Effects of Face Masks on Physiological Parameters and Voice Production during Cycling Activity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Face Masks Selection
2.2. Participants, Test Facility, and Organization
2.3. Measurement of Vocal Parameters
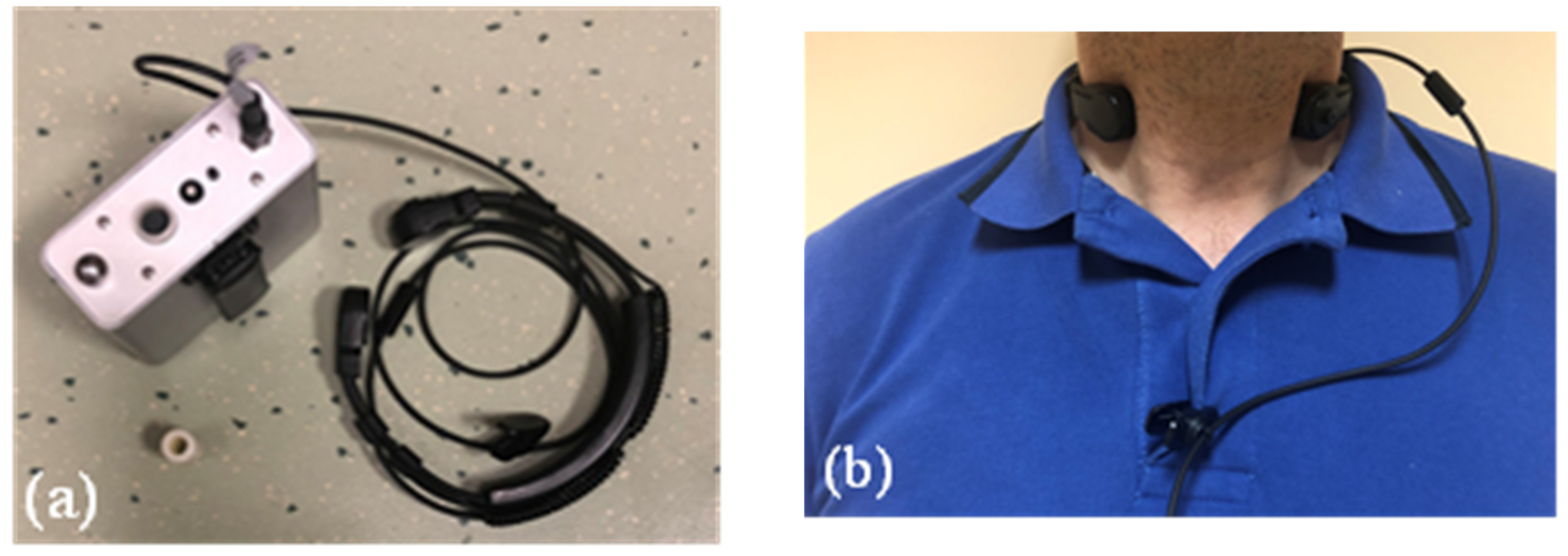
Voice Monitoring Device
2.4. Voice Monitoring Procedure
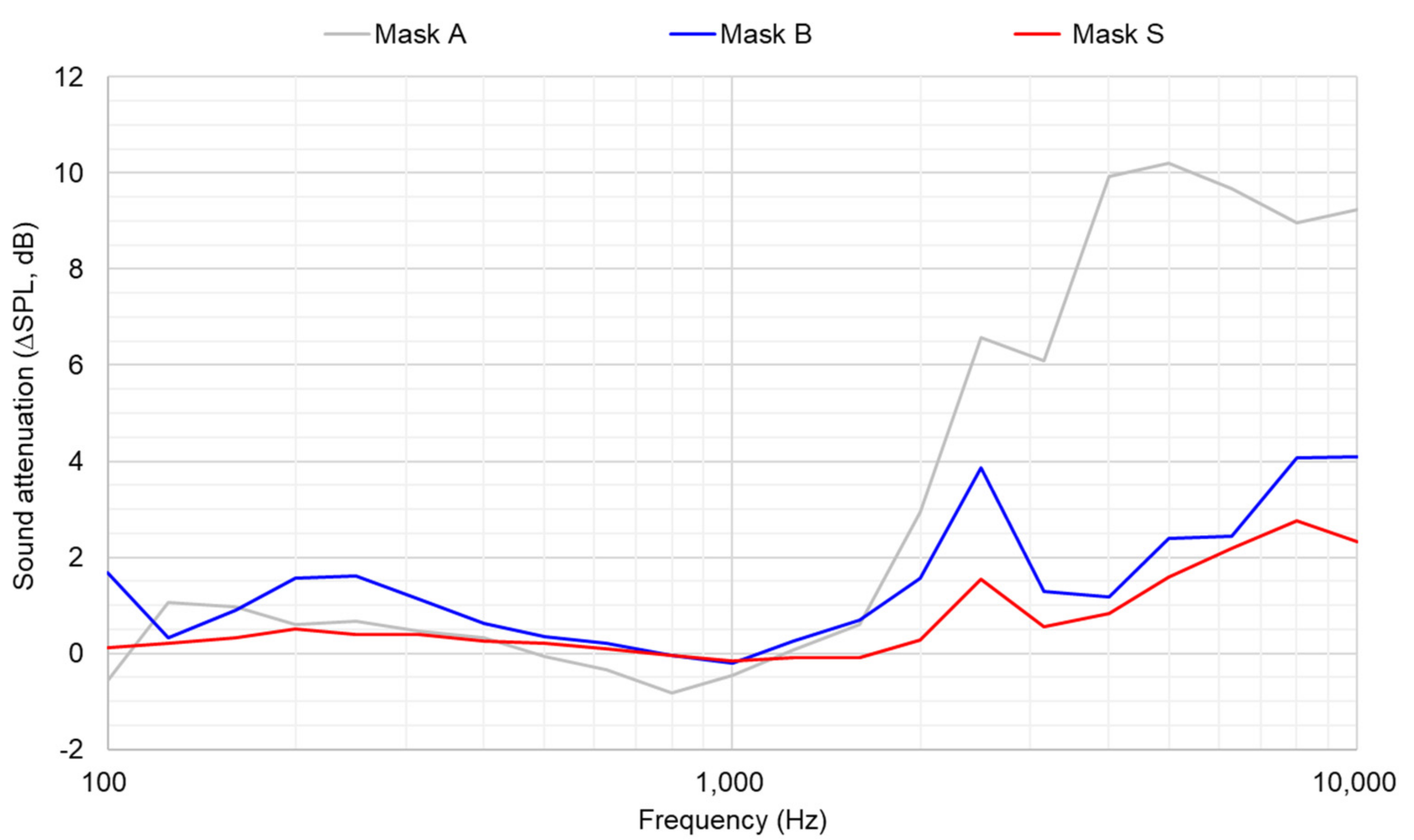
2.5. Acoustic Characterization of the Face Masks
2.6. Measurement of Air Filtration Performance
2.6.1. Breathing Resistance
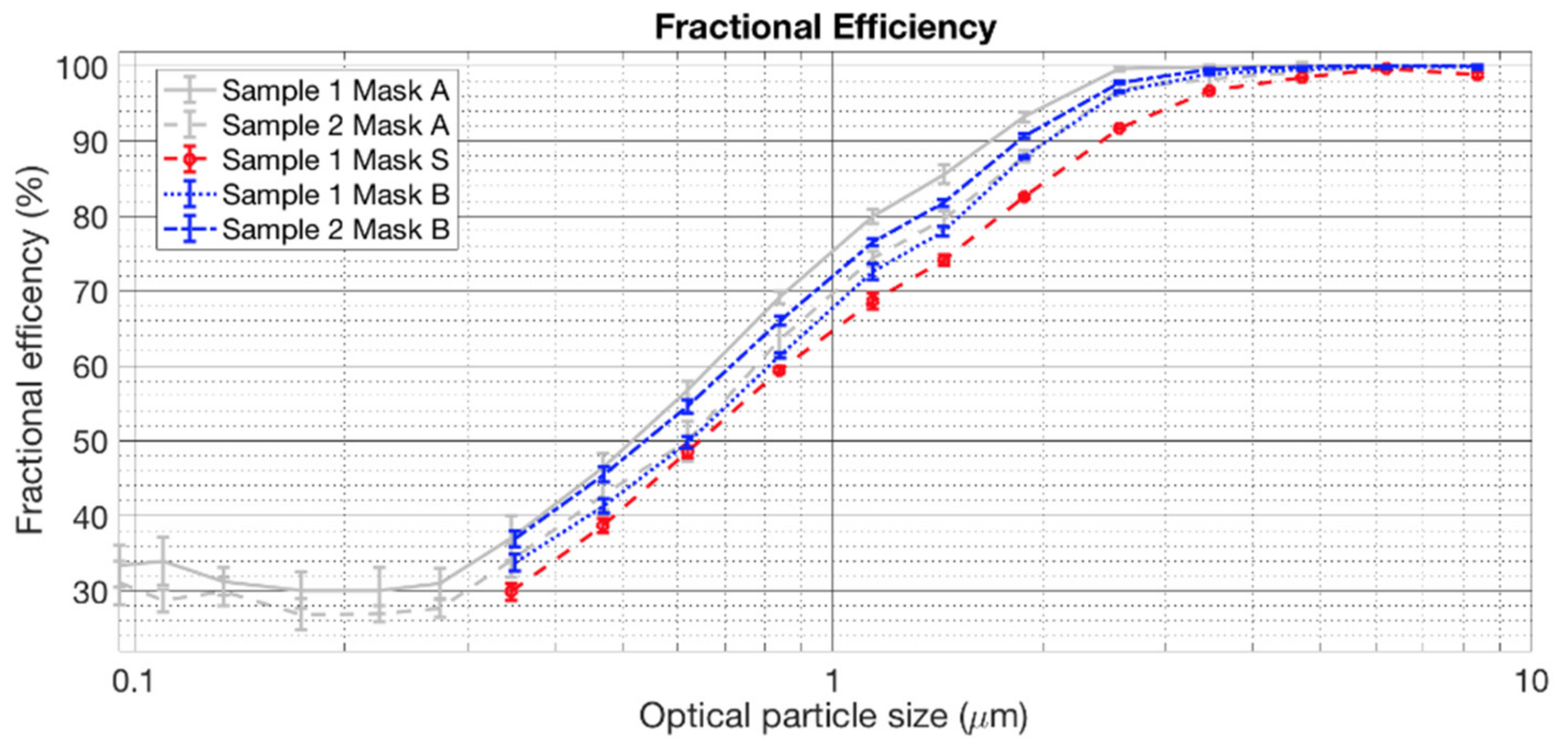
2.6.2. Filtration Efficiency
2.7. Statistical Analysis for Differences among the Masks
3. Results and Discussion
3.1. Face Masks Characterization
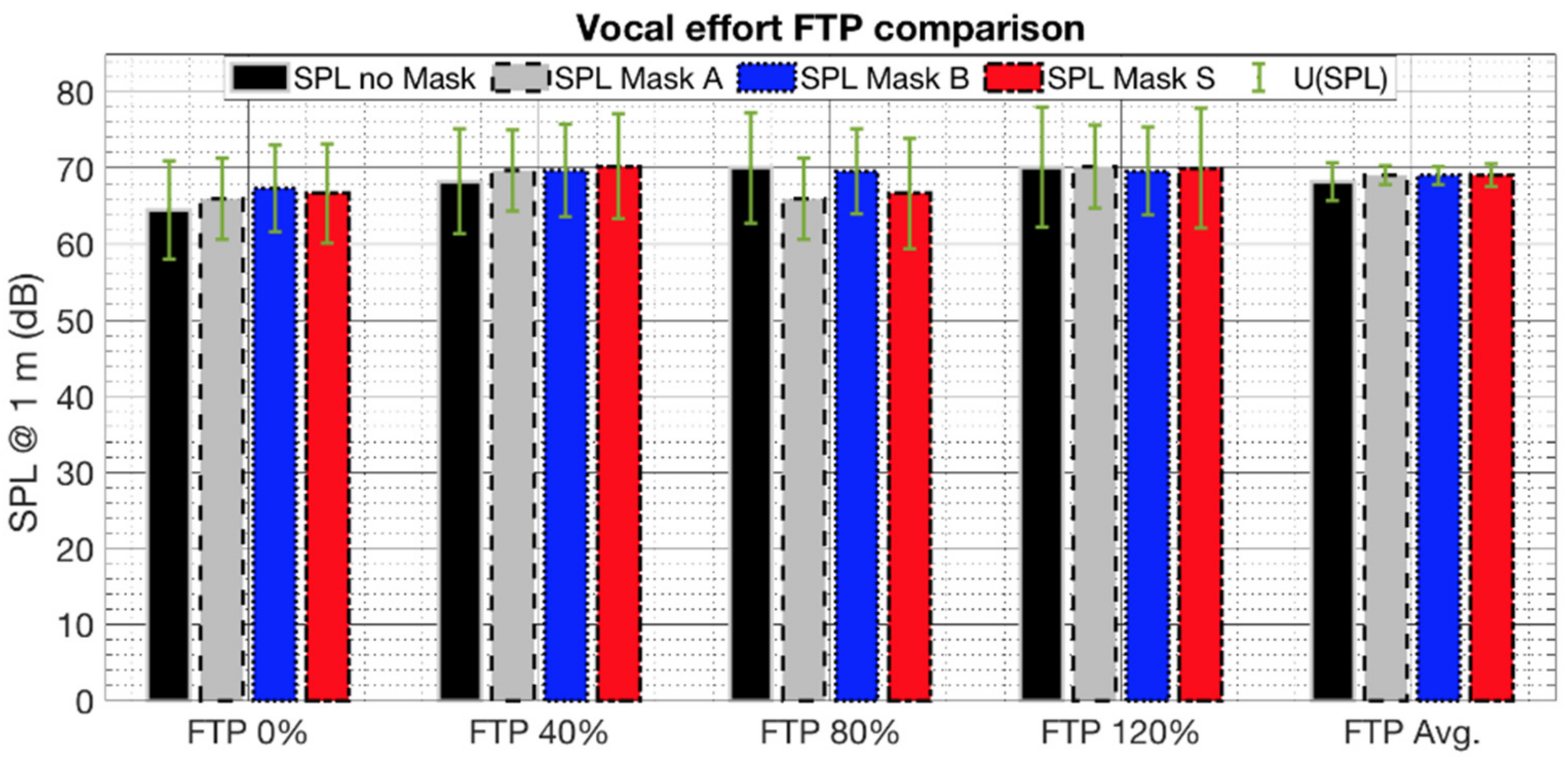
3.2. Voice Monitoring
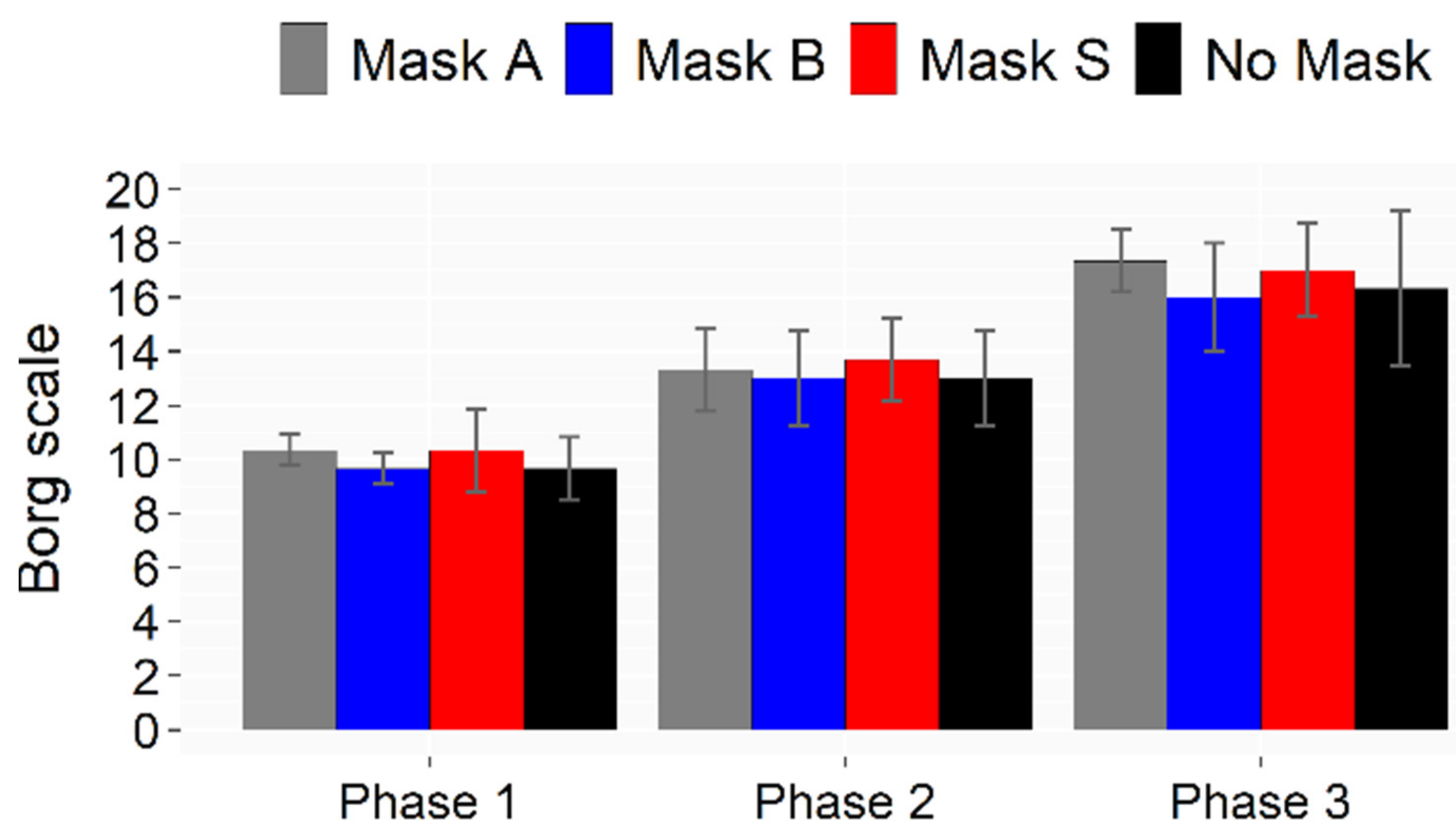
3.3. Sport Activity Tests and Physiological Outcomes
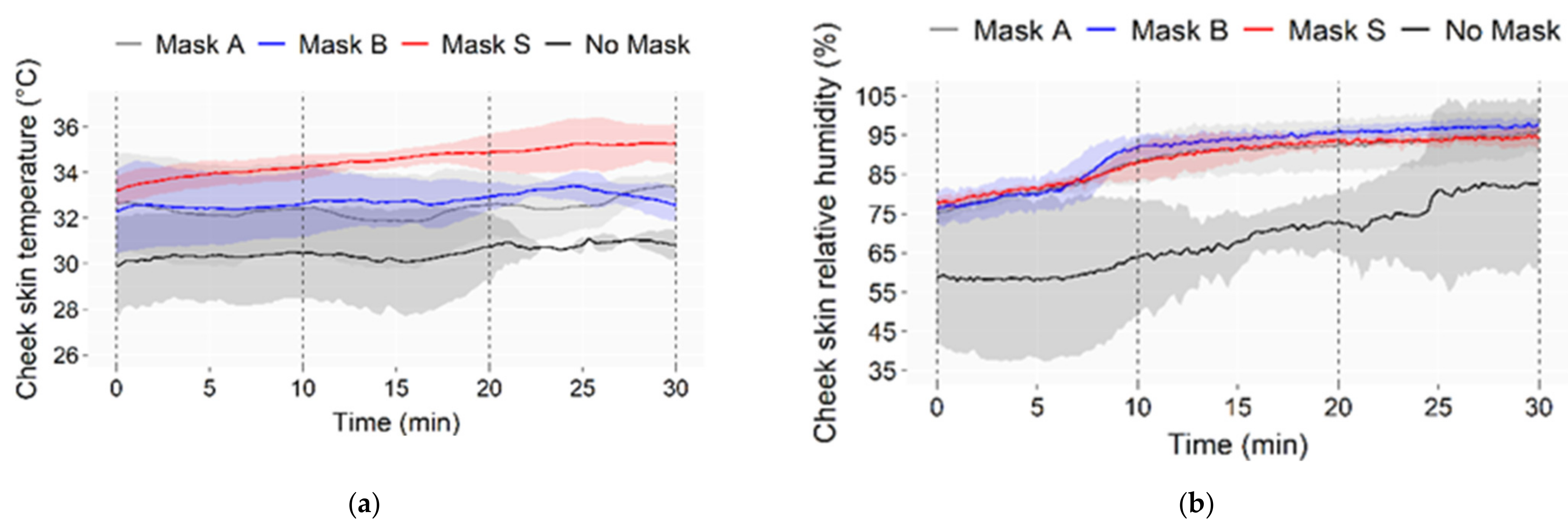
3.3.1. Cheek Skin Temperature and Humidity
3.3.2. Mask Wettability
3.3.3. Heart Rate
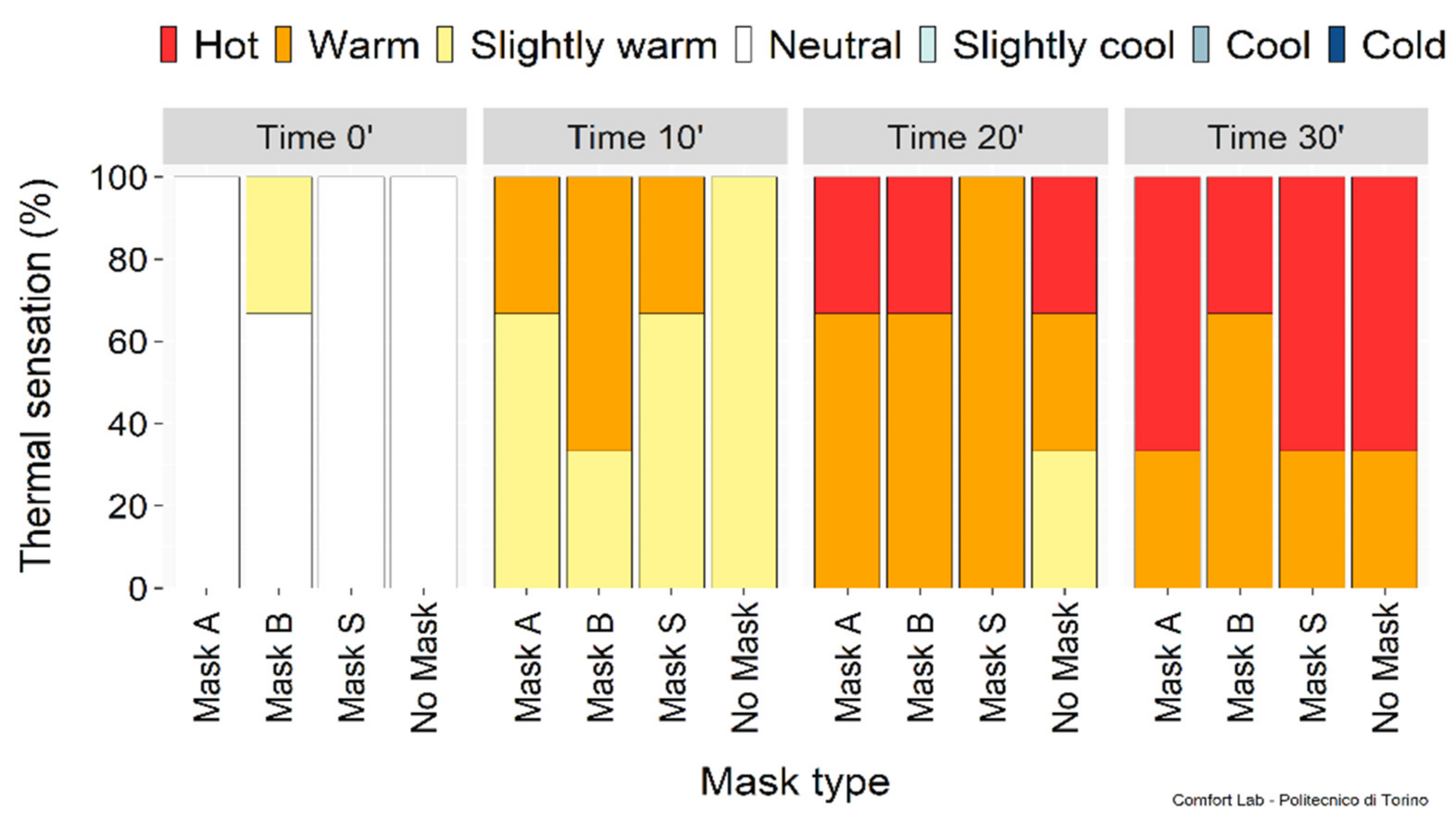
3.3.4. Subjective Sensations
3.4. Overall Statistical Evaluation of the Three Masks
4. Conclusions
- Masks B and S behave similarly and better (lower) in terms of sound attenuation, sound transmission loss, and breathing resistance than Mask A, although mask A performs better (higher) for filtration efficiency, but not to a larger extent;
- Skin temperature under the mask increased by (3–4) °C compared to bare skin. Similar temperatures were observed for Masks A and B, while a significantly higher temperature was measured with Mask S in the last phases of incremental physical activity. However, this does not reflect in the correspondent’s subjective perception;
- No differences were found in the voice monitoring due to the face masks compared to the no mask condition.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rumbach, A.F. Vocal problems of group fitness instructors: Prevalence of self-reported sensory and auditory-perceptual voice symptoms and the need for preventative education and training. J. Voice 2013, 27, e11–e21. [Google Scholar] [CrossRef] [PubMed]
- Fontan, L.; Fraval, M.; Michon, A.; Déjean, S.; Welby-Gieusse, M. Vocal problems in sports and fitness instructors: A study of prevalence, risk factors, and need for prevention in France. J. Voice 2017, 3, e33–e38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venkatraman, A.; Brinton Fujiki, R.; Preeti Sivasankar, M. A review of factors associated with voice problems in the fitness instructor population. J. Voice 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Hamdan, A.-L.; Thayer Sataloff, R.; Hawkshaw, M.J. Voice Disorders in Athletes, Coaches and Other Sports Professionals; Springer Nature Edition: Berlin, Germany, 2021. [Google Scholar]
- Bottalico, P.; Murgia, S.; Puglisi, G.E.; Astolfi, A.; Kirk, K.I. Effect of masks on speech intelligibility in auralized classrooms. J. Acoust. Soc. Am. 2020, 148, 2878–2884. [Google Scholar] [CrossRef] [PubMed]
- Bottalico, P.; Murgia, S.; Puglisi, G.E.; Astolfi, A.; Ishikawa, K. Intelligibility of dysphonic speech in auralized classrooms. J. Acoust. Soc. Am. 2021, 150, 2912–2920. [Google Scholar] [CrossRef]
- Lumb, A.B. Nunn’s Applied Respiratory Physiology, 8th ed.; Elsevier: Amsterdam, The Netherlands, 2017; pp. 227–234. [Google Scholar]
- Goldin, A.; Weinstein, B.E.; Shiman, N. How do medical masks degrade speech perception? Hear. Rev. 2020, 27, 8–9. [Google Scholar]
- Astolfi, A.; Carullo, A.; Pavese, L.; Puglisi, G.E. Duration of voicing and silence periods of continuous speech in different acoustic environments. J. Acoust. Soc. Am. 2015, 137, 565–579. [Google Scholar] [CrossRef] [Green Version]
- D’Orazio, D.; De Salvio, D.; Anderlucci, L.; Garai, M. Measuring the speech level and the student activity in lecture halls: Visual- vs blind-segmentation methods. Appl. Acoust. 2020, 169, 107448. [Google Scholar] [CrossRef]
- Smiljanic, R.; Keerstock, S.; Meemann, K.; Ransom, S.M. Face masks and speaking style affect audio-visual word recognition and memory of native and non-native speech. J. Acoust. Soc. Am. 2021, 149, 4013–4023. [Google Scholar] [CrossRef]
- Puglisi, G.E.; Warzybok, A.; Astolfi, A.; Kollmeier, B. Effect of reverberation and noise type on speech intelligibility in real complex acoustic scenarios. Build. Env. 2021, 204, 108137. [Google Scholar] [CrossRef]
- Litwinowicz, K.; Choroszy, M.; Ornat, M.; Wróbel, A.; Waszczuk, E. Bayesian network meta-analysis of face masks’ impact on human physiology. Sci. Rep. 2022, 12, 5823. [Google Scholar] [CrossRef] [PubMed]
- Farquharson, C.; Baguley, K. Responding to the severe acute respiratory syndrome (SARS) outbreak: Lessons learned in a Toronto emergency department. J. Emerg. Nurs. 2003, 23, 222–228. [Google Scholar] [CrossRef] [Green Version]
- Epstein, D.; Korytny, A.; Isenberg, Y.; Marcusohn, E.; Zukermann, R.; Bishop, B.; Minha, S.; Raz, A.; Miller, A. Return to training in the COVID-19 era: The physiological effects of face masks during exercise. Scand. J. Med. Sci. Sports 2021, 31, 70–75. [Google Scholar] [CrossRef]
- Ruth, N.; Berglund, L.G.; Gwosdow, A.R.; Dubois, A.B. Thermal sensation of the body as influenced by the thermal microclimate in a face mask. Ergonomics 1987, 30, 1689–1703. [Google Scholar]
- Li, Y.; Tokura, H.; Guo, Y.P.; Wong, A.S.W.; Wong, T.; Chung, J.; Newton, E. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int. Arch. Occup. Environ. Health 2005, 78, 501–509. [Google Scholar] [CrossRef]
- Person, E.; Lemercier, C.; Royer, A.; Reychler, G. Effet du port d’un masque de soins lors d’un test de marche de six minutes chez des sujets sains. Rev. Des Mal. Respir. 2018, 35, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Cox, T.; Dodgson, G.; Harris, L.; Perugia, E.; Stone, M.A.; Walsh, M. Improving the measurement and acoustic performance of transparent face masks and shields. J. Acoust. Soc. Am. 2022, 151, 2931–2944. [Google Scholar] [CrossRef]
- Steeneken, H.J.; Houtgast, T. Mutual dependence of the octave-band weights in predicting speech intelligibility. Speech Commun. 1999, 28, 109–123. [Google Scholar] [CrossRef]
- Hinds, W.C. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles; John Wiley: New York, NY, USA, 1999. [Google Scholar]
- EN 149:2001+A1:2009; Respiratory Protective Devices—Filtering Half Masks to Protect against Particles—Requirements, Testing, Marking. European Committee for Standardization: Brussels, Belgium, 2009.
- ISO 16890-2:2016; Air Filters for General Ventilation—Part 2: Measurement of Fractional Efficiency and Air Flow Resistance. International Organization for Standardization: Geneva, Switzerland, 2016.
- Johnson, G.; Morawska, L.; Ristovski, Z.D.; Hargreaves, M.; Mengersen, K.; Chao, C.Y.H.; Wan, M.P.; Li, Y.; Xie, X.; Katoshevski, D.; et al. Modality of human expired aerosol size distributions. J. Aerosol Sci. 2021, 42, 839–851. [Google Scholar] [CrossRef]
- Morawska, L.; Johnson, G.R.; Ristovski, Z.D.; Hargreaves, M.; Mengersen, K.; Corbett, S.; Chao, C.Y.H.; Li, Y.; Katoshevski, D. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. J. Aerosol Sci. 2009, 40, 256–269. [Google Scholar] [CrossRef] [Green Version]
- Konda, A.; Prakash, A.; Moss, G.A.; Schmoldt, M.; Grant, G.D.; Guha, S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano 2020, 14, 6339–6347. [Google Scholar] [CrossRef] [PubMed]
- Aydin, O.; Emon, B.; Cheng, S.; Hong, L.; Chamorro, L.P.; Saif, M.T.A. Performance of fabrics for home-made masks against spread of COVID-19 through droplets: A quantitative mechanistic study. Extrem. Mech. Lett. 2020, 40, 100924. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Li, M.; Zheng, M.; Cai, X.; Yang, J.; Zhang, S.; Yilifate, A.; Zheng, Y.; Lin, Q.; Liang, J.; et al. Effect of surgical masks on cardiopulmonary function in healthy young subjects: A crossover study. Front. Psychol. 2021, 12, 710573. [Google Scholar] [CrossRef] [PubMed]
- UNI EN 14683:2019; Maschere Facciali Ad Uso Medico—Requisiti E Metodi Di Prova. Ente Italiano di Normazione: Milano, Italy, 2019.
- Available online: https://www.ufimask.com (accessed on 1 April 2022).
- Denham, J.; Scott-Hamilton, J.; Hagstrom, A.D.; Gray, A.J. Cycling power outputs predict functional threshold power and maximum oxygen uptake. J. Strength Cond. Res. 2020, 34, 3489–3497. [Google Scholar] [CrossRef]
- EN ISO 28802:2012; Ergonomics of the Physical Environment—Assessment of Environments by Means of an Environmental Survey Involving Physical Measurements of the Environment and Subjective Responses of People. European Committee for Standardization: Brussels, Belgium, 2012.
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Mehta, D.D.; Zañartu, M.; Feng, S.W.; Cheyne, H.A.; Hillman, R.E. Mobile Voice Health Monitoring Using a Wearable Accelerometer Sensor and a Smartphone Platform. IEEE Trans. Bio. Eng. 2012, 59, 3090–3096. [Google Scholar] [CrossRef] [Green Version]
- Carullo, A.; Vallan, A.; Astolfi, A. Design issues for a portable vocal analyzer. IEEE Trans. Instrum. Meas. 2013, 62, 1084–1093. [Google Scholar] [CrossRef]
- Bottalico, P.; Ipsaro Passione, I.; Astolfi, A.; Carullo, A.; Hunter, E.J. Accuracy of the quantities measured by four vocal dosimeters and its uncertainty. J. Acoust. Soc. Am. 2018, 143, 1591–1602. [Google Scholar] [CrossRef]
- Astolfi, A.; Castellana, A.; Carullo, A.; Puglisi, G.E. Uncertainty of speech level parameters measured with a contact-sensor-based device and a headworn microphone. J. Acoust. Soc. Am. 2018, 143, EL496–EL502. [Google Scholar] [CrossRef]
- Carullo, A.; Penna, A.; Vallan, A.; Astolfi, A.; Pavese, L.; Puglisi, G.E. Traceability and uncertainty of vocal parameters estimated through a contact microphone. In Proceedings of the 2014 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Lisbon, Portugal, 11–12 June 2014. [Google Scholar]
- Carullo, A.; Vallan, A.; Astolfi, A.; Pavese, L.; Puglisi, G.E. Validation of calibration procedures and uncertainty estimation of contact-microphone based vocal analyzers. Measurement 2015, 74, 130–142. [Google Scholar] [CrossRef] [Green Version]
- Castellana, A.; Carullo, A.; Astolfi, A.; Puglisi, G.E.; Fugiglando, U. Intra-speaker and inter-speaker variability in speech sound pressure level across repeated readings. J. Acoust. Soc. Am. 2017, 141, 2353–2363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puglisi, G.E.; Cantor Cutiva, L.C.; Pavese, L.; Castellana, A.; Bona, M.; Fasolis, S.; Lorenzatti, V.; Carullo, A.; Burdorf, A.; Bronuzzi, F.; et al. Acoustic comfort in high-school classrooms for students and teachers. Energy Procedia 2015, 78, 3096–3101. [Google Scholar] [CrossRef] [Green Version]
- Calosso, G.; Puglisi, G.E.; Astolfi, A.; Castellana, A.; Carullo, A.; Pellerey, F. A one-school year longitudinal study of secondary school teachers’ voice parameters and the influence of classroom acoustics. J. Acoust. Soc. Am. 2017, 142, 1055–1066. [Google Scholar] [CrossRef] [PubMed]
- Puglisi, G.E.; Astolfi, A.; Cantor Cutiva, L.C.; Carullo, A. Four-day-follow-up study on the voice monitoring of primary school teachers: Relationships with conversational task and classroom acoustics. J. Acoust. Soc. Am. 2017, 141, 441–452. [Google Scholar] [CrossRef] [PubMed]
- Anderson, A.; Bader, M.; Bard, E.; Boyle, E.; Doherty, G.M.; Garrod, S.; Isard, S.; Kowtko, J.; McAllister, J.; Miller, J.; et al. The HCRC map task corpus. Lang. Speech 1991, 34, 351–366. [Google Scholar] [CrossRef]
- ANSI S3.5-1997 (Riconfermata da ANSI nel 2002); Methods for Calculation of the Speech Intelligibility Index. ANSI: Washington, DC, USA, 1997.
- Chmelík, V.; Urbán, D.; Zelem, L.; Rychtáriková, M. Effect of mouth mask and face shield on speech spectrum in Slovak language. Appl. Sci. 2021, 11, 4829. [Google Scholar] [CrossRef]
- ISO 10534-2:1998; Acoustics—Determination of Sound Absorption Coefficient and Impedance in Impedance Tubes—Part 2: Transfer-Function Method. International Organization for Standardization: Geneva, Switzerland, 1998.
- ASTM E1050-19; Standard Test Method for Impedance and Absorption of Acoustical Materials Using a Tube, Two Microphones and a Digital Frequency Analysis System. ASTM International: West Conshohocken, PA, USA, 2019. Available online: www.astm.org (accessed on 1 April 2022).
- ASTM E2611-19; Standard Test Method for Normal Incidence Determination of Porous Material Acoustical Properties Based on the Transfer Matrix Method. ASTM International: West Conshohocken, PA, USA, 2019. Available online: www.astm.org (accessed on 1 April 2022).
- Pilon, D.; Panneton, R.; Sgard, F. Behavioural criterion quantifying the effects of circumferential air gaps on porous materials in the standing wave tube. J. Acoust. Soc. Am. 2004, 116, 344–356. [Google Scholar] [CrossRef]
- Taborri, J.; Stocchi, B.; Calabrò, G.; Rossi, S. On the breathability measurement of surgical masks: Uncertainty, repeatability, and reproducibility analysis. IEEE T. Instrum. Meas. 2022, 71, 1000709. [Google Scholar] [CrossRef]
- Tronville, P.; Sala, R. Minimization of resistance in pleated-media air filter designs: Empirical and CFD approaches. HVACR Res. 2003, 9, 95–106. [Google Scholar] [CrossRef]
- UNI/PdR:2020. Maschere Di Comunità—Parte 2: Metodi Di Prova; Ente Italiano di Normazione (UNI): Milano, Italy, 2020. [Google Scholar]
- Siegel, S.; Castellan, N.J., Jr. Nonparametric Statistics for the Behavioral Sciences; McGraw-Hill Edition: New York, NY, USA, 1988; pp. 1–399. [Google Scholar]






| Title 1 | Tester 1 | Tester 2 | Tester 3 |
|---|---|---|---|
| Age | 22 | 22 | 22 |
| Height (cm) | 181 | 165 | 172 |
| Weight (kg) | 65 | 60 | 63 |
| BMI 1 | 19.8 | 22.0 | 21.3 |
| FTP 2 (W) | 210 | 210 | 175 |
| Mask A | Mask B | Mask S | |
|---|---|---|---|
| ∆SPL0.4–5 kHz 3rd oct (dB) | 2.9 (4.2) | 1.0 (1.2) | 0.4 (0.6) |
| ∆SPL1.6–5 kHz 3rd oct (dB) | 6.1 (3.8) | 1.8 (1.1) | 0.8 (0.7) |
| α0, 1–5 kHz (-) | 0.14 (0.08) | 0.10 (0.07) | 0.15 (0.07) |
| α0, 0.9–3 kHz (-) | 0.18 (0.05) | 0.13 (0.05) | 0.18 (0.06) |
| STL1–5 kHz (dB) | 2.6 (0.6) | 1.6 (0.2) | 1.2 (0.1) |
| STL1–3 kHz (dB) | 2.8 (0.4) | 1.6 (0.2) | 1.3 (0.0) |
| Breathing Resistance (Pa) | 353 | 123 | 66 |
| eCFC (%) | 98 | 93 | 87 |
| Mask A | Mask B | Mask S | |
|---|---|---|---|
| Average moisture content (g) | 2.0 ± 0.5 | 1.7 ± 0.1 | 9.3 ± 0.4 |
| Weight gain (%) | 37.7 | 55.4 | 43.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Astolfi, A.; Puglisi, G.E.; Shtrepi, L.; Tronville, P.; Marval Diaz, J.A.; Carullo, A.; Vallan, A.; Atzori, A.; Ferri, A.; Dotti, F. Effects of Face Masks on Physiological Parameters and Voice Production during Cycling Activity. Int. J. Environ. Res. Public Health 2022, 19, 6491. https://doi.org/10.3390/ijerph19116491
Astolfi A, Puglisi GE, Shtrepi L, Tronville P, Marval Diaz JA, Carullo A, Vallan A, Atzori A, Ferri A, Dotti F. Effects of Face Masks on Physiological Parameters and Voice Production during Cycling Activity. International Journal of Environmental Research and Public Health. 2022; 19(11):6491. https://doi.org/10.3390/ijerph19116491
Chicago/Turabian StyleAstolfi, Arianna, Giuseppina Emma Puglisi, Louena Shtrepi, Paolo Tronville, Jesús Alejandro Marval Diaz, Alessio Carullo, Alberto Vallan, Alessio Atzori, Ada Ferri, and Francesca Dotti. 2022. "Effects of Face Masks on Physiological Parameters and Voice Production during Cycling Activity" International Journal of Environmental Research and Public Health 19, no. 11: 6491. https://doi.org/10.3390/ijerph19116491
APA StyleAstolfi, A., Puglisi, G. E., Shtrepi, L., Tronville, P., Marval Diaz, J. A., Carullo, A., Vallan, A., Atzori, A., Ferri, A., & Dotti, F. (2022). Effects of Face Masks on Physiological Parameters and Voice Production during Cycling Activity. International Journal of Environmental Research and Public Health, 19(11), 6491. https://doi.org/10.3390/ijerph19116491












