Educational Interventions to Promote Cervical Cancer Screening among Rural Populations: A Systematic Review
Abstract
:1. Introduction
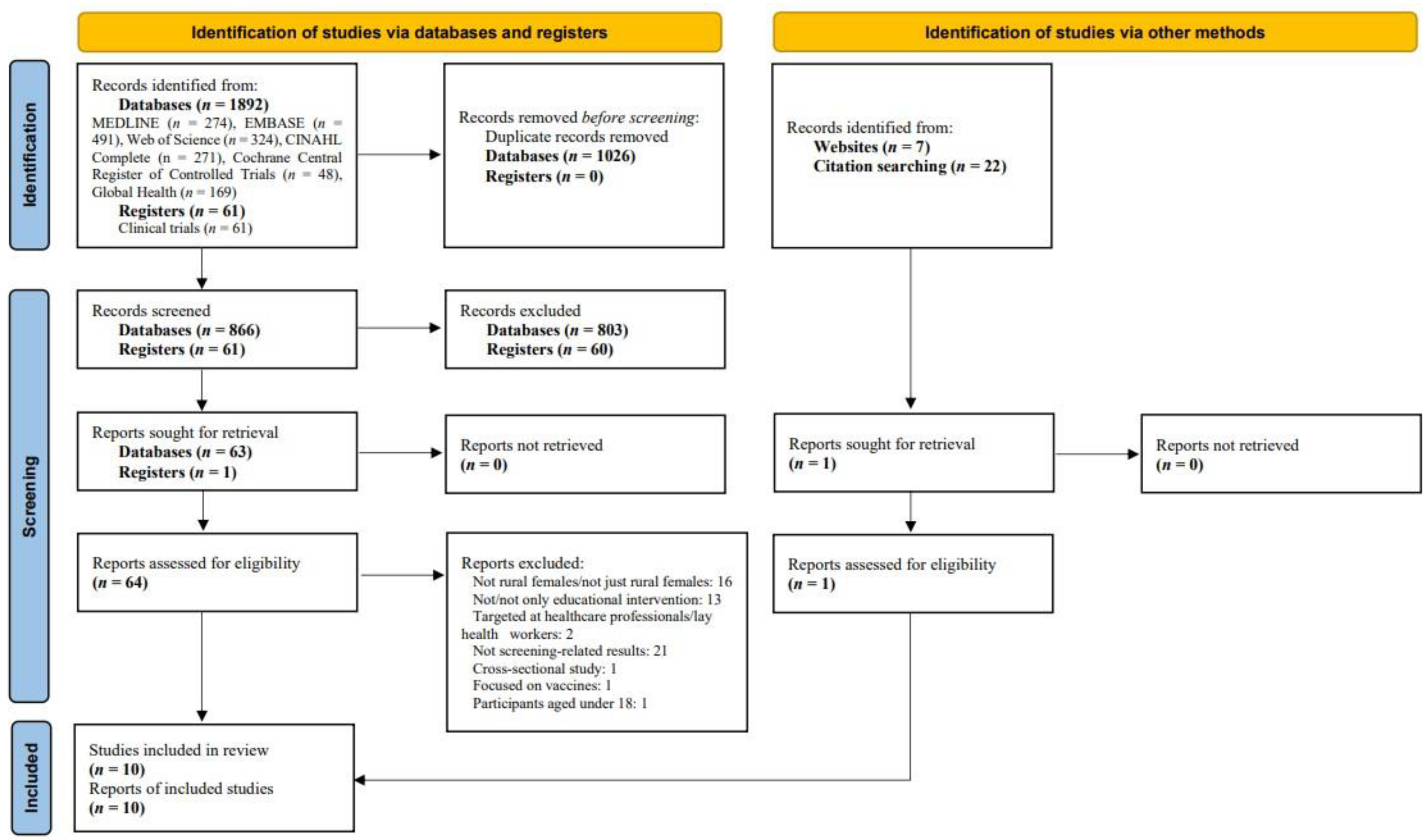
2. Methods
2.1. Data Search and Sources
2.2. Study Inclusion and Exclusion Criteria
2.3. Study Selection
2.4. Quality Appraisal and Data Extraction
2.5. Data Synthesis
3. Results
3.1. Quality Appraisal
3.2. Characteristics of the Study Population
3.3. Characteristics of Educational Interventions for Use among Females in Rural Areas
3.3.1. Theoretical Framework
3.3.2. Intervention Delivery Mode
3.3.3. Intervention Deliverer
3.3.4. Settings
3.3.5. Educational Content
3.3.6. Educational Materials
3.4. Effectiveness of Educational Intervention on Cervical Cancer Screening
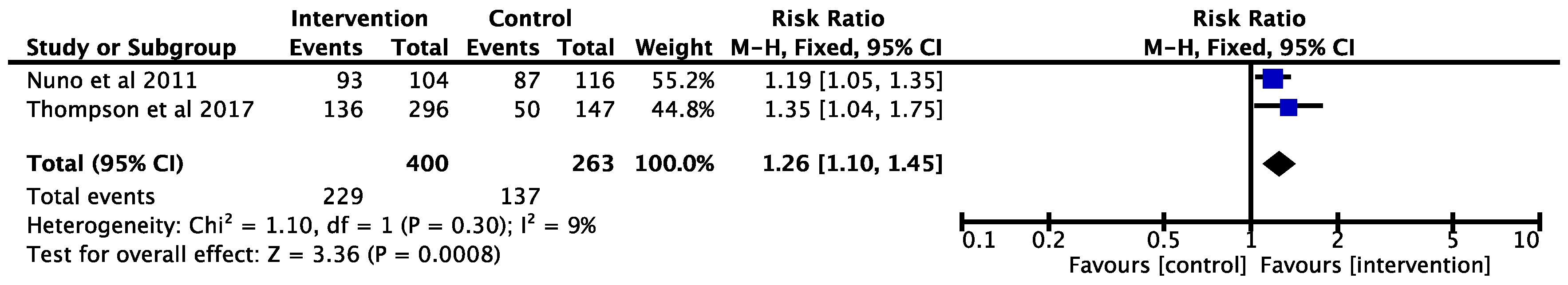
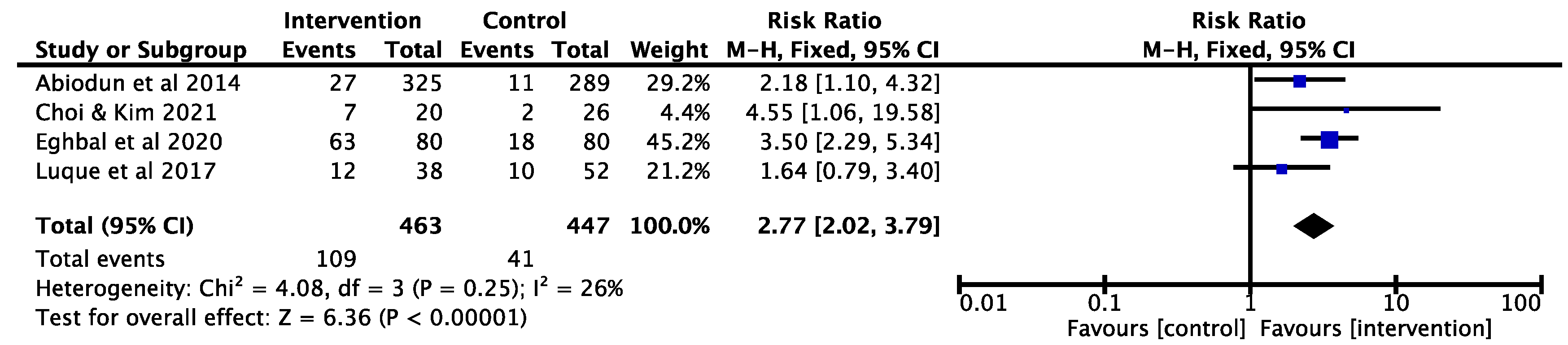
3.4.1. Primary Outcome: Screening Uptake
3.4.2. Secondary Outcomes: Knowledge, Attitude, and Intention
3.4.3. Outcomes by Educational Intervention
Group Education and Individual Education
Healthcare Professional-Led Education and Lay Health Worker-Led Education
4. Discussion
5. Strengths and Limitations
6. Implications
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cancer, I.A.f.R.o. Cancer Today Population Fact Sheets. Available online: http://gco.iarc.fr/today/fact-sheets-populations (accessed on 30 January 2022).
- Blake, K.D.; Moss, J.L.; Gaysynsky, A.; Srinivasan, S.; Croyle, R.T. Making the Case for Investment in Rural Cancer Control: An Analysis of Rural Cancer Incidence, Mortality, and Funding Trends. Cancer Epidemiol. Biomark. Prev. 2017, 26, 992–997. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pan, R.; Zhu, M.; Yu, C.; Lv, J.; Guo, Y.; Bian, Z.; Yang, L.; Chen, Y.; Hu, Z.; Chen, Z.; et al. Cancer incidence and mortality: A cohort study in China, 2008–2013. Int. J. Cancer 2017, 141, 1315–1323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, B.; Xie, X.; Wu, Q.; Zhang, X.; Cheng, H.; Tao, S.; Quan, H. Inequality in the health services utilization in rural and urban china: A horizontal inequality analysis. Medicine 2020, 99, e18625. [Google Scholar] [CrossRef] [PubMed]
- Hart, L.; Larson, E.; Lishner, D. Rural Definitions for Health Policy and Research. Am. J. Public Health 2005, 95, 1149–1155. [Google Scholar] [CrossRef] [PubMed]
- Lourenço, A.E. The meaning of ‘rural’ in rural health: A review and case study from Brazil. Glob. Public Health 2011, 7, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Strasser, R. Rural health around the world: Challenges and solutions. Fam. Pract. 2003, 20, 457–463. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Comprehensive Cervical Cancer Control. In A Guide to Essential Practice; World Health Organization, Ed.; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Sit, J.W.; Chair, S.Y.; Choi, K.C.; Chan, C.W.; Lee, D.T.; Chan, A.W.; Cheung, J.L.; Tang, S.W.; Chan, P.S.; Taylor-Piliae, R.E. Do empowered stroke patients perform better at self-management and functional recovery after a stroke? A randomized controlled trial. Clin. Interv. Aging 2016, 11, 1441–1450. [Google Scholar] [CrossRef] [Green Version]
- Marván, M.; Ehrenzweig, Y.; Catillo-López, R. Knowledge about cervical cancer prevention and psychosocial barriers to screening among Mexican women. J. Psychosom. Obstet. Gynaecol. 2013, 34, 163–169. [Google Scholar] [CrossRef]
- Nuño, T.; Gerald, J.; Harris, R.; Martinez, M.; Estrada, A.; García, F. Comparison of breast and cervical cancer screening utilization among rural and urban Hispanic and American Indian women in the Southwestern United States. Cancer Causes Control CCC 2012, 23, 1333–1341. [Google Scholar] [CrossRef]
- Orwat, J.; Caputo, N.; Key, W.; Sa, J. Comparing Rural and Urban Cervical and Breast Cancer Screening Rates in a Privately Insured Population. Soc. Work Public Health 2017, 32, 1–13. [Google Scholar] [CrossRef]
- So, W.K.W.; Wong, C.L.; Chow, K.M.; Chen, J.M.T.; Lam, W.W.T.; Chan, C.W.H.; Choi, K.C. The uptake of cervical cancer screening among South Asians and the general population in Hong Kong: A comparative study. J. Cancer Policy 2017, 12, 90–96. [Google Scholar] [CrossRef]
- Wang, B.; He, M.; Chao, A.; Engelgau, M.; Saraiya, M.; Wang, L. Cervical Cancer Screening Among Adult Women in China, 2010. Oncologist 2015, 20, 627–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Woldetsadik, A.; Amhare, A.; Bitew, S.; Pei, L.; Lei, J.; Han, J. Socio-demographic characteristics and associated factors influencing cervical cancer screening among women attending in St. Paul’s Teaching and Referral Hospital, Ethiopia. BMC Women’s Health 2020, 20, 70. [Google Scholar] [CrossRef] [PubMed]
- Buchanan Lunsford, N.; Ragan, K.; Smith, J.; Saraiya, M.; Aketch, M. Environmental and Psychosocial Barriers to and Benefits of Cervical Cancer Screening in Kenya. Oncologist 2017, 22, 173–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, C.; Choi, K.; Wong, R.; Chow, K.; So, W.; Leung, D.; Lam, W.; Goggins, W. Examining the Cervical Screening Behaviour of Women Aged 50 or above and Its Predicting Factors: A Population-Based Survey. Int. J. Environ. Res. Public Health 2016, 13, 1195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perng, P.; Perng, W.; Ngoma, T.; Kahesa, C.; Mwaiselage, J.; Merajver, S.; Soliman, A. Promoters of and barriers to cervical cancer screening in a rural setting in Tanzania. Int. J. Gynaecol. Obstet. Off. Organ Int. Fed. Gynaecol. Obstet. 2013, 123, 221–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thapa, N.; Maharjan, M.; Petrini, M.; Shah, R.; Shah, S.; Maharjan, N.; Shrestha, N.; Cai, H. Knowledge, attitude, practice and barriers of cervical cancer screening among women living in mid-western rural, Nepal. J. Gynecol. Oncol. 2018, 29, e57. [Google Scholar] [CrossRef]
- Yang, H.; Li, S.-P.; Chen, Q.; Morgan, C. Barriers to cervical cancer screening among rural women in eastern China: A qualitative study. BMJ Open 2019, 9, e026413. [Google Scholar] [CrossRef] [Green Version]
- Everett, T.; Bryant, A.; Griffin, M.; Martin-Hirsch, P.; Forbes, C.; Jepson, R. Interventions targeted at women to encourage the uptake of cervical screening. Cochrane Database Syst. Rev. (Online) 2011, 5, CD002834. [Google Scholar] [CrossRef]
- Agide, F.; Garmaroudi, G.; Sadeghi, R.; Shakibazadeh, E.; Yaseri, M.; Birhanu, Z.; Tigabu, B. A systematic review of the effectiveness of health education interventions to increase cervical cancer screening uptake. Eur. J. Public Health 2018, 28, 1156–1162. [Google Scholar] [CrossRef] [Green Version]
- Atere-Roberts, J.; Smith, J.; Hall, I. Interventions to increase breast and cervical cancer screening uptake among rural women: A scoping review. Cancer Causes Control 2020, 31, 965–977. [Google Scholar] [CrossRef]
- Saei Ghare Naz, M.; Kariman, N.; Ozgoli, G.; Ghasemi, V.; Fakari, F. Educational Interventions for Cervical Cancer Screening Behavior of Women: A Systematic Review. Asian Pac. J. Cancer Prev. 2018, 19, 875–884. [Google Scholar] [PubMed]
- Weinhold, I.; Gurtner, S. Understanding Shortages of Sufficient Health Care in Rural Areas. Health Policy 2014, 118, 201–214. [Google Scholar] [CrossRef] [PubMed]
- Aljassim, N.; Ostini, R. Health literacy in rural and urban populations: A systematic review. Patient Educ. Couns. 2020, 103, 2142–2154. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Gómez, M.; Ruiz-Pérez, I.; Martín-Calderón, S.; Pastor-Moreno, G.; Artazcoz, L.; Escribà-Agüir, V. Effectiveness of patient-targeted interventions to increase cancer screening participation in rural areas: A systematic review. Int. J. Nurs. Stud. 2019, 101, 103401. [Google Scholar] [CrossRef] [PubMed]
- Page, M.; McKenzie, J.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, C.; Shamseer, L.; Tetzlaff, J.; Akl, E.; Brennan, S.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Institute, J.B. JBI Critical Appraisal Checklist for Randomised Controlled Trials. Available online: https://jbi.global/jbi-search?q=JBI+Critical+Appraisal+Checklist+for+Randomised+Controlled+Trials#gsc.tab=0&gsc.q=JBI%20Critical%20Appraisal%20Checklist%20for%20Randomised%20Controlled%20Trials&gsc.page=1 (accessed on 28 January 2022).
- Institute, J.B. JBI Critical Appraisal Checklist for Quasi-Experimental Studies. Available online: https://jbi.global/jbi-search?q=JBI+Critical+Appraisal+Checklist+for+Quasi-experimental+studies.+#gsc.tab=0&gsc.q=JBI%20Critical%20Appraisal%20Checklist%20for%20Quasi-experimental%20studies.%20&gsc.page=1 (accessed on 28 January 2022).
- Dizon, J.M.; Lizarondo, L. A systematic review of the effectiveness of Evidence Based Practice (EBP) programs for allied health professionals. JBI Evid. Synth. 2010, 8, 1–13. [Google Scholar]
- Nuño, T.; Martinez, M.; Harris, R.; García, F. A Promotora-administered group education intervention to promote breast and cervical cancer screening in a rural community along the U.S.-Mexico border: A randomized controlled trial. Cancer Causes Control CCC 2011, 22, 367–374. [Google Scholar] [CrossRef]
- Sossauer, G.; Zbinden, M.; Tebeu, P.M.; Fosso, G.K.; Untiet, S.; Vassilakos, P.; Petignat, P. Impact of an educational intervention on women’s knowledge and acceptability of human papillomavirus self-sampling: A randomized controlled trial in Cameroon. PLoS ONE 2014, 9, e109788. [Google Scholar] [CrossRef]
- Thompson, B.; Carosso, E.A.; Jhingan, E.; Wang, L.; Holte, S.E.; Byrd, T.L.; Benavides, M.C.; Lopez, C.; Martinez-Gutierrez, J.; Ibarra, G.; et al. Results of a randomized controlled trial to increase cervical cancer screening among rural Latinas. Cancer 2017, 123, 666–674. [Google Scholar] [CrossRef] [Green Version]
- Abiodun, O.A.; Olu-Abiodun, O.O.; Sotunsa, J.O.; Oluwole, F.A. Impact of health education intervention on knowledge and perception of cervical cancer and cervical screening uptake among adult women in rural communities in Nigeria. BMC Public Health 2014, 14, 814. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, J.A.; Kim, O. Cervical Cancer Prevention Education Program for Rural Korean Immigrant Women. West. J. Nurs. Res. 2021, 44, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Eghbal, S.B.; Karimy, M.; Kasmaei, P.; Roshan, Z.A.; Valipour, R.; Attari, S.M. Evaluating the effect of an educational program on increasing cervical cancer screening behavior among rural women in Guilan, Iran. BMC Women’s Health 2020, 20, 149. [Google Scholar] [CrossRef] [PubMed]
- Luque, J.S.; Tarasenko, Y.N.; Reyes-Garcia, C.; Alfonso, M.L.; Suazo, N.; Rebing, L.; Ferris, D.G. Salud es Vida: A Cervical Cancer Screening Intervention for Rural Latina Immigrant Women. J. Cancer Educ. 2017, 32, 690–699. [Google Scholar] [CrossRef]
- Nagamma, T.; Ashok, L.; Konuri, A.; Chandrasekaran, V. Effectiveness of audio-visual and print media intervention on knowledge of cervical health among rural women in Southern India. Niger. Postgrad Med. J. 2020, 27, 343–347. [Google Scholar] [CrossRef]
- Caster, M.M.; Norris, A.H.; Butao, C.; Reese, P.C.; Chemey, E.; Phuka, J.; Turner, A.N. Assessing the Acceptability, Feasibility, and Effectiveness of a Tablet-Based Cervical Cancer Educational Intervention. J. Cancer Educ. 2017, 32, 35–42. [Google Scholar] [CrossRef]
- Thahirabanuibrahim, I.; Logaraj, M. Impact of health education intervention in promoting cervical cancer screening among rural women of Chengalpattu district-The community based interventional study. Clin. Epidemiol. Glob. Health 2021, 12, 100895. [Google Scholar] [CrossRef]
- Das, S.; Mia, M.N.; Hanifi, S.M.; Hoque, S.; Bhuiya, A. Health literacy in a community with low levels of education: Findings from Chakaria, a rural area of Bangladesh. BMC Public Health 2017, 17, 203. [Google Scholar] [CrossRef] [Green Version]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [Green Version]
- Bandura, A. On the Functional Properties of Perceived Self-Efficacy Revisited. J. Manag. 2012, 38, 9–44. [Google Scholar] [CrossRef] [Green Version]
- Bandura, A. Human Agency in Social Cognitive Theory. Am. Psychol. 1989, 44, 1175–1184. [Google Scholar] [CrossRef] [PubMed]
- Bashirian, S.; Mohammadi, Y.; Barati, M.; Moaddabshoar, L.; Dogonchi, M. Effectiveness of the Theory-Based Educational Interventions on Screening of Breast Cancer in Women: A Systematic Review and Meta-Analysis. Int. Q. Community Health Educ. 2019, 40, 219–236. [Google Scholar] [CrossRef] [PubMed]
- Altundağ, S.; Bayat, M. Peer Interaction and Group Education for Adaptation to Disease in Adolescents with Type 1 Diabetes Mellitus. Pak. J. Med. Sci. 2016, 32, 1010–1014. [Google Scholar] [CrossRef] [PubMed]
- Reis, S.; Visser, A.; Frankel, R. Health information and communication technology in healthcare communication: The good, the bad, and the transformative. Patient Educ. Couns. 2013, 93, 359–362. [Google Scholar] [CrossRef] [PubMed]
- Lewin, S.; Munabi-Babigumira, S.; Glenton, C.; Daniels, K.; Bosch-Capblanch, X.; Van Wyk, B.; Odgaard-Jensen, J.; Johansen, M.; Aja, G.; Zwarenstein, M.; et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases (Review). Cochrane Database Syst. Rev. (Online) 2010, 3, CD004015. [Google Scholar] [CrossRef]
- Nkonki, L.; Cliff, J.; Sanders, D. Lay Health Worker Attrition: Important but Often Ignored. Bull. World Health Organ. 2011, 89, 919–923. [Google Scholar] [CrossRef]
- Heerboth, S.; Hennessey, C.; Omondi, B.; Wafula, M.; Mbeya, J.; Rogers, A.; Ressler, D.; Davidson, M.; Moon, T. Knowledge of Obstetric and Neonatal Danger Signs among Community Health Workers in the Rongo Sub-County of Migori County, Kenya: Results of a Community-based Cross-Sectional Survey. Afr. J. Reprod. Health 2020, 24, 121–132. [Google Scholar] [CrossRef]
- Liang, S.; Deng, H.; Liu, S.; Wang, G.; Li, L.; Wang, M.; Pu, J.; Xing, W.; Luo, X.; Ehiri, J.; et al. Competency building for lay health workers is an intangible force driving basic public health services in Southwest China. BMC Health Serv. Res. 2019, 19, 596. [Google Scholar] [CrossRef]
- Chen, Y.; Yin, Z.; Xie, Q. Suggestions to ameliorate the inequity in urban/rural allocation of healthcare resources in China. Int. J. Equity Health 2014, 13, 34. [Google Scholar] [CrossRef] [Green Version]
- Franco, C.M.; Lima, J.G.; Giovanella, L. Primary healthcare in rural areas: Access, organization, and health workforce in an integrative literature review. Cad. Saude Publica 2021, 37, e00310520. [Google Scholar] [CrossRef]
- Baezconde-Garbanati, L.; Agurto, I.; Gravitt, P.; Luciani, S.; Murphy, S.; Ochoa, C.; Gallegos, K.; Barahona, R.; Rodríguez, Y. Barriers and innovative interventions for early detection of cervical cancer. Salud Pública De México 2019, 61, 456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vasiljevic, M.; Ng, Y.L.; Griffin, S.J.; Sutton, S.; Marteau, T.M. Is the intention-behaviour gap greater amongst the more deprived? A meta-analysis of five studies on physical activity, diet, and medication adherence in smoking cessation. Br. J. Health Psychol. 2016, 21, 11–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faries, M.D. Why We Don’t ”Just Do It”: Understanding the Intention-Behavior Gap in Lifestyle Medicine. Am. J. Lifestyle Med. 2016, 10, 322–329. [Google Scholar] [CrossRef] [PubMed]
| Nuno et al., 2011 [32] | Sossauer et al., 2014 [33] | Thompson et al., 2017 [34] | |
|---|---|---|---|
| Q1 | U | Y | U |
| Q2 | U | U | U |
| Q3 | Y | Y | Y |
| Q4 | U | U | Y |
| Q5 | U | U | Y |
| Q6 | U | U | Y |
| Q7 | Y | Y | Y |
| Q8 | Y | Y | Y |
| Q9 | Y | Y | Y |
| Q10 | Y | Y | Y |
| Q11 | Y | Y | Y |
| Q12 | Y | Y | Y |
| Q13 | NA | NA | NA |
| Total score | 7 | 8 | 10 |
| Abiodun, 2014 [35] | Choi, 2021 [36] | Eghbal, 2020 [37] | Luque, 2017 [38] | Nagamma, 2020 [39] | Caster, 2017 [40] | Thahirabanuibrahim, 2021 [41] | |
|---|---|---|---|---|---|---|---|
| Q1 | Y | Y | Y | Y | Y | Y | Y |
| Q2 | Y | Y | Y | Y | Y | Y | Y |
| Q3 | U | U | Y | Y | Y | NA | NA |
| Q4 | Y | Y | Y | Y | Y | N | N |
| Q5 | Y | Y | Y | Y | Y | Y | Y |
| Q6 | N | Y | Y | Y | Y | Y | Y |
| Q7 | Y | Y | Y | Y | Y | Y | Y |
| Q8 | Y | Y | Y | Y | Y | Y | Y |
| Q9 | Y | Y | Y | Y | Y | Y | Y |
| Total score | 7 | 8 | 9 | 9 | 9 | 7 | 7 |
| Study | Study Design | Population | Screening | Intervention | Comparison | Follow-Up | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Target People | Financial Situation | Educational Background | Sample Size (IG/CG) | Duration | Withdraw (IG/CG) | |||||
| Nuño et al., 2011, USA [32] | RCT | 50–66 years and even older | Average monthly income: IG: $895 CG: $933 | 77.4% in elementary school or lower | 381 (190/191) | Pap smear | Promotora- administered group education | Usual care | 2 years | 10 (7/3) |
| Sossauer et al., 2014, Cameroon [33] | RCT | 25–65 years | Not report | High school graduate took the largest account (56.3%) | 302 (152/150) | HPV self-sampling | Educational intervention | Usual care | Immediately after the intervention | 1 (0/1) |
| Thompson et al., 2017, USA [34] | RCT (Three-armed) | 21–64 years; have not had a Pap test within the past 3 years | 24.9% had health insurance now, 18.3% never had | 93.2% in high school or lower | 443 (296/147) | Pap smear | A: culturally appropriate video B: culturally appropriate in home Promotora-led educational intervention | Usual care | 7 months | 40 (28/12) |
| Abiodun et al., 2014, Nigeria [35] | QE (with a control group) | 25–64 years | Average monthly income: 76.9% lower than 15,000 Naira (lower than $40) | 86.9% in secondary school or lower | 700 (350/350) | VIA | Multiple media health education based on a movie | Breast cancer education | 13 weeks | 86 (25/61) |
| Choi and Kim, 2021, USA [36] | QE (with a control group) | 21–65 years, have not had a Pap test within the past 3 years | Most (97.8%) had health insurance | College/university graduate took the largest account (73.9%) | 46 (20/26) | Pap smear | Cervical cancer prevention education program | Not report | 8 weeks | 0 |
| Eghbal et al., 2020, Iran [37] | QE (with a control group) | 20–65 years and married at least once | Not report | 67.5% in elementary or lower | 160 (80/80) | Pap smear | Educational program | Usual care | 2 months | 0 |
| Luque et al., 2017, USA [38] | QE (with a control group) | 22–62 years and had not received a Pap test in 2 years or more | Median weekly income: $250–$500 | Not report | 90 (38/52) | Pap test | Salud es Vida | Nutrition class | 6 months | 0 |
| Nagamma et al., 2020, India [39] | QE (with a control group) | 18–55 years | Not report | Secondary graduate took the largest account (43.4%) | 166 (82/84) | Pap smear | Audio-visual media intervention | Pamphlet | Immediately after the intervention | 0 |
| Caster et al., 2017, Malawi [40] | QE (single group pre-post test) | 18–77 years | Monthly income: most (74%) less than $42 | Standard 4–8 took the largest account (46%) | 243 (117 in pre-and post-test group) | Not report | Tablet-based education program | Immediately after the intervention | —— | —— |
| Thahirabanuibrahim and Loga raj, 2021, India [41] | QE (single group pre-post test) | 30–60 years | Lower class took the largest account (32.43%) | Primary graduate took the largest account (32.4%) | 370 | Pap smear | Health education model | Not report | —— | —— |
| Study | Intervention | Intervention Components | |||||
|---|---|---|---|---|---|---|---|
| Theoretical Framework | Delivery Mode | Dosage | Intervener | Settings | |||
| Duration | Frequency | ||||||
| Nuño et al., 2011, USA [32] | Promotora-administered group education | Social Cognitive Theory | Face-to-face group educational sessions: 3–12 women in one group | 2 h a session | Participants needed to attend at least one class | Promotora | Community (participants’ home) |
| Sossauer et al., 2014, Cameroon [33] | Educational intervention | Not report | Face-to-face group education | Discussion: 5 min, Video: 6 min | Not report | Healthcare professional (research team) | Healthcare center |
| Thompson et al., 2017, USA [34] | A: culturally appropriate video B: culturally appropriate in home Promotora-led educational intervention | Social Cognitive Theory | A: Self-directed learning: watching video B: Individual home visit | A: video: 13 min B: Not report | A: Not report B: once | A: self-direct learning B: Promotora | Community (participants’ home) |
| Abiodun et al., 2014, Nigeria [35] | Multiple media health education based on a movie | Not report | Face-to-face group educational sessions, 50 women in one group | More than 4 h a day | 7 days | Healthcare professional (research team) | Not report |
| Choi and Kim, 2021 USA [36] | Cervical cancer prevention education program | Theory of Planned Behavior | Face-to-face group educational sessions | 1 h a session | Once a week for 4 weeks | Healthcare professional (research team) | Community (church) |
| Eghbal et al., 2020, Iran [37] | Educational program | Health Belief Model | Face-to-face group educational sessions | 50–60 min each session | Once a week for 3 weeks | Healthcare professional (research team) | Healthcare center |
| Luque et al., 2017, USA [38] | Salud es Vida | Social Cognitive Theory and Popular Education | Face-to-face group educational sessions, an average of 7 women in one group | 3 h each class | A total of 17 classes held with small groups | Promotora | Community (public places in the community and individual homes) |
| Nagamma et al., 2020, India [39] | Audio-visual media intervention | Not reported | A: Face-to-face group educational session | A: 30 min | A: seven sessions | Healthcare professional (research team) | Community |
| Caster et al., 2017, Malawi [40] | Tablet-based education program | Not report | Tablet | 30 min | Once | Healthcare professional (research team) | Not reported |
| Thahirabanuibrahim and Logaraj, 2021, India [41] | Health education model | Theory of Planned Behavior | Video presentation | Not report | Once | Healthcare professional (research team) | Community |
| Author, Year | Basic Knowledge | Psychological Issues | Barriers to Screening and Overcoming Strategies | Locally Available Resources |
|---|---|---|---|---|
| Nuño et al., 2011 [32] | ü | ü | ü | |
| Sossauer et al., 2014 [33] | ü | ü | ||
| Thompson et al., 2017 [34] | ü | ü | ü | |
| Abiodun, et al., 2014 [35] | ü | |||
| Choi and Kim, 2021 [36] | ü | ü | ||
| Eghbal et al., 2020 [37] | ü | ü | ü | ü |
| Luque et al., 2017 [38] | ü | ü | ü | |
| Nagamma et al., 2020 [39] | ü | |||
| Caster et al., 2017 [40] | ü | ü | ||
| Thahirabanuibrahim and Logaraj, 2021 [41] | ü | ü |
| Author, Year | Audio-Visual Materials | Reading Materials |
|---|---|---|
| Video/Audio | Leaflet/Brochure/Pamphlet/Booklet | |
| Nuño et al., 2011 [32] | Not report | |
| Sossauer et al., 2014 [33] | ü | |
| Thompson et al., 2017 [34] | ü | ü |
| Abiodun, et al., 2014 [35] | ü | ü |
| Choi and Kim, 2021 [36] | Not report | |
| Eghbal et al., 2020 [37] | ü | ü |
| Luque et al., 2017 [38] | ü | ü |
| Nagamma et al., 2020 [39] | ü | ü |
| Caster et al., 2017 [40] | ü | |
| Thahirabanuibrahim and Logaraj, 2021 [41] | ü | |
| Author, Year, Study Site | Outcomes | Conclusion |
|---|---|---|
| Nuño et al., 2011, USA [32] | Uptake: post-intervention 89% of rural females in IG got screening while in CG it was 75% (p < 0.01) | A Promotora-based educational intervention effective on increasing cervical cancer screening uptake |
| Sossauer et al., 2014, Cameroon [33] | Knowledge: post-intervention 81.6% of rural females in IG got good knowledge while in CG it was 10.1% (p < 0.01) Acceptability: no significant difference in post-intervention level between the IG and CG Willingness: no significant difference in post-intervention level between the IG and CG | Educational intervention effective on increasing knowledge about HPV and cervical cancer, but not on Self-HPV acceptability |
| Thompson et al., 2017, USA [34] | Uptake: post-intervention 53.4% of rural females in IG B got screening, while in CG it was 34.0% (p < 0.01); No significant difference between IG A and CG Knowledge: post-intervention correct response rate of IG A was 40.7%; IG B was 36.7%; CG was 26.7% (p < 0.05) Self-efficacy: no significant difference in post-intervention self-efficacy level between the IG and CG | Culturally appropriate in-home Promotora-led educational intervention successful in increasing cervical cancer screening |
| Abiodun et al., 2014, Nigeria [35] | Uptake: post-intervention 8.3% of rural females in IG got screening while in CG it was 3.8% (p < 0.05) Knowledge: post-intervention score of IG was (25.69 ± 6.20), and CG was (2.22 ± 6.04) (p < 0.01) Awareness: post-intervention 100% rural females in IG aware while in CG it was 10.7% (p < 0.01) Perception: post-intervention score of IG was (4.43 ± 0.92), and CG was (1.17 ± 0.88) (p < 0.01) Willingness: no significant difference in post-intervention willingness between the IG and CG | Multiple media health education based on a movie effective in creating awareness and improving the knowledge, perception, and uptake of cervical cancer screening |
| Choi and Kim, 2021, USA [36] | Uptake: post-intervention 35.5% of rural females in IG got screening while in CG it was 7.7% (p < 0.05) | Cervical cancer prevention education program effective on increase Pap screening rate |
| Eghbal et al., 2020, Iran [37] | Uptake: IG increased from 18.75% to 78.75% while CG increased from 16.25% to 22.5% (p < 0.01) Knowledge: post-intervention score of IG was (25.2 ± 2.1), and CG was (19.7 ± 1.6) (p < 0.01) Self-efficacy: post-intervention score of IG was (24.7 ± 1.0), and CG was (19.1 ± 3.0) (p < 0.01) | Educational program effective on increasing cervical cancer screening behavior among rural women |
| Luque et al., 2017, USA [38] | Uptake: no significant difference between IG and CG Knowledge: post-intervention score of IG was (11.5 ± 2.1), and CG was (10.7 ± 1.7) (p < 0.05) Self-efficacy: no significant difference in post-intervention self-efficacy between the IG and CG | Group educational intervention associated with increased cervical cancer knowledge, but not uptake of Pap test |
| Nagamma et al., 2020, India [39] | Knowledge: post-intervention knowledge about Pap smear increased in both two groups (p < 0.01) | Face-to-face interactive sessions positive on increasing cervical cancer-related knowledge |
| Caster et al., 2017, Malawi [40] | Knowledge: post-test correct respond about screening increased (p < 0.01) Desire: post-test 93% participants showed a desire for cervical cancer screening | Tablet-based educational program effective, feasible and acceptable to disseminate cervical cancer information |
| Thahirabanuibrahim and Logaraj, 2021, India [41] | Knowledge: pre-test score 1.34, post-test score 2.34 (p < 0.05) Attitude: pre-test score 1.11, post-test score 1.96 (p < 0.01) Uptake: post-test: 30.1% participants finished the screening | Health education model proved to be efficacious on cervical cancer prevention |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, M.; Sit, J.W.H.; Chan, D.N.S.; Akingbade, O.; Chan, C.W.H. Educational Interventions to Promote Cervical Cancer Screening among Rural Populations: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 6874. https://doi.org/10.3390/ijerph19116874
Zhang M, Sit JWH, Chan DNS, Akingbade O, Chan CWH. Educational Interventions to Promote Cervical Cancer Screening among Rural Populations: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(11):6874. https://doi.org/10.3390/ijerph19116874
Chicago/Turabian StyleZhang, Mengyue, Janet W. H. Sit, Dorothy Ngo Sheung Chan, Oluwadamilare Akingbade, and Carmen W. H. Chan. 2022. "Educational Interventions to Promote Cervical Cancer Screening among Rural Populations: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 11: 6874. https://doi.org/10.3390/ijerph19116874
APA StyleZhang, M., Sit, J. W. H., Chan, D. N. S., Akingbade, O., & Chan, C. W. H. (2022). Educational Interventions to Promote Cervical Cancer Screening among Rural Populations: A Systematic Review. International Journal of Environmental Research and Public Health, 19(11), 6874. https://doi.org/10.3390/ijerph19116874







