The Effects of Meditation with Stabilization Exercise in Marine Region on Pain, Tactile Sense, Muscle Characteristics and Strength, Balance, Quality of Life, and Depression in Female Family Caregivers of People with Severe Physical Disabilities: A Randomized Single-Blinded Controlled Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
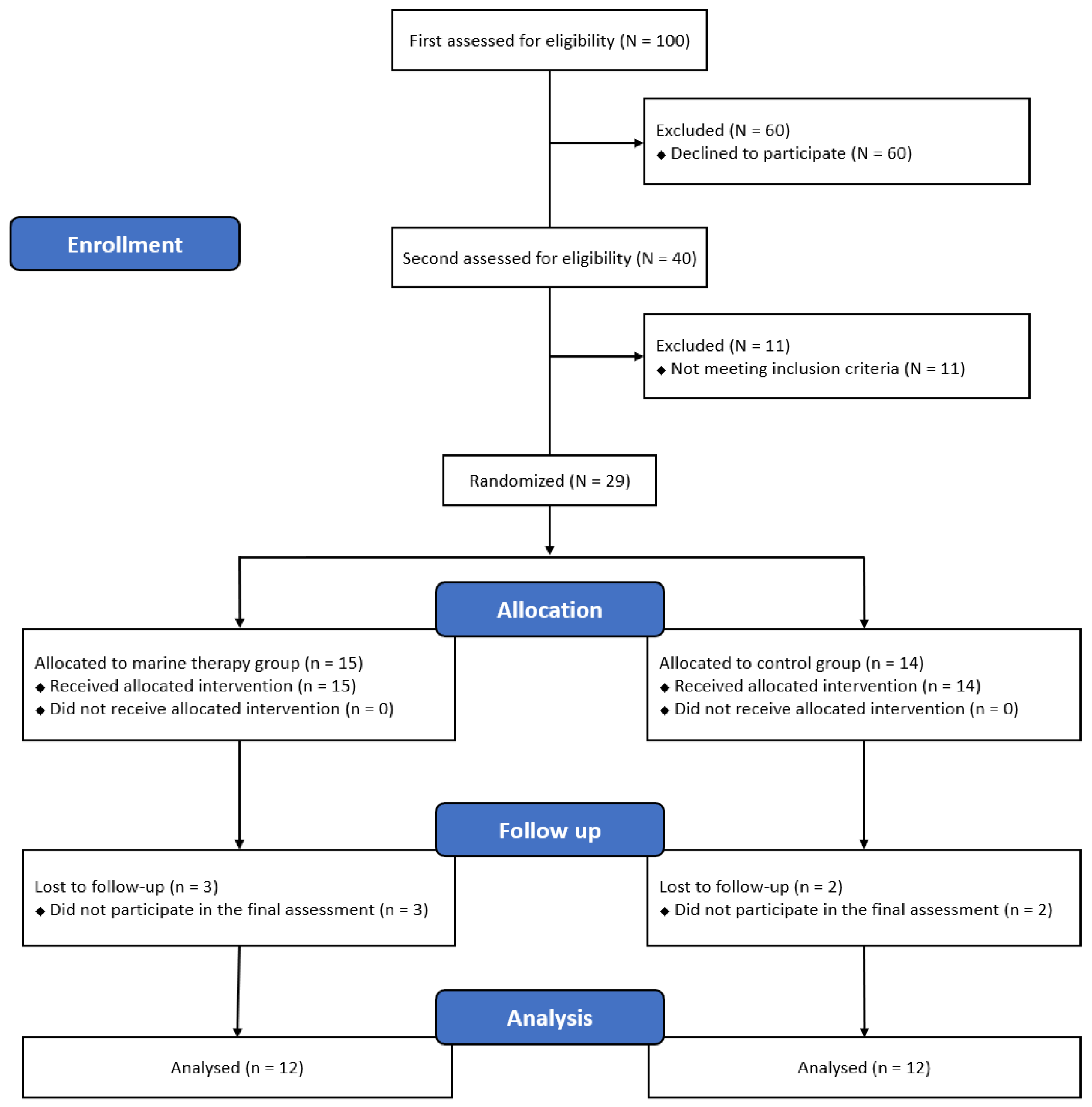
2.1. Participants
2.2. Procedure
2.3. Measurement
2.3.1. Pain Intensity
2.3.2. Pain Pressure Threshold
2.3.3. Tactile Spatial Acuity
2.3.4. Muscle Characteristics
2.3.5. Muscle Strength
2.3.6. Dynamic Balance
2.3.7. Quality of Life
2.3.8. Depression
2.4. Intervention
2.4.1. Meditation (35 min)
2.4.2. Stabilization Exercise (25 min)
2.5. Statistics Analysis
3. Results
3.1. Pain Intensity
3.2. Pain Pressure Threshold
3.3. Tactile Spatial Acuity
3.4. Muscle Chatracteristics
3.5. Muscle Strength
3.6. Dynamic Balance
3.7. Quality of Life
3.8. Depression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Chuluunbaatar, E.; Chou, Y.J.; Pu, C. Quality of life of stroke survivors and their informal caregivers: A prospective study. Disabil. Health J. 2016, 9, 306–312. [Google Scholar] [CrossRef]
- Hong, S.E.; Kim, C.H.; Kim, E.J.; Joa, K.L.; Kim, T.H.; Kim, S.K.; Han, H.J.; Lee, E.C.; Jung, H.Y. Effect of a Caregiver’s Education Program on Stroke Rehabilitation. Ann. Rehabil. Med. 2017, 41, 16–24. [Google Scholar] [CrossRef] [Green Version]
- Roth, D.L.; Fredman, L.; Haley, W.E. Informal caregiving and its impact on health: A reappraisal from population-based studies. Gerontologist 2015, 55, 309–319. [Google Scholar] [CrossRef] [Green Version]
- Statistics Canada; Turcotte, M. 2013. Available online: https://www150.statcan.gc.ca/n1/pub/75-006-x/2013001/article/11858-eng.pdf (accessed on 13 June 2018).
- Vincent-Onabajo, G.; Ali, A.; Hamzat, T. Quality of life of Nigerian informal caregivers of community-dwelling stroke survivors. Scand. J. Caring Sci. 2013, 27, 977–982. [Google Scholar] [CrossRef]
- Darragh, A.R.; Sommerich, C.M.; Lavender, S.A.; Tanner, K.J.; Vogel, K.; Campo, M. Musculoskeletal Discomfort, Physical Demand, and Caregiving Activities in Informal Caregivers. J. Appl. Gerontol. 2015, 34, 734–760. [Google Scholar] [CrossRef] [Green Version]
- Chung, M.L.; Lennie, T.A.; Mudd-Martin, G.; Dunbar, S.B.; Pressler, S.J.; Moser, D.K. Depressive symptoms in patients with heart failure negatively affect family caregiver outcomes and quality of life. Eur. J. Cardiovasc. Nurs. 2016, 15, 30–38. [Google Scholar] [CrossRef]
- Lim, Y.M.; Ahn, Y.H.; Ahn, J.Y. Multidimensional Caregiving Burden of Female Family Caregivers in Korea. Clin. Nurs. Res. 2016, 25, 665–682. [Google Scholar] [CrossRef]
- Kim, M.D.; Hong, S.C.; Lee, C.I.; Kim, S.Y.; Kang, I.O.; Lee, S.Y. Caregiver burden among caregivers of Koreans with dementia. Gerontology 2009, 55, 106–113. [Google Scholar] [CrossRef]
- Pascoe, M.C.; Thompson, D.R.; Ski, C.F. Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology 2017, 86, 152–168. [Google Scholar] [CrossRef]
- de Bruin, E.I.; Formsma, A.R.; Frijstein, G.; Bögels, S.M. Mindful2Work: Effects of Combined Physical Exercise, Yoga, and Mindfulness Meditations for Stress Relieve in Employees. A Proof of Concept Study. Mindfulness 2017, 8, 204–217. [Google Scholar] [CrossRef] [Green Version]
- Waelde, L.C.; Thompson, L.; Gallagher-Thompson, D. A pilot study of a yoga and meditation intervention for dementia caregiver stress. J. Clin. Psychol. 2004, 60, 677–687. [Google Scholar] [CrossRef]
- Waelde, L.C.; Meyer, H.; Thompson, J.M.; Thompson, L.; Gallagher-Thompson, D. Randomized controlled trial of inner resources meditation for family dementia caregivers. J. Clin. Psychol. 2017, 73, 1629–1641. [Google Scholar] [CrossRef]
- Hurley, R.V.; Patterson, T.G.; Cooley, S.J. Meditation-based interventions for family caregivers of people with dementia: A review of the empirical literature. Aging Ment. Health 2014, 18, 281–288. [Google Scholar] [CrossRef]
- Kaplan, S. The restorative benefits of nature: Towards an integrative framework. J. Environ. Psychol. 1995, 16, 169–182. [Google Scholar] [CrossRef]
- Lim, K.H.; Nam, K.J.; Rah, Y.C.; Cha, J.; Lee, S.J.; Lee, M.G.; Choi, J. The Effect of Natural Ocean Sound Exposure and Ocean-Side Relaxation on Chronic Tinnitus Patients: A Pilot Study in Korea. Ear Nose Throat J. 2021, 100, NP256–NP262. [Google Scholar] [CrossRef] [Green Version]
- Katz, U.; Shoenfeld, Y.; Zakin, V.; Sherer, Y.; Sukenik, S. Scientific evidence of the therapeutic effects of dead sea treatments: A systematic review. Semin. Arthritis Rheum. 2012, 42, 186–200. [Google Scholar] [CrossRef]
- Shin, H.J.; Kim, S.H.; Jeon, E.T.; Lee, M.G.; Lee, S.J.; Cho, H.Y. Effects of therapeutic exercise on sea sand on pain, fatigue, and balance in patients with chronic ankle instability: A feasibility study. J. Sports Med. Phys. Fit. 2019, 59, 1200–1205. [Google Scholar] [CrossRef]
- Krüger, C.; Smythe, J.W.; Spencer, J.D.; Hasse, S.; Panske, A.; Chiuchiarelli, G.; Schallreuter, K.U. Significant immediate and long-term improvement in quality of life and disease coping in patients with vitiligo after group climatotherapy at the Dead Sea. Acta Derm.-Venereol. 2011, 91, 152–159. [Google Scholar] [CrossRef]
- Binnie, M.J.; Dawson, B.; Pinnington, H.; Landers, G.; Peeling, P. Sand training: A review of current research and practical applications. J. Sports Sci. 2014, 32, 8–15. [Google Scholar] [CrossRef]
- Hu, P.; Yang, Q.; Kong, L.; Hu, L.; Zeng, L. Relationship between the anxiety/depression and care burden of the major caregiver of stroke patients. Medicine 2018, 97, e12638. [Google Scholar] [CrossRef]
- Muchada, M.; Rubiera, M.; Rodriguez-Luna, D.; Pagola, J.; Flores, A.; Kallas, J.; Sanjuan, E.; Meler, P.; Alvarez-Sabin, J.; Ribo, M.; et al. Baseline National Institutes of Health stroke scale-adjusted time window for intravenous tissue-type plasminogen activator in acute ischemic stroke. Stroke 2014, 45, 1059–1063. [Google Scholar] [CrossRef] [Green Version]
- Boonstra, A.M.; Schiphorst Preuper, H.R.; Reneman, M.F.; Posthumus, J.B.; Stewart, R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 2008, 31, 165–169. [Google Scholar] [CrossRef] [Green Version]
- Pires, D.; Cruz, E.B.; Caeiro, C. Aquatic exercise and pain neurophysiology education versus aquatic exercise alone for patients with chronic low back pain: A randomized controlled trial. Clin. Rehabil. 2015, 29, 538–547. [Google Scholar] [CrossRef]
- Wylde, V.; Palmer, S.; Learmonth, I.D.; Dieppe, P. Test-retest reliability of Quantitative Sensory Testing in knee osteoarthritis and healthy participants. Osteoarthr. Cartil. 2011, 19, 655–658. [Google Scholar] [CrossRef] [Green Version]
- Simons, D.G.; Travell, J.; Simons, L.S. Osteoarthritis and Cartilage, 2nd ed.; Williams & Wilkins: Baltimore, MD, USA, 1999; Volume 1. [Google Scholar]
- Harvie, D.S.; Kelly, J.; Buckman, H.; Chan, J.; Sutherland, G.; Catley, M.; Novak, J.; Tuttle, N.; Sterling, M. Tactile acuity testing at the neck: A comparison of methods. Musculoskelet. Sci. Pract. 2017, 32, 23–30. [Google Scholar] [CrossRef]
- Chuang, L.L.; Wu, C.Y.; Lin, K.C. Reliability, validity, and responsiveness of myotonometric measurement of muscle tone, elasticity, and stiffness in patients with stroke. Arch. Phys. Med. Rehabil. 2012, 93, 532–540. [Google Scholar] [CrossRef]
- Pruyn, E.C.; Watsford, M.L.; Murphy, A.J. Validity and reliability of three methods of stiffness assessment. J. Sport Health Sci. 2016, 5, 476–483. [Google Scholar] [CrossRef] [Green Version]
- Hamilton, G.F.; McDonald, C.; Chenier, T.C. Measurement of grip strength: Validity and reliability of the sphygmomanometer and jamar grip dynamometer. J. Orthop. Sports Phys. Ther. 1992, 16, 215–219. [Google Scholar] [CrossRef]
- Shim, J.H.; Roh, S.Y.; Kim, J.S.; Lee, D.C.; Ki, S.H.; Yang, J.W.; Jeon, M.K.; Lee, S.M. Normative measurements of grip and pinch strengths of 21st century korean population. Arch. Plast. Surg. 2013, 40, 52–56. [Google Scholar] [CrossRef] [Green Version]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Skevington, S.M.; Lotfy, M.; O’Connell, K.A.; WHOQOL Group. The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual. Life Res. 2004, 13, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Min, S.K.; Lee, C.I.; Kim, K.I.; Suh, S.Y.; Kim, D.K. Development of Korean version of WHO quality of life scale abbreviated version (WHOQOL-BREF). J. Korean Neuropsychiatr. Assoc. 2000, 571–579. [Google Scholar]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yi, J.S.; Bae, S.O.; Ahn, Y.M.; Park, D.B.; Noh, K.S.; Shin, H.K.; Woo, H.W.; Lee, H.S.; Han, S.I.; Kim, Y.S. Validity and reliability of the Korean version of the Hamilton Depression Rating Scale (K-HDRS). J. Korean Neuropsychiatr. Assoc. 2005, 44, 456–464. [Google Scholar]
- Menezes, C.B.; de Paula Couto, M.C.; Buratto, L.G.; Erthal, F.; Pereira, M.G.; Bizarro, L. The improvement of emotion and attention regulation after a 6-week training of focused meditation: A randomized controlled trial. Evid.-Based Complementary Altern. Med. 2013, 2013, 984678. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Lee, M.M. Effects of a Progressive Stabilization Exercise Program Using Respiratory Resistance for Patients with Lumbar Instability: A Randomized Controlled Trial. Med. Sci. Monit. 2019, 25, 1740–1748. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power for the Social Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Kim, J.S.; Ju, M.Y.; Bae, S.S. The effect of dynamic lumbar stabilization exercise on low back pain patients. J. Korean Phys. Ther. 2001, 13, 495–507. [Google Scholar]
- Kim, E.J.; Hwang, B.J.; Kim, J.H. The Effect of core strength exercises on balance and walking in patients with stroke. J. Korean Phys. Ther. 2009, 21, 17–22. [Google Scholar]
- Sisto, S.A.; Dyson-Hudson, T. Dynamometry testing in spinal cord injury. J. Rehabil. Res. Dev. 2007, 44, 123–136. [Google Scholar] [CrossRef]
- Rajalaxmi, V.; Manickam, M.; Srilakshmi, M.; Arunselvi, J.; Jayabarathi, R.; Anupreethi, P.; Sujatha, K. The role of multistep core stability exercise with and without conventional neck exercises in the treatment of chronic non-specific neck pain a randomized controlled trial. Biomedicine 2020, 40, 232–235. [Google Scholar] [CrossRef]
- Celenay, S.T.; Akbayrak, T.; Kaya, D.O. A Comparison of the Effects of stabilization exercises plus manual therapy to those of stabilization exercises alone in patients with nonspecific mechanical neck pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2016, 46, 44–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Celenay, S.T.; Kaya, D.O.; Akbayrak, T. Cervical and scapulothoracic stabilization exercises with and without connective tissue massage for chronic mechanical neck pain: A prospective, randomised controlled trial. Man. Ther. 2016, 21, 144–150. [Google Scholar] [CrossRef]
- Başkurt, Z.; Başkurt, F.; Gelecek, N.; Özkan, M.H. The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. J. Back Musculoskelet. Rehabil. 2011, 24, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Moezy, A.; Sepehrifar, S.; Solaymani Dodaran, M. The effects of scapular stabilization based exercise therapy on pain, posture, flexibility and shoulder mobility in patients with shoulder impingement syndrome: A controlled randomized clinical trial. Med. J. Islamic Repub. Iran 2014, 28, 87. [Google Scholar]
- Kobesova, A.; Dzvonik, J.; Kolar, P.; Sardina, A.; Andel, R. Effects of shoulder girdle dynamic stabilization exercise on hand muscle strength. Isokinet. Exerc. Sci. 2015, 23, 21–32. [Google Scholar] [CrossRef] [Green Version]
- Thomas, E.M.; Sahlberg, M.; Svantesson, U. The effect of resistance training on handgrip strength in young adults. Isokinet. Exerc. Sci. 2008, 16, 125–131. [Google Scholar] [CrossRef]
- Hwang, B.J.; Kim, J.W. Effects of lumbar stabilization exercise on lumbar and lower extremity strength of the elderly women. J. Korean Soc. Phys. Med. 2011, 6, 267–275. [Google Scholar]
- Lee, W.J.; Lim, C.H. Effect of unstable surface lumbar stabilization exercise on trunk posture and balance ability in patients with scoliosis. J. Korean Soc. Phys. Med. 2012, 7, 59–67. [Google Scholar] [CrossRef]
- Kabat-Zinn, J.; Lipworth, L.; Burney, R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J. Behav. Med. 1985, 8, 163–190. [Google Scholar] [CrossRef]
- Cramer, H.; Haller, H.; Lauche, R.; Dobos, G. Mindfulness-based stress reduction for low back pain. A systematic review. BMC Complementary Altern. Med. 2012, 12, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lauche, R.; Cramer, H.; Dobos, G.; Langhorst, J.; Schmidt, S. A systematic review and meta-analysis of mindfulness-based stress reduction for the fibromyalgia syndrome. J. Psychosom. Res. 2013, 75, 500–510. [Google Scholar] [CrossRef]
- Lee, C.; Crawford, C.; Hickey, A.; Active Self-Care Therapies for Pain (PACT) Working Group. Mind-body therapies for the self-management of chronic pain symptoms. Pain Med. 2014, 15 (Suppl. 1), S21–S39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aftanas, L.; Golosheykin, S. Impact of regular meditation practice on EEG activity at rest and during evoked negative emotions. Int. J. Neurosci. 2014, 115, 893–909. [Google Scholar] [CrossRef]
- Aftanas, L.I.; Golocheikine, S.A. Non-linear dynamic complexity of the human EEG during meditation. Neurosci. Lett. 2002, 330, 143–146. [Google Scholar] [CrossRef]
- Benarroch, E.E. Pain-autonomic interactions. Neurol. Sci. 2006, 27 (Suppl. 2), S130–S133. [Google Scholar] [CrossRef]
- Lee, J.M.; Yi, C.H.; Kwon, O.Y.; Jeon, H.S. The effect of lumbar stabilization exercise for caregivers with chronic low back pain. Phys. Ther. Korea 2011, 18, 9–17. [Google Scholar]
- Cuthbert, C.A.; King-Shier, K.M.; Ruether, J.D.; Tapp, D.M.; Wytsma-Fisher, K.; Fung, T.S.; Culos-Reed, S.N. The Effects of Exercise on Physical and Psychological Outcomes in Cancer Caregivers: Results From the RECHARGE Randomized Controlled Trial. Ann. Behav. Med. 2018, 52, 645–661. [Google Scholar] [CrossRef]
- Park, B.J.; MIYAZAKI, Y. Physiological effects of viewing forest landscapes: Results of field tests in Atsugi city, Japan. J. Korean Soc. For. Sci. 2008, 97, 634–640. [Google Scholar]
- Choi, J.H.; Kim, H.J. The Effect of 12-week forest walking on functional fitness and body image in the elderly women. J. Korean Inst. For. Recreat. Welf. 2017, 21, 47–56. [Google Scholar] [CrossRef]
- Cloutier, R.; Horr, S.; Niemi, J.B.; D’Andrea, S.; Lima, C.; Harry, J.D.; Veves, A. Prolonged mechanical noise restores tactile sense in diabetic neuropathic patients. Int J Low Extrem Wounds 2009, 8, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Luedtke, K.; Adamczyk, W.; Mehrtens, K.; Moeller, I.; Rosenbaum, L.; Schaefer, A.; Schroeder, J.; Szikszay, T.; Zimmer, C.; Wollesen, B. Upper cervical two-point discrimination thresholds in migraine patients and headache-free controls. J Headache Pain 2018, 19, 47. [Google Scholar] [CrossRef] [PubMed]
- Moseley, L.G.; Zalucki, N.M.; Wiech, K. Tactile discrimination, but not tactile stimulation alone, reduces chronic limb pain. Pain 2008, 137, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Quevedo, A.S.; Mørch, C.D.; Andersen, O.K.; Coghill, R.C. Lateral inhibition during nociceptive processing. Pain 2017, 158, 1046–1052. [Google Scholar] [CrossRef]
- Hughes, J.W.; Fresco, D.M.; Myerscough, R.; van Dulmen, M.H.; Carlson, L.E.; Josephson, R. Randomized controlled trial of mindfulness-based stress reduction for prehypertension. Psychosom. Med. 2013, 75, 721–728. [Google Scholar] [CrossRef] [Green Version]
- Innes, K.E.; Selfe, T.K.; Khalsa, D.S.; Kandati, S. Effects of meditation versus music listening on perceived stress, mood, sleep, and quality of life in adults with early memory loss: A pilot randomized controlled trial. J. Alzheimer’s Dis. 2016, 52, 1277–1298. [Google Scholar] [CrossRef] [Green Version]
- Chandran, S.; Raman, R.; Kishor, M.; Nandeesh, H.P. The effectiveness of mindfulness meditation in relief of symptoms of depression and quality of life in patients with gastroesophageal reflux disease. Indian J. Gastroenterol. 2019, 38, 29–38. [Google Scholar] [CrossRef]
- Serpa, J.G.; Taylor, S.L.; Tillisch, K. Mindfulness-based stress reduction (MBSR) reduces anxiety, depression, and suicidal ideation in veterans. Med. Care 2014, 52, S19–S24. [Google Scholar] [CrossRef]
- Im, B.; Kim, Y.; Chung, Y.; Hwang, S. Effects of scapular stabilization exercise on neck posture and muscle activation in individuals with neck pain and forward head posture. J. Phys. Ther. Sci. 2016, 28, 951–955. [Google Scholar] [CrossRef] [Green Version]
- Ağıl, A.; Abıke, F.; Daşkapan, A.; Alaca, R.; Tüzün, H. Short-term exercise approaches on menopausal symptoms, psychological health, and quality of life in postmenopausal women. Obstet. Gynecol. Int. 2010, 2010, 274261. [Google Scholar] [CrossRef] [Green Version]
- Kroenke, K.; Wu, J.; Bair, M.J.; Krebs, E.E.; Damush, T.M.; Tu, W. Reciprocal relationship between pain and depression: A 12-month longitudinal analysis in primary care. J. Pain 2011, 12, 964–973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demyttenaere, K.; Bonnewyn, A.; Bruffaerts, R.; Brugha, T.; De Graaf, R.; Alonso, J. Comorbid painful physical symptoms and depression: Prevalence, work loss, and help seeking. J. Affect. Disord. 2006, 92, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Marchand, W.R. Mindfulness-based stress reduction, mindfulness-based cognitive therapy, and Zen meditation for depression, anxiety, pain, and psychological distress. J. Psychiatr. Pract. 2012, 18, 233–252. [Google Scholar] [CrossRef] [PubMed]
- Sephton, S.E.; Salmon, P.; Weissbecker, I.; Ulmer, C.; Floyd, A.; Hoover, K.; Studts, J.L. Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: Results of a randomized clinical trial. Arthritis Rheum. 2007, 57, 77–85. [Google Scholar] [CrossRef]
- Grossman, P.; Tiefenthaler-Gilmer, U.; Raysz, A.; Kesper, U. Mindfulness training as an intervention for fibromyalgia: Evidence of postintervention and 3-year follow-up benefits in well-being. Psychother. Psychosom. 2007, 76, 226–233. [Google Scholar] [CrossRef] [Green Version]
- Kim, I.D.; Koo, C.D. A Study of Walking, Viewing and Fragrance-based Forest Therapy Programs Effect on Living Alone Adults’ Dementia Prevention. Korean J. Environ. Ecol. 2019, 33, 107–115. [Google Scholar] [CrossRef]
- Lee, S.A.; Lee, S.J.; Yook, Y.S.; Huh, Y.J.; Lee, M.G.; Choi, H.Y.; Lee, J.H. Effects of a mindfulness-based mind-body intervention program using marine resources on the improvement of sleep quality and mood symptoms in Korean female emotional labor workers: A pilot study. Sleep Med. Psychophysiol. 2018, 25, 58–67. [Google Scholar] [CrossRef]
| Variables | MTG (n = 12) | CG (n = 12) | t or Chi-Square (df) | p-Value | |
|---|---|---|---|---|---|
| Age (year) | 52.11 ± 10.34 | 53.40 ± 8.88 | −0.292 (22) * | 0.774 | |
| Height (cm) | 157.21 ± 4.23 | 156.14 ± 6.18 | 0.436 (22) * | 0.669 | |
| Weight (kg) | 57.18 ± 8.68 | 61.12 ± 9.62 | −0.934 (22) * | 0.364 | |
| BMI (kg/m2) | 23.14 ± 3.44 | 25.04 ± 3.41 | −1.204 (22) * | 0.245 | |
| Care period (month) | 24.44 ± 25.02 | 15.90 ± 17.47 | 0.871 (22) * | 0.396 | |
| Relationship | |||||
| Wife | 7 (58.30) | 6 (50.00) | 0.220 (3) # | 0.974 | |
| Grandmother | 1 (8.30) | 1 (8.30) | |||
| Daughter | 3 (25.00) | 4 (33.30) | |||
| Daughter-in-law | 1 (8.30) | 1 (8.30) |
| Variables | PRE | PI | FU | Source | F (df) | p | Partial η2 |
|---|---|---|---|---|---|---|---|
| VAS (mm) | |||||||
| Resting pain | |||||||
| MTG | 34.89 ± 9.96 | 10.11 ± 10.06 a,* | 13.78 ± 10.91 a,* | Time | 72.719 (1,22) | <0.001 | 0.81 |
| CG | 34.40 ± 6.79 | 25.50 ± 4.88 a | 33.50 ± 7.09 | Group | 10.487 (1,22) | 0.005 | 0.38 |
| d | 0.37 | 1.45 | 1.64 | T*G | 23.184 (1,22) | <0.001 | 0.58 |
| Movement pain | |||||||
| MTG | 51.33 ± 14.86 | 17.22 ± 9.72 a,* | 23.78 ± 7.40 a,* | Time | 24.952 (1,22) | <0.001 | 0.60 |
| CG | 46.40 ± 20.51 | 34.20 ± 17.74 | 39.10 ± 18.60 | Group | 2.250 (1,22) | 0.152 | 0.12 |
| d | 0.24 | 1.07 | 1.02 | T*G | 6.384 (1,22) | 0.004 | 0.27 |
| PPT (kg) | |||||||
| UT | |||||||
| MTG | 4.13 ± 2.29 | 4.67 ± 1.30 | 4.91 ± 1.46 | Time | 0.765 (1,22) | 0.473 | 0.04 |
| CG | 5.08 ± 1.81 | 5.29 ± 2.80 | 5.40 ± 2.56 | Group | 0.686 (1,22) | 0.419 | 0.04 |
| d | 0.36 | 0.26 | 0.21 | T*G | 0.136 (1,22) | 0.873 | 0.01 |
| LS | |||||||
| MTG | 3.92 ± 1.35 | 4.12 ± 1.04 | 4.89 ± 1.38 | Time | 0.213 (1,22) | 0.809 | 0.01 |
| CG | 4.83 ± 1.21 | 4.68 ± 1.28 | 4.26 ± 1.40 | Group | 0.384 (1,22) | 0.543 | 0.02 |
| d | 0.57 | 0.41 | 0.37 | T*G | 2.967 (1,22) | 0.065 | 0.15 |
| SC | |||||||
| MTG | 4.91 ± 2.22 | 4.89 ± 1.58 | 4.68 ± 1.05 | Time | 0.186 (1,22) | 0.831 | 0.01 |
| CG | 5.15 ± 1.17 | 4.93 ± 1.78 | 4.92 ± 1.93 | Group | 0.076 (1,22) | 0.786 | 0.00 |
| d | 0.10 | 0.02 | 0.14 | T*G | 0.046 (1,22) | 0.955 | 0.00 |
| Variables | PRE | PI | FU | Source | F (df) | p | Partial η2 |
|---|---|---|---|---|---|---|---|
| Upper part (cm) | |||||||
| MTG | 3.58 ± 0.47 | 2.88 ± 0.34 a | 2.83 ± 0.43 a,* | Time | 14.460 (1,22) | <0.001 | 0.46 |
| CG | 3.51 ± 0.65 | 3.16 ± 0.25 | 3.21 ± 0.23 | Group | 1.898 (1,22) | 0.186 | 0.10 |
| d | 0.10 | 0.74 | 0.82 | T*G | 2.169 (1,22) | 0.130 | 0.11 |
| Lower part (cm) | |||||||
| MTG | 8.39 ± 0.94 | 7.24 ± 0.61 a,* | 7.23 ± 1.20 a,* | Time | 7.672 (1,22) | 0.002 | 0.31 |
| CG | 8.49 ± 0.88 | 8.25 ± 0.71 | 8.34 ± 0.69 | Group | 5.341 (1,22) | 0.034 | 0.24 |
| d | 0.09 | 1.27 | 0.86 | T*G | 3.891 (1,22) | 0.030 | 0.19 |
| Variables | PRE | PI | FU | Source | F (df) | p | Partial η2 |
|---|---|---|---|---|---|---|---|
| UT stiffness (N/m) | |||||||
| MTG | 237.33 ± 29.74 | 223.11 ± 28.14 | 230.33 ± 18.46 | Time | 1.486 (1,22) | 0.241 | 0.08 |
| CG | 239.10 ± 22.42 | 240.20 ± 27.48 | 231.40 ± 20.83 | Group | 0.438 (1,22) | 0.517 | 0.03 |
| d | 0.05 | 0.50 | 0.05 | T*G | 1.871 (1,22) | 0.170 | 0.10 |
| UT Elasticity (logarithm) | |||||||
| MTG | 1.92 ± 0.35 | 1.84 ± 0.34 | 1.94 ± 0.28 | Time | 0.358 (1,22) | 0.702 | 0.02 |
| CG | 2.00 ± 0.58 | 1.91 ± 0.51 | 1.90 ± 0.44 | Group | 0.044 (1,22) | 0.837 | 0.00 |
| d | 0.14 | 0.13 | 0.11 | T*G | 0.195 (1,22) | 0.824 | 0.01 |
| LS stiffness (N/m) | |||||||
| MTG | 239.22 ± 31.16 | 240.00 ± 31.18 | 251.11 ± 25.48 | Time | 2.440 (1,22) | 0.102 | 0.13 |
| CG | 236.70 ± 18.57 | 243.60 ± 21.51 | 257.80 ± 35.89 | Group | 0.081 (1,22) | 0.779 | 0.01 |
| d | 0.07 | 0.10 | 0.19 | T*G | 0.180 (1,22) | 0.836 | 0.01 |
| LS Elasticity (logarithm) | |||||||
| MTG | 1.52 ± 0.22 | 1.50 ± 0.27 | 1.61 ± 0.25 | Time | 0.544 (1,22) | 0.585 | 0.03 |
| CG | 1.73 ± 0.24 | 1.70 ± 0.23 | 1.71 ± 0.23 | Group | 3.481 (1,22) | 0.079 | 0.17 |
| d | 0.74 | 0.64 | 0.34 | T*G | 0.580 (1,22) | 0.565 | 0.03 |
| SC stiffness (N/m) | |||||||
| MTG | 340.44 ± 63.91 | 366.22 ± 32.56 | 354.11 ± 45.43 | Time | 5.814 (1,22) | 0.007 | 0.26 |
| CG | 342.90 ± 31.90 | 381.50 ± 57.75 | 395.40 ± 51.53 | Group | 1.149 (1,22) | 0.299 | 0.06 |
| d | 0.04 | 0.29 | 0.71 | T*G | 1.602 (1,22) | 0.216 | 0.09 |
| SC Elasticity (logarithm) | |||||||
| MTG | 1.46 ± 0.12 | 1.47 ± 0.24 | 1.35 ± 0.22 | Time | 6.707 (1,22) | 0.004 | 0.28 |
| CG | 1.54 ± 0.11 | 1.53 ± 0.16 a | 1.38 ± 0.19 | Group | 0.652 (1,22) | 0.431 | 0.04 |
| d | 0.54 | 0.22 | 0.08 | T*G | 0.225 (1,22) | 0.799 | 0.01 |
| Variables | PRE | PI | FU | Source | F (df) | p | Partial η2 |
|---|---|---|---|---|---|---|---|
| Muscle strength (kg) | |||||||
| Grip strength (Rt) | |||||||
| MTG | 22.67 ± 2.77 | 24.28 ± 3.30 a | 24.06 ± 3.57 a | Time | 5.439 (1,22) | 0.009 | 0.24 |
| CG | 22.89 ± 5.13 | 23.51 ± 5.06 | 23.04 ± 5.27 | Group | 0.070 (1,22) | 0.794 | 0.00 |
| d | 0.05 | 0.16 | 0.20 | T*G | 1.792 (1,22) | 0.182 | 0.10 |
| Grip strength (Lt) | |||||||
| MTG | 19.66 ± 3.76 | 21.95 ± 3.77 a | 21.84 ± 3.77 a | Time | 5.979 (1,22) | 0.006 | 0.26 |
| CG | 21.81 ± 6.73 | 22.17 ± 5.92 | 21.24 ± 5.83 | Group | 0.064 (1,22) | 0.803 | 0.00 |
| d | 0.36 | 0.04 | 0.11 | T*G | 6.711 (1,22) | 0.003 | 0.28 |
| Pinch grip (Rt) | |||||||
| MTG | 6.62 ± 0.71 a | 7.50 ± 0.73 | 6.71 ± 1.02 | Time | 15.265 (1,22) | 0.000 | 0.47 |
| CG | 6.51 ± 0.99 a | 7.28 ± 1.57 | 6.66 ± 1.27 | Group | 0.073 (1,22) | 0.790 | 0.00 |
| d | 0.11 | 0.17 | 0.04 | T*G | 0.141 (1,22) | 0.869 | 0.01 |
| Pinch grip (Lt) | |||||||
| MTG | 6.29 ± 0.41 a | 6.86 ± 0.65 | 6.76 ± 0.65 | Time | 4.234 (1,22) | 0.023 | 0.20 |
| CG | 6.19 ± 0.92 | 6.21 ± 0.96 | 6.36 ± 0.98 | Group | 1.255 (1,22) | 0.278 | 0.07 |
| d | 0.13 | 0.69 | 0.42 | T*G | 2.530 (1,22) | 0.095 | 0.13 |
| Timed up and go (s) | |||||||
| MTG | 8.09 ± 1.17 a | 7.63 ± 0.96 | 7.38 ± 0.90 | Time | 4.196 (1,22) | 0.024 | 0.20 |
| CG | 8.02 ± 0.86 | 7.63 ± 0.55 | 7.79 ± 0.75 | Group | 0.103 (1,22) | 0.752 | 0.01 |
| d | 0.06 | 0.00 | 0.39 | T*G | 1.069 (1,22) | 0.355 | 0.06 |
| Variables | PRE | PI | FU | Source | F (df) | p | Partial η2 |
|---|---|---|---|---|---|---|---|
| K-WHOQOL-BREF (score) | |||||||
| Overall QOL & GH | |||||||
| MTG | 53.33 ± 15.81 | 65.56 ± 19.44 | 70.00 ± 14.14 a | Time | 5.443 (1,22) | 0.009 | 0.24 |
| CG | 58.00 ± 4.22 | 63.00 ± 4.83 | 61.00 ± 5.68 | Group | 0.328 (1,22) | 0.574 | 0.02 |
| d | 0.29 | 0.13 | 0.61 | T*G | 2.215 (1,22) | 0.125 | 0.12 |
| Physical health | |||||||
| MTG | 50.48 ± 12.29 | 68.25 ± 14.81 a | 68.89 ± 11.38 a | Time | 13.991 (1,22) | < 0.001 | 0.45 |
| CG | 59.43 ± 5.99 | 68.86 ± 8.13 | 60.57 ± 9.11 | Group | 0.012 (1,22) | 0.914 | 0.00 |
| d | 0.69 | 0.04 | 0.64 | T*G | 5.302 (1,22) | 0.010 | 0.24 |
| Psychological | |||||||
| MTG | 51.85 ± 13.45 | 65.18 ± 18.72 a | 65.93 ± 14.02 a | Time | 9.946 (1,22) | < 0.001 | 0.37 |
| CG | 55.67 ± 8.32 | 65.67 ± 8.47 | 60.00 ± 10.18 | Group | 0.013 (1,22) | 0.911 | 0.00 |
| d | 0.23 | 0.04 | 0.42 | T*G | 1.611 (1,22) | 0.215 | 0.09 |
| Social relationships | |||||||
| MTG | 51.85 ± 13.45 | 65.18 ± 18.72 | 65.93 ± 14.02 | Time | 1.051 (1,22) | 0.361 | 0.06 |
| CG | 55.67 ± 8.32 | 65.67 ± 8.47 | 60.00 ± 10.18 | Group | 1.217 (1,22) | 0.285 | 0.07 |
| d | 0.05 | 0.36 | 0.53 | T*G | 0.535 (1,22) | 0.591 | 0.03 |
| Environmental | |||||||
| MTG | 48.61 ± 9.36 | 62.78 ± 10.42 a | 63.06 ± 9.66 a | Time | 20.004 (1,22) | < 0.001 | 0.54 |
| CG | 55.25 ± 9.24 | 59.50 ± 12.35 | 60.25 ± 13.51 | Group | 0.002 (1,22) | 0.968 | 0.00 |
| d | 0.53 | 0.22 | 0.20 | T*G | 5.229 (1,22) | 0.010 | 0.24 |
| Total | |||||||
| MTG | 53.30 ± 10.48 | 66.13 ± 12.71 a | 67.50 ± 10.03 a | Time | 11.958 (1,22) | < 0.001 | 0.41 |
| CG | 58.07 ± 3.66 | 64.20 ± 5.22 | 60.90 ± 6.10 | Group | 72.719 (1,22) | < 0.001 | 0.81 |
| d | 0.42 | 0.12 | 0.63 | T*G | 24.952 (1,22) | < 0.001 | 0.60 |
| K-HDRS (score) | |||||||
| MTG | 17.56 ± 7.35 | 11.00 ± 1.22 a | 11.89 ± 2.03 | Time | 13.312 (1,22) | < 0.001 | 0.44 |
| CG | 17.60 ± 4.20 | 12.20 ± 1.75 a | 13.00 ± 1.94 | Group | 0.781 (1,22) | 0.389 | 0.04 |
| d | 0.01 | 0.69 | 0.45 | T*G | 0.131 (1,22) | 0.877 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, H.-J.; Kim, S.-H.; Cho, H.-Y.; Lee, J.-H. The Effects of Meditation with Stabilization Exercise in Marine Region on Pain, Tactile Sense, Muscle Characteristics and Strength, Balance, Quality of Life, and Depression in Female Family Caregivers of People with Severe Physical Disabilities: A Randomized Single-Blinded Controlled Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 6025. https://doi.org/10.3390/ijerph19106025
Shin H-J, Kim S-H, Cho H-Y, Lee J-H. The Effects of Meditation with Stabilization Exercise in Marine Region on Pain, Tactile Sense, Muscle Characteristics and Strength, Balance, Quality of Life, and Depression in Female Family Caregivers of People with Severe Physical Disabilities: A Randomized Single-Blinded Controlled Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(10):6025. https://doi.org/10.3390/ijerph19106025
Chicago/Turabian StyleShin, Ho-Jin, Sung-Hyeon Kim, Hwi-Young Cho, and Jae-Hon Lee. 2022. "The Effects of Meditation with Stabilization Exercise in Marine Region on Pain, Tactile Sense, Muscle Characteristics and Strength, Balance, Quality of Life, and Depression in Female Family Caregivers of People with Severe Physical Disabilities: A Randomized Single-Blinded Controlled Pilot Study" International Journal of Environmental Research and Public Health 19, no. 10: 6025. https://doi.org/10.3390/ijerph19106025
APA StyleShin, H.-J., Kim, S.-H., Cho, H.-Y., & Lee, J.-H. (2022). The Effects of Meditation with Stabilization Exercise in Marine Region on Pain, Tactile Sense, Muscle Characteristics and Strength, Balance, Quality of Life, and Depression in Female Family Caregivers of People with Severe Physical Disabilities: A Randomized Single-Blinded Controlled Pilot Study. International Journal of Environmental Research and Public Health, 19(10), 6025. https://doi.org/10.3390/ijerph19106025







