A Comparison of Three Measures to Identify Postnatal Anxiety: Analysis of the 2020 National Maternity Survey in England
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting and Participants
2.2. Anxiety Measures
2.3. Sociodemographic, Clinical and Psychological Variables
2.4. Statistical Analysis
3. Results
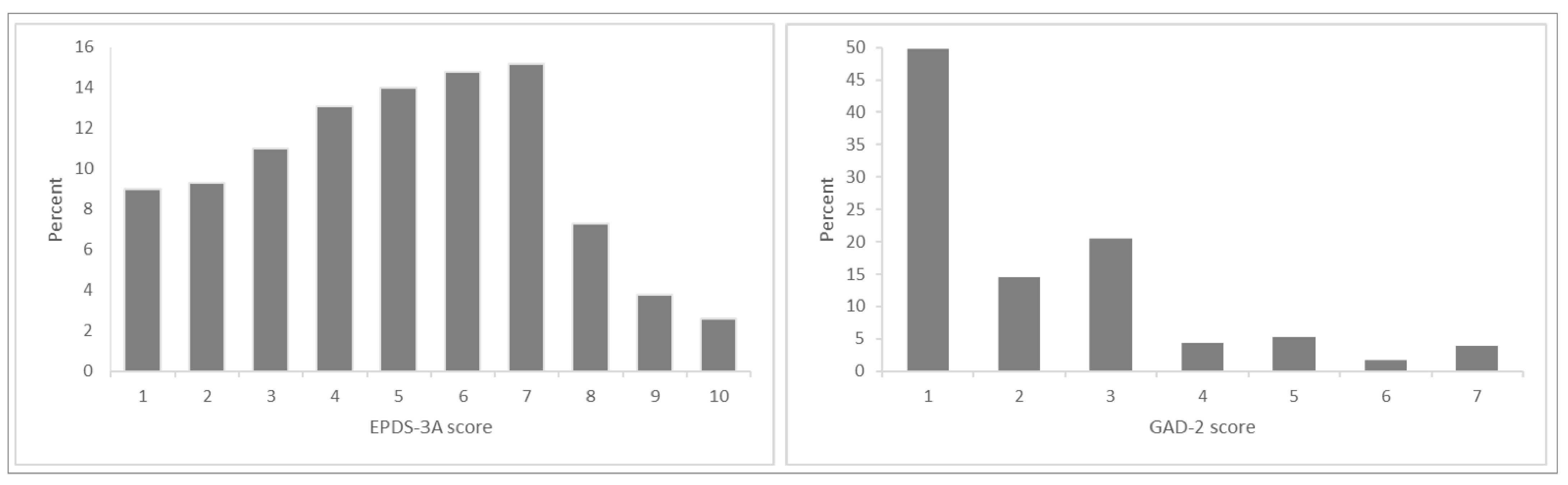
3.1. Prevalence of Anxiety Symptoms
3.2. Agreement between Anxiety Measures
3.3. Characteristics of Women with Anxiety
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Howard, L.M.; Molyneaux, E.; Dennis, C.L.; Rochat, T.; Stein, A.; Milgrom, J. Non-psychotic mental disorders in the perinatal period. Lancet 2014, 384, 1775–1788. [Google Scholar] [CrossRef]
- Harrison, S.; Alderdice, F. Challenges of defining and measuring perinatal anxiety. J. Reprod. Infant. Psychol. 2020, 38, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Dennis, C.-L.; Falah-Hassani, K.; Shiri, R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Fawcett, E.J.; Fairbrother, N.; Cox, M.L.; White, I.R.; Fawcett, J.M. The Prevalence of Anxiety Disorders During Pregnancy and the Postpartum Period: A Multivariate Bayesian Meta-Analysis. J. Clin. Psychiatry 2019, 80, 1181. [Google Scholar] [CrossRef]
- Nielsen-Scott, M.; Fellmeth, G.; Opondo, C.; Alderdice, F. Prevalence of perinatal anxiety in low- and middle-income countries: A systematic review and meta-analysis. J. Affect. Disord. 2022, 306, 71–79. [Google Scholar] [CrossRef]
- Centre for Mental Health and London School of Economics. The Costs of Perinatal Mental Health Problems; Centre for Mental Health: London, UK, 2014; Available online: http://eprints.lse.ac.uk/59885/1/__lse.ac.uk_storage_LIBRARY_Secondary_libfile_shared_repository_Content_Bauer%2C%20M_Bauer_Costs_perinatal_%20mental_2014_Bauer_Costs_perinatal_mental_2014_author.pdf (accessed on 27 May 2022).
- Gelaye, B.; Rondon, M.B.; Araya, R.; Williams, M.A. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry 2016, 3, 973–982. [Google Scholar] [CrossRef] [Green Version]
- Abel, K.M.; Hope, H.; Swift, E.; Parisi, R.; Ashcroft, D.; Kosidou, K.; Osam, C.S.; Dalman, C.; Pierce, M. Prevalence of maternal mental illness among children and adolescents in the UK between 2005 and 2017: A national retrospective cohort analysis. Lancet Public Health 2019, 4, e291–e300. [Google Scholar] [CrossRef] [Green Version]
- O’Hara, M.W.; Wisner, K. Perinatal mental illness: Definition, description and aetiology. Best Pr. Res. Clin. Obstet. Gynaecol. 2013, 28, 3–12. [Google Scholar] [CrossRef]
- Smith, M.S.; Cairns, L.; Pullen, L.S.W.; Opondo, C.; Fellmeth, G.; Alderdice, F. Validated tools to identify common mental disorders in the perinatal period: A systematic review of systematic reviews. J. Affect. Disord. 2021, 298, 634–643. [Google Scholar] [CrossRef]
- NICE (National Institute for Health and Care Excellence). Antenatal and postnatal mental health: Clinical management and service guidance (CG192); NICE: London, UK, 2014. [Google Scholar]
- Silverwood, V.; Nash, A.; Chew-Graham, C.A.; Walsh-House, J.; Sumathipala, A.; Bartlam, B.; Kingstone, T. Healthcare professionals’ perspectives on identifying and managing perinatal anxiety: A qualitative study. Br. J. Gen. Pract. 2019, 69, e768–e776. [Google Scholar] [CrossRef]
- Downe, S.M.; Butler, E.; Hinder, S. Screening tools for depressed mood after childbirth in UK-based South Asian women: A systematic review. J. Adv. Nurs. 2007, 57, 565–583. [Google Scholar] [CrossRef] [PubMed]
- Brealey, S.D.; Hewitt, C.; Green, J.M.; Morrell, J.; Gilbody, S. Screening for postnatal depression—Is it acceptable to women and healthcare professionals? A systematic review and meta-synthesis. J. Reprod. Infant Psychol. 2010, 28, 328–344. [Google Scholar] [CrossRef]
- Fellmeth, G.; Harrison, S.; McNeill, J.; Lynn, F.; Redshaw, M.; Alderdice, F. Identifying postnatal anxiety: Comparison of self-identified and self-reported anxiety using the Edinburgh Postnatal Depression Scale. BMC Pregnancy Childbirth 2022, 22, 180. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.; Alderdice, F.; McLeish, J.; Quigley, M.A. You and Your Baby: A national survey of health and care during the 2020 Covid-19 pandemic. In National Perinatal Epidemiology Unit; University of Oxford: Oxford, UK, 2021. [Google Scholar]
- Dillman, D.A. Mail and internet surveys. In the Tailored Design Method, 2nd ed.; John Wiley & Sons: Hoboken, NJ, USA, 2007. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [Green Version]
- Swalm, D.; Brooks, J.; Doherty, D.; Nathan, E.; Jacques, A. Using the Edinburgh postnatal depression scale to screen for perinatal anxiety. Arch. Women’s Ment. Health 2010, 13, 515–522. [Google Scholar] [CrossRef]
- Matthey, S.; Fisher, J.; Rowe, H. Using the Edinburgh postnatal depression scale to screen for anxiety disorders: Conceptual and methodological considerations. J. Affect. Disord. 2013, 146, 224–230. [Google Scholar] [CrossRef]
- Bowen, A.; Bowen, R.; Maslany, G.; Muhajarine, N. Anxiety in a Socially High-Risk Sample of Pregnant Women in Canada. Can. J. Psychiatry 2008, 53, 435–440. [Google Scholar] [CrossRef] [Green Version]
- Department for Communities and Local Government. The English Index of Multiple Deprivation (IMD) 2015–Guidance; Department for Communities and Local Government: London, UK, 2015. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/464430/English_Index_of_Multiple_Deprivation_2015_-_Guidance.pdf (accessed on 27 May 2022).
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Bhat, A.; Nanda, A.; Murphy, L.; Ball, A.L.; Fortney, J.; Katon, J. A systematic review of screening for perinatal depression and anxiety in community-based settings. Arch. Women’s Ment. Health 2021, 25, 33–49. [Google Scholar] [CrossRef] [PubMed]
- Fellmeth, G.; Fazel, M.; Plugge, E. Migration and perinatal mental health in women from low- and middle-income countries: A systematic review and meta-analysis. Bjog 2017, 124, 742–752. [Google Scholar] [CrossRef]
- Gennaro, S.; O’Connor, C.; McKay, E.A.; Gibeau, A.; Aviles, M.; Hoying, J.; Melnyk, B.M. Perinatal Anxiety and Depression in Minority Women. MCN: Am. J. Matern. Nurs. 2020, 45, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Sidebottom, A.; Vacquier, M.; LaRusso, E.; Erickson, D.; Hardeman, R. Perinatal depression screening practices in a large health system: Identifying current state and assessing opportunities to provide more equitable care. Arch. Women’s Ment. Health 2020, 24, 133–144. [Google Scholar] [CrossRef]
- Watson, H.; Harrop, D.; Walton, E.; Young, A.; Soltani, H. A systematic review of ethnic minority women’s experiences of perinatal mental health conditions and services in Europe. PLoS ONE 2019, 14, e0210587. [Google Scholar] [CrossRef]
- Button, S.; Thornton, A.; Lee, S.; Shakespeare, J.; Ayers, S. Seeking help for perinatal psychological distress: A meta-synthesis of women’s experiences. Br. J. Gen. Pract. 2017, 67, e692–e699. [Google Scholar] [CrossRef] [Green Version]
- Harrison, S.; Alderdice, F.; Henderson, J.; Redshaw, M.; Quigley, M.A. Trends in response rates and respondent characteristics in five National Maternity Surveys in England during 1995–2018. Arch. Public Health 2020, 78, 46. [Google Scholar] [CrossRef]
- Galea, S.; Tracy, M. Participation rates in epidemiologic studies. Ann. Epidemiol. 2007, 17, 643–653. [Google Scholar] [CrossRef]
- Harrison, S.; Henderson, J.; Alderdice, F.; Quigley, M.A. Methods to increase response rates to a population-based maternity survey: A comparison of two pilot studies. BMC Med Res. Methodol. 2019, 19, 65. [Google Scholar] [CrossRef]


| Measure | n | % |
|---|---|---|
| Single measure | ||
| Self-identified anxiety | 786 | 17.1 |
| GAD-2 score ≥3 | 645 | 15.0 |
| EPDS-3A score ≥6 | 1295 | 28.8 |
| Anxiety on at least one measure | 1609 | 36.0 |
| Multiple measures | 382 | 8.5 |
| Self-identified anxiety and GAD-2 score ≥3 | 382 | 8.5 |
| Self-identified anxiety and EPDS-3A score ≥6 | 558 | 12.1 |
| GAD-2 score ≥3 and EPDS-3A score ≥6 | 511 | 11.6 |
| Anxiety on all three measures | 334 | 7.3 |
| No anxiety on any measure | 2971 | 65.9 |
| GAD-2 | Concordance % (95% CI) [Kappa] | |||
|---|---|---|---|---|
| Anxiety | No Anxiety | |||
| Self- identified | Anxiety | 8.5% (382) | 8.6% (404) | 85.2% (84.1–86.2) [0.439] |
| No anxiety | 6.5% (263) | 76.4% (3459) | ||
| EPDS-3A | Concordance % (95% CI) [Kappa] | |||
|---|---|---|---|---|
| Anxiety | No Anxiety | |||
| Self- identified | Anxiety | 12.1% (558) | 5.0% (228) | 78.6% (77.4–79.8) [0.399] |
| No anxiety | 16.7% (737) | 66.2% (2985) | ||
| EPDS-3A | Concordance % (95% CI) [Kappa] | |||
|---|---|---|---|---|
| Anxiety | No Anxiety | |||
| GAD-2 | Anxiety | 11.6% (511) | 3.4% (134) | 79.6% (78.4–80.1) [0.415] |
| No anxiety | 17.2% (784) | 67.8% (3079) | ||
| Self-Identified Anxiety (6 m) | EPDS-3A | GAD-2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n (%) | uOR (95% CI) | aOR (95% CI) | n (%) | uOR (95% CI) | aOR (95% CI) | n (%) | uOR (95% CI) | aOR (95% CI) | |
| Age | |||||||||
| Under 25 years | 78 (23.5) | 1.52 (1.12–2.07) | 1.29 (0.91–1.84) | 123 (39.4) | 1.63 (1.24–2.14) | 1.32 (0.96–1.82) | 75 (22.5) | 1.71 (1.25–2.34) | 1.23 (0.85–1.79) |
| 25–34 years | 478 (16.8) | Ref | Ref | 800 (28.6) | Ref | Ref | 380 (14.5) | Ref | Ref |
| 35 years and over | 226 (15.1) | 0.89 (0.73–1.07) | 0.89 (0.72–1.09) | 363 (24.9) | 0.83 (0.70–0.98) | 0.80 (0.67–0.96) | 183 (12.7) | 0.85 (0.69–1.05) | 0.88 (0.70–1.10) |
| Education | |||||||||
| Under 16 years | 94 (19.4) | 1.26 (0.95–1.67) | 0.83 (0.61–1.15) | 164 (33.2) | 1.41 (1.11–1.79) | 1.05 (0.80–1.37) | 94 (19.1) | 1.57 (1.18–2.09) | 1.06 (0.76–0.47) |
| 17–18 years | 213 (18.1) | 1.16 (0.94–1.42) | 0.86 (0.68–1.09) | 370 (32.2) | 1.34 (1.13–1.59) | 1.07 (0.88–1.30) | 188 (16.7) | 1.33 (1.07–1.66) | 0.99 (0.76–1.28) |
| 19 years and over | 473 (16.1) | Ref | Ref | 748 (26.2) | Ref | Ref | 354 (13.1) | Ref | Ref |
| Ethnicity | |||||||||
| White | 726 (19.3) | Ref | Ref | 1130 (30.1) | Ref | Ref | 577 (16.0) | Ref | Ref |
| Black or minority ethnic | 54 (8.0) | 0.36 (0.26–0.51) | 0.44 (0.30–0.64) | 148 (23.4) | 0.71 (0.56–0.90) | 0.93 (0.71–1.21) | 60 (10.8) | 0.64 (0.46–0.88) | 0.86 (0.59–1.25) |
| Country of birth | |||||||||
| UK | 681 (20.0) | Ref | Ref | 1097 (31.7) | Ref | Ref | 557 (17.4) | Ref | Ref |
| Outside of UK | 102 (10.7) | 0.48 (0.37–0.62) | 0.79 (0.59–1.04) | 191 (22.5) | 0.62 (0.51–0.76) | 0.81 (0.64–1.01) | 83 (9.6) | 0.50 (0.38–0.66) | 0.66 (0.49–0.89) |
| IMD | |||||||||
| 1 (most deprived) | 120 (17.2) | 1.05 (0.79–1.40) | 1.06 (0.77–1.46) | 209 (30.9) | 1.14 (0.90–1.45) | 1.05 (0.81–1.36) | 123 (18.2) | 1.45 (1.08–1.95) | 1.34 (0.97–1.87) |
| 2 | 152 (17.4) | 1.06 (0.82–1.38) | 1.20 (0.91–1.60) | 239 (28.7) | 1.03 (0.82–1.29) | 1.00 (0.78–1.29) | 131 (15.6) | 1.21 (0.91–1.60) | 1.22 (0.90–1.66) |
| 3 | 166 (17.2) | 1.05 (0.81–1.36) | 1.04 (0.79–1.36) | 266 (27.6) | 0.98 (0.79–1.21) | 0.94 (0.75–1.18) | 137 (14.1) | 1.08 (0.82–1.43) | 1.05 (0.78–1.41) |
| 4 | 184 (17.0) | 1.04 (0.81–1.33) | 1.04 (0.79–1.35) | 301 (28.2) | 1.01 (0.82–1.23) | 1.00 (0.80–1.25) | 125 (12.4) | 0.93 (0.70–1.23) | 0.91 (0.68–1.23) |
| 5 (least deprived) | 164 (16.5) | Ref | Ref | 280 (28.1) | Ref | Ref | 129 (13.2) | Ref | Ref |
| Planned pregnancy | |||||||||
| Planned | 608 (16.1) | Ref | Ref | 987 (26.7) | Ref | Ref | 471 (13.2) | Ref | Ref |
| Unplanned | 175 (20.4) | 1.33 (1.08–1.66) | 1.05 (0.79–1.40) | 299 (35.1) | 1.49 (1.24–1.79) | 1.12 (0.89–1.41) | 168 (20.1) | 1.65 (1.32–2.06) | 1.01 (0.76–1.36) |
| Reaction to pregnancy | |||||||||
| Pleased or happy | 610 (16.0) | Ref | Ref | 993 (26.9) | Ref | Ref | 461 (12.7) | Ref | Ref |
| Mixed or unhappy | 164 (22.0) | 1.48 (1.18–1.85) | 1.13 (0.85–1.50) | 275 (36.3) | 1.55 (1.28–1.88) | 1.22 (0.96–1.55) | 173 (23.6) | 2.12 (1.69–2.65) | 1.71 (1.30–2.25) |
| Multiple birth | |||||||||
| Singleton | 780 (17.3) | Ref | Ref | 1273 (28.8) | Ref | Ref | 638 (15.1) | Ref | Ref |
| Twin | 6 (9.3) | 0.49 (0.18–1.35) | 0.56 (0.18–1.78) | 15 (26.2) | 0.88 (0.41–1.85) | 0.89 (0.39–2.01) | 5 (9.1) | 0.56 (0.19–1.68) | 0.40 (0.10–1.62) |
| Antenatal anxiety | |||||||||
| No | 386 (10.4) | Ref | Ref | 770 (22.0) | Ref | Ref | 316 (9.5) | Ref | Ref |
| Yes | 398 (40.9) | 5.93 (4.89–7.18) | 5.35 (4.37–6.55) | 517 (53.2) | 4.03 (3.39–4.80) | 3.64 (3.03–4.36) | 327 (34.5) | 5.00 (4.08–6.13) | 4.16 (3.35–5.15) |
| Chronic health conditions | |||||||||
| No | 677 (16.3) | Ref | Ref | 1097 (27.2) | Ref | Ref | 544 (14.1) | Ref | Ref |
| Yes | 107 (23.3) | 1.56 (1.19–2.05) | 1.16 (0.85–1.59) | 189 (41.0) | 1.87 (1.48–2.35) | 1.49 (1.16–1.93) | 99 (22.1) | 1.73 (1.31–2.27) | 1.21 (0.89–1.65) |
| NICU admission | |||||||||
| No | 688 (18.7) | Ref | Ref | 1148 (28.7) | Ref | Ref | 577 (15.2) | Ref | Ref |
| Yes | 95 (16.9) | 1.13 (0.85–1.51) | 1.01 (0.74–1.39) | 141 (29.6) | 1.05 (0.81–1.36) | 0.94 (0.71–1.26) | 67 (15.0) | 1.01 (0.72–1.41) | 0.86 (0.61–1.20) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fellmeth, G.; Harrison, S.; Quigley, M.A.; Alderdice, F. A Comparison of Three Measures to Identify Postnatal Anxiety: Analysis of the 2020 National Maternity Survey in England. Int. J. Environ. Res. Public Health 2022, 19, 6578. https://doi.org/10.3390/ijerph19116578
Fellmeth G, Harrison S, Quigley MA, Alderdice F. A Comparison of Three Measures to Identify Postnatal Anxiety: Analysis of the 2020 National Maternity Survey in England. International Journal of Environmental Research and Public Health. 2022; 19(11):6578. https://doi.org/10.3390/ijerph19116578
Chicago/Turabian StyleFellmeth, Gracia, Siân Harrison, Maria A. Quigley, and Fiona Alderdice. 2022. "A Comparison of Three Measures to Identify Postnatal Anxiety: Analysis of the 2020 National Maternity Survey in England" International Journal of Environmental Research and Public Health 19, no. 11: 6578. https://doi.org/10.3390/ijerph19116578
APA StyleFellmeth, G., Harrison, S., Quigley, M. A., & Alderdice, F. (2022). A Comparison of Three Measures to Identify Postnatal Anxiety: Analysis of the 2020 National Maternity Survey in England. International Journal of Environmental Research and Public Health, 19(11), 6578. https://doi.org/10.3390/ijerph19116578





