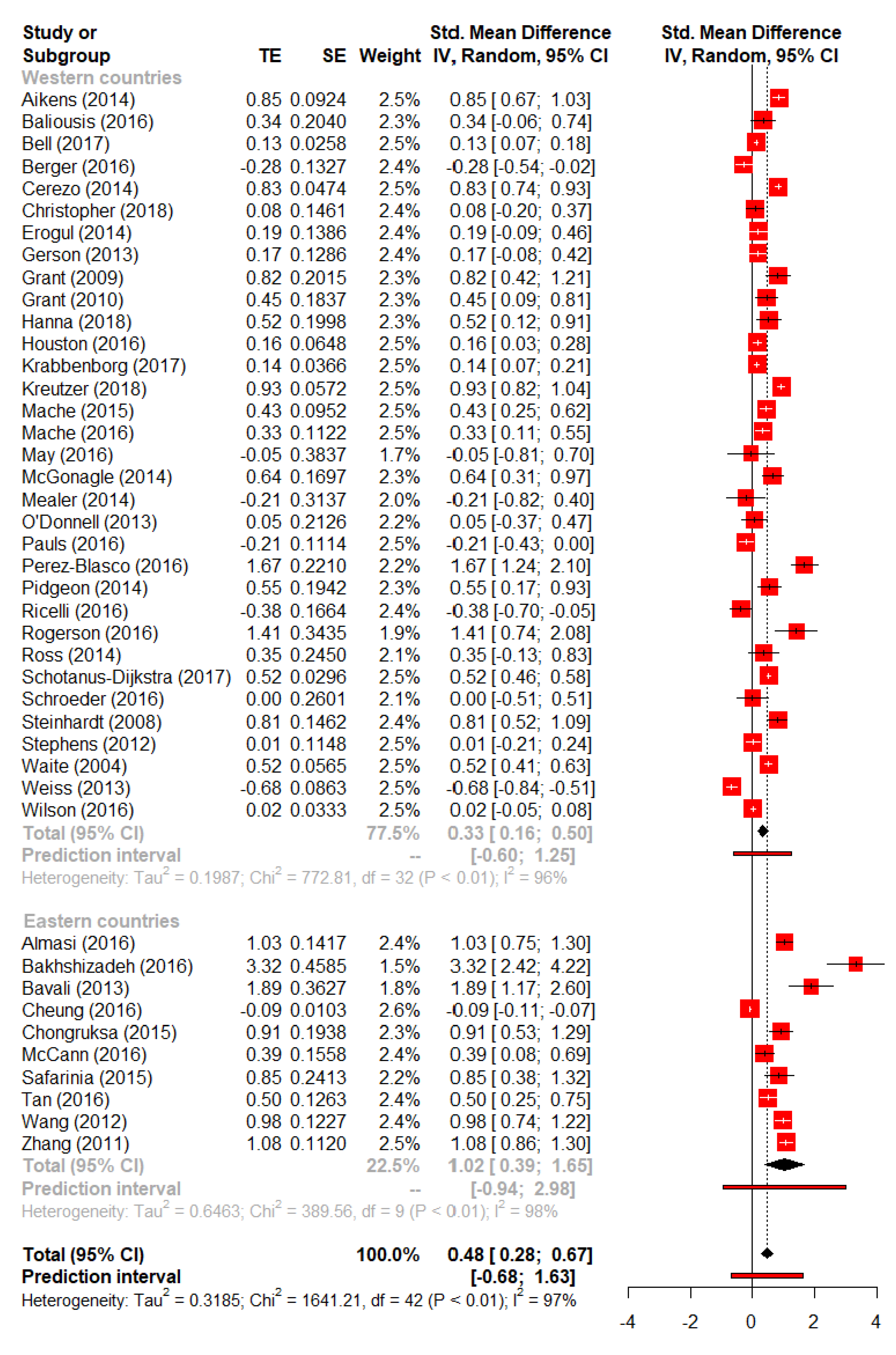
3.4.1. Resilience
3.4.2. Anxiety
3.4.3. Depressive Symptoms
3.4.4. Quality of Life
3.4.5. Perceived Stress
3.4.6. Social Support
4. Discussion
4.1. Principal Findings
4.2. Comparison to the Literature
4.3. Limitations
4.4. Implications
4.5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kalisch, R.; Baker, D.G.; Basten, U.; Boks, M.P.; Bonanno, G.A.; Brummelman, E.; Chmitorz, A.; Fernandez, G.; Fiebach, C.J.; Galatzer-Levy, I.; et al. The resilience framework as a strategy to combat stress-related disorders. Nat. Hum. Behav. 2017, 1, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.C.; Luecken, L.; Lemery-Chalfant, K. Resilience in common life: Introduction to the special issue. J. Pers. 2009, 77, 1637–1644. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S. Ordinary magic: Resilience processes in development. Am. Psychol. 2001, 56, 227–238. [Google Scholar] [CrossRef] [PubMed]
- Masten, A.S. Resilience in developing systems: Progress and promise as the fourth wave rises. Dev. Psychopathol. 2007, 19, 921–930. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A.; Diminich, E.D. Annual research review: Positive adjustment to adversity—Trajectories of minimal-impact resilience and emergent resilience. J. Child Psychol. Psychiatr. 2013, 54, 378–401. [Google Scholar] [CrossRef]
- Ioannidis, K.; Askelund, A.D.; Kievit, R.A.; Van Harmelen, A.-L. The complex neurobiology of resilient functioning after childhood maltreatment. BMC Med. 2020, 18, 32. [Google Scholar] [CrossRef]
- Yates, T.M.; Masten, A.S. Fostering the future: Resilience theory and the practice of positive psychology. In Positive Psychology in Practice; Linley, P.A., Joseph, S., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2004. [Google Scholar]
- Rutter, M. Resilience as a dynamic concept. Dev. Psychopathol. 2012, 24, 335–344. [Google Scholar] [CrossRef]
- Davydov, D.; Stewart, R.; Ritchie, K.; Chaudieu, I. Resilience and mental health. Clin. Psychol. Rev. 2010, 30, 479–495. [Google Scholar] [CrossRef]
- Ungar, M. A Constructionist discourse on resilience. Youth Soc. 2016, 35, 341–365. [Google Scholar] [CrossRef]
- Chmitorz, A.; Kunzler, A.; Helmreich, I.; Tuscher, O.; Kalisch, R.; Kubiak, T.; Wessa, M.; Lieb, K. Intervention studies to foster resilience—A systematic review and proposal for a resilience framework in future intervention studies. Clin. Psychol. Rev. 2018, 59, 78–100. [Google Scholar] [CrossRef]
- Kunzler, A.M.; Helmreich, I.; Chmitorz, A.; Konig, J.; Binder, H.; Wessa, M.; Lieb, K. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database Syst. Rev. 2020, 7, CD012527. [Google Scholar] [CrossRef] [PubMed]
- Kunzler, A.M.; Helmreich, I.; Konig, J.; Chmitorz, A.; Wessa, M.; Binder, H.; Lieb, K. Psychological interventions to foster resilience in healthcare students. Cochrane Database Syst. Rev. 2020, 7, CD013684. [Google Scholar] [CrossRef] [PubMed]
- Robertson, I.T.; Cooper, C.L.; Sarkar, M.; Curran, T. Resilience training in the workplace from 2003 to 2014: A systematic review. J. Occup. Organ. Psychol. 2015, 88, 533–562. [Google Scholar] [CrossRef]
- Shweder, R.A. Why cultural psychology? Ethos 1999, 27, 62–73. [Google Scholar] [CrossRef]
- Ungar, M. Resilience across cultures. Br. J. Soc. Work. 2006, 38, 218–235. [Google Scholar] [CrossRef]
- Henrich, J.; Heine, S.J.; Norenzayan, A. The weirdest people in the world? Behav. Brain Sci. 2010, 33, 61–83. [Google Scholar] [CrossRef]
- Henrich, J.; Heine, S.J.; Norenzayan, A. Most people are not WEIRD. Nature 2010, 446, 29. [Google Scholar] [CrossRef]
- Antweiler, C. Zur Universalität von Emotionen. Befunde und Kritik kulturvergleichender Ansätze. In Emotionen—Perspektiven auf Innen und Außen; Kienlin, T.L., Koch, L.C., Eds.; Universitätsforschungen zur Prähistorischen Archäologie: Bonn, Germany, 2017; Volume 305, pp. 125–147. [Google Scholar]
- Gureje, O.; Simon, G.E.; Ustun, T.B.; Goldberg, D.P. Somatization in cross-cultural perspective: A World Health Organization study in primary care. Am. J. Psychiatry 1997, 154, 989–995. [Google Scholar]
- Gureje, O.; Simon, G.E.; Von Korff, M. A cross-national study of the course of persistent pain in primary care. Pain 2001, 92, 195–200. [Google Scholar] [CrossRef]
- Palmer, K.T.; Reading, I.; Linaker, C.; Calnan, M.; Coggon, D. Population-based cohort study of incident and persistent arm pain: Role of mental health, self-rated health and health beliefs. Pain 2008, 136, 30–37. [Google Scholar] [CrossRef]
- Bener, A.; Ghuloum, S.; Al-Mulla, A.A.; Al-Marri, S.; Hashim, M.S.; Elbagi, I.E. Prevalence of somatisation and psychologisation among patients visiting primary health care centres in the State of Qatar. Libyan J. Med. 2010, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Cheung, P. Somatisation as a presentation in depression and post-traumatic stress disorder among Cambodian refugees. Aust. New Zealand J. Psychiatry 1993, 27, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Sadeghian, F.; Sadeghian, A.; Raei, M.; Kasaeian, A. Musculoskeletal disorders among oil field workers: Influences of health beliefs, mental health and somatisation tendency. J. Med. Sci. 2012, 12, 114–120. [Google Scholar] [CrossRef]
- Helmreich, I.; Kunzler, A.; Chmitorz, A.; König, J.; Binder, H.; Wessa, M.; Lieb, K. Psychological interventions for resilience enhancement in adults. Cochrane Database Syst. Rev. 2017, 2017, 1–43. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Handbook for Systematic Reviews of Interventions Version 6.2; Cochrane: London, UK, 2021. [Google Scholar]
- Microsoft Corporation. Microsoft Excel, 16.0; Microsoft Corporation: Redmond, WA, USA, 2019. [Google Scholar]
- Review Manager Web (RevMan Web), The Cochrane Collaboration: London, UK, 2020.
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- Wickham, H.; Bryan, J. readxl: Read Excel Files; R Package 1.3.1; Microsoft Corporation: Redmond, WA, USA, 2019. [Google Scholar]
- Dragulescu, A.; Arendt, C. xlsx: Read, Write, Format Excel 2007 and Excel 97/2000/XP/2003 Files; Microsoft Corporation: Redmond, WA, USA, 2020; Volume 9. [Google Scholar]
- Wickham, H.; François, F.; Henry, L.; Müller, K. dplyr: A Grammar of Data Manipulation, R Package Version 1.0.2. 2020. Available online: https://dplyr.tidyverse.org/ (accessed on 2 June 2022).
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to perform a meta-analysis with R: Apractical tutorial. Évid. Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Navarro, D.J. Learning Statistics with R: A Tutorial for Psychology Students and Other Beginners; Version 0.5; University of Adelaide: Adelaide, Australia, 2015. [Google Scholar]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- Cuijpers, P. Meta-Analyses in Mental Health Research. A Practical Guide; Pim Cuijpers Uitgeverij: Amsterdam, The Netherlands, 2016. [Google Scholar]
- IntHout, J.; Ioannidis, J.P.A.; Borm, G.F. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med. Res. Methodol. 2014, 14, 1–12. [Google Scholar] [CrossRef]
- Adler, A.B.; Bliese, P.D.; McGurk, D.; Hoge, C.W.; Castro, C.A. Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: Randomization by platoon. J. Consult. Clin. Psychol. 2009, 77, 928–940. [Google Scholar] [CrossRef]
- Adler, A.B.; Williams, J.; McGurk, D.; Moss, A.; Bliese, P.D. Resilience training with soldiers during basic combat training: Randomisation by platoon. Appl. Psychol. Health Well Being 2015, 7, 85–107. [Google Scholar] [CrossRef]
- Aikens, K.A.; Astin, J.; Pelletier, K.R.; Levanovich, K.; Baase, C.M.; Park, Y.Y.; Bodnar, C.M. Mindfulness goes to work: Impact of an online workplace intervention. J. Occup. Environ. Med. 2014, 56, 721–731. [Google Scholar] [CrossRef]
- Alschuler, K.N.; Arewasikporn, A.; Nelson, I.K.; Molton, I.R.; Ehde, D.M. Promoting resilience in individuals aging with multiple sclerosis: Results from a pilot randomized controlled trial. Rehabil. Psychol. 2018, 63, 338–348. [Google Scholar] [CrossRef] [PubMed]
- Anshel, M.H.; Gregory, W.; Kaczmarek, M. The effectiveness of a stress training program in coping with criticism in sport: A test of the COPE model. J. Sport Behav. 1990, 14, 194–217. [Google Scholar]
- Arch, J.J.; Brown, K.W.; Dean, D.J.; Landy, L.N.; Brown, K.D.; Laudenslager, M.L. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology 2014, 42, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Ashing, K.; Rosales, M. A telephonic-based trial to reduce depressive symptoms among Latina breast cancer survivors. Psychooncology 2014, 23, 507–515. [Google Scholar] [CrossRef]
- Ashing, K.T.; Miller, A.M. Assessing the utility of a telephonically delivered psychoeducational intervention to improve health-related quality of life in African American breast cancer survivors: A pilot trial. Psychooncology 2016, 25, 236–238. [Google Scholar] [CrossRef]
- Baliousis, M.; Rennoldson, M.; Mills, J.; Watson, L.; Dawson, D.; Das Nair, R. Psychological intervention to alleviate distress in haematopoietic stem cell transplantation: A Phase 2 study. In Proceedings of the 42nd Annual Meeting of the European Society for Blood and Marrow Transplantation, EBMT 2016, Valencia, Spain, 3–6 April 2016; pp. 547–548, Bone Marrow Transplantation 2016. [Google Scholar]
- Bartley, E.; Robinson, M.; Fillingim, R. Optimizing resilience in orofacial pain and nociception (ORION): Exploring the efficacy of a hope intervention for pain. J. Pain 2016, 17, S98. [Google Scholar] [CrossRef]
- Bauman, L.V. The Impact of a Psychological Capital Intervention on College Student Well-Being; Azusa Pacific University: Azusa, CA, USA, 2015. [Google Scholar]
- Beadel, J.R.; Mathews, A.; Teachman, B.A. Cognitive bias modification to enhance resilience to a panic challenge. Cogn. Ther. Res. 2016, 40, 799–812. [Google Scholar] [CrossRef]
- Bekki, J.; Bernstein, B.; Fabert, N.; Gildar, N.; Way, A. Efficacy of an online resource for teaching interpersonal problem solving skills to women graduate students in engineering. Adv. Eng. Educ. 2014, 4, n2. [Google Scholar]
- Bell, K.R.; Fann, J.R.; Brockway, J.A.; Cole, W.R.; Bush, N.E.; Dikmen, S.; Hart, T.; Lang, A.J.; Grant, G.; Gahm, G.; et al. Telephone problem solving for service members with mild traumatic brain injury: A randomized, clinical trial. J. Neurotrauma 2017, 34, 313–321. [Google Scholar] [CrossRef]
- Botello, S.A.; Moan, E.R. An Exploratory Comparative Study of a Cognitive Behavioral Intervention, an Art Intervention, and No Treatment on Mood, Stress, and Quality of Life in Adult Women. Ph.D. Thesis, Northern Arizona University, San Francisco, AZ, USA, 2015. [Google Scholar]
- Bradshaw, B.G.; Richardson, G.E.; Kumpfer, K.; Carlson, J.; Stanchfield, J.; Overall, J.; Brooks, A.M.; Kulkarni, K. Determining the efficacy of a resiliency training approach in adults with type 2 diabetes. Diabetes Educ. 2007, 33, 650–659. [Google Scholar] [CrossRef]
- Broome, K.M.; Bennett, J.B. Reducing heavy alcohol consumption in young restaurant workers. J. Stud. Alcohol Drugs 2011, 71, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.W.; Coogle, C.L.; Wegelin, J. A pilot randomized controlled trial of mindfulness-based stress reduction for caregivers of family members with dementia. Aging Ment. Health 2016, 20, 1157–1166. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Adler, A.B.; Lester, P.B.; McGurk, D.; Thomas, J.L.; Chen, H.Y.; Cacioppo, S. Building social resilience in soldiers: A double dissociative randomized controlled study. J. Pers. Soc. Psychol. 2015, 109, 90–105. [Google Scholar] [CrossRef]
- Castro, C.A.; Hoge, C.W.; Milliken, C.W.; McGurk, D.; Adler, A.B.; Cox, A.; Bliese, P.D. Battlemind Training: Transitioning Home from Combat; Walter Reed Army Institute of Research: Silver Spring, MD, USA, 2006; Available online: https://apps.dtic.mil/sti/pdfs/ADA481083.pdf (accessed on 2 June 2022).
- Castro, C.A.; Adler, A.B.; McGurk, D.; Bliese, P.D. Mental health training with soldiers four months after returning from Iraq: Randomization by platoon. J. Trauma Stress 2012, 25, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Chandler, G.E.; Roberts, S.J.; Chiodo, L. Resilience intervention for young adults with adverse childhood experiences. J. Am. Psychiatry Nurses Assoc. 2015, 21, 406–416. [Google Scholar] [CrossRef] [PubMed]
- Chesak, S.S.; Bhagra, A.; Schroeder, D.R.; Foy, D.A.; Cutshall, S.M.; Sood, A. Enhancing resilience among new nurses: Feasibility and efficacy of a pilot intervention. Ochsner J. 2015, 15, 38–44. [Google Scholar]
- Schroeder, D.A.; Stephens, E.; Colgan, D.; Hunsinger, M.; Rubin, D.; Christopher, M.S. A brief mindfulness-based intervention for Primary care physicians: A pilot randomized controlled trial. Am. J. Lifestyle Med. 2016, 12, 83–91. [Google Scholar] [CrossRef]
- Christopher, M.S.; Hunsinger, M.; Goerling, L.R.J.; Bowen, S.; Rogers, B.S.; Gross, C.R.; Dapolonia, E.; Pruessner, J.C. Mindfulness-based resilience training to reduce health risk, stress reactivity, and aggression among law enforcement officers: A feasibility and preliminary efficacy trial. Psych. Res. 2018, 264, 104–115. [Google Scholar] [CrossRef]
- Church, D.; Sparks, T.; Clond, M. EFT (Emotional Freedom Techniques) and resiliency in veterans at risk for PTSD: A randomized controlled trial. Explore 2016, 12, 355–365. [Google Scholar] [CrossRef]
- Creswell, J.D.; Pacilio, L.E.; Lindsay, E.K.; Brown, K.W. Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology 2014, 44, 1–12. [Google Scholar] [CrossRef]
- Deckro, G.R.; Ballinger, K.M.; Hoyt, M.; Wilcher, M.; Dusek, J.; Myers, P.; Greenberg, B.; Rosenthal, D.S.; Benson, H. The evaluation of a mind/body intervention to reduce psychological distress and perceived stress in college students. J. Am. Coll. Health 2002, 50, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Erogul, M.; Singer, G.; McIntyre, T.; Stefanov, D.G. Abridged mindfulness intervention to support wellness in first-year medical students. Teach. Learn. Med. 2014, 26, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Esmer, G.; Blum, J.; Rulf, J.; Pier, J. Mindfulness-based stress reduction for failed back surgery syndrome: A randomized controlled trial. J. Am. Osteopath. Assoc. 2010, 110, 646–652. [Google Scholar] [PubMed]
- Falb, M.D. Effects of Mindfulness Training on Individuals Experiencing Post-Breakup Distress: A Randomized Controlled Trial; Bowling Green State University: Bowling Green, OH, USA, 2016; p. 77. [Google Scholar]
- Ferguson, L.J. Coaching for Hardiness: A Study of Women Clergy and Stress Resistance; Adelphi University, The Institute of Advanced Psychological Studies: Garden City, NY, USA, 2004. [Google Scholar]
- Foran, H.M.; Adler, A.B.; McGurk, D.; Bliese, P.D. Soldiers’ perceptions of resilience training and postdeployment adjustment: Validation of a measure of resilience training content and training process. Psychol. Serv. 2012, 9, 390–403. [Google Scholar] [CrossRef]
- Frye, M.S. Promoting Caregiver and Child Resilience: The ACHIEVER Adult Resilience Curriculum; University of Washington: Seattle, WA, USA, 2015; p. 77. [Google Scholar]
- Gance-Cleveland, B.; Mays, M.Z. School-based support groups for adolescents with a substance-abusing parent. J. Am. Psychiatry Nurses Assoc. 2008, 14, 297–309. [Google Scholar] [CrossRef]
- Garland, E.L.; Manusov, E.G.; Froeliger, B.; Kelly, A.; Williams, J.M.; Howard, M.O. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: Results from an early-stage randomized controlled trial. J. Consult. Clin. Psychol. 2014, 82, 448–459. [Google Scholar] [CrossRef]
- Gaugler, J.E.; Reese, M.; Sauld, J. A Pilot evaluation of psychosocial support for family caregivers of relatives with dementia in long-term care: The residential care transition module. Res. Gerontol. Nurs. 2015, 8, 161–172. [Google Scholar] [CrossRef]
- Gerson, M.W.; Fernandez, N. PATH: A program to build resilience and thriving in undergraduates. J. Appl. Soc. Psychol. 2013, 43, 2169–2184. [Google Scholar] [CrossRef]
- Hallowell, S.R. Coping Processes as a Functional Diagnostic Dimension? A Randomized Controlled Trial Using Acceptance and Commitment Therapy and Cognitive Therapy; ProQuest: Ann Arbor, MI, USA, 2011. [Google Scholar]
- Hargrove, M.B. Antecedents and Outcomes Associated with the Individual Stress Response; University of Texas: Arlington, TX, USA, 2012. [Google Scholar]
- Heydarpour, S.; Parvaneh, E.; Saqqezi, A.; Ziapour, A.; Dehghan, F.; Parvaneh, A. Effectiveness of Group Counseling Based on the Reality Therapy on Resilience and Psychological Well-Being of Mothers with an Intellectual Disabled Child. Int J. Pediatr. 2018, 6, 7851–7860. [Google Scholar]
- Hodges, T.D. An Experimental Study of the Impact of Psychological Capital on Performance, Engagement, and the Contagion Effect; The University of Nebraska-Lincoln: Lincoln, NE, USA, 2010. [Google Scholar]
- Hoge, E.A.; Bui, E.; Marques, L.; Metcalf, C.A.; Morris, L.K.; Robinaugh, D.J.; Worthington, J.J.; Pollack, M.H.; Simon, N.M. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: Effects on anxiety and stress reactivity. J. Clin. Psychiatry 2013, 74, 786–792. [Google Scholar] [CrossRef]
- Hourani, L.L.; Kizakevich, P.N.; Holiday, D.B.; Hubal, R.; Bryant, S.; Spira, J.; Strange, L.B.; McLean, A.N. Predeployment stress inoculation training for primary prevention of combat-related stress disorders. J. CyberTherapy Rehabil. 2011, 4, 101–116. [Google Scholar]
- Hourani, L.; Tueller, S.; Kizakevich, P.; Lewis, G.; Strange, L.; Weimer, B.; Bryant, S.; Bishop, E.; Hubal, R.; Spira, J. Toward preventing post-traumatic stress disorder: Development and testing of a pilot predeployment stress inoculation training program. Mil. Med. 2016, 181, 1151–1160. [Google Scholar] [CrossRef] [PubMed]
- Houston, J.B.; First, J.; Spialek, M.L.; Sorenson, M.E.; Mills-Sandoval, T.; Lockett, M.; First, N.L.; Nitiema, P.; Allen, S.F.; Pfefferbaum, B. Randomized controlled trial of the Resilience and Coping Intervention (RCI) with undergraduate university students. J. Am. Coll. Health 2016, 65, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jennings, D.A. The Effects of Resiliency Training on Physical Activity Participation, Job Satisfaction, and Protective Factors Among Nonmanagerial Females at the Worksite. Ph.D. Thesis, Department of Exercise and Sport Science, University of Utah, Salt Lake City, UT, USA, 2002. [Google Scholar]
- Jennings, P.A.; Snowberg, K.E.; Coccia, M.A.; Greenberg, M.T. Improving classroom learning environments by cultivating awareness and resilience in education (cAre): Results of two pilot studies. J. Classr. Interact. 2011, 46, 37–48. [Google Scholar]
- Jennings, P.A.; Brown, J.L.; Frank, J.L.; Doyle, S.; Oh, Y.; Davis, R.; Rasheed, D.; DeWeese, A.; DeMauro, A.A.; Cham, H.; et al. Impacts of the CARE for Teachers program on teachers’ social and emotional competence and classroom interactions. J. Educ. Psychol. 2017, 109, 1010–1028. [Google Scholar] [CrossRef]
- Kane, J.M.; Robinson, D.G.; Schooler, N.R.; Mueser, K.T.; Penn, D.L.; Rosenheck, R.A.; Addington, J.; Brunette, M.F.; Correll, C.U.; Estroff, S.E.; et al. Comprehensive versus usual community care for first-episode psychosis: 2-Year outcomes from the NIMH RAISE early treatment program. Am. J. Psychiatr. 2016, 173, 362–372. [Google Scholar] [CrossRef] [PubMed]
- Kanekar, A.; Sharma, M.; Atri, A. Enhancing social support, hardiness, and acculturation to improve mental health among Asian Indian international students. Int. Q. Community Health Educ. 2009, 30, 55–68. [Google Scholar] [CrossRef]
- Kent, M.; Davis, M.C.; Stark, S.L.; Stewart, L.A. A resilience-oriented treatment for posttraumatic stress disorder: Results of a preliminary randomized clinical trial. J. Trauma Stress 2011, 24, 591–595. [Google Scholar] [CrossRef]
- Duchemin, A.M.; Steinberg, B.A.; Marks, D.R.; Vanover, K.; Klatt, M. A small randomized pilot study of a workplace mindfulness-based intervention for surgical intensive care unit personnel: Effects on salivary alpha-amylase levels. J. Occup. Environ. Med. 2015, 57, 393–399. [Google Scholar] [CrossRef]
- Klatt, M.; Steinberg, B.; Duchemin, A.M. Mindfulness in Motion (MIM): An onsite mindfulness based intervention (MBI) for chronically high stress work environments to increase resiliency and work engagement. J. Vis. Exp. 2015, 57, e52359. [Google Scholar] [CrossRef]
- Kreutzer, J.S.; Marwitz, J.H.; Sima, A.P.; Mills, A.; Hsu, N.H.; Lukow, H.R., II. Efficacy of the resilience and adjustment intervention after traumatic brain injury: A randomized controlled trial. Brain Inj. 2018, 32, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Lancer, K.M. Immune function and psychological distress in familial dementia caregivers: A controlled trial of a cognitive-behavioral intervention. Diss. Abstr. Int. Sect. B Sci. Eng. 2007, 68, 1931. [Google Scholar]
- Lantieri, L.; Kyse, E.N.; Harnett, S.; Malkmus, C.; Reevy, G.M.; Frydenberg, E. Building Inner Resilience in Teachers and Students; Information Age Publishing: Charlotte, NC, USA, 2011; pp. 267–292. [Google Scholar]
- Loprinzi, C.E.; Prasad, K.; Schroeder, D.R.; Sood, A. Stress management and resilience training (SMART) program to decrease stress and enhance resilience among breast cancer survivors: A pilot randomized clinical trial. Clin. Breast Cancer 2011, 11, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Luthans, F.; Avey, J.B.; Patera, J.L. Experimental analysis of a web-based training intervention to develop positive psychological capital. Acad. Manag. Learn. Educ. 2008, 7, 209–221. [Google Scholar] [CrossRef]
- Luthans, F.; Avey, J.B.; Avolio, B.J.; Peterson, S.J. The development and resulting performance impact of positive psychological capital. Hum. Resour. Dev. Q. 2010, 21, 41–67. [Google Scholar] [CrossRef]
- Luthans, B.C.; Luthans, K.W.; Avey, J.B. Building the leaders of tomorrow. J. Leadersh. Organ. Stud. 2014, 21, 191–199. [Google Scholar] [CrossRef]
- Luthar, S.S.; Suchman, N.E. Relational psychotherapy mothers’ group: A developmentally informed intervention for at-risk mothers. Dev. Psychopathol. 2000, 12, 235–253. [Google Scholar] [CrossRef]
- Luthar, S.S.; Curlee, A.; Tye, S.J.; Engelman, J.C.; Stonnington, C.M. Fostering resilience among mothers under stress:″Authentic Connections Groups″ for medical professionals. Women’s Health Issues 2017, 27, 382–390. [Google Scholar] [CrossRef]
- Luthar, S.S.; Suchman, N.E.; Altomare, M. Relational psychotherapy mothers’ group: A randomized clinical trial for substance abusing mothers. Dev. Psychopathol. 2007, 19, 243–261. [Google Scholar] [CrossRef]
- Maddi, S.R.; Kahn, S.; Maddi, K.L. The effectiveness of hardiness training. Consult. Psychol. J. Pract. Res. 1998, 50, 78–86. [Google Scholar] [CrossRef]
- May, A.C.; Cronan, T. Acceptance and Commitment Therapy for Patients with Breast Cancer: A Pilot Study. Ph.D. Thesis, San Diego State University, San Diego, CA, USA, 2016. [Google Scholar]
- Jennings, P.A.; Frank, J.L.; Snowberg, K.E.; Coccia, M.A.; Greenberg, M.T. Improving classroom learning environments by Cultivating Awareness and Resilience in Education (CARE): Results of a randomized controlled trial. Sch. Psychol. Q. 2013, 28, 374–390. [Google Scholar] [CrossRef] [PubMed]
- McCraty, R.; Atkinson, M. Resilience training program reduces physiological and psychological stress in police officers. Glob. Adv. Health Med. 2012, 1, 44–66. [Google Scholar] [CrossRef] [PubMed]
- McGonagle, A.K.; Beatty, J.E.; Joffe, R. Coaching for workers with chronic illness: Evaluating an intervention. J. Occup. Health Psychol. 2014, 19, 385–398. [Google Scholar] [CrossRef] [PubMed]
- Mealer, M.; Conrad, D.; Evans, J.; Jooste, K.; Solyntjes, J.; Rothbaum, B.; Moss, M. Feasibility and acceptability of a resilience training program for intensive care unit nurses. Am. J. Crit. Care 2014, 23, e97–e105. [Google Scholar] [CrossRef] [PubMed]
- Mejia-Downs, A.M. An Intervention Enhances Resilience in Physical Therapy Students. Ph.D. Thesis, Utah Rocky Mountain University of Health Professions, Provo, UT, USA, 2016. [Google Scholar]
- Mistretta, E.G.; Davis, M.C.; Temkit, M.; Lorenz, C.; Darby, B.; Stonnington, C.M. Resilience training for work-related stress among health care workers: Results of a randomized clinical trial comparing in-person and smartphone-delivered interventions. J. Occup. Environ. Med. 2018, 60, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, K.L. Evidence-Based Practice and Practice-Based Evidence: Examining the Impact of Delinquency Prevention in Schools. Ph.D. Thesis, The University of Texas at Austin, Austin, TX, USA, 2013. [Google Scholar]
- Nichols, L.O.; Martindale-Adams, J.; Zuber, J.; Graney, M.; Burns, R.; Clark, C. Support for spouses of postdeployment service members. Mil. Behav. Health 2015, 3, 125–137. [Google Scholar] [CrossRef]
- O′Donnell, P.J. Psychological Effects of a Strength-Based Intervention Among Inpatients in Rehabilitation for Pain and Disability. Ph.D. Thesis, Northcentral University, Scottsdale, AZ, USA, 2013; p. 75. [Google Scholar]
- Oken, B.S.; Wakeland, W. A Systems Approach to Stress and Resilience in Humans: Mindfulness Meditation, Aging, and Cognitive Function. Ph.D. Thesis, Portland State University, Portland, OR, USA, 2016. [Google Scholar] [CrossRef]
- Oman, D.; Shapiro, S.L.; Thoresen, C.E.; Plante, T.G.; Flinders, T. Meditation lowers stress and supports forgiveness among college students: A randomized controlled trial. J. Am. Coll. Health 2008, 56, 569–578. [Google Scholar] [CrossRef]
- Park, J.H. Look Beyond and Rejoice: A Spiritual Intervention for Patients with Life-Threatening Illness or Chronic Pain; Loma Linda University: Loma Linda, CA, USA, 2008. [Google Scholar]
- Petree, R.D. Exploring and reducing Stress in young restaurant workers: Results of a randomized field trial. Am. J. Health Promot. 2012, 26, 217–224. [Google Scholar] [CrossRef]
- Pyatak, E.A.; Carandang, K.; Vigen, C.L.P.; Blanchard, J.; Diaz, J.; Concha-Chavez, A.; Sequeira, P.A.; Wood, J.R.; Whittemore, R.; Spruijt-Metz, D. Occupational therapy intervention improves glycemic control and quality of life among young adults with diabetes: The Resilient, empowered, active living with diabetes (REAL Diabetes) randomized controlled trial. Diabetes Care 2018, 41, 696–704. [Google Scholar] [CrossRef]
- Ricelli, S.E.; Nezu, A.M.; Nezu, C.M. Problem-Solving Therapy to Foster Resilience among Veterans Who Are Homeless or At-Risk for Homelessness: A Pilot Randomized Controlled Trial. Ph.D. Thesis, Drexel University, Philadelphia, PA, USA, 2016. [Google Scholar]
- Rose, R.D.; Buckey, J.C., Jr.; Zbozinek, T.D.; Motivala, S.J.; Glenn, D.E.; Cartreine, J.A.; Craske, M.G. A randomized controlled trial of a self-guided, multimedia, stress management and resilience training program. Behav. Res. Ther. 2013, 51, 106–112. [Google Scholar] [CrossRef]
- Roy, M.J.; Highland, K.; Costanzo, M. GETSmart: Guided education and training via smart phones to promote resilience. Annu. Rev. Cybertherapy Telemed. 2016, 219, 123–128. [Google Scholar] [CrossRef]
- Sadow, D.; Hopkins, B. Resiliency training and empowerment among homeless, substance-abusing veterans. Increasing a sense of self-efficacy and internal attribution of control as a result of resiliency training. Res. Commun. Psychol. Psychiatry Behav. 1993, 18, 121–134. [Google Scholar]
- Schachman, K.A.; Lee, R.K.; Lederman, R.P. Baby boot camp: Facilitating maternal role adaption among military wives. Nurs. Res. 2004, 53, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Seligman, M.E.; Schulman, P.; Tryon, A.M. Group prevention of depression and anxiety symptoms. Behav. Res. Ther. 2007, 45, 1111–1126. [Google Scholar] [CrossRef]
- Sharma, V.; Saito, Y.; Amit, S. Mind-body medicine and irritable bowel syndrome: A randomized control trial using stress reduction and resiliency training. J. Altern. Complement. Med. 2014, 20, A94. [Google Scholar] [CrossRef]
- Sood, A.; Prasad, K.; Schroeder, D.; Varkey, P. Stress management and resilience training among Department of Medicine faculty: A pilot randomized clinical trial. J. Gen. Intern. Med. 2011, 26, 858–861. [Google Scholar] [CrossRef]
- Sood, A.; Sharma, V.; Schroeder, D.R.; Gorman, B. Stress Management and Resiliency Training (SMART) program among Department of Radiology faculty: A pilot randomized clinical trial. Explore 2014, 10, 358–363. [Google Scholar] [CrossRef]
- Steinhardt, M.; Dolbier, C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J. Am. Coll. Health 2008, 56, 445–453. [Google Scholar] [CrossRef]
- Stephens, T.M. Increasing Resilience in Adolescent Nursing Students. Ph.D. Thesis, University of Tennessee, Knoxville, TN, USA, 2012. [Google Scholar]
- Stoiber, K.C.; Gettinger, M. Functional assessment and positive support strategies for promoting resilience: Effects on teachers and high-risk children. Psychol. Sch. 2011, 48, 686–706. [Google Scholar] [CrossRef]
- Taylor, L.M. The Relation Between Resilience, Coaching, Coping Skills Training, and Perceived Stress During a Career-threatening Milestone. Ph.D. Thesis, Georgia State University, Atlanta, GA, USA, 1997. [Google Scholar]
- Tierney, M.J.; Lavelle, M. An investigation into modification of personality hardiness in staff nurses. J. Nurs. Staff. Dev. 1997, 13, 212–217. [Google Scholar]
- Victorson, D.; Hankin, V.; Burns, J.; Weiland, R.; Maletich, C.; Sufrin, N.; Schuette, S.; Gutierrez, B.; Brendler, C. Feasibility, acceptability and preliminary psychological benefits of mindfulness meditation training in a sample of men diagnosed with prostate cancer on active surveillance: Results from a randomized controlled pilot trial. Psychooncology 2017, 26, 1155–1163. [Google Scholar] [CrossRef] [PubMed]
- Vranceanu, A.M.; Riklin, E.; Merker, V.L.; Macklin, E.A.; Park, E.R.; Plotkin, S.R. Mind-body therapy via videoconferencing in patients with neurofibromatosis. Am. Acad. Neurol. 2016, 87, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Waite, P.J. Determining the efficacy of resiliency training in the worksite. Diss. Abstr. Int. Sect. A Humanit. Soc. Sci. 2004, 33, 62. [Google Scholar]
- Weissberg-Benchell, J.; Rausch, J.; Iturralde, E.; Jedraszko, A.; Hood, K. A randomized clinical trial aimed at preventing poor psychosocial and glycemic outcomes in teens with type 1 diabetes (T1D). Contemp. Clin. Trials 2016, 49, 78–84. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Rabatin, J.T.; Call, T.G.; Davidson, J.H.; Multari, A.; Romanski, S.A.; Hellyer, J.M.; Sloan, J.A.; Shanafelt, T.D. Intervention to promote physician well-being, job satisfaction, and professionalism: A randomized clinical trial. JAMA Intern. Med. 2014, 174, 527–533. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Satele, D.; Shanafelt, T.D. A randomized controlled trial evaluating the effect of COMPASS (COlleagues Meeting to Promote and Sustain Satisfaction) small group sessions on physician well-being, meaning, and job satisfaction. J. Gen. Intern. Med. 2015, 30, 45. [Google Scholar]
- Wilson, I. Effectiveness of Stress Inoculation and Stress Management Approaches for Enhancing Resilience in a U.S. Military Combat Population. Ph.D. Thesis, Alliant International University, Alhambra, CA, USA, 2016; p. 76.
- Zautra, A.J.; Davis, M.C.; Reich, J.W.; Nicassario, P.; Tennen, H.; Finan, P.; Kratz, A.; Parrish, B.; Irwin, M.R. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. J. Consult. Clin. Psychol. 2008, 76, 408–421. [Google Scholar] [CrossRef]
- Akbari, B. Effectiveness of training psychological resilience on aggression and happiness among students. J. Holist. Nurs. Midwifery 2017, 27, 1–7. [Google Scholar] [CrossRef]
- Almasi, A.; Hatami, F.; Sharifi, A.; Ahmadijouybari, T.; Kaviannezhad, R.; Ebrahimzadeh, F. Effectiveness of stress coping skills training on the resiliency of mothers of handicapped children. Sci. J. Kurd. Univ. Med. Sci. 2016, 21, 34–42. (In Persian) [Google Scholar]
- Bahamin, G.; Taheri, F.; Moghaddas, A.; Sohrabi, F.; Dortaj, F. The effects of hardiness training on suicide ideation, quality of life and plasma levels of lipoprotein (a) in patients with depressive disorder. Procedia Soc. Behav. Sci. 2012, 46, 4236–4243. [Google Scholar] [CrossRef]
- Bakhshizadeh, S.H.; Afrooz, G.H.A.; Beh-pajooh, A.; Ghobari Bonab, B.; Shokoohi Yekta, M. Effectiveness of resiliency based on islamic spirituality training on mental health & spiritual resiliency among mothers of slow pace (mentally retarded) children. Armaghane-Danesh 2016, 21, 492–512. [Google Scholar]
- Bari, N.S.; Bahrainian, S.A.; Azargoon, H.; Abedi, H.; Aghaee, F. The effectiveness of reality therapy on resiliency of divorced women in Neyshabour city of Iran. World Sci. J. 2013, 1, 115–123. [Google Scholar]
- Bavali, F.; Faramarzi, S.; Manshaie, G.; Khaledian, M. Effectiveness of Group Logo Therapy on resiliency of the mothers with intellectual disability children. Int. Res. J. Appl. Basic Sci. 2013, 6, 160–164. [Google Scholar]
- Hadizad, T.; Sajedi, F.; Movallali, G.; Reza Soltani, P. Effectiveness of resiliency training in improving mother-child relationship in mothers of children with mental retardation. Iran. Rehabil. J. 2016, 14, 171–178. [Google Scholar] [CrossRef]
- Haidarabadi, Z.G. Effectiveness of reality therapy education to increase happiness and hardiness of mothers who have blind child. Kuwait Chapter Arab. J. Bus. Manag. Rev. 2014, 3, 293. [Google Scholar] [CrossRef][Green Version]
- Haydari, L.; Farhadian, M. Effectiveness resiliency training to reduce stress and improve the quality of life of female-headed household. Res. J. Fish. Hydrobiol. 2015, 10, 105–110. [Google Scholar]
- Kaboudi, M.; Abbasi, P.; Heidarisharaf, P.; Dehghan, F.; Ziapour, A. The Effect of resilience training on the condition of style of coping and parental stress in mothers of children with leukemia. Int. J. Pediatric. 2018, 6, 7299–7310. [Google Scholar] [CrossRef]
- Kaveh, M.; Alizadeh, H.; Delavar, A.; Borjali, A. Development of a resilience fostering program against stress and its impact on quality of life components in parents of children with mild intellectual disability. J. Ophthalmol. Eye Care 2011, 11, 119–140. [Google Scholar]
- Khodabakhshi, A.; Derakhshandeh, M. Effectiveness of hope-oriented group therapy on life meaning and resilience in mothers with physical-motor disabled children. Iran. J. Pediatric. Nurs. 2015, 1, 3. [Google Scholar]
- Moghimi, M.; Karimi, Z.; Esmaeilpour, N.; Zoladl, M. The Effect of resilience education by the teach-back method on the stress of mothers of educable mentally retarded children: A field trial study. Int. J. Pediatric. 2017, 5, 6347–6358. [Google Scholar] [CrossRef]
- Naemi, A.M. Effectiveness of family-based education on mental health and resiliency of women with addicted husband (Case study: Sabzevar). Women Dev. Politics 2015, 13, 41–52. [Google Scholar]
- Norouzi, H.; Rahimian-Boogar, I.; Talepasand, S. Effectiveness of mindfulness-based cognitive therapy on posttraumatic growth, self-management and functional disability among patients with breast cancer. Nurs. Pract. Today 2017, 4, 190–202. [Google Scholar]
- Rahmati, M.; Khaledi, B.; Salari, N.; Bazrafshan, M.; Haydarian, A. The effects of religious and spiritual interventions on the resilience of family members of patients in the ICU. Shiraz E-Med. J. 2017, 18, e13007. [Google Scholar] [CrossRef]
- Roghanchi, M.; Mohamad, A.R.; Mey, S.C.; Momeni, K.M.; Golmohamadian, M. The effect of integrating rational emotive behavior therapy and art therapy on self-esteem and resilience. Arts Psychother. 2013, 40, 179–184. [Google Scholar] [CrossRef]
- Roshan, F.J.; Ahmadi, S.; Eslami, S. The effectiveness of group training based on positive-oriented psychotherapy on the resiliency and public health of the wives with addicte. Biomed. Pharmacol. J. 2015, 8, 185–191. [Google Scholar] [CrossRef][Green Version]
- Roustaei, A.; Bakhshipoor, B.; Doostian, Y.; Akbar Goodiny, A.; Koohikar, M.; Massah Choolabi, O. Effectiveness of resilience training on ego-control and hardiness of illicit drug users. Addict. Health 2017, 9, 24–31. [Google Scholar]
- Safarinia, M.; Aghayoosefi, A.; Mehmannavazan, A.; Dehestani, M. The effectiveness of training problem solving skills on the resiliency of the students residing at the dormitory of the Industrial University of Khaje Nasiredin Toosi. Res. J. Pharm. Biol. Chem. Sci. 2015, 6, 1497–1504. [Google Scholar]
- Abbott, J.; Klein, B.; Hamilton, C.; Rosenthal, A. The impact of online resilience training for sales managers on wellbeing and performance. E-J. Appl. Psychol. 2009, 5, 89–95. [Google Scholar] [CrossRef]
- Devilly, G.; Varker, T. The Prevention of Trauma Reactions in Police Officers: Decreasing Reliance on Drugs and Alcohol; National Drug Law Enforcement Research Fund: Canberra, Australia, 2013. [Google Scholar]
- Fuller-Tyszkiewicz, M.; Richardson, B.; Little, K.; Teague, S.; Hartley-Clark, L.; Capic, T.; Khor, S.; Cummins, R.A.; Craig Olsson, C.; Hutchinson, D. The StressLess Mobile App Study: Helping Carers Thrive; School of Psychology, Deakin University: Victoria, Australia, 2017. [Google Scholar]
- Grant, A.M.; Curtayne, L.; Burton, G. Executive coaching enhances goal attainment, resilience and workplace well-being: A randomised controlled study. J. Posit. Psychol. 2009, 4, 396–407. [Google Scholar] [CrossRef]
- Grant, A.M.; Green, L.S.; Rynsaardt, J. Developmental coaching for high school teachers: Executive coaching goes to school. Consult. Psychol. J. Pract. Res. 2010, 62, 151–168. [Google Scholar] [CrossRef]
- Hanna, A.; Pidgeon, A.M. Leveraging mindfulness to build resilience and professional quality of life in human service professionals. OBM Integr. Complementary Med. 2018, 3, 1. [Google Scholar] [CrossRef]
- Hawkes, A.L.; Pakenham, K.I.; Chambers, S.K.; Patrao, T.A.; Courneya, K.S. Effects of a multiple health behavior change intervention for colorectal cancer survivors on psychosocial outcomes and quality of life: A randomized controlled trial. Ann. Behav. Med. 2014, 48, 359–370. [Google Scholar] [CrossRef] [PubMed]
- Pidgeon, A.M.; Ford, L.; Klaassen, F. Evaluating the effectiveness of enhancing resilience in human service professionals using a retreat-based Mindfulness with Metta Training Program: A randomised control trial. Psychol. Health Med. 2013, 19, 355–364. [Google Scholar] [CrossRef] [PubMed]
- Pidgeon, M.A.; O′Brien, B.; Hanna, A.; Klaassen, F. Cultivating a resilient response to stress through mindfulness and cognitive re-appraisal: A Pilot randomised control trial. GSTF J. Psychol. 2014, 1, 8–13. [Google Scholar] [CrossRef][Green Version]
- Poulsen, A.A.; Sharpley, C.F.; Baumann, K.C.; Henderson, J.; Poulsen, M.G. Evaluation of the effect of a 1-day interventional workshop on recovery from job stress for radiation therapists and oncology nurses: A randomised trial. Med. Imaging Radiat. Oncol. 2015, 59, 491–498. [Google Scholar] [CrossRef]
- Rogerson, S.; Meir, R.; Crowley-McHattan, Z.; McEwen, K.; Pastoors, R. A Randomized controlled pilot trial investigating the impact of a workplace resilience program during a time of significant organizational change. J. Occup. Environ. Med. 2016, 58, 329–334. [Google Scholar] [CrossRef]
- Sansom-Daly, U.; Wakefield, C.; Bryant, R.; Ellis, S.; Doolan, E.; Cohn, R. Adapting evidence-based psychological therapy to the computer screen for adolescent and young adult cancer survivors: Preliminary results from the “recapture life” randomised controlled trial. Asia-Pac. J. Clin. Oncol. 2014, 10, 36. [Google Scholar]
- Shakespeare-Finch, J.E.; Shochet, I.M.; Roos, C.R.; Craig, C.; Armstrong, D.; Young, R.M.; Wurfl, A. Promoting posttraumatic growth in police recruits: Preliminary results of a randomised controlled resilience intervention trial. In Proceedings of the 2014 Australian and New Zealand Disaster and Emergency Management Conference, Gold Coast, Australia, 5–7 May 2014. [Google Scholar]
- Shochet, I.M.; Shakespeare-Finch, J.; Craig, C.; Roos, C.; Wurfl, A.; Hoge, R.; McD Young, R.; Brough, P. The DeInd implementation of the promoting resilient officers (PRO) program. Traumatology 2011, 17, 43–51. [Google Scholar] [CrossRef]
- Skeffington, P.M.; Rees, C.S.; Mazzucchelli, T.G.; Kane, R.T. The primary prevention of PTSD in firefighters: Preliminary results of an RCT with 12-month follow-up. PLoS ONE 2016, 11, e0155873. [Google Scholar] [CrossRef]
- Turkstra, E.; Gamble, J.; Creedy, D.K.; Fenwick, J.; Barclay, L.; Buist, A.; Ryding, E.L.; Scuffham, P.A. PRIME: Impact of previous mental health problems on health-related quality of life in women with childbirth trauma. Arch. Women’s Ment. Health 2013, 16, 561–564. [Google Scholar] [CrossRef]
- Tyson, O.; Roberts, C.M.; Kane, R. Can implementation of a resilience program for primary school children enhance the mental health of teachers? Aust. J. Guid. Couns. 2009, 19, 116–130. [Google Scholar] [CrossRef]
- Varker, T.; Devilly, G.J. An analogue trial of inoculation/resilience training for emergency services personnel: Proof of concept. J. Anxiety Disord 2012, 26, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, C.E.; Sansom-Daly, U.M.; McGill, B.C.; Ellis, S.J.; Doolan, E.L.; Robertson, E.G.; Mathur, S.; Cohn, R.J. Acceptability and feasibility of an e-mental health intervention for parents of childhood cancer survivors: “Cascade”. Support. Care Cancer 2016, 24, 2685–2694. [Google Scholar] [CrossRef] [PubMed]
- Bian, Y.; Xiong, H.; Zhang, L.; Tang, T.; Liu, Z.; Xu, R.; Lin, H.; Xu, B. Change in coping strategies following intensive intervention for special-service military personnel as civil emergency responders. J. Occup. Health 2011, 53, 36–44. [Google Scholar] [CrossRef]
- Chan, C.H.; Chan, C.L.; Ng, E.H.; Ho, P.C.; Chan, T.H.; Lee, G.L.; Hui, W.H. Incorporating spirituality in psychosocial group intervention for women undergoing in vitro fertilization: A prospective randomized controlled study. Psychol. Psychother. 2012, 85, 356–373. [Google Scholar] [CrossRef]
- Cheung, Y.L. Psychological first aid as a public health disaster response preparedness strategy for responders in critical incidents and disasters. Diss. Abstr. Int. Sect. B Sci. Eng. 2016, 76, 1–361. [Google Scholar]
- Ho, R.T.; Fong, T.C.; Lo, P.H.; Ho, S.M.; Lee, P.W.; Leung, P.P.; Spiegel, D.; Chan, C.L. Randomized controlled trial of supportive-expressive group therapy and body-mind-spirit intervention for Chinese non-metastatic breast cancer patients. Support. Care Cancer 2016, 24, 4929–4937. [Google Scholar] [CrossRef][Green Version]
- Hsiao, F.H.; Jow, G.M.; Kuo, W.H.; Chang, K.J.; Liu, Y.F.; Ho, R.T.; Ng, S.M.; Chan, C.L.; Lai, Y.M.; Chen, Y.T. The effects of psychotherapy on psychological well-being and diurnal cortisol patterns in breast cancer survivors. Psychother. Psychosom. 2012, 81, 173–182. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, H.; Zhai, H. Effects of positive-psychology-based group counseling on college students with mental crisis. J. Nurs. 2012, 19, 1–4. [Google Scholar]
- Wong, M.C.; Sun, J.; Lee, A.; Stewart, D.; Cheng, F.F.; Kan, W.; Ho, M. The impact of a newly designed resilience-enhancing programme on parent- and teacher-perceived resilience environment among Health Promoting Schools in Hong Kong. J. Epidemiol. Commun. Health 2009, 63, 209–214. [Google Scholar] [CrossRef]
- Ye, Z.J.; Liang, M.Z.; Qiu, H.Z.; Liu, M.L.; Hu, G.Y.; Zhu, Y.F.; Zeng, Z.; Zhao, J.J.; Quan, X.M. Effect of a multidiscipline mentor-based program, Be Resilient to Breast Cancer (BRBC), on female breast cancer survivors in mainland China-A randomized, controlled, theoretically-derived intervention trial. Breast Cancer Res. Treat. 2016, 158, 509–522. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.J.; Qiu, H.Z.; Liang, M.Z.; Liu, M.L.; Li, P.F.; Chen, P.; Sun, Z.; Yu, Y.L.; Wang, S.N.; Zhang, Z.; et al. Effect of a mentor-based, supportive-expressive program, Be Resilient to Breast Cancer, on survival in metastatic breast cancer: A randomised, controlled intervention trial. Br. J. Cancer 2017, 117, 1486–1494. [Google Scholar] [CrossRef] [PubMed]
- Yuen, W.W.Y.; Wong, W.C.W.; Tang, C.S.K.; Holroyd, E.; Tiwari, A.F.Y.; Fong, D.Y.T.; Chin, W.Y. Promoting resilience for HIV prevention in female sex workers in Hong Kong: A randomised controlled trial. Lancet 2015, 386, s140–s6736. [Google Scholar] [CrossRef]
- Zhang, J. Research on the Characteristics of Psychological Resilience and the Promotion of Psychological Resilience of Military College Students; Third Military Medical University: Chongqing, China, 2011. [Google Scholar]
- Zhang, W.; Yan, T.T.; Du, Y.S.; Liu, X.H. Brief report: Effects of solution-focused brief therapy group-work on promoting post-traumatic growth of mothers who have a child with ASD. J. Autism Dev. Disord. 2014, 44, 2052–2056. [Google Scholar] [CrossRef]
- Zhang, J.; Zhou, Y.; Feng, Z.; Fan, Y.; Zeng, G.C.; Li, W. Randomized controlled trial of mindfulness-based stress reduction (MBSR) on posttraumatic growth of Chinese breast cancer survivors psychology. Health Med. 2017, 22, 94–109. [Google Scholar]
- Chung, P.; Cheng, K.C.; Li, H.Y.; Jiang, X.; Su, N.; Zhang, C.; Si, G. The effect of resilience training for Hong Kong junior athletes. Int. J. Sport Exerc. Psychol. 2013, 11, 228–242. [Google Scholar] [CrossRef]
- Yu, X.; Stewart, S.M.; Chui, J.P.; Ho, J.L.; Li, A.C.; Lam, T.H. A pilot randomized controlled trial to decrease adaptation difficulties in chinese new immigrants to Hong Kong. Behav. Ther. 2014, 45, 137–152. [Google Scholar] [CrossRef]
- Aubin, S.; Rosberger, Z.; Petr, K.; Gerald, B. Reporting on the clinical utility of a coping skills intervention program for AYAC: What have we learned thus far. Psycho-Oncology 2011, 20, 105–300. [Google Scholar] [CrossRef]
- Carlson, L.E.; Doll, R.; Stephen, J.; Faris, P.; Tamagawa, R.; Drysdale, E.; Speca, M. Randomized controlled trial of Mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer. J. Clin. Oncol. 2013, 31, 3119–3126. [Google Scholar] [CrossRef]
- Kovacs, A.H.; Grace, S.L.; Kentner, A.C.; Nolan, R.P.; Silversides, C.K.; Irvine, M.J. Feasibility and outcomes in a pilot randomized controlled trial of a psychosocial intervention for adults with congenital heart disease. Can. J. Cardiol. 2018, 34, 766–773. [Google Scholar] [CrossRef]
- Porter, S.; Johnson, A.M. Increasing paramedic students’ resiliency to stress: Assessing correlates and the impact of intervention. Coll. Q. 2008, 11, n3. [Google Scholar]
- Roeser, R.W.; Schonert-Reichl, K.A.; Jha, A.; Cullen, M.; Wallace, L.; Wilensky, R.; Oberle, E.; Thomson, K.; Taylor, C.; Harrison, J. Mindfulness training and reductions in teacher stress and burnout: Results from two randomized, waitlist-control field trials. J. Educ. Psychol. 2013, 105, 787–804. [Google Scholar] [CrossRef]
- Waddell, J.; Bauer, M. Career planning and development for students: Building a career in a professional practice discipline. Can. J. Career Dev. 2005, 4, 4–13. [Google Scholar]
- Waddell, J.; Spalding, K.; Canizares, G.; Navarro, J.; Connell, M.; Jancar, S.; Stinson, J.; Victor, C. Integrating a career planning and development program into the baccalaureate nursing curriculum: Part I. Impact on students’ career resilience. Int. J. Nurs. Educ. Scholarsh. 2015, 12, 162–173. [Google Scholar] [CrossRef]
- Weir, R.; Stewart, L.; Browne, G.; Roberts, J.; Gafni, A.; Easton, S.; Seymour, L. The efficacy and effectiveness of process consultation in improving staff morale and absenteeism. Med. Care 1997, 35, 334–353. [Google Scholar] [CrossRef]
- Zernicke, K.A.; Campbell, T.S.; Speca, M.; McCabe-Ruff, K.; Flowers, S.; Carlson, L.E. A randomized wait-list controlled trial of feasibility and efficacy of an online mindfulness-based cancer recovery program: The eTherapy for cancer applying mindfulness trial. Psychosom. Med. 2014, 76, 257–267. [Google Scholar] [CrossRef]
- Geschwind, N.; Peeters, F.; Drukker, M.; Van Os, J.; Wichers, M. Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: A randomized controlled trial. J. Consult. Clin. Psychol. 2011, 79, 618–628. [Google Scholar] [CrossRef]
- Krabbenborg, M.A.M.; Boersma, S.N.; van der Veld, W.M.; Van Hulst, B.; Vollebergh, W.A.M.; Wolf, J.R.L.M. A cluster randomized controlled trial testing the effectiveness of houvast. Res. Soc. Work. Pract. 2017, 27, 639–652. [Google Scholar] [CrossRef]
- Schotanus-Dijkstra, M.; Drossaert, C.H.C.; Pieterse, M.E.; Boon, B.; Walburg, J.A.; Bohlmeijer, E.T. An early intervention to promote well-being and flourishing and reduce anxiety and depression: A randomized controlled trial. Internet Interv. 2017, 9, 15–24. [Google Scholar] [CrossRef]
- Smeets, E.; Neff, K.; Alberts, H.; Peters, M. Meeting suffering with kindness: Effects of a brief self-compassion intervention for female college students. J. Clin. Psychol. 2014, 70, 794–807. [Google Scholar] [CrossRef]
- Strijk, J.E.; Proper, K.I.; Van Mechelen, W.; Van Der Beek, A.J. Effectiveness of a worksite lifestyle intervention on vitality, work engagement, productivity, and sick leave: Results of a randomized controlled trial. Scand. J. Work Environ. Health 2013, 39, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Van Berkel, J.; Boot, C.R.; Proper, K.I.; Bongers, P.M.; Van Der Beek, A.J. Effectiveness of a worksite mindfulness-related multi-component health promotion intervention on work engagement and mental health: Results of a randomized controlled trial. PLoS ONE 2014, 9, e84118. [Google Scholar] [CrossRef] [PubMed]
- Van Der Spek, N.; Vos, J.; Van Uden-Kraan, C.F.; Breitbart, W.; Cuijpers, P.; Holtmaat, K.; Witte, B.I.; Tollenaar, R.; Verdonck-de Leeuw, I.M. Efficacy of meaning-centered group psychotherapy for cancer survivors: A randomized controlled trial. Psychol Med. 2017, 47, 1990–2001. [Google Scholar] [CrossRef] [PubMed]
- Van Zelst, C.J. Inside Out: On Stereotype Awareness, Childhood Trauma and Stigma in Psychosis; University of Maastricht: Maastricht, The Netherlands, 2010. [Google Scholar]
- Weiss, L.A.; Westerhof, G.J.; Bohlmeijer, E.T. Nudging socially isolated people towards well-being with the ‘Happiness Route’: Design of a randomized controlled trial for the evaluation of a happiness-based intervention. Health Qual. Life Outcomes 2013, 11, 1–11. [Google Scholar] [CrossRef]
- Bernburg, M.; Baresi, L.; Groneberg, D.; Mache, S. Does psychosocial competency training for junior physicians working in pediatric medicine improve individual skills and perceived job stress. Eur. J. Pediatr. 2016, 175, 1905–1912. [Google Scholar] [CrossRef]
- Mache, S.; Danzer, G.; Klapp, B.; Groneberg, D.A. Evaluation of a multicomponent psychosocial skill training program for junior physicians in their first year at work: A pilot study. Fam. Med. 2015, 47, 693–698. [Google Scholar] [PubMed]
- Mache, S.; Bernburg, M.; Baresi, L.; Groneberg, D.A. Evaluation of self-care skills training and solution-focused counselling for health professionals in psychiatric medicine: A pilot study. Int. J. Psychiatry Clin. Pract. 2016, 20, 239–244. [Google Scholar] [CrossRef]
- Pauls, N.; Schlett, C.; Soucek, R.; Ziegler, M.; Frank, N. Enhancing resilience through training of personal resources: Evaluation of a web-based mindfulness intervention. Gio Gruppe Interaktion Organisation Zeitschrift Fuer Angewandte Organisationspsychologie (GIO) 2016, 47, 105–117. [Google Scholar] [CrossRef]
- Pietrowsky, R.; Mikutta, J. Effects of positive psychology interventions in depressive patients—A randomized control study. Psychology 2012, 3, 1067–1073. [Google Scholar] [CrossRef]
- Wagner, B.; Knaevelsrud, C.; Maercker, A. Post-traumatic growth and optimism as outcomes of an internet-based intervention for complicated grief. Cogn. Behav. Ther. 2007, 36, 156–161. [Google Scholar] [CrossRef]
- Galante, J.; Dufour, G.; Vainre, M.; Wagner, A.P.; Stochl, J.; Benton, A.; Lathia, N.l.; Howarth, E.; Jones, P.B. A mindfulness-based intervention to increase resilience to stress in university students (the Mindful Student Study): A pragmatic randomised controlled trial. Lancet Public Health 2018, 3, e72–e81. [Google Scholar] [CrossRef]
- Johnson, J.; Gooding, P.A.; Wood, A.M.; Fair, K.L.; Tarrier, N. A Therapeutic Tool for Boosting Mood: The Broad-Minded Affective Coping Procedure (BMAC). Cogn. Ther. Res. 2013, 37, 61–70. [Google Scholar] [CrossRef]
- Rigby, S.A.; Thornton, E.W.; Young, C.A. A randomized group intervention trial to enhance mood and self-efficacy in people with multiple sclerosis. Br. J. Health Psychol. 2008, 13, 619–631. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.C. Positive Mental Training: Efficacy, Experience and Underlying Mechanisms of a Health Promotion Intervention for Resilience and Wellbeing in the Workplace; The University of Edinburgh: Edinburgh, UK, 2014. [Google Scholar]
- Sprange, K.; Mountain, G.A.; Brazier, J.; Cook, S.P.; Craig, C.; Hind, D.; Walters, S.J.; Windle, G.; Woods, R.; Keetharuth, A.D.; et al. Lifestyle Matters for maintenance of health and wellbeing in people aged 65 years and over: Study protocol for a randomised controlled trial. Trials 2013, 14, 302. [Google Scholar] [CrossRef] [PubMed]
- Wild, J. An evaluation of Mind’s resilience intervention for emergency workers. Final Report. Available online: https://www.mind.org.uk/media-a/4866/strand-3.pdf.
- Botella, C.; Mira, A.; Moragrega, I.; Garcia-Palacios, A.; Breton-Lopez, J.; Castilla, D.; Riera Lopez Del Amo, A.; Soler, C.; Molinari, G.; Quero, S.; et al. An Internet-based program for depression using activity and physiological sensors: Efficacy, expectations, satisfaction, and ease of use. Neuropsychiatr. Dis. Treat. 2016, 12, 393–406. [Google Scholar] [CrossRef] [PubMed]
- Cerezo, V.M.; Ortiz-Tallo, M.; Cardenal, V.; De La Torre-Luque, A. Positive psychology group intervention for breast cancer patients: A randomised trial. Psychol. Rep. 2014, 115, 44–64. [Google Scholar] [CrossRef] [PubMed]
- González, S.G.; Rodríguez, C.F.; Rodríguez, J.P.; Amigo, I. Secondary prevention of depression in primary care. Psicothema 2006, 18, 471–477. [Google Scholar]
- Perez-Blasco, J.; Sales, A.; Meléndez, J.C.; Mayordomo, T. The effects of mindfulness and self-compassion on improving the capacity to adapt to stress situations in elderly people living in the community. Clin. Gerontol. 2016, 39, 90–103. [Google Scholar] [CrossRef]
- Sanchez-Teruel, D.; Robles-Bello, M.A. Responding to a program of resilience applied parents of children with Down Syndrome. Universitas Psychologica 2015, 14, 645–657. [Google Scholar]
- Berger, R.; Gelkopf, M. An intervention for reducing secondary traumatization and improving professional self-efficacy in well baby clinic nurses following war and terror: A random control group trial. Int. J. Nurs. Stud. 2011, 48, 601–610. [Google Scholar] [CrossRef]
- Berger, R.; Abu-Raiya, H.; Benatov, J. Reducing primary and secondary traumatic stress symptoms among educators by training them to deliver a resiliency program (ERASE-Stress) following the Christchurch earthquake in New Zealand. Am. J. Orthopsychiatry 2016, 86, 236–251. [Google Scholar] [CrossRef] [PubMed]
- Farchi, M.; Gidron, Y. The effects of ″psychological inoculation″ versus ventilation on the mental resilience of Israeli citizens under continuous war stress. J. Nerv. Ment. Dis. 2010, 198, 382–384. [Google Scholar] [CrossRef] [PubMed]
- Yun, Y.H.; Kim, Y.A.; Lee, M.K.; Sim, J.A.; Nam, B.H.; Kim, S.; Lee, E.S.; Noh, D.Y.; Lim, J.Y.; Kim, S.; et al. A randomized controlled trial of physical activity, dietary habit, and distress management with the Leadership and Coaching for Health (LEACH) program for disease-free cancer survivors. BMC Cancer 2017, 17, 298. [Google Scholar] [CrossRef] [PubMed]
- Yu, E.S.; Kim, B.S.; Lee, J.H.; Kim, J.H. A randomized controlled trial of stress management program for breast cancer patients under treatment. Asia-Pac. J. Clin. Oncol. 2012, 8, 299–300. [Google Scholar]
- Yun, Y.H.; Lee, M.K.; Bae, Y.; Shon, E.J.; Shin, B.R.; Ko, H.; Lee, E.S.; Noh, D.Y.; Lim, J.Y.; Kim, S.; et al. Efficacy of a training program for long-term disease- free cancer survivors as health partners: A randomized controlled trial in Korea. Asian Pac. J. Cancer Prev. 2013, 14, 7229–7235. [Google Scholar] [CrossRef]
- Jensen, C.G.; Lansner, J.; Petersen, A.; Vangkilde, S.A.; Ringkobing, S.P.; Frokjaer, V.G.; Adamsen, D.; Knudsen, G.M.; Denninger, J.W.; Hasselbalch, S.G. Open and calm—A randomized controlled trial evaluating a public stress reduction program in Denmark. BMC Public Health 2015, 15, 1245. [Google Scholar] [CrossRef]
- Klatt, M.; Norre, C.; Reader, B.; Yodice, L.; White, S. Mindfulness in motion: A mindfulness-based intervention to reduce stress and enhance quality of sleep in Scandinavian employees. Mindfulness 2016, 8, 481–488. [Google Scholar] [CrossRef]
- Pawar, A.; Panda, J.; Bobdey, S. Effectiveness of mindfulness based mental fitness training: An impact evaluation study. Int. J. Res. Med. Sci. 2016, 4, 3433–3439. [Google Scholar] [CrossRef][Green Version]
- Safren, S.A.; Thomas, B.E.; Mayer, K.H.; Biello, K.B.; Mani, J.; Rajagandhi, V.; Periyasamy, M.; Swaminathan, S.; Mimiaga, M.J. A pilot RCT of an intervention to reduce HIV sexual risk and increase self-acceptance among MSM in Chennai, India. AIDS Behav. 2014, 18, 1904–1912. [Google Scholar] [CrossRef][Green Version]
- Caruso, R.; Sabato, S.; Massarenti, S.; Nanni, M.G.; Grassi, L. The experience of cancer in advanced phases of illness: Italian CALM project. In Proceedings of the IPOS 16th World Congress of Psycho-Oncology and Psychosocial, Lisbon, Portugal, 20–24 October 2014; pp. 26–27, Psycho-Oncology 2014. [Google Scholar]
- Villani, D.; Grassi, A.; Cognetta, C.; Toniolo, D.; Cipresso, P.; Riva, G. Self-help stress management training through mobile phones: An experience with oncology nurses. Psychol. Serv. 2013, 10, 315–322. [Google Scholar] [CrossRef]
- Cieslak, R.; Benight, C.C.; Rogala, A.; Smoktunowicz, E.; Kowalska, M.; Zukowska, K.; Yeager, C.; Luszczynska, A. Effects of Internet-based self-efficacy intervention on secondary traumatic stress and secondary posttraumatic growth among health and human services professionals exposed to indirect trauma. Front. Psychol. 2016, 7, 1009. [Google Scholar] [CrossRef] [PubMed]
- Rogala, A.; Smoktunowicz, E.; Zukowska, K.; Kowalska, M.; Cieslak, R. The helpers′ stress: Effectiveness of a web-based intervention for professionals working with trauma survivors in reducing job burnout and improving work engagement. Med. Pr. 2016, 67, 223–228. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Patrão, I.; Deep, C.N.; Leal, I. Cancer related fatigue and a cognitive behavioral intervention in quality of life in subjects undergoing radiotherapy–Alongitudinal and randomised trial. In PSYCHO-ONCOLOGY; Wiley-Blackwell: Hoboken, NJ, USA, 2014; pp. 170–171. [Google Scholar]
- Ramos, C.; Leal, I.; Tedeschi, R.G. Protocol for the psychotherapeutic group intervention for facilitating posttraumatic growth in nonmetastatic breast cancer patients. BMC Womens Health 2016, 16, 22. [Google Scholar] [CrossRef] [PubMed]
- Arnetz, B.B.; Nevedal, D.C.; Lumley, M.A.; Backman, L.; Lublin, A. Trauma resilience training for police: Psychophysiological and performance effects. J. Police Crim. Psychol. 2009, 24, 1–9. [Google Scholar] [CrossRef]
- Arnetz, B.B.; Arble, E.; Backman, L.; Lynch, A.; Lublin, A. Assessment of a prevention program for work-related stress among urban police officers. Int. Arch. Occup. Environ. Health 2013, 86, 79–88. [Google Scholar] [CrossRef]
- Chongruksa, D.; Prinyapol, P.; Sawatsri, S.; Pansomboon, C. Integrated group counselling to enhance mental health and resilience of Thai army rangers. Asia Pac. J. Couns. Psychother. 2015, 6, 41–57. [Google Scholar] [CrossRef]
- McCann, T.V.; Songprakun, W.; Stephenson, J. Efficacy of a self-help manual in increasing resilience in carers of adults with depression in Thailand. Int. J. Ment. Health Nurs. 2016, 25, 62–70. [Google Scholar] [CrossRef]
- Geschwind, N.; Meulders, M.; Peters, M.L.; Vlaeyen, J.W.; Meulders, A. Can experimentally induced positive affect attenuate generalization of fear of movement-related pain? J. Pain 2015, 16, 258–269. [Google Scholar] [CrossRef]
- Mulligan, K.; Fear, N.T.; Jones, N.; Alvarez, H.; Hull, L.; Naumann, U.; Wessely, S.; Greenberg, N. Postdeployment Battlemind training for the U.K. armed forces: A cluster randomized controlled trial. J. Consult. Clin. Psychol. 2012, 80, 331–341. [Google Scholar] [CrossRef]
- Melendez, J.C.; Fortuna, F.B.; Sales, A.; Mayordomo, T. The effects of instrumental reminiscence on resilience and coping in elderly. Arch. Gerontol. Geriatr. 2015, 60, 294–298. [Google Scholar] [CrossRef]
- Vuori, J.; Toppinen-Tanner, S.; Mutanen, P. Effects of resource-building group intervention on career management and mental health in work organizations: Randomized controlled field trial. J. Appl. Psychol. 2012, 97, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, Z.; Rigo, A.; Kokonyei, G.; Szabo, E.D.K.; Sebestyen, A.; Balogh, B.; Prezenszki, Z.; Nagy, M. Complex psycho-social intervention program complementing conventional antitumor therapy—Promising results. Magyar Onkologia 2012, 56, 247–257. [Google Scholar] [PubMed]
- O’Brien, I. Supported Self-Management: A Novel Cancer Survivorship Care Pathway. A Phase I/II Intervention Study With Cancer Survivors in New Zealand. Ph.D. Thesis, University of Otago, Dunedin, New Zeland, 2016. [Google Scholar]
- Betancourt, T.S.; McBain, R.; Newnham, E.A.; Akinsulure-Smith, A.M.; Brennan, R.T.; Weisz, J.R.; Hansen, N.B. A behavioral intervention for war-affected youth in Sierra Leone: A randomized controlled trial. J. Am. Acad. Child. Adolesc. Psychiatry 2014, 53, 1288–1297. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.K.; Chan, S.W.; Wang, W.; Vehvilainen-Julkunen, K. A salutogenic program to enhance sense of coherence and quality of life for older people in the community: A feasibility randomized controlled trial and process evaluation. Patient Educ. Couns. 2016, 99, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Gelkopf, M.; Ryan, P.; Cotton, S.J.; Berger, R. The impact of ″training the trainers″ course for helping tsunami-survivor children on Sri Lankan disaster volunteer workers. Int. J. Stress Manag. 2008, 15, 117–135. [Google Scholar] [CrossRef]
- Liu, C.J.; Hsiung, P.C.; Chang, K.J.; Liu, Y.F.; Wang, K.C.; Hsiao, F.H.; Ng, S.M.; Chan, C.L. A study on the efficacy of body-mind-spirit group therapy for patients with breast cancer. J. Clin. Nurs. 2008, 17, 2539–2549. [Google Scholar] [CrossRef]
- Meichenbaum, D. Stress inoculation training: A preventative and treatment approach. In Principles and Practice of Stress Management; Lehrer, P.M., Woolfolk, R.L., Sime, W.S., Eds.; Guilford Press: New York, NY, USA, 2007; Volume 3, pp. 497–518. [Google Scholar]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef]
- Luthar, S.S.; Lyman, E.L.; Crossman, E.J. Resilience and Positive Psychology. In Handbook of Developmental Psychopathology; Springer: Berlin/Heidelberg, Germany, 2014; pp. 125–140. [Google Scholar]
- Nowack, K.M. Coping style, cognitive hardiness, and health status. J. Behav. Med. 1989, 12, 145–158. [Google Scholar] [CrossRef]
- Cohen, J. Statistical power analysis for the behavioral sciences. Curr. Dir. Psychol. Sci. 1988, 1, 98–101. [Google Scholar] [CrossRef]
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions version 6.3; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2022. [Google Scholar]
- Hofstede, G. Dimensionalizing Cultures: The Hofstede Model in Context. In Online Readings in Psychology and Culture; Centre for Applied Cross-cultural Research, The Berkeley Electronic Press: Wellington, New Zealand, 2011; Available online: http://scholarworks.gvsu.edu/orpc/vol2/iss1/8 (accessed on 2 June 2022).
- Joyce, S.; Shand, F.; Tighe, J.; Laurent, S.J.; Bryant, R.A.; Harvey, S.B. Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018, 8, e017858. [Google Scholar] [CrossRef]
- Liu, J.J.W.; Ein, N.; Gervasio, J.; Battaion, M.; Fung, K. The pursuit of resilience: A meta-analysis and systematic review of resilience-promoting interventions. J. Happiness Stud. 2021, 23, 1771–1791. [Google Scholar] [CrossRef]
- Raghavan, S.; Sandanapitchai, P. The relationship between cultural variables and resilience to psychological trauma: A systematic review of the literature. Traumatology 2020, 1–15. [Google Scholar] [CrossRef]
- Kalisch, R.; Muller, M.B.; Tuscher, O. A conceptual framework for the neurobiological study of resilience. Behav. Brain Sci. 2015, 38, e92. [Google Scholar] [CrossRef] [PubMed]
- Ungar, M.; Liebenberg, L. Assessing resilience across cultures using mixed methods: Construction of the child and youth resilience measure. J. Mix. Methods Res. 2011, 5, 126–149. [Google Scholar] [CrossRef]
- Copas, J.B.; Jackson, D.; White, I.R.; Riley, R.D. The role of secondary outcomes in multivariate meta-analysis. J. R. Stat. Soc. Ser. C 2018, 67, 1177–1205. [Google Scholar] [CrossRef]
- Kunzler, A.M.; Stoffers-Winterling, J.; Stoll, M.; Mancini, A.L.; Lehmann, S.; Blessin, M.; Gilan, D.; Helmreich, I.; Hufert, F.; Lieb, K. Mental health and psychosocial support strategies in highly contagious emerging disease outbreaks of substantial public concern: A systematic scoping review. PLoS ONE 2021, 16, e0244748. [Google Scholar] [CrossRef]
- Heath, C.; Sommerfield, A.; Von Ungern-Sternberg, B.S. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: A narrative review. Anaesthesia 2020, 75, 1364–1371. [Google Scholar] [CrossRef]

| Country | Western/Eastern | k = 221 (100%) |
|---|---|---|
| USA [39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140] | Western | 102 (46.2%) |
| Iran [141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160] | Eastern | 20 (9.0%) |
| Australia [161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179] | Western | 19 (8.6%) |
| China [180,181,182,183,184,185,186,187,188,189,190,191,192,193,194] | Eastern | 15 (6.8%) |
| Canada [195,196,197,198,199,200,201,202,203] | Western | 9 (4.1%) |
| Netherlands [204,205,206,207,208,209,210,211,212] | Western | 9 (4.1%) |
| Germany [213,214,215,216,217,218] | Western | 6 (2.7%) |
| United Kingdom [219,220,221,222,223,224] | Western | 6 (2.7%) |
| Spain [225,226,227,228,229] | Western | 5 (2.3%) |
| Israel [230,231,232] | Western | 3 (1.4%) |
| South Korea [233,234,235] | Eastern | 3 (1.4%) |
| Denmark [236,237] | Western | 2 (0.9%) |
| India [238,239] | Eastern | 2 (0.9%) |
| Italy [240,241] | Western | 2 (0.9%) |
| Poland [242,243] | Western | 2 (0.9%) |
| Portugal [244,245] | Western | 2 (0.9%) |
| Sweden [246,247] | Western | 2 (0.9%) |
| Thailand [246,247] | Eastern | 2 (0.9%) |
| Belgium [248] | Western | 1 (0.5%) |
| Cyprus [249] | Western | 1 (0.5%) |
| Dominican Republic [250] | Eastern | 1 (0.5%) |
| Finland [251] | Western | 1 (0.5%) |
| Hungary [252] | Western | 1 (0.5%) |
| New Zealand [253] | Western | 1 (0.5%) |
| Sierra Leone [254] | Eastern | 1 (0.5%) |
| Singapore [255] | Eastern | 1 (0.5%) |
| Sri Lanka [256] | Eastern | 1 (0.5%) |
| Taiwan [257] | Eastern | 1 (0.5%) |
| Setting | k = 221 (100%) |
|---|---|
| Group | 125 (56.5%) |
| Western [39,40,43,47,49,53,54,55,56,57,58,59,60,61,62,67,71,72,73,76,79,80,82,83,84,90,91,92,94,98,99,100,101,102,103,106,109,111,113,115,116,117,119,122,123,124,128,130,132,133,135,136,137,138,140,162,166,168,170,171,172,173,175,177,178,196,197,198,199,201,203,207,210,211,213,214,215,221,224,226,229,230,231,245,249,251,261,262] | 88 (39.8%) |
| Eastern [141,142,144,145,146,147,149,150,151,152,153,154,155,156,157,158,160,181,182,183,184,185,186,187,188,190,191,193,194,234,235,246,250,254,256,257] | 37 (16.7%) |
| Individual | 44 (19.9%) |
| Western [42,44,45,46,48,51,52,64,69,70,77,89,93,97,107,114,118,120,121,125,126,161,163,167,195,206,212,216,218,220,222,225,232,236,240,241,242,243,244,248,253] | 41 (18.6%) |
| Eastern [233,238,249] | 3 (1.4%) |
| Combination | 43 (19.5%) |
| Western [41,63,66,68,74,75,78,81,85,86,87,88,95,96,104,105,108,110,112,127,129,131,134,139,164,165,174,179,200,202,204,208,209,217,219,223,227,228,237,252] | 40 (18.1%) |
| Eastern [180,192,239] | 3 (1.4%) |
| Unspecified | 9 (4.1%) |
| Western [50,65,169,176,205] | 5 (2.3%) |
| Eastern [143,148,159,257] | 4 (1.8%) |
| Mode of Delivery | k = 221 (100%) |
| Face to face | 146 (66.1%) |
| Western [39,40,43,47,48,49,53,54,55,56,57,58,59,60,62,64,66,67,71,72,73,74,76,79,81,82,83,84,85,90,92,94,95,98,99,100,101,102,103,104,106,109,111,113,114,115,116,117,118,119,122,123,126,128,130,131,132,133,135,136,137,138,139,140,162,164,165,166,168,170,171,175,178,196,197,198,199,201,202,204,205,207,208,210,211,212,213,214,215,217,219,220,221,223,224,226,229,230,231,240,244,245,249,251,252,253,261,262] | 108 (48.9%) |
| Eastern [141,142,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,160,180,181,182,183,185,186,188,189,190,191,193,194,234,239,246,250,254,255,256,257] | 38 (17.2%) |
| Combination | 45 (20.4%) |
| Western [41,42,45,46,61,63,68,75,77,78,80,86,87,88,91,93,96,105,108,110,120,121,124,125,127,167,173,174,176,177,195,200,209,222,227,228,236,237] | 38 (17.2%) |
| Eastern [184,187,192,233,235,238,249] | 7 (3.2%) |
| Online | 15 (6.8%) |
| Western [51,69,89,97,129,134,161,172,179,203,216,218,225,242,243] | 15 (6.8%) |
| Telephone | 5 (2.3%) |
| Western [52,70,107,112,232] | 5 (2.3%) |
| Laboratory | 3 (1.4%) |
| Western [44,50,250] | 3 (1.4%) |
| Unspecified | 3 (1.4%) |
| Western [169] | 1 (0.5%) |
| Eastern [143,159] | 2 (0.9%) |
| Smartphone | 2 (0.9%) |
| Western [163,241] | 2 (0.9%) |
| Bibliotherapy | 1 (0.5%) |
| Western [206] | 1 (0.5%) |
| Audio | 1 (0.5%) |
| Western [65] | 1 (0.5%) |
| Population | k = 221 (100%) |
| Employees in organizations of different branches | 51 (23.1%) |
| Western [41,53,55,61,62,70,72,78,80,85,91,92,97,101,103,107,108,110,117,126,127,132,135,137,138,161,164,166,168,169,170,171,175,202,208,209,213,214,215,216,222,224,227,230,237,241,242,243,251] | 49 (22.2%) |
| Eastern [182,189] | 2(0.9%) |
| Patients (physical health conditions) | 44 (19.9%) |
| Western [42,45,46,47,48,54,68,74,93,96,104,113,116,118,125,133,134,136,140,167,172,195,196,197,203,210,221,226,240,244,245,252,253] | 33 (14.9%) |
| Eastern [155,181,183,184,187,188,192,233,234,235,257] | 11 (5%) |
| Students | 32 (14.5%) |
| Western [43,44,49,50,51,60,65,66,67,73,76,84,89,98,99,109,111,115,120,124,128,129,131,198,200,201,207,219] | 28 (12.7%) |
| Eastern [141,157,160,238] | 4 (1.8%) |
| Military/police | 26 (11.8%) |
| Western [39,40,52,57,58,59,63,64,71,82,83,90,106,119,121,122,139,162,173,174,249,261,262] | 23 (10.4%) |
| Eastern [180,190,248] | 3 (1.4%) |
| General population (e.g., volunteers) | 25 (11.3%) |
| Western [69,112,114,123,176,178,205,206,212,223,225,228,232,236,250] | 15 (6.8%) |
| Eastern [145,149,186,193,194,239,250,254,255,256] | 10 (4.5%) |
| Family caregivers | 21 (9.5%) |
| Western [56,75,79,94,163,179,229] | 7 (3.2%) |
| Eastern [142,144,146,147,148,150,151,152,153,154,156,158,191,247] | 14 (6.3%) |
| Patients (mental health conditions) | 12 (5.4%) |
| Western [81,88,100,102,185,204,211,217,218,220] | 9 (4.1%) |
| Eastern [143,159] | 3 (1.4%) |
| Employees—teachers | 10 (4.5%) |
| Western [77,86,87,95,105,130,165,177,199,231] | 10 (4.5%) |
| Theoretical Approach of the Intervention | k = 221 (100%) |
| Multimodal resilience training (several theoretical approaches); several resilience factors trained without naming certain theoretical approaches | 131 (59.3%) |
| Western [39,40,43,44,45,46,47,49,51,52,53,54,55,57,58,59,60,64,66,70,71,72,73,74,75,76,78,79,80,85,88,89,90,95,97,98,99,100,101,102,103,106,107,108,110,111,112,113,116,117,118,123,128,129,130,131,132,134,135,136,137,162,164,165,166,168,169,170,171,173,174,175,197,200,201,202,205,207,208,210,212,213,214,215,217,220,222,223,224,226,229,230,231,236,240,245,248,249,251,252,253] | 101 (45.7%) |
| Eastern [141,146,148,151,152,153,155,156,157,158,159,180,181,182,183,184,188,189,190,191,193,194,239,246,250,254,255,256,257] | 30 (13.6%) |
| Mindfulness-based therapy | 30 (13.6%) |
| Western [41,56,62,63,65,67,68,69,81,86,87,91,92,105,114,115,133,139,140,196,199,203,204,209,216,219,228,237] | 28 (12.7%) |
| Eastern [192,238] | 2 (0.9%) |
| CBT | 23 (10.4%) |
| Western [93,94,120,121,124,161,163,172,176,177,179,198,211,218,221,225,242,243,244] | 19 (8.6%) |
| Eastern [142,147,154,249] | 4 (1.8%) |
| Unspecified | 15 (6.8%) |
| Western [48,109,122,138,195,227,247] | 7 (3.2%) |
| Eastern [143,144,145,149,150,186,233,235] | 8 (3.6%) |
| AIT | 6 (2.7%) |
| Western [61,96,125,126,127] | 5 (2.3%) |
| Eastern [187] | 1 (0.5%) |
| Stress inoculation training | 6 (2.7%) |
| Western [82,83,178,232,241,246] | 6 (2.7%) |
| Problem-solving training | 3 (1.4%) |
| Western [84,119] | 2 (0.9%) |
| Eastern [160] | 1 (0.5%) |
| ACT | 3 (1.4%) |
| Western [77,104,167] | 3 (1.4%) |
| Positive Psychology | 3 (1.4%) |
| Western [42,206] | 2 (0.9%) |
| Eastern [185] | 1 (0.5%) |
| Cognitive bias modification | 1 (0.5%) |
| Western [50] | 1 (0.5%) |
| Duration | k = 221 (%) |
| High intensity | 86 (38.9%) |
| Western [39,54,62,63,67,68,73,74,77,81,87,90,95,100,102,103,105,108,111,116,117,124,130,133,135,136,137,139,140,166,168,169,173,174,177,196,198,201,202,203,204,208,209,210,213,214,215,219,223,224,228,229,230,231,236,244,251,252,261,262] | 60 (27.1%) |
| Eastern [141,144,145,147,148,151,155,157,158,160,180,183,184,185,186,188,190,192,194,234,246,247,254,255,256,257] | 26 (11.8%) |
| Moderate intensity | 80 (36.2%) |
| Western [41,42,43,45,46,52,55,56,57,58,60,64,66,70,72,75,78,79,88,91,92,93,94,96,101,104,106,107,109,110,112,114,115,118,119,123,128,132,134,138,161,163,164,165,167,170,172,179,197,199,200,206,211,216,218,225,226,237,240,242,245] | 61 (27.6%) |
| Eastern [142,143,146,149,150,152,153,154,156,159,181,182,187,189,191,193,233,239,250] | 19 (8.6%) |
| Low intensity | 47 (21.3%) |
| Western [40,44,47,48,49,50,51,53,59,61,65,69,71,76,80,82,83,84,85,89,97,98,99,113,120,121,125,126,127,129,131,171,175,178,195,207,212,217,220,221,222,232,241,248,249,253] | 46 (20.8%) |
| Eastern [238] | 1 (0.5%) |
| Unspecified | 8 (3.6%) |
| Western [86,122,162,176,205,227,243] | 7 (3.2%) |
| Eastern [235] | 1 (0.5%) |
| Control Group Design | k = 221 (%) |
| Waitlist Control | 52 (23.5%) |
| Western [41,42,49,51,53,62,66,68,73,76,78,85,86,87,90,91,92,93,95,96,105,106,107,109,114,115,116,126,127,128,138,161,164,172,179,195,199,204,218,226,227,228,229,230,237] | 46 (20.8%) |
| Eastern [148,154,157,182,235,252] | 6 (2.7%) |
| No Intervention | 52 (23.5%) |
| Western [55,59,60,63,67,69,70,79,80,84,94,101,108,110,117,124,130,131,132,135,137,166,168,171,198,200,202,213,214,215,225,244] | 32 (14.5%) |
| Eastern [141,142,143,144,145,146,147,149,150,151,152,153,155,159,160,180,181,186,190,191] | 20 (9%) |
| TAU | 43 (19.5%) |
| Western [39,47,52,54,58,64,72,75,88,100,112,113,123,139,167,173,174,175,177,197,201,205,206,210,219,223,236,240,245,249,253,261,262] | 33 (14.9%) |
| Eastern [187,189,192,233,234,238,239,256,257,259] | 10 (4.5%) |
| Attention Control | 34 (15.4%) |
| Western [40,44,48,50,56,65,81,89,97,98,99,102,103,104,118,122,129,134,136,140,176,178,203,207,211,216,217,222,231,232,241,243,248] | 33 (14.9%) |
| Eastern [193] | 1 (0.5%) |
| Active Control | 29 (13.1%) |
| Western [43,45,46,57,61,74,82,83,111,120,121,125,133,162,163,170,196,208,209,212,220,224,253] | 23 (19.4%) |
| Eastern [183,184,188,194,248,258] | 6 (2.7%) |
| unspecified | 9 (4.1%) |
| Western [71,77,169,221,242,254] | 6 (2.7%) |
| Eastern [156,158,185] | 3 (1.4%) |
| Combination | 2 (0.9%) |
| Western [119] | 1 (0.5%) |
| Eastern [247] | 1 (0.5%) |
| Outcome | SMD | 95% CI | k (Studies) | N (Participants) | I2 |
|---|---|---|---|---|---|
| Resilience Western | 0.33 | 0.16 to 0.50 | 33 | 3346 | 95.9% |
| Resilience Eastern | 1.02 | 0.39 to 1.65 | 10 | 1451 | 97.7% |
| Anxiety Western | −0.32 | −0.55 to −0.08 | 24 | 2157 | 94.5% |
| Anxiety Eastern | −0.67 | −0.76 to −0.58 | 5 | 279 | 0% |
| Depressive symptoms Western | −0.44 | −0.62 to −0.26 | 14 | 1576 | 91.1% |
| Depressive symptoms Eastern | −0.55 | −2.96 to 1.86 | 2 | 130 | 66.4% |
| Quality of life Western | 0.28 | −0.13 to 0.44 | 33 | 4610 | 98.3% |
| Quality of life Eastern | 0.37 | −0.03 to 0.76 | 5 | 1135 | 85.1% |
| Perceived stress Western | −0.41 | −0.61 to −0.20 | 35 | 2789 | 91.4% |
| Perceived stress Eastern | −0.71 | −3.74 to 2.32 | 2 | 129 | 85.0% |
| Social support Western | −0.12 | −2.56 to 2.32 | 2 | 275 | 89.4% |
| Social support Eastern | 0.21 | −2.67 to 3.09 | 2 | 1314 | 99.7% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blessin, M.; Lehmann, S.; Kunzler, A.M.; van Dick, R.; Lieb, K. Resilience Interventions Conducted in Western and Eastern Countries—A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 6913. https://doi.org/10.3390/ijerph19116913
Blessin M, Lehmann S, Kunzler AM, van Dick R, Lieb K. Resilience Interventions Conducted in Western and Eastern Countries—A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(11):6913. https://doi.org/10.3390/ijerph19116913
Chicago/Turabian StyleBlessin, Manpreet, Sophie Lehmann, Angela M. Kunzler, Rolf van Dick, and Klaus Lieb. 2022. "Resilience Interventions Conducted in Western and Eastern Countries—A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 11: 6913. https://doi.org/10.3390/ijerph19116913
APA StyleBlessin, M., Lehmann, S., Kunzler, A. M., van Dick, R., & Lieb, K. (2022). Resilience Interventions Conducted in Western and Eastern Countries—A Systematic Review. International Journal of Environmental Research and Public Health, 19(11), 6913. https://doi.org/10.3390/ijerph19116913






