“Lived the Pandemic Twice”: A Scoping Review of the Unequal Impact of the COVID-19 Pandemic on Asylum Seekers and Undocumented Migrants
Abstract
:1. Introduction
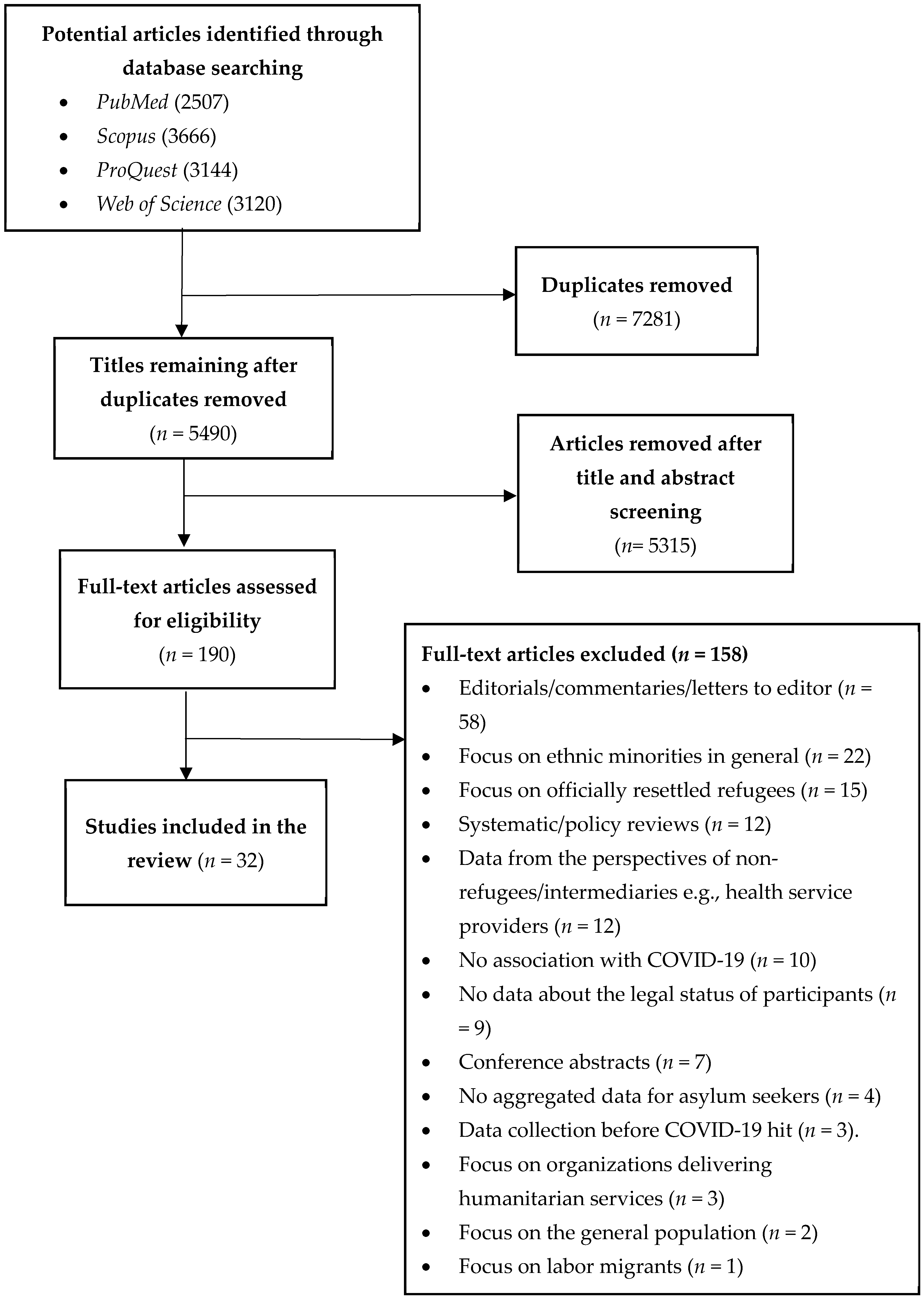
2. Methods
2.1. Inclusion and Exclusion Criteria
2.2. Study Selection
2.3. Data Analysis and Synthesis
2.4. Patient and Public Involvement
2.5. Ethics Approval
3. Results
| First Author | Year | Country of Study | Population | Ethnicity | Methodology | Data Collection Approach | Main Framework Pathway/s Captured and Outcome Reported |
|---|---|---|---|---|---|---|---|
| Al-Awaida [23] | 2021 | Jordan | Refugees seeking asylum | Syrian | Quantitative | Survey (n = 2380) | Differential adverse consequences of control measures. Demonstrated a high prevalence of PTSD, in which PTSD showed incidence of 82.5% and 66.5% in Syrian refugees and Jordanian populations, respectively. |
| Alsharif [24] | 2021 | Saudi Arabia | Undocumented migrants | Sub-Saharan Africa and Southeast Asia | Qualitative | Interview (n = 15) | Differential disease consequences and differential effectiveness of control measures. Undocumented migrants do not access health care due to fear of deportation. |
| Aragona [25] | 2021 | Italy | Asylum seekers, refugees, and forced and undocumented migrants. | Africa, Europe, Middle East, South/Central America, and Asia | Quantitative | Survey (n = 81) | Differential adverse consequences of control measures. Mental health treatment adherence negatively impacted by COVID-19, 32% discontinued pharmacological treatment, and 52% discontinued psychotherapy. |
| Aragona [26] | 2020 | Italy | Asylum seekers, refugees, forced migrants, undocumented migrants | Africa, Europe, Middle East, South/Central America, and Asia | Quantitative | Electronic medical record data (n = 555) | Differential adverse consequences of control measures. Mental health follow-up treatment attendance shows higher decline compared to previous years (30% in 2020 vs. 17% in 2017–2019). |
| Aung [27] | 2021 | Malaysia | Refugees seeking asylum | Rohingya | Quantitative | Survey (n = 283) | Differential vulnerability to infection. Demonstrated high health and social vulnerabilities for the COVID-19 infection. |
| Baggio [28] | 2021 | Switzerland | Undocumented migrants | N/A | Quantitative | Survey (n = 215) | Differential vulnerability to infection and differential disease consequences. Proportion of positive tests significantly higher among undocumented migrants (32.1% vs. 23.6%) compared to host population. |
| Banati [29] | 2020 | Lebanon | Refugees seeking asylum | Syrian and Palestinian | Qualitative | Interview (n = 100) | Differential adverse consequences of control measures. COVID-19 compounds pre-existing disadvantage: issues in getting food and supplies, intra-family problems, fear of violence and scapegoating, anxiety about the future, social isolation, lack of privacy worsening. |
| Bigelow [30] | 2021 | United States | Undocumented migrants | Latinx | Quantitative | Electronic medical record (n = 1786) | Differential exposure and differential disease consequences. Highest positivity rate detected among Latinx at (31.5%) 10 times higher than whites. |
| Blackburn [31] | 2021 | United States | Undocumented migrants and service providers | Hispanic | Qualitative | Interview (n = 13) | Differential adverse consequences of control measures. Anti-immigrant rhetoric has made undocumented migrants less willing to access healthcare. |
| Budak [32] | 2020 | Turkey | Asylum seekers | Syrian | Quantitative | Survey (n = 414) | Differential disease consequences. Some groups underestimate seriousness of COVID-19; not enough information or PPE is available. |
| Burton [7] | 2020 | Switzerland | Undocumented migrants | Latin American, Asia, Africa, and Non-EU Europe | Mixed methods | Survey (n =117) and interview (n = 17) | Differential disease consequences, differential social consequences and differential adverse consequences of control measures. Identified high prevalence of exposure to COVID-19, poor mental health along with frequent avoidance of health care, and loss of work and income. |
| Cervantes [33] | 2021 | United States | Undocumented migrants | Latinx | Qualitative | Interview (n = 60) | Differential exposure, differential social consequences, and differential effectiveness of control measures. Patients who survived hospitalisation described initial disease misinformation and economic and immigration fears as having driven exposure and delays in presentation. |
| Deal [34] | 2021 | United Kingdom | Asylum seekers and undocumented migrants | Africa, Venezuela, Eastern Mediterranean and Europe, and Sri Lanka | Qualitative | Interview (n = 32) | Differential exposure, differential social consequences, and differential effectiveness of control measures. Majority are hesitant in accepting vaccines and facing multiple unique barriers to access (lack of accessible information and poor health literacy, fear of deportation, distrust). |
| Devillanova [35] | 2020 | Italy | Undocumented migrants | n/A | Quantitative | Survey (n = 1590) | Differential exposure, differential disease consequences, and differential effectiveness of control measures. Lockdown triggered sharp reduction in health visits, increased number of presentations with COVID-19 symptoms, shutdown of outpatient clinics, and patients reporting deteriorating housing conditions. |
| Fiorini [36] | 2020 | Italy | Undocumented migrants | Africa, Asia, Latin America, Eastern Europe | Quantitative | Survey (n = 272) | Differential exposure, differential vulnerability to infection, and differential disease consequences. All had risk factors and predispositions that increased severity and outcomes. |
| Gosselin [37] | 2021 | France | Undocumented migrants and asylum seekers | Sub-Saharan Africa | Quantitative | Survey (n = 100) | Differential effectiveness of control measures and differential adverse consequences of control measures. Food insecurity was more often reported during lockdown than before (62% vs. 52%) and increased rate of severe depression post lockdown. |
| Hajjar [38] | 2021 | Lebanon | Refugees seeking asylum | Syrian | Quantitative | Survey (n = 129) | Differential exposure and differential adverse consequences of control measures. Documented massive job loss and reduced wages, discontinued education for children, and high stress and anxiety due to lack of assistance. |
| Hamadneh [39] | 2021 | Jordan | Refugees seeking asylum | Syrian | Quantitative | Survey (n = 389) | Differential effectiveness of control measures. Refugee mothers were knowledgeable about COVID-19 transmission and prevention but lacked knowledge about transmission between mother and child and smoking risks associated with COVID-19. |
| Karajerjian [40] | 2021 | Lebanon | Refugees seeking asylum | Syrian | Qualitative | FGD and interview (n = 50) | Differential exposure and differential adverse consequences of control measures. COVID-19 compounds disadvantage and mental health issues for refugee women already in precarious situations. Fear and anxiety about the disease is high, and access to healthcare is uncertain. |
| Kondilis [41] | 2021 | Greece | Asylum seekers and refugees | N/A | Quantitative | Retrospective surveillance data | Differential disease consequences. Twenty-five COVID-19 outbreaks were identified in refugee and asylum-seeker reception facilities. |
| Longchamps [42] | 2021 | France | Undocumented migrants | Europe, Africa, Eastern Mediterranean | Quantitative | Survey (n = 240) | Differential vulnerability to infection and differential effectiveness of control measures. Reported significant vaccine hesitancy (41%). |
| MacCarthy [43] | 2020 | United States | Undocumented migrants, asylum and humanitarian visa holders | Latinx | Mixed methods | Survey and interview (n = 52) | Differential adverse consequences of control measures Participants reported increased interpersonal conflict and alcohol consumption due to lockdown; disruption in accessing medical care, job loss, and no assistance for those undocumented. |
| Martuscelli [44] | 2020 | Brazil | Refugees seeking asylum | Syria, DRC, Guyana, Venezuela | Qualitative | Interview (n = 29) | Differential adverse consequences of control measures. Refugees are affected by border closures and their rights to documentation, healthcare, and social assistance (state emergency benefit) are violated. |
| Martuscelli [45] | 2021 | Brazil | Refugees seeking asylum | Syria, DRC, Guyana, Venezuela | Qualitative | Interview (n = 29) | Differential exposure, differential effectiveness of control measures, and differential adverse consequences of control measures. Continued lack of culturally and linguistically adapted information makes accessing services difficult. |
| Quandt [46] | 2020 | United States | Undocumented migrants, mixed-status families, and residents | Latinx | Mixed methods | Survey (n = 105) | Differential exposure, differential effectiveness of control measures, and differential adverse consequences of control measures. Families engaged in frequent interpersonal contact that could expose community members and themselves to COVID-19. |
| Quandt [47] | 2021 | United States | Undocumented migrants, mixed-status families, and residents | Latinx | Mixed methods | Survey (n =105) | Differential exposure, differential effectiveness of control measures, and differential adverse consequences of control measures. Rural workers reported fewer workplace protective measures for COVID-19. Fear and anxiety, particularly about finances and children, dominated their experiences. |
| Redditt [48] | 2020 | Canada | Asylum seekers | N/A | Quantitative | COVID-19 outbreak management data (n = 60) | Differential effectiveness of control measures and differential disease consequences. Documented a very high rate of infection in a humanitarian shelter (41.7% of tested residents are positive). |
| Reynolds [49] | 2021 | Mexico | Asylum seekers and service provides | El Salvador, Nicaragua, Honduras, Mexico, Cuba, Bolivia, and Guatemala | Qualitative | Interview (n = 30) | Differential effectiveness of control measures and differential adverse consequences of control measures. COVID-19 caused mental health burdens and less adherence to disease-reduction strategies. Control measures created distrust and decreased health care services use. |
| Sabri [50] | 2021 | United States | Undocumented immigrants and service providers | Asian, Latina, African | Qualitative | Interview (n = 62) | Differential adverse consequences of control measures. COVID-19 is connected to increased intimate partner violence, and assistance is not available to undocumented women. |
| Serafini [51] | 2021 | United States | Undocumented migrants | Hispanic | Quantitative | Survey (n = 35) | Differential adverse consequences of control measures. Participants reported worsened anxiety (49%) and depression (46%) levels due to the pandemic. |
| Terp [52] | 2021 | United States | Undocumented migrants | N/A | Quantitative | Review of death reports (n = 35) | Differential vulnerability to infection and differential disease consequences. COVID-19 is a leading cause of death rate among undocumented migrants. |
| Turunen [53] | 2021 | Finland | Asylum seekers | N/A | Quantitative | Screening tool + medical record review and interviews (n = 260) | Differential exposure and differential disease consequences. High COVID-19 infection rate identified among asylum seekers. |
3.1. Differential Exposure
3.2. Differential Vulnerability to Infection
3.3. Differential Disease Consequences
3.4. Differential Social Consequences of the Disease
3.5. Differential Effectiveness of Control Measures
3.5.1. Information and Communication
3.5.2. Vaccination
3.6. Differential Adverse Consequences of Control Measures
3.6.1. Differential Mental Health Consequences
3.6.2. Restricted Access to Health Care
3.6.3. Exclusion from Pandemic Induced Policy Measures
3.6.4. Visa Processing Delays
3.6.5. Economic Instability
3.6.6. Social Isolation
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- WHO. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 5 April 2022).
- WHO. ApartTogether Survey: Preliminary Overview of Refugees and Migrants Self-Reported Impact of COVID-19; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Brickhill-Atkinson, M.; Hauck, F.R. Impact of COVID-19 on Resettled Refugees. Prim. Care 2021, 48, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Kluge, H.H.P.; Jakab, Z.; Bartovic, J.; D’Anna, V.; Severoni, S. Refugee and migrant health in the COVID-19 response. Lancet 2020, 395, 1237–1239. [Google Scholar] [CrossRef]
- Nisanci, A.; Kahraman, R.; Alcelik, Y.; Kiris, U. Working with refugees during COVID-19: Social worker voices from Turkey. Int. Soc. Work 2020, 63, 685–690. [Google Scholar] [CrossRef]
- Thomas, C.M.; Osterholm, M.T.; Stauffer, W.M. Critical Considerations for COVID-19 Vaccination of Refugees, Immigrants, and Migrants. Am. J. Trop. Med. Hyg. 2021, 104, 433–435. [Google Scholar] [CrossRef] [PubMed]
- Burton-Jeangros, C.; Duvoisin, A.; Lachat, S.; Consoli, L.; Fakhoury, J.; Jackson, Y. The Impact of the COVID-19 Pandemic and the Lockdown on the Health and Living Conditions of Undocumented Migrants and Migrants Undergoing Legal Status Regularization. Front. Public Health 2020, 8, 940. [Google Scholar] [CrossRef]
- Mukumbang, F.C. Pervasive systemic drivers underpin COVID-19 vulnerabilities in migrants. Int. J. Equity Health 2021, 20, 146. [Google Scholar] [CrossRef]
- Etti, M.; Fofie, H.; Razai, M.; Crawshaw, A.F.; Hargreaves, S.; Goldsmith, L.P. Ethnic minority and migrant underrepresentation in COVID-19 research: Causes and solutions. EClinical Med. 2021, 36, 100903. [Google Scholar] [CrossRef]
- Mukumbang, F.C. Are asylum seekers, refugees and foreign migrants considered in the COVID-19 vaccine discourse? BMJ Glob. Health 2020, 5, e004085. [Google Scholar] [CrossRef]
- Bojorquez-Chapela, I.; Infante, C.; Larrea-Schiavon, S.; Vieitez-Martinez, I. In-Transit Migrants and Asylum Seekers: Inclusion Gaps In Mexico’s COVID-19 Health Policy Response. Health Aff. 2021, 40, 1154–1161. [Google Scholar] [CrossRef]
- Knights, F.; Carter, J.; Deal, A.; Crawshaw, A.F.; Hayward, S.E.; Jones, L.; Hargreaves, S. Impact of COVID-19 on migrants’ access to primary care and implications for vaccine roll-out: A national qualitative study. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2021, 71, e583–e595. [Google Scholar] [CrossRef]
- UNHCR. Report of the United Nations High Commissioner for Refugees; United Nations: New York, NY, USA, 2021. [Google Scholar]
- Reed, H. Forced migration and undocumented migration and development. CUNY Inst. Demogr. Res. 2018, 15, 2021. [Google Scholar]
- Hintermeier, M.; Gencer, H.; Kajikhina, K.; Rohleder, S.; Hövener, C.; Tallarek, M.; Spallek, J.; Bozorgmehr, K. SARS-CoV-2 among migrants and forcibly displaced populations: A rapid systematic review. J. Migr. Health 2021, 4, 100056. [Google Scholar] [CrossRef] [PubMed]
- Júnior, J.G.; de Sales, J.P.; Moreira, M.M.; Pinheiro, W.R.; Lima, C.K.T.; Neto, M.L.R. A crisis within the crisis: The mental health situation of refugees in the world during the 2019 coronavirus (2019-nCoV) outbreak. Psychiatry Res. 2020, 288, 113000. [Google Scholar] [CrossRef]
- Katikireddi, S.V.; Lal, S.; Carrol, E.D.; Niedzwiedz, C.L.; Khunti, K.; Dundas, R.; Diderichsen, F.; Barr, B. Unequal impact of the COVID-19 crisis on minority ethnic groups: A framework for understanding and addressing inequalities. J. Epidemiol. Community Health 2021, 75, 970. [Google Scholar] [CrossRef]
- Mackey, K.; Ayers, C.K.; Kondo, K.K.; Saha, S.; Advani, S.M.; Young, S.; Hunter, S.; Rusek, M.; Anderson, J.; Veazie, S.; et al. Racial and Ethnic Disparities in COVID-19–Related Infections, Hospitalizations, and Deaths: A Systematic Review. Ann. Intern. Med. 2021, 174, 362–373. [Google Scholar] [CrossRef]
- Sze, S.; Pan, D.; Nevill, C.R.; Gray, L.J.; Martin, C.A.; Nazareth, J.; Minhas, J.S.; Divall, P.; Khunti, K.; Abrams, K.R. Ethnicity and clinical outcomes in COVID-19: A systematic review and meta-analysis. EClinicalMedicine 2020, 29, 100630. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- World Bank. The World by Income and Region: World Bank. Available online: https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html (accessed on 19 December 2021).
- Fereday, J.; Muir-Cochrane, E. Demonstrating Rigor Using Thematic Analysis: A Hybrid Approach of Inductive and Deductive Coding and Theme Development. Int. J. Qual. Methods 2006, 5, 80–92. [Google Scholar] [CrossRef]
- Al-Awaida, W.; Al-Ameer, H.J.; Al-Turk, H.; Al Bawareed, O.; Khalil, R.; Al Deek, A.; Fatima, G.; Imraish, A.; Mohanad Al-Dabet, M.; Akash, M.W. Psychological effects of quarantine on Syrian refugees, compared to the Jordanian populations. Int. Migr. 2021, 60, 12847. [Google Scholar] [CrossRef]
- Alsharif, F. Undocumented migrants in Saudi Arabia: COVID-19 and amnesty reforms. Int. Migr. 2021. [Google Scholar] [CrossRef]
- Aragona, M.; Tumiati, M.C.; Ferrari, F.; Viale, S.; Nicolella, G.; Barbato, A.; Cavani, A.; Costanzo, G.; Mirisola, C. Psychopathological effects of the Coronavirus (Sars-CoV-2) imposed lockdown on vulnerable patients in treatment in a mental health outpatient department for migrants and individuals in poor socioeconomic conditions. Int. J. Soc. Psychiatry 2021, 68, 203–209. [Google Scholar] [CrossRef]
- Aragona, M.; Barbato, A.; Cavani, A.; Costanzo, G.; Mirisola, C. Negative impacts of COVID-19 lockdown on mental health service access and follow-up adherence for immigrants and individuals in socio-economic difficulties. Public Health 2020, 186, 52–56. [Google Scholar] [CrossRef]
- Aung, T.S.; Fischer, T.B.; Wang, Y.H. Conceptualization of Health and Social Vulnerability of Marginalized Populations During COVID-19 Using Quantitative Scoring Approach. J. Immigr. Refug. Stud. 2022, 20, 1–16. [Google Scholar] [CrossRef]
- Baggio, S.; Jacquerioz, F.; Salamun, J.; Spechbach, H.; Jackson, Y. Equity in access to COVID-19 testing for undocumented migrants and homeless persons during the initial phase of the pandemic. J. Migr. Health 2021, 4, 100051. [Google Scholar] [CrossRef]
- Banati, P.; Jones, N.; Youssef, S. Intersecting Vulnerabilities: The Impacts of COVID-19 on the Psycho-emotional Lives of Young People in Low- and Middle-Income Countries. Eur. J. Dev. Res. 2020, 32, 1613–1638. [Google Scholar] [CrossRef]
- Bigelow, B.F.; Saxton, R.E.; Flores-Miller, A.; Mostafa, H.H.; Loss, M.J.; Phillips, K.H.; Moore, A.M.; Hale, W.D.; Tolson, T.M.; McCann, N.S.; et al. Community Testing and SARS-CoV-2 Rates for Latinxs in Baltimore. Am. J. Prev. Med. 2021, 60, E279–E284. [Google Scholar] [CrossRef]
- Blackburn, C.C.; Sierra, L.A. Anti-Immigrant Rhetoric, Deteriorating Health Access, and COVID-19 in the Rio Grande Valley, Texas. Health Secur. 2021, 19, S50–S56. [Google Scholar] [CrossRef]
- Budak, F.; Bostan, S. The Effects of COVID-19 Pandemic on Syrian Refugees in Turkey: The Case of Kilis. Soc. Work Public Health 2020, 35, 579–589. [Google Scholar] [CrossRef]
- Cervantes, L.; Martin, M.; Frank, M.G.; Farfan, J.F.; Kearns, M.; Rubio, L.A.; Tong, A.; Matus Gonzalez, A.; Camacho, C.; Collings, A.; et al. Experiences of Latinx Individuals Hospitalized for COVID-19: A Qualitative Study. JAMA Netw. Open 2021, 4, e210684. [Google Scholar] [CrossRef]
- Deal, A.; Hayward, S.E.; Huda, M.; Knights, F.; Crawshaw, A.F.; Carter, J.; Hassan, O.B.; Farah, Y.; Ciftci, Y.; Rowland-Pomp, M.; et al. Strategies and action points to ensure equitable uptake of COVID-19 vaccinations: A national qualitative interview study to explore the views of undocumented migrants, asylum seekers, and refugees. J. Migr. Health 2021, 4, 100050. [Google Scholar] [CrossRef]
- Devillanova, C.; Colombo, C.; Garofolo, P.; Spada, A. Health care for undocumented immigrants during the early phase of the COVID-19 pandemic in Lombardy, Italy. Eur. J. Public Health 2020, 30, 1186–1188. [Google Scholar] [CrossRef] [PubMed]
- Fiorini, G.; Rigamonti, A.E.; Galanopoulos, C.; Adamoli, M.; Ciriaco, E.; Franchi, M.; Genovese, E.; Corrao, G.; Cella, S.G. Undocumented migrants during the COVID-19 pandemic: Socio-economic determinants, clinical features and pharmacological treatment. J. Public Health Res. 2020, 9, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Gosselin, A.; Melchior, M.; Carillon, S.; Gubert, F.; Ridde, V.; Kohou, V.; Zoumenou, I.; Senne, J.-N.; du Loû, A.D. Deterioration of mental health and insufficient COVID-19 information among disadvantaged immigrants in the greater Paris area. J. Psychosom. Res. 2021, 146, 1. [Google Scholar] [CrossRef] [PubMed]
- Hajjar, M.S.; Abu-Sittah, G.S. The multidimensional burden of COVID-19 on Syrian refugees in Lebanon. J. Glob. Health 2021, 11, 05003. [Google Scholar] [CrossRef] [PubMed]
- Hamadneh, S.; Hamadneh, J.; Amarin, Z.; Kassab, M.; Obeidat, R.; Rawashdeh, H. Knowledge and attitudes regarding COVID-19 among Syrian refugee women in Jordan. Int. J. Clin. Pract. 2021, 75, e14021. [Google Scholar] [CrossRef] [PubMed]
- Karajerjian, S. ‘Mama take us to a country where there is no war’: COVID-19 and mental health challenges for Syrian refugee women in Lebanon. Gend. Dev. 2021, 29, 95–109. [Google Scholar] [CrossRef]
- Kondilis, E.; Papamichail, D.; McCann, S.; Carruthers, E.; Veizis, A.; Orcutt, M.; Hargreaves, S. The impact of the COVID-19 pandemic on refugees and asylum seekers in Greece: A retrospective analysis of national surveillance data from 2020. EClin. Med. 2021, 37, 100958. [Google Scholar] [CrossRef]
- Longchamps, C.; Ducarroz, S.; Crouzet, L.; Vignier, N.; Pourtau, L.; Allaire, C.; Colleville, A.C.; El Aarbaoui, T.; Melchior, M.; Echo Study, G. COVID-19 vaccine hesitancy among persons living in homeless shelters in France. Vaccine 2021, 39, 3315–3318. [Google Scholar] [CrossRef]
- MacCarthy, S.; Izenberg, M.; Barreras, J.L.; Brooks, R.A.; Gonzalez, A.; Linnemayr, S. Rapid mixed-methods assessment of COVID-19 impact on Latinx sexual minority men and Latinx transgender women. PLoS ONE 2020, 15, e0244421. [Google Scholar] [CrossRef]
- Martuscelli, P.N. How are refugees affected by Brazilian responses to COVID-19? Rev. Adm. Publica 2020, 54, 1446–1457. [Google Scholar] [CrossRef]
- Martuscelli, P.N. How Are Forcibly Displaced People Affected by the COVID-19 Pandemic Outbreak? Evidence From Brazil. Am. Behav. Sci. 2021, 65, 1342–1364. [Google Scholar] [CrossRef]
- Quandt, S.A.; LaMonto, N.J.; Mora, D.C.; Talton, J.W.; Laurienti, P.J.; Arcury, T.A. COVID-19 Pandemic among Latinx Farmworker and Nonfarmworker Families in North Carolina: Knowledge, Risk Perceptions, and Preventive Behaviors. Int. J. Environ. Res. Public Health 2020, 17, 5786. [Google Scholar] [CrossRef] [PubMed]
- Quandt, S.A.; LaMonto, N.J.; Mora, D.C.; Talton, J.W.; Laurienti, P.J.; Arcury, T.A. COVID-19 Pandemic Among Immigrant Latinx Farmworker and Non-farmworker Families: A Rural–Urban Comparison of Economic, Educational, Healthcare, and Immigration Concerns. New Solut. 2021, 31, 30–47. [Google Scholar] [CrossRef] [PubMed]
- Redditt, V.; Wright, V.; Rashid, M.; Male, R.; Bogoch, I. Outbreak of SARS-CoV-2 infection at a large refugee shelter in Toronto, April 2020: A clinical and epidemiologic descriptive analysis. CMAJ Open 2020, 8, E819–E824. [Google Scholar] [CrossRef]
- Reynolds, C.W.; Ramanathan, V.; Lorenzana, E.; Das, P.J.; Sagal, K.M.; Lozada-Soto, K.M.; Deda, L.C.; Haque, A.S.; Schmitzberger, F.F.; Quiroga, G.; et al. Challenges and Effects of the COVID-19 Pandemic on Asylum Seeker Health at the US-Mexico Border. Health Equity 2021, 5, 169–180. [Google Scholar] [CrossRef]
- Sabri, B.; Hartley, M.; Saha, J.; Murray, S.; Glass, N.; Campbell, J.C. Effect of COVID-19 pandemic on women’s health and safety: A study of immigrant survivors of intimate partner violence. Health Care Women Int. 2020, 41, 1294–1312. [Google Scholar] [CrossRef]
- Serafini, R.A.; Powell, S.K.; Frere, J.J.; Saali, A.; Krystal, H.L.; Kumar, V.; Yashaswini, C.; Hernandez, J.; Moody, K.; Aronson, A.; et al. Psychological distress in the face of a pandemic: An observational study characterizing the impact of COVID-19 on immigrant outpatient mental health. Psychiatry Res. 2021, 295, 113595. [Google Scholar] [CrossRef]
- Terp, S.; Ahmed, S.; Burner, E.; Ross, M.; Grassini, M.; Fischer, B.; Parmar, P. Deaths in Immigration and Customs Enforcement (ICE) detention: FY2018-2020. Aims Public Health 2021, 8, 81–89. [Google Scholar] [CrossRef]
- Turunen, T.; Kontunen, K.; Sugulle, K.; Hieta, P.; Snellman, O.; Hussein, I.; Dub, T.; Melin, M.; Haveri, A.; Ekström, N.; et al. COVID-19 outbreak at a reception centre for asylum seekers in Espoo, Finland. J. Migr. Health 2021, 3, 100043. [Google Scholar] [CrossRef]
- Mistry, S.K.; Ali, A.R.M.M.; Yadav, U.N.; Ghimire, S.; Hossain, M.B.; Saha, M.; Reza, S.; Bakshi, P.; Bhuiyan, A.T.M.R.H.; Harris, M. Misconceptions about COVID-19 among older Rohingya (forcefully displaced Myanmar nationals) adults in Bangladesh: Findings from a cross-sectional study. BMJ OPEN 2021, 11, e050427. [Google Scholar] [CrossRef]
- Han, Q.; Zheng, B.; Cristea, M.; Agostini, M.; Bélanger, J.J.; Gützkow, B.; Kreienkamp, J.; Leander, N.P. Trust in government regarding COVID-19 and its associations with preventive health behaviour and prosocial behaviour during the pandemic: A cross-sectional and longitudinal study. Psychol. Med. 2021, 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hwang, T.-J.; Rabheru, K.; Peisah, C.; Reichman, W.; Ikeda, M. Loneliness and social isolation during the COVID-19 pandemic. Int. Psychogeriatr. 2020, 32, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Boswell, C. “We Also Want to be Safe”: Undocumented Migrants Facing COVID in a Hostile Environment; Joint Council for the Welfare of Immigrants: London, UK, 2022. [Google Scholar]
- Betts, A.; Easton-Calabria, E.; Pincock, K. Localising Public Health: Refugee-led organisations as first and last responders in COVID-19. World Dev. 2021, 139, 105311. [Google Scholar] [CrossRef] [PubMed]
| COVID-19 | (TITLE-ABS-KEY (“2019 novel coronavirus disease” OR “ COVID-19 virus disease” OR “COVID 19” OR “ COVID-19 pandemic” OR “SARS-CoV-2 infection” OR “nCoV” OR “2019-nCoV disease” OR “2019-nCoV” OR “Novel corona” OR “novel-Covid” OR “ COVID-19” OR “2019 novel coronavirus infection” OR “ COVID-19 infection” OR “2019-nCoV infection” OR “coronavirus disease 2019” OR “coronavirus disease-19” OR “Coronavirus disease 2019” OR “ COVID-19 virus infection” OR “Covid” OR “covid-19” OR “COVID19” OR “Covid-2019” OR “Covid 2019” OR “covid-2019” OR corona OR “corona virus” OR Sars-Cov-2) |
| Population | AND TITLE-ABS-KEY (refugee OR “asylum seeker” OR “asyl*” OR (displaced AND (person* OR people)) OR “migra*” OR “forced migra*” OR migration OR immigra* OR “human migration” OR stateless OR “state-less” OR “irregular migra*” OR “regular migra*” OR “undocumented migra*” OR “internally displaced” OR “detainees” OR “residence status” OR “foreign-born” OR “displaced person” OR “noncitizen” OR “outsider” OR “newcomer” OR “newly arrived” OR “new arrival” OR “recent entrant” OR “non national” OR “non-national” OR “transient” OR “minorities” OR “ethnic”)) |
| Limits | AND (LIMIT-TO (PUBYEAR, 2021) OR LIMIT-TO (PUBYEAR, 2021) OR LIMIT-TO (PUBYEAR, 2020) OR LIMIT-TO (PUBYEAR, 2019)) AND (LIMIT-TO (DOCTYPE, “ar”)) AND (LIMIT-TO (LANGUAGE, “English”)) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mengesha, Z.; Alloun, E.; Weber, D.; Smith, M.; Harris, P. “Lived the Pandemic Twice”: A Scoping Review of the Unequal Impact of the COVID-19 Pandemic on Asylum Seekers and Undocumented Migrants. Int. J. Environ. Res. Public Health 2022, 19, 6624. https://doi.org/10.3390/ijerph19116624
Mengesha Z, Alloun E, Weber D, Smith M, Harris P. “Lived the Pandemic Twice”: A Scoping Review of the Unequal Impact of the COVID-19 Pandemic on Asylum Seekers and Undocumented Migrants. International Journal of Environmental Research and Public Health. 2022; 19(11):6624. https://doi.org/10.3390/ijerph19116624
Chicago/Turabian StyleMengesha, Zelalem, Esther Alloun, Danielle Weber, Mitchell Smith, and Patrick Harris. 2022. "“Lived the Pandemic Twice”: A Scoping Review of the Unequal Impact of the COVID-19 Pandemic on Asylum Seekers and Undocumented Migrants" International Journal of Environmental Research and Public Health 19, no. 11: 6624. https://doi.org/10.3390/ijerph19116624
APA StyleMengesha, Z., Alloun, E., Weber, D., Smith, M., & Harris, P. (2022). “Lived the Pandemic Twice”: A Scoping Review of the Unequal Impact of the COVID-19 Pandemic on Asylum Seekers and Undocumented Migrants. International Journal of Environmental Research and Public Health, 19(11), 6624. https://doi.org/10.3390/ijerph19116624







