Formative Assessment to Improve Cancer Screenings in American Indian Men: Native Patient Navigator and mHealth Texting
Abstract
1. Introduction
2. Materials and Methods
2.1. Target Population
2.2. Approval to Conduct Research
2.3. H.O.P.I. Cancer Support Services
2.4. Community Advisory Committee
2.5. Native Patient Navigator and Training
2.6. Formative Assessment
2.7. Enrollment, Consenting, and Data Collection Process
2.8. Statistical Analysis
3. Results
3.1. Evaluation of Text Messaging Use among Buddy Challenge Program Participants
3.2. Community Audience Response System (ARS)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rhoades, E.R. The health status of American Indian and Alaska Native males. Am. J. Public Health 2003, 93, 774–778. [Google Scholar] [CrossRef] [PubMed]
- Groom, A.V.; Hennessy, T.W.; Singleton, R.J.; Butler, J.C.; Holve, S.; Cheek, J.E. Pneumonia and influenza mortality among American Indian and Alaska Native people, 1990–2009. Am. J. Public Health 2014, 104, S460–S469. [Google Scholar] [CrossRef] [PubMed]
- Schieb, L.J.; Ayala, C.; Valderrama, A.L.; Veazie, M.A. Trends and disparities in stroke mortality by region for American Indians and Alaska Natives. Am. J. Public Health 2014, 104, S368–S376. [Google Scholar] [CrossRef]
- Plescia, M.; Henley, S.J.; Pate, A.; Underwood, J.M.; Rhodes, K. Lung cancer deaths among American Indians and Alaska Natives, 1990–2009. Am. J. Public Health 2014, 104, S388–S395. [Google Scholar] [CrossRef]
- Mowery, P.D.; Dube, S.R.; Thorne, S.L.; Garrett, B.E.; Homa, D.M.; Nez Henderson, P. Disparities in smoking-related mortality among American Indians/Alaska Natives. Am. J. Prev. Med. 2015, 49, 738–744. [Google Scholar] [CrossRef]
- Dankovchik, J.; Hoopes, M.J.; Warren-Mears, V.; Knaster, E. Disparities in life expectancy of Pacific Northwest American Indians and Alaska Natives: Analysis of linkage-corrected life tables. Public Health Rep. 2015, 130, 71–80. [Google Scholar] [CrossRef]
- Hutchinson, R.N.; Shin, S. Systematic review of health disparities for cardiovascular diseases and associated factors among American Indian and Alaska Native populations. PLoS ONE 2014, 9, e80973. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef]
- White, M.C.; Espey, D.K.; Swan, J.; Wiggins, C.L.; Eheman, C.; Kaur, J.S. Disparities in cancer mortality and incidence among American Indians and Alaska Natives in the United States. Am. J. Public Health 2014, 104, S377–S387. [Google Scholar] [CrossRef]
- Perdue, D.G.; Haverkamp, D.; Perkins, C.; Daley, C.M.; Provost, E. Geographic variation in colorectal cancer incidence and mortality, age of onset, and stage at diagnosis among American Indian and Alaska Native people, 1990–2009. Am. J. Public Health 2014, 104, S404–S414. [Google Scholar] [CrossRef]
- Hoffman, R.M.; Li, J.; Henderson, J.A.; Ajani, U.A.; Wiggins, C. Prostate cancer deaths and incident cases among American Indian/Alaska Native men, 1999–2009. Am. J. Public Health 2014, 104, S439–S445. [Google Scholar] [CrossRef] [PubMed]
- Emerson, M.A.; Banegas, M.P.; Chawla, N.; Achacoso, N.; Alexeeff, S.E.; Adams, A.S.; Habel, L.A. Disparities in prostate, lung, breast, and colorectal cancer survival and comorbidity status among Urban American Indians and Alaskan Natives. Cancer Res. 2017, 77, 6770–6776. [Google Scholar] [CrossRef] [PubMed]
- Jim, M.A.; Arias, E.; Seneca, D.S.; Hoopes, M.J.; Jim, C.C.; Johnson, N.J.; Wiggins, C.L. Racial misclassification of American Indians and Alaska Natives by Indian Health Service Contract Health Service Delivery Area. Am. J. Public Health 2014, 104, S295–S302. [Google Scholar] [CrossRef] [PubMed]
- Creswell, P.D.; Strickland, R.; Stephenson, L.; Pierce-Hudson, K.; Matloub, J.; Waukau, J. Look local: The value of cancer surveillance and reporting by American Indian clinics. Prev. Chronic Dis. 2013, 10, E197. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tilburt, J.C.; Koller, K.; Tiesinga, J.J.; Wilson, R.T.; Trinh, A.C.; Hill, K.; Hall, I.J.; Smith, J.L.; Ekwueme, D.U.; Petersen, W.O. Patterns of clinical response to PSA elevation in American Indian/Alaska Native men: A multi-center pilot study. J. Health Care Poor Underserved 2013, 24, 1676–1685. [Google Scholar] [CrossRef]
- Batai, K.; Gachupin, F.C.; Estrada, A.L.; Garcia, D.O.; Gomez, J.; Kittles, R.A. Patterns of cancer related health disparities in Arizona. Cancer Health Disparities 2019, 3, e1–e20. [Google Scholar]
- Arizona Cancer Registry. Cancer in Arizona: Cancer Incidence and Mortality 2008–2009; Arizona Department of Health Services: Phoenix, AZ, USA, 2013. [Google Scholar]
- Lantz, P.M.; Mullen, J. The National Breast and Cervical Cancer Early Detection Program: 25 Years of public health service to low-income women. Cancer Causes Control 2015, 26, 653–656. [Google Scholar] [CrossRef]
- Fedewa, S.A.; Sauer, A.G.; Siegel, R.L.; Jemal, A. Prevalence of major risk factors and use of screening tests for cancer in the United States. Cancer Epidemiol. Biomark. Prev. 2015, 24, 637–652. [Google Scholar] [CrossRef]
- Steele, C.B.; Cardinez, C.J.; Richardson, L.C.; Tom-Orme, L.; Shaw, K.M. Surveillance for health behaviors of American Indians and Alaska Natives—Findings from the behavioral risk factor surveillance system, 2000–2006. Cancer 2008, 113, 1131–1141. [Google Scholar] [CrossRef]
- Cobb, N.; Espey, D.; King, J. Health behaviors and risk factors among American Indians and Alaska Natives, 2000–2010. Am. J. Public Health 2014, 104, S481–S489. [Google Scholar] [CrossRef]
- Batai, K.; Sanderson, P.R.; Hsu, C.H.; Joshweseoma, L.; Russell, D.; Joshweseoma, L.; Ojeda, J.; Burhansstipanov, L.; Brown, S.R.; Ami, D.; et al. Factors associated with cancer screening among Hopi men. J. Cancer Educ. 2020. [Google Scholar] [CrossRef] [PubMed]
- Filippi, M.K.; James, A.S.; Brokenleg, S.; Talawyma, M.; Perdue, D.G.; Choi, W.S.; Greiner, K.A.; Daley, C.M. Views, barriers, and suggestions for colorectal cancer screening among American Indian women older than 50 years in the midwest. J. Prim. Care Community Health 2013, 4, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Daley, C.M.; James, A.S.; Filippi, M.; Weir, M.; Braiuca, S.; Kaur, B.; Choi, W.S.; Greiner, K.A. American Indian community leader and provider views of needs and barriers to colorectal cancer screening. J. Health Dispar. Res. Pract. 2012, 5, 2. [Google Scholar] [PubMed]
- James, A.S.; Filippi, M.K.; Pacheco, C.M.; Cully, L.; Perdue, D.; Choi, W.S.; Greiner, K.A.; Daley, C.M. Barriers to colorectal cancer screening among American Indian men aged 50 or older, Kansas and Missouri, 2006–2008. Prev. Chronic Dis. 2013, 10, E170. [Google Scholar] [CrossRef]
- Rogers, C.R.; Perdue, D.G.; Boucher, K.; Korous, K.M.; Brooks, E.; Petersen, E.; Inadomi, J.M.; Tuuhetaufa, F.; Levant, R.F.; Paskett, E.D. Masculinity Barriers to Ever Completing Colorectal Cancer Screening among American Indian/Alaska Native, Black, and White Men (Ages 45–75). Int. J. Environ. Res. Public Health 2022, 19, 3071. [Google Scholar] [CrossRef]
- Zuckerman, S.; Haley, J.; Roubideaux, Y.; Lillie-Blanton, M. Health service access, use, and insurance coverage among American Indians/Alaska Natives and Whites: What role does the Indian Health Service play? Am. J. Public Health 2004, 94, 53–59. [Google Scholar] [CrossRef]
- Allen, E.M.; Call, K.T.; Beebe, T.J.; McAlpine, D.D.; Johnson, P.J. Barriers to care and health care utilization among the publicly insured. Med. Care 2017, 55, 207–214. [Google Scholar] [CrossRef]
- Call, K.T.; McAlpine, D.D.; Johnson, P.J.; Beebe, T.J.; McRae, J.A.; Song, Y. Barriers to care among American Indians in public health care programs. Med. Care 2006, 44, 595–600. [Google Scholar] [CrossRef]
- Itty, T.L.; Hodge, F.S.; Martinez, F. Shared and unshared barriers to cancer symptom management among urban and rural American Indians. J. Rural Health 2014, 30, 206–213. [Google Scholar] [CrossRef]
- Krebs, L.U.; Burhansstipanov, L.; Watanabe-Galloway, S.; Pingatore, N.L.; Petereit, D.G.; Isham, D. Navigation as an intervention to eliminate disparities in American Indian communities. Semin. Oncol. Nurs. 2013, 29, 118–127. [Google Scholar] [CrossRef]
- Warren-Mears, V.; Dankovchik, J.; Patil, M.; Fu, R. Impact of patient navigation on cancer diagnostic resolution among Northwest Tribal communities. J. Cancer Educ. 2013, 28, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Menon, U.; Lance, P.; Szalacha, L.A.; Candito, D.; Bobyock, E.P.; Yellowhair, M.; Hatcher, J. Adaptation of colorectal cancer screening tailored navigation content for American Indian communities and early results using the intervention. Implement. Sci. Commun. 2022, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Head, K.J.; Noar, S.M.; Iannarino, N.T.; Grant Harrington, N. Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Soc. Sci. Med. 2013, 97, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Muller, C.J.; Robinson, R.F.; Smith, J.J.; Jernigan, M.A.; Hiratsuka, V.; Dillard, D.A.; Buchwald, D. Text message reminders increased colorectal cancer screening in a randomized trial with Alaska Native and American Indian people. Cancer 2017, 123, 1382–1389. [Google Scholar] [CrossRef]
- Sanderson, P.R.; Teufel-Shone, N.I.; Baldwin, J.A.; Sandoval, N.; Robinson, F. Breast cancer education for Navajo women: A pilot study evaluating a culturally relevant video. J. Cancer Educ. 2010, 25, 217–223. [Google Scholar] [CrossRef]
- Thompson, N.R.; Sloat, C.D. The use of oral literature to provide community health education on the southern northwest coast. Am. Indian Cult. Res. J. 2004, 28, 1–28. [Google Scholar] [CrossRef]
- Teague, L.S. Prehistory and the traditions of the O’odham and Hopi. KIVA 2009, 75, 239–259. [Google Scholar] [CrossRef]
- Courlander, H. Hopi Voices: Recollections, Traditions and Narratives of the Hopi Indians; University of New Mexico Press: Albuquerque, NM, USA, 1982. [Google Scholar]
- Wall, D.; Masayesva, V. People of the corn: Teachings in Hopi traditional agriculture, spirituality, and sustainability. Am. Indian Q. 2004, 28, 435–453. [Google Scholar] [CrossRef]
- Bernardini, W. Hopi Oral Tradition and the Archeology of Identity; The University of Arizona Press: Tucson, AZ, USA, 2005. [Google Scholar]
- Brown, S.R.; Joshweseoma, L.; Saboda, K.; Sanderson, P.; Ami, D.; Harris, R. Cancer screening on the Hopi reservation: A model for success in a Native American community. J. Community Health 2015, 40, 1165–1172. [Google Scholar] [CrossRef]
- Brown, S.R.; Nuno, T.; Joshweseoma, L.; Begay, R.C.; Goodluck, C.; Harris, R.B. Impact of a community-based breast cancer screening program on Hopi women. Prev. Med. 2011, 52, 390–393. [Google Scholar] [CrossRef]
- Cordova, F.M.; Harris, R.B.; Teufel-Shone, N.I.; Nisson, P.L.; Joshweseoma, L.; Brown, S.R.; Sanderson, P.R.; Ami, D.; Saboda, K.; Mastergeorge, A.M.; et al. Caregiving on the Hopi reservation: Findings from the 2012 Hopi survey of cancer and chronic disease. J. Community Health 2016, 41, 1177–1186. [Google Scholar] [CrossRef] [PubMed]
- Mayer, B.; Joshweseoma, L.; Sehongva, G. Environmental risk perceptions and community health: Arsenic, air pollution, and threats to traditional values of the Hopi Tribe. J. Community Health 2019, 44, 896–902. [Google Scholar] [CrossRef] [PubMed]
- Burhansstipanov, L.; Krebs, L.U.; Harjo, L.; Ragan, K.; Kaur, J.S.; Marsh, V.; Painter, D. Findings from American Indian Needs Assessments. J. Cancer Educ. 2018, 33, 576–582. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.; Joshweseoma, L.; Harris, R.; Sobada, K. 2012 Hopi Survey of Cancer and Chronic Disease; Report to Hopi Tribe: Kykotsmovi, AZ, USA, 2014. [Google Scholar]
- Uy, C.; Lopez, J.; Trinh-Shevrin, C.; Kwon, S.C.; Sherman, S.E.; Liang, P.S. Text messaging interventions on cancer screening rates: A systematic review. J. Med. Internet Res. 2017, 19, e296. [Google Scholar] [CrossRef]
- Jongerius, C.; Russo, S.; Mazzocco, K.; Pravettoni, G. Research-tested mobile apps for breast cancer care: Systematic review. JMIR Mhealth Uhealth 2019, 7, e10930. [Google Scholar] [CrossRef]
- U.S. Preventive Services Task Force. Screening for prostate cancer: Us preventive services task force recommendation statement. JAMA 2018, 319, 1901–1913. [Google Scholar] [CrossRef]
- Teufel-Shone, N.I.; Schwartz, A.L.; Hardy, L.J.; de Heer, H.D.; Williamson, H.J.; Dunn, D.J.; Polingyumptewa, K.; Chief, C. Supporting new community-based participatory research partnerships. Int. J. Environ. Res. Public Health 2019, 16, 44. [Google Scholar] [CrossRef]
- Chen, M.S., Jr.; Lara, P.N.; Dang, J.H.T.; Paterniti, D.A.; Kelly, K. Twenty years post-NIH Revitalization Act: Enhancing minority participation in clinical trials (EMPaCT): Laying the groundwork for improving minority clinical trial accrual. Cancer 2014, 120, 1091–1096. [Google Scholar] [CrossRef]
- Burchard, E.G.; Oh, S.S.; Foreman, M.G.; Celedón, J.C. Moving toward true inclusion of racial/ethnic minorities in federally funded studies. A key step for achieving respiratory health equality in the United States. Am. J. Respir. Crit. Care Med. 2015, 191, 514–521. [Google Scholar] [CrossRef]
- Hodge, F.S.; Weinmann, S.; Roubideaux, Y. Recruitment of American Indians and Alaska Natives Into clinical trials. Ann. Epidemiol. 2000, 10 (Suppl. S8), S41–S48. [Google Scholar] [CrossRef]
- Slattery, M.L.; Schumacher, M.C.; Lanier, A.P.; Edwards, S.; Edwards, R.; Murtaugh, M.A.; Sandidge, J.; Day, G.E.; Kaufman, D.; Kanekar, S.; et al. A prospective cohort of American Indian and Alaska Native people: Study design, methods, and implementation. Am. J. Epidemiol. 2007, 166, 606–615. [Google Scholar] [CrossRef] [PubMed]
- Best, L.G.; García-Esquinas, E.; Yeh, J.-L.; Yeh, F.; Zhang, Y.; Lee, E.T.; Howard, B.V.; Farley, J.H.; Welty, T.K.; Rhoades, D.A.; et al. Association of diabetes and cancer mortality in American Indians: The Strong Heart Study. Cancer Causes Control 2015, 26, 1551–1560. [Google Scholar] [CrossRef] [PubMed]
| Variables | n (%) |
|---|---|
| Reported Age | |
| 50–64 years | 54 (65.1%) |
| 65–80 years | 23 (27.7%) |
| 81 years or older | 2 (2.4%) |
| Missing | 4 (4.8%) |
| Highest Reported Education | |
| Junior High | 4 (4.8%) |
| High School but never completed | 2 (2.4%) |
| High school graduate/GED | 19 (22.9%) |
| Trade, technical or vocational school after High School | 30 (36.1%) |
| Some college but no degree | 23 (27.7%) |
| Bachelor degree or greater | 5 (6.0%) |
| Married | 30 (36.1%) |
| Employed full-time | 27 (32.5%) |
| Household income | |
| Less than $10,000 | 18 (21.7%) |
| $10,000–$20,000 | 9 (10.8%) |
| $20,001–$30,000 | 11 (13.3%) |
| $30,001–$40,000 | 14 (16.9%) |
| ≥$50,001 | 16 (19.3%) |
| Don’t know/Refused | 15 (18.1%) |
| Own Cell phone | 70 (84.3%) |
| Use cellular for texting | 65 (78.3%) |
| Hopi Culture | |
| Primary language at home: Hopi | 65 (78.3%) |
| Screening history | |
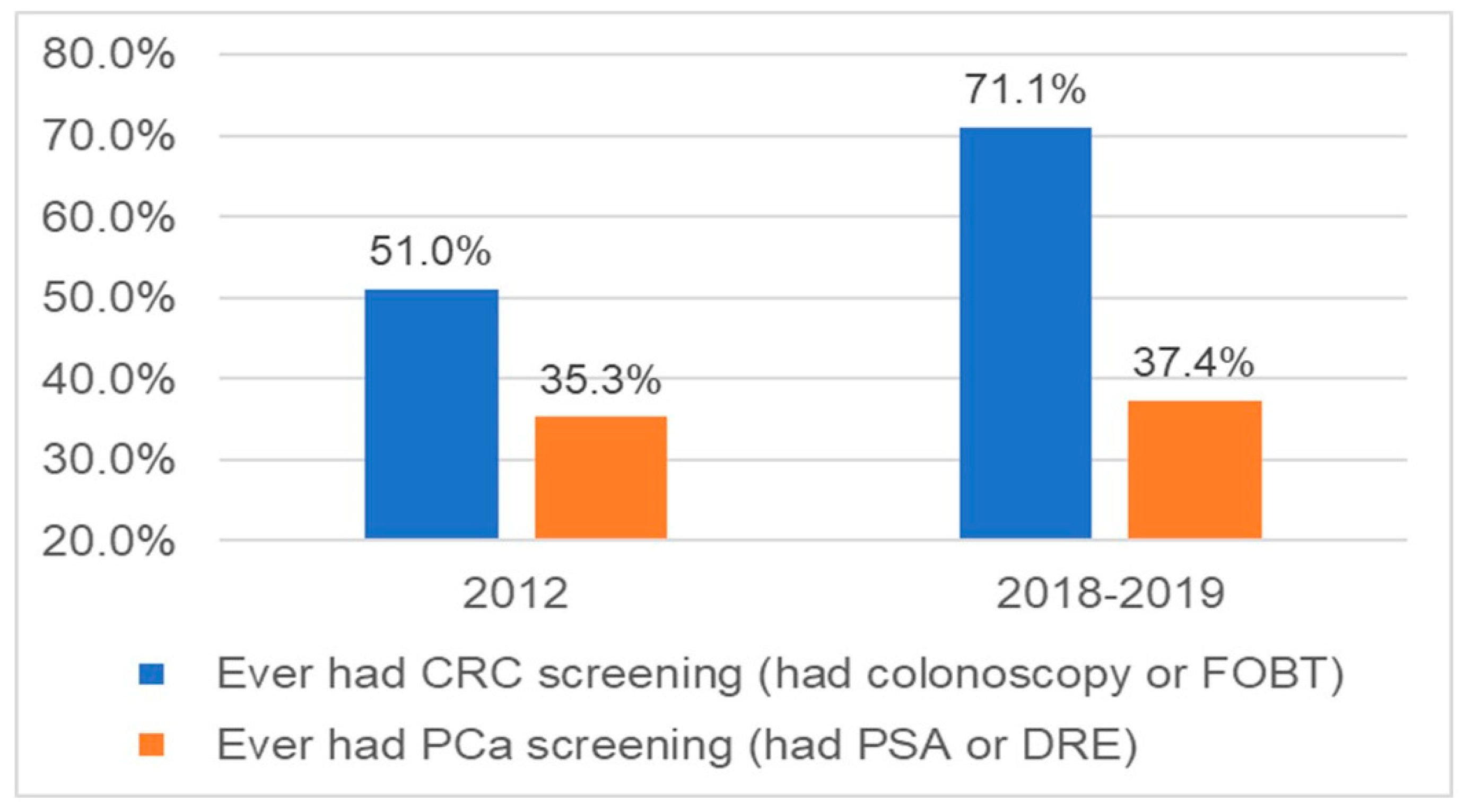
| Ever had colorectal cancer screening | 59 (71.1%) |
| Ever had prostate cancer screening | 31 (37.4%) |
| Cancer experience | |
| Has/had cancer | 6 (7.2%) |
| Family members diagnosed with cancer | 37 (44.5%) |
| Health Status | |
| Diabetes | 36 (43.4%) |
| Hypertension | 44 (53.0%) |
| High cholesterol | 25 (30.1%) |
| Thinks his health is good, very good or excellent | 59 (71.1%) |
| Hopi Health Care Center for primary care services | 36 (43.4%) |
| Medicare/Medicaid, or AHCCCs health insurance | 40 (48.2%) |
| Learn about cancer screening from | |
| Family members | 16 (19.5%) |
| Friends | 5 (6.1%) |
| Employers and coworkers | 4 (4.9%) |
| Health care providers | 11 (13.4%) |
| Community education events | 6 (7.3%) |
| H.O.P.I. Cancer Support Services staff | 28 (34.2%) |
| Media | 6 (7.3%) |
| None of the above | 6 (7.3%) |
| Last annual physical exam in 2018 | 43 (51.8%) |
| Looked for medical information in the past year using electronic devices | 27 (32.5%) |
| Made medical appointment using electronic devices in the past years | 24 (28.9%) |
| Sent/received text from health professionals | 26 (31.3%) |
| Heath wellness apps on smartphone/tablet | 16 (19.3%) |
| Received text from Hopi men’s health project | 68 (81.4%) |
| FOBT | Colonoscopy | PSA | DRE | |
|---|---|---|---|---|
| 11 (13.3%) | 51 (61.5%) | 14 (16.9%) | 18 (21.7%) | |
| Within the last year | 8 (19.5%) | 8 (28.6%) | ||
| Within the last 3 years | 13 (31.7%) | 9 (32.1%) | ||
| Within the last 5 years | 12 (29.3%) | 8 (28.6%) | ||
| Within the last 10 years | 5 (12.2%) | 2 (7.1%) | ||
| Longer than 10 years ago | 3 (7.3%) | 1 (3.6%) | ||
| Missing | 18 | 3 | ||
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age < 65 | 0.24 (0.06–0.90) | 0.03 | 0.35 (0.09–1.40) | 0.14 |
| Some college education | 1.03 (0.38–2.80) | 0.96 | ||
| Married | 2.79 (0.92–8.50) | 0.07 | ||
| Employed full-time | 1.25 (0.44–3.50) | 0.68 | ||
| Income < $40 K | 1.39 (0.53–3.69) | 0.51 | ||
| Own Cell phone | 1.68 (0.49–5.77) | 0.41 | ||
| Use cellular for texting | 0.93 (0.29–2.98) | 0.90 | ||
| Primary language at home: Hopi | 0.42 (0.11–1.61) | 0.20 | ||
| Ever had prostate screening | 6.32 (1.70–23.51) | 0.01 | 5.33 (1.38–20.59) | 0.02 |
| Cancer experience | ||||
| Has/had cancer | 2.13 (0.24–19.25) | 0.50 | ||
| Family history of cancer | 0.93 (0.36–2.42) | 0.88 | ||
| Diabetes | 1.10 (0.42–2.88) | 0.84 | ||
| Hypertension | 3.13 (1.16–8.48) | 0.02 | 2.56 (0.88–7.46) | 0.09 |
| High cholesterol | 2.76 (0.83–9.16) | 0.10 | ||
| Thinks his health is good, very good or excellent | 1.76 (0.64–4.85) | 0.27 | ||
| HHCC primary care services | 0.54 (0.21–1.41) | 0.21 | ||
| Medicare/Medicaid, or AHCCCs health insurance | 0.56 (0.22–1.47) | 0.24 | ||
| Last annual physical exam in 2018 | 1.11 (0.43–2.86) | 0.83 | ||
| Looked for medical information in the past year using electronic devices | 0.95 (0.35–2.61) | 0.92 | ||
| Made medical appointment using electronic devices in the past years | 0.57 (0.21–1.56) | 0.27 | ||
| Sent/received text from health professionals | 0.67 (0.25–1.83) | 0.44 | ||
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age < 65 | 0.42 (0.16–1.09) | 0.07 | ||
| Some college education | 0.90 (0.35–2.31) | 0.83 | ||
| Married | 0.60 (0.23–1.57) | 0.30 | ||
| Employed full-time | 1.56 (0.61–3.99) | 0.35 | ||
| Income < $40 K | 1.05 (0.41–2.65) | 0.92 | ||
| Own Cell phone | 9.00 (1.11–73.07) | 0.04 | 5.42 (0.60–3.89) | 0.13 |
| Use cellular for texting | 2.49 (0.74–8.39) | 0.14 | ||
| Primary language at home: Hopi | 0.51 (0.18–1.47) | 0.21 | ||
| Ever had CRC screening | 6.32 (1.70–23.51) | 0.01 | 5.37 (1.36–21.17) | 0.02 |
| Has/had cancer | 3.70 (0.64–21.54) | 0.15 | ||
| Family history of cancer | 1.57 (0.64–3.86) | 0.32 | ||
| Diabetes | 0.91 (0.37–2.24) | 0.84 | ||
| Hypertension | 1.71 (0.69–4.23) | 0.25 | ||
| High cholesterol | 3.07 (1.16–8.11) | 0.02 | 2.05 (0.70–6.02) | 0.19 |
| Thinks his health is good, very good or excellent | 0.77 (0.29–2.04) | 0.60 | ||
| HHCC primary care services | 2.11 (0.85–5.21) | 0.11 | ||
| Medicare/Medicaid, or AHCCCs health insurance | 0.35 (0.14–0.89) | 0.03 | 0.42 (0.15–1.19) | 0.10 |
| Last annual physical exam in 2018 | 0.99 (0.41–2.41) | 0.98 | ||
| Looked for medical information in the past year using electronic devices | 1.96 (0.77–5.02) | 0.16 | ||
| Made medical appointment using electronic devices in the past years | 2.11 (0.80–5.55) | 0.13 | ||
| Sent/received text from health professionals | 1.36 (0.53–3.51) | 0.53 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Batai, K.; Sanderson, P.R.; Joshweseoma, L.; Burhansstipanov, L.; Russell, D.; Joshweseoma, L.; Hsu, C.-H. Formative Assessment to Improve Cancer Screenings in American Indian Men: Native Patient Navigator and mHealth Texting. Int. J. Environ. Res. Public Health 2022, 19, 6546. https://doi.org/10.3390/ijerph19116546
Batai K, Sanderson PR, Joshweseoma L, Burhansstipanov L, Russell D, Joshweseoma L, Hsu C-H. Formative Assessment to Improve Cancer Screenings in American Indian Men: Native Patient Navigator and mHealth Texting. International Journal of Environmental Research and Public Health. 2022; 19(11):6546. https://doi.org/10.3390/ijerph19116546
Chicago/Turabian StyleBatai, Ken, Priscilla R. Sanderson, Lori Joshweseoma, Linda Burhansstipanov, Dana Russell, Lloyd Joshweseoma, and Chiu-Hsieh Hsu. 2022. "Formative Assessment to Improve Cancer Screenings in American Indian Men: Native Patient Navigator and mHealth Texting" International Journal of Environmental Research and Public Health 19, no. 11: 6546. https://doi.org/10.3390/ijerph19116546
APA StyleBatai, K., Sanderson, P. R., Joshweseoma, L., Burhansstipanov, L., Russell, D., Joshweseoma, L., & Hsu, C.-H. (2022). Formative Assessment to Improve Cancer Screenings in American Indian Men: Native Patient Navigator and mHealth Texting. International Journal of Environmental Research and Public Health, 19(11), 6546. https://doi.org/10.3390/ijerph19116546







