Abstract
Dust is a major component of fine particulate matter (PM2.5) in arid regions; therefore, concentrations of this pollutant in countries such as Kuwait exceed air quality standards. There is limited understanding on the impact and burden of high PM2.5 concentrations on morbidity in these countries. In this study, we explore the association of PM2.5 and the risk of respiratory hospital admissions in Kuwait. A time-series regression model was used to investigate daily variations in respiratory admissions and PM2.5 concentrations from 2010 to 2018. Due to the lack of historical air quality sampling in Kuwait, we used estimated daily PM2.5 levels from a hybrid PM2.5 prediction model. Individual and cumulative lag effects of PM2.5 over a 5-day period were estimated using distributed lag linear models. Associations were stratified by sex, age, and nationality. There were 218,749 total respiratory admissions in Kuwait during the study period. Results indicate that for every 10 μg/m3 increase in PM2.5, a 1.61% (95% CI = 0.87, 2.35%) increase in respiratory admissions followed over a 5-day cumulative lag. Our estimates show that a 10 μg/m3 reduction in average exposure will potentially avert 391 yearly respiratory admissions (95% CI = 211,571), with 265 fewer admissions among Kuwaitis (95% CI = 139,393) and 262 fewer admissions among children under 15 years of age (95% CI = 125,351). Different strata of the Kuwaiti population are vulnerable to respiratory hospitalization with short-term exposure to PM2.5, especially those under 15 years of age. The findings are informative for public health authorities in Kuwait and other dust-prone countries.
1. Introduction
Kuwait is well known for its desert climate, with dry, hot summers, scarce vegetation, and strong winds []. Countries with such unique weather conditions are prone to a considerable amount of dust and dust storms [,]. Because dust is a major component of ambient particulate matter with aerodynamic diameter less than 2.5 microns (PM2.5) in the region, concentrations of PM2.5 in Kuwait far exceed the World Health Organization (WHO) 24 h (15 μg/m3) and annual (5 μg/m3) air quality standards [,].
Exposure to particulate matter is associated with detrimental health effects such as mortality [,] and low birth weight in newborns [,].
Several studies found significant increases in the risk of respiratory hospital admissions across all age groups associated with high PM2.5 [,,,,]. Those with pre-existing respiratory conditions such as asthma are more susceptible, with an increase in asthma admissions associated with increases in PM2.5 concentrations [,,]. The extent to which we understand the impact and burden of high PM2.5 concentrations on morbidity in the country is limited.
To date, only two studies have assessed the health impacts of particulate pollution in Kuwait. The first, investigated the effects of particulate matter from dust storms on respiratory-related admissions in hospitals in Kuwait from January 1996 to December 2000 []. The study, however, only looked at exposure to particulate matter with aerodynamic diameter less than 10 microns (PM10). PM2.5 is rather more harmful than PM10 because fine particles can penetrate the lungs’ small airways and reach the alveoli as compared to large and coarse particles, which cannot penetrate deep into the lungs []. The second study assessed exposure to PM2.5 and its impact on cardiovascular and respiratory disease mortality and morbidity. The findings suggest that the proportion of excess cases of respiratory diseases attributable to PM2.5 exposure was higher than that of cardiovascular diseases []. PM2.5 exposure is shown to be a risk factor for respiratory disease morbidity in the country.
New studies are warranted to investigate the harmful effects of PM2.5 to contribute to the country’s environmental policies on air quality health assessments due to the ubiquitous nature of dust in the region and the associated regulatory challenges. Since there is a lack of historical air quality sampling and ground monitoring stations in Kuwait, assessment of the health impact of particulate matter exposure is lacking. To address this, we used PM2.5 prediction models to estimate average daily PM2.5 levels. According to Jing et al. [], this novel approach can be used in regions with limited monitoring networks. In this study, we examined the association between predicted PM2.5 and the risk of respiratory-related hospital admissions among different strata of the Kuwait population.
2. Materials and Methods
2.1. Admissions Data
Upon ethical approval from the Ministry of Health, we obtained daily respiratory-related hospital admissions data in Kuwait across 17 public hospitals for the period from 1 January 2010 to 31 December 2018, from the National Center for Health Information, Department of Vital Statistics, Ministry of Health, Kuwait. The cause of admission was classified based on the international classification of diseases version 10 (ICD-10) codes; J00–J99 used for total respiratory admissions and J45 for asthma admissions.
2.2. Environmental Data
We estimated daily PM2.5 levels in micrograms per cubic meter (μg/m3) using a hybrid PM2.5 prediction model. The detailed methodology can be found in Li et al. []. In brief, using machine learning methods and generalized additive mixed models combining visibility, satellite retrievals of aerosol optic depth, land use data, and ground-based observations, the model predicted PM2.5 levels in Iraq and Kuwait at a high spatial (1 × 1 km) and temporal (daily) resolution []. The model was evaluated with the 10-fold cross validation with an R2 value of 0.71. For each day, PM2.5 was averaged from all urban pixels in the country. The exposure data are available from the corresponding author (JL) upon reasonable request. Meteorological variables such as daily average temperature (°C) and relative humidity (%) were obtained from the Meteorological Department of the Directorate General of Civil Aviation for the same study period.
2.3. Study Design & Statistical Analysis
To assess the association between daily counts of respiratory admissions and daily PM2.5 exposure, we applied generalized linear models (GLMs) for a time-series structured data using Quasi-Poisson regression to account for overdispersion. The linearity of PM2.5 was initially assessed in generalized additive models (GAMs) by applying penalized splines. We then fitted a linear term for PM2.5 in the GLMs. Time was modeled with natural splines (7 degrees of freedom per calendar year) and a categorical variable for the day of the week [,]. To account for potential delayed effects, 3- and 5-day moving average were used for PM2.5. We also fitted distributed lag linear models (DLM) to estimate individual and cumulative lag effects of PM2.5 over a 5-day period. Temperature was modeled using distributed lag nonlinear models (DLNM); a natural spline with 3 degrees of freedom for the temperature exposure and a 7-day lag period and natural spline with 3 degrees of freedom equally spaced in the log scale for the lag basis. Relative humidity was modeled with natural spline with 3 degrees of freedom. The final model can be described as follows:
where E[Yi] is the expected count of total respiratory admissions on day i, PM2.5 refers to daily mean ambient PM2.5 concentrations with l moving average lag days, T is the temperature DLNM cross-basis function for t lag days, RH is relative humidity, DOW is day of the week, ns is a natural spline, and df is degrees of freedom.
We also estimated the burden of hospital admissions from PM2.5 exposure by calculating the potential admissions averted for every 10 μg/m3 reduction. We used the approach presented by Dominici, et al. [] and Krishna, et al. [], where attributable averted admissions are defined as (exp (β × ∆x) − 1) × N, where β being the coefficient for a 1 μg/m3 increase in PM2.5, ∆x being 10 μg/m3, and N being the total number of admissions in a defined time period. In an additional analysis, we investigated the impact of PM2.5 on asthma-only admissions. Analyses were carried out using R statistical software version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria) and dlnm package version 2.4.6.
3. Results
3.1. Summary Statistics
Over the 3294 days between 1 January 2010 and 31 December 2018, there were 218,749 total respiratory admissions in Kuwait. The highest mean admissions per day were found among males, Kuwaitis, and those under the age of 15. The median respiratory admissions per day were 66 (interquartile range [IQR] = 35) and the median PM2.5 exposure was 44 μg/m3 (IQR = 15.09). Summary statistics of all variables are provided in Table 1.

Table 1.
Descriptive statistics of the population and environmental exposures over the study period (1 January 2010 to 31 December 2018).
3.2. Regression Results
Table 2 shows the percentage increase in admission for every 10 μg/m3 increase in PM2.5 exposure for same-day exposure up to 5 days after exposure.

Table 2.
Increase in total respiratory admission for 10 μg/m3 increase in PM2.5 exposure for 0–5 lag days using distributed lag models and moving average of 3 and 5 days.
Table 3 and Figure 1 present increased admissions among the various strata examined over 5-day cumulative distributed lags. Overall, we observed a 0.6% (95% confidence intervals [CI] = 0.17, 1.03%) increase in respiratory admissions with every 10 μg/m3 increase in same-day PM2.5 exposure and a 1.61% (95% CI = 0.87, 2.35%) increase over a 5-day cumulative distributed lag. Moving average lagged effects for 3- and 5-days were significant, showing an increase in total admission of 1.32% (95% CI = 0.77, 1.87%) and 1.38% (95% CI = 0.7, 2.05%), respectively. Although the confidence intervals overlap, there was some heterogeneity in effect size across age groups with every 10 μg/m3 increase in exposure contributing to a 1.76% (95% CI = 0.84, 2.68%) increase in admissions among those under 15 years of age, and a 2.24% (95% CI = 0.6, 3.92%) increase in those above 65 years of age. The risk estimates were not statistically significant for the 15–64 age group. A significant association was observed in both males and females, with each 10 μg/m3 exposure increment contributing to 1.52% (95% CI = 0.66, 2.39%) and 1.72% (95% CI = 0.76, 2.69%) increase in admissions, respectively. Furthermore, Kuwaitis showed a higher risk of admission than non-Kuwaitis in total.

Table 3.
Sub-group analysis for the association between average PM2.5 and respiratory admissions over 0–5 cumulative days lag period using distributed lag models.
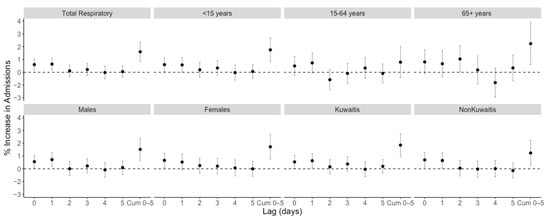
Figure 1.
Associations between delayed respiratory admission and PM2.5 exposure among different subgroups for distributed lag models up to 5 days lag. All models were adjusted for ambient temperature, relative humidity, long-term trends, and day of the week. Cum; cumulative.
Based on our in-depth subgroup analyses, stratifying the subpopulations by nationality, then by sex, then by age (Table 4), we found that Kuwaiti female children had the highest effect estimates. Non-Kuwaiti males showed a higher RR of admission than Kuwaiti males in total. Although nonsignificant, non-Kuwaiti females had the lowest risk of admission. As shown in Figure S1, Tables S1 and S2, results for asthma admissions were associated with a wide uncertainty (Supplementary Materials).

Table 4.
In-depth subgroup analysis for the association between average PM2.5 and respiratory admissions over 0–5 cumulative days lag period using distributed lag models.
3.3. Admissions Averted by Reducing Exposures
Table 5 shows the total respiratory admissions that can be averted for a 10 μg/m3 reduction in PM2.5 exposure in Kuwait. Our estimates show that a 10 μg/m3 reduction in average exposure may potentially reduce respiratory admissions by 391 (95% CI= 211, 571) patients each year.

Table 5.
Respiratory admissions potentially averted for 10 μg/m3 reduction in PM2.5 exposure in Kuwait.
4. Discussion
In this study, we were able to leverage statistical models to obtain a spatiotemporally resolved PM2.5 over a historical period in Kuwait that otherwise did not exist. We used this dataset to investigate the associations with respiratory-related hospital admissions. We estimate that a total of 391 respiratory admissions each year can be averted if PM2.5 levels in the country drop by 10 μg/m3. Overall, for every 10 μg/m3 increase in PM2.5, there is a 1.61% increase in total respiratory admissions over a 5-day cumulative distributed lag. Different strata of the Kuwait population are vulnerable to PM2.5 exposure, especially the elderly and those under 15 years of age.
Differences in PM2.5 impacts on the Kuwaiti population by age, sex, and nationality were investigated to determine the vulnerability of the population. Those aged 65 and over were especially susceptible to PM2.5 exposure, followed by those under 15 years of age. The strength of these associations is consistent with studies showing stronger impacts of PM2.5 on respiratory admissions among the elderly []. Adverse impacts on the elderly are expected based on the literature and are likely related to weakened immune system and decreased lung function within this age group [,,]. It is also important to note that respiratory diseases such as pneumonia, chronic obstructive pulmonary disease (COPD), and chest infections are more prevalent in this older age group, and PM2.5 exposure is likely contributing to larger effect estimates in the presence of these diseases [,,]. The other significant association was seen among the <15 age group, which is expected given that children’s lungs are not fully developed. Children breathe more air relative to body size than adults and are likely to spend more time outdoors, increasing their exposure to pollutants []. With regard to sex, a study exploring the differential impact of PM2.5 on respiratory outcomes for males and females in different counties in the USA found that PM2.5 exposure was associated with a higher relative increase in hospitalization for respiratory tract infections and asthma in women than in men [,]. Similarly, Shakerkhatibi, et al. [] reported that the odds ratio for females was 1.5 times higher than males for risk of respiratory admission due to PM2.5 exposure. We found Kuwaiti females to have a high risk of admission compared to males. The exact reason for these differences is unclear, but could be attributed to physiological, behavioral, and/or psychosocial determinants of health []. Possible differences in lifestyle between the sexes could result in differences in exposure patterns and, thus, result in this disparity []. The pathways through which PM2.5 exposure affects the health of men and women differently needs to be further explored.
As expected, non-Kuwaiti males exhibited a large relative risk of admissions. Non-Kuwaiti adult males are more vulnerable to higher ambient pollutant exposure given the outdoor nature of many migrant worker jobs such as construction and sanitation []. This is further supported by a previous study conducted in Kuwait on the impact of poor air quality on mortality that reported an increase in non-Kuwaiti male mortality rates associated with exposure to air pollution and dust storms []. This study, however, used visibility, a binary outcome, to describe adverse air quality, whereas in our study we used continuous PM2.5, which is more quantifiable and can provide better regulatory inference and allow for comparison across different studies. Our finding could be influenced by social factors related to access to healthcare, where Kuwaitis can utilize public hospital services for free, whereas non-Kuwaitis must pay a fee to be admitted and/or receive treatment. This likely played a role in potentially underestimating the risk of respiratory hospital admissions among the non-Kuwaiti subgroup. In Thalib and Al-Taiar’s [] paper investigating the impact of dust storms on respiratory hospital admissions in Kuwait, binary measures for exposure were employed (dust storm vs. non-dust storm days) for the period between 1996 to 2000. Our study used continuous PM2.5 measures instead and provided an analysis on hospital admissions using recent data from the past decade.
Overall, our findings are in line with previous studies conducted globally. A study in China reported a respiratory admission relative risk of 1.06 per 10 μg/m3 rise in exposure PM2.5 at lag 0–2 days []. A meta-analysis of 110 peer-reviewed time-series studies assessing associations between PM2.5 and daily mortality and hospital admissions concluded that a 10 μg/m3 increment in PM2.5 is associated with an increase in risk of admission for respiratory diseases by 0.96% [].
Particulate matter exposure impacts health negatively especially among individuals with pre-existing lung conditions. PM inhalation among respiratory patients is associated with pulmonary function decrements where reductions in forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC) are observed [,,,]. Research has also demonstrated that increased levels of particulate matter seem to increase symptoms of respiratory distress (i.e., wheezing and shortness of breath) and asthma medication use [,,,]. Furthermore, pollutants in the air are known to interact with airborne allergens, increasing the risk of atopic sensitization and exacerbation of respiratory disease symptoms [,]. When fine PM along with these allergens penetrate deep into the lungs, irritation is caused which induces alveolar inflammation that limits air flow and in turn results in acute respiratory episodes []. The impacts of acute PM inhalation pose a threat to the health of the population, especially vulnerable groups. Therefore, assessing the relationship between PM2.5 and respiratory outcomes is of optimum importance.
Limitations
Based on the literature review, we believe that this is the first study in the region to examine the association of PM2.5 with respiratory admissions. However, the study has a few limitations. The use of estimated daily mean PM2.5 measurements rather than direct measurements from monitoring stations in Kuwait is potentially associated with exposure measurement error. However, these PM2.5 prediction models ensure that there are no days with missing data. Although we believe that the PM2.5 prediction models had good predictive ability (R2 = 0.71), it is still less preferred than direct ground monitoring readings, as less measurement error in the exposure would occur had we measured PM2.5 continuously from ground stations for the study period. Despite this, the predictions are the best available data, since historical ground monitoring in Kuwait does not exist. Additionally, in this study, we assumed that all individuals in the population were exposed to PM2.5 at the same level, since we did not have address data for admitted patients. Moreover, for future directions, it would be valuable to examine hospital readmissions to assess their association with exposure to PM2.5 in the long-term. Finally, the findings of this study should be interpreted within the local context and population characteristics in Kuwait.
5. Conclusions
The present study is the first to explore the impact of PM2.5 exposures on daily respiratory admissions in Kuwait. Our analysis suggests that different strata of the Kuwaiti population are vulnerable to respiratory disease hospitalization when exposed to PM2.5 in the short-term, especially the elderly and those under 15 years of age. The results of the study highlight the importance of preventative care for Kuwait’s susceptible population to decrease the risk of respiratory complications during bad weather events. Potential warning systems can be put in place with air quality alerts to protect those who are vulnerable, especially children. In addition, with such information, hospitals would be able to predict increases in admissions and, thus, be better equipped to handle high volumes of emergency visits during days with higher PM levels. These findings contribute to the limited evidence related to the association between health and exposure to dust-dominant ambient PM2.5 in Kuwait and in the Middle East.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19105998/s1, Figure S1: Associations between delayed asthma admission and PM2.5 exposure among the total population for distributed lag models up to a 5-day lag. All models were adjusted for ambient temperature, relative humidity, long-term trends, and day of the week. Cum; cumulative. Table S1: Increase in total asthma admission for 10 μg/m3 increase in PM2.5 exposure for 0–5 lag days using distributed lag models and a moving average of 3 and 5 days. Table S2: Subgroup analysis for the association between average PM2.5 and asthma admissions over 0–5 cumulative days lag period using distributed lag models.
Author Contributions
Conceptualization, S.A., B.A. and A.A.-H.; methodology, J.L.; formal analysis, S.A. and B.A.; data collection, J.L. and H.A.; data curation, S.A.; writing—original draft preparation, S.A.; writing—review and editing, S.A., B.A., J.L., A.A.-H., J.G. and M.A.-Z.; supervision, B.A. and M.A.-Z. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Ministry of Health, Kuwait (3832, 6 May 2021).
Informed Consent Statement
Patient consent was waived due to the nature of data; the collection of data was not done specifically for this research. The acquired secondary data was de-identified and not coded, i.e., no names, ID numbers or codes were mentioned.
Data Availability Statement
Restrictions apply to the availability of these data. Data was obtained from the Kuwait Ministry of Health and are available, from the corresponding author S.A., with the permission of the Kuwait Ministry of Health.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Khalaf, F.; Al-Ajmi, D. Aeolian processes and sand encroachment problems in Kuwait. Geomorphology 1993, 6, 111–134. [Google Scholar] [CrossRef]
- Al-Awadhi, J.M.; Omar, S.A.; Misak, R.F. Land degradation indicators in Kuwait. Land Degrad. Dev. 2005, 16, 163–176. [Google Scholar] [CrossRef]
- Goudie, A.S. Desert dust and human health disorders. Environ. Int. 2014, 63, 101–113. [Google Scholar] [CrossRef] [PubMed]
- Alahmad, B.; Al-Hemoud, A.; Kang, C.-M.; Almarri, F.; Kommula, V.; Wolfson, J.M.; Bernstein, A.S.; Garshick, E.; Schwartz, J.; Koutrakis, P. A two-year assessment of particulate air pollution and sources in Kuwait. Environ. Pollut. 2021, 282, 117016. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. What Are the Who Air Quality Guidelines? Available online: https://www.who.int/news-room/feature-stories/detail/what-are-the-who-air-quality-guidelines#:~:text=The%20WHO%20Air%20quality%20guidelines%20are%20a%20set%20of%20evidence,the%20guidelines%20was%20in%201987 (accessed on 30 April 2022).
- Brunekreef, B.; Beelen, R.; Hoek, G.; Schouten, L.; Bausch-Goldbohm, S.; Fischer, P.; Armstrong, B.; Hughes, E.; Jerrett, M.; van den Brandt, P. Effects of long-term exposure to traffic-related air pollution on respiratory and cardiovascular mortality in the Netherlands: The NLCS-AIR study. Res. Rep. Health Eff. Inst. 2009, 139, 5–71. [Google Scholar]
- Shi, L.; Zanobetti, A.; Kloog, I.; Coull, B.A.; Koutrakis, P.; Melly, S.J.; Schwartz, J.D. Low-concentration PM2.5 and mortality: Estimating acute and chronic effects in a population-based study. Environ. Health Perspect. 2016, 124, 46–52. [Google Scholar] [CrossRef] [Green Version]
- Ibrahimou, B.; Salihu, H.; Gasana, J.; Owusu, H. Risk of low birth weight and very low birth weight from exposure to particulate matter (PM2.5) speciation metals during pregnancy. Gynecol. Obs. 2014, 4, 2161-0932. [Google Scholar]
- Wu, H.; Jiang, B.; Geng, X.; Zhu, P.; Liu, Z.; Cui, L.; Yang, L. Exposure to fine particulate matter during pregnancy and risk of term low birth weight in Jinan, China, 2014–2016. Int. J. Hyg. Environ. Health 2018, 221, 183–190. [Google Scholar] [CrossRef]
- Atkinson, R.W.; Kang, S.; Anderson, H.R.; Mills, I.C.; Walton, H.A. Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: A systematic review and meta-analysis. Thorax 2014, 69, 660–665. Available online: http://www.ncbi.nlm.nih.gov/pubmed/24706041 (accessed on 2 January 2019). [CrossRef] [Green Version]
- Bell, M.L.; Ebisu, K.; Leaderer, B.P.; Gent, J.F.; Lee, H.J.; Koutrakis, P.; Wang, Y.; Dominici, F.; Peng, R.D. Associations of PM2.5 Constituents and Sources with Hospital Admissions: Analysis of Four Counties in Connecticut and Massachusetts (USA) for Persons ≥ 65 Years of Age. Environ. Health Perspect. 2014, 122, 138–144. [Google Scholar] [CrossRef] [Green Version]
- Linares, C.; Diaz, J. Short-term effect of PM2.5 on daily hospital admissions in Madrid (2003–2005). Int. J. Environ. Health Res. 2010, 20, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Ostro, B.; Roth, L.; Malig, B.; Marty, M. The Effects of Fine Particle Components on Respiratory Hospital Admissions in Children. Environ. Health Perspect. 2009, 117, 475–480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tecer, L.H.; Alagha, O.; Karaca, F.; Tuncel, G.; Eldes, N. Particulate Matter (PM2.5, PM10–2.5, and PM10) and Children’s Hospital Admissions for Asthma and Respiratory Diseases: A Bidirectional Case-Crossover Study. J. Toxicol. Environ. Health Part A 2008, 71, 512–520. [Google Scholar] [CrossRef] [PubMed]
- E Gordian, M.; Ozkaynak, H.; Xue, J.; Morris, S.S.; Spengler, J.D. Particulate air pollution and respiratory disease in Anchorage, Alaska. Environ. Health Perspect. 1996, 104, 290–297. [Google Scholar] [CrossRef]
- Sheppard, L.; Levy, D.; Norris, G.; Larson, T.V.; Koenig, J.Q. Effects of ambient air pollution on nonelderly asthma hospital admissions in Seattle, Washington, 1987–1994. Epidemiology 1999, 10, 23–30. Available online: http://www.jstor.org/stable/3702178 (accessed on 20 June 2021). [CrossRef]
- Thalib, L.; Al-Taiar, A. Dust storms and the risk of asthma admissions to hospitals in Kuwait. Sci. Total Environ. 2012, 433, 347–351. [Google Scholar] [CrossRef]
- Guarnieri, M.; Balmes, J.R. Outdoor air pollution and asthma. Lancet 2014, 383, 1581–1592. [Google Scholar] [CrossRef] [Green Version]
- Al-Hemoud, A.; Gasana, J.; Al-Dabbous, A.; Alajeel, A.; Al-Shatti, A.; Behbehani, W.; Malak, M. Exposure levels of air pollution (PM2.5) and associated health risk in Kuwait. Environ. Res. 2019, 179, 108730. [Google Scholar] [CrossRef]
- Li, J.; Garshick, E.; Hart, J.E.; Li, L.; Shi, L.; Al-Hemoud, A.; Huang, S.; Koutrakis, P. Estimation of ambient PM2.5 in Iraq and Kuwait from 2001 to 2018 using machine learning and remote sensing. Environ. Int. 2021, 151, 106445. [Google Scholar] [CrossRef]
- Alahmad, B.; Shakarchi, A.; Alseaidan, M.; Fox, M. The effects of temperature on short-term mortality risk in Kuwait: A time-series analysis. Environ. Res. 2019, 171, 278–284. [Google Scholar] [CrossRef]
- Alahmad, B.; Shakarchi, A.F.; Khraishah, H.; Alseaidan, M.; Gasana, J.; Al-Hemoud, A.; Koutrakis, P.; Fox, M.A. Extreme temperatures and mortality in Kuwait: Who is vulnerable? Sci. Total Environ. 2020, 732, 139289. [Google Scholar] [CrossRef] [PubMed]
- Dominici, F.; Peng, R.D.; Bell, M.L.; Pham, L.; McDermott, A.; Zeger, S.L.; Samet, J.M. Fine Particulate Air Pollution and Hospital Admission for Cardiovascular and Respiratory Diseases. JAMA 2006, 295, 1127–1134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krishna, B.; Mandal, S.; Madhipatla, K.; Reddy, K.S.; Prabhakaran, D.; Schwartz, J.D. Daily nonaccidental mortality associated with short-term PM2.5 exposures in Delhi, India. Environ. Epidemiol. 2021, 5, e167. [Google Scholar] [CrossRef] [PubMed]
- Ren, Z.; Liu, X.; Liu, T.; Chen, D.; Jiao, K.; Wang, X.; Suo, J.; Yang, H.; Liao, J.; Ma, L. Effect of ambient fine particulates (PM2.5) on hospital admissions for respiratory and cardiovascular diseases in Wuhan, China. Respir. Res. 2021, 22, 128. [Google Scholar] [CrossRef]
- Peled, R. Air pollution exposure: Who is at high risk? Atmos. Environ. 2011, 45, 1781–1785. [Google Scholar] [CrossRef]
- Simon, A.K.; Hollander, G.A.; McMichael, A. Evolution of the immune system in humans from infancy to old age. Proc. R. Soc. B Biol. Sci. 2015, 282, 20143085. [Google Scholar] [CrossRef]
- Tao, Y.; Mi, S.; Zhou, S.; Wang, S.; Xie, X. Air pollution and hospital admissions for respiratory diseases in Lanzhou, China. Environ. Pollut. 2014, 185, 196–201. [Google Scholar] [CrossRef]
- Ito, K.; de Leon, S.F.; Lippmann, M. Associations between Ozone and Daily Mortality: Analysis and Meta-Analysis. Epidemiology 2005, 16, 446–457. Available online: http://www.jstor.org/stable/20486080 (accessed on 30 May 2021). [CrossRef]
- Lippmann, M.; Ito, K.; Nádas, A.; Burnett, R.T. Association of particulate matter components with daily mortality and morbidity in urban populations. Res. Rep. (Health Eff. Inst.) 2000, 95, 5–72. [Google Scholar]
- Gasana, J.; Dillikar, D.; Mendy, A.; Forno, E.; Vieira, E.R. Motor vehicle air pollution and asthma in children: A meta-analysis. Environ. Res. 2012, 117, 36–45. [Google Scholar] [CrossRef]
- Bell, M.L.; Son, J.-Y.; Peng, R.D.; Wang, Y.; Dominici, F. Brief Report, Ambient PM2.5 and Risk of Hospital Admissions Do Risks Differ for Men and Women? Epidemiology 2015, 26, 575–579. [Google Scholar] [CrossRef] [PubMed]
- Shakerkhatibi, M.; Seifipour, H.; Sabeti, Z.; Kahe, D.; Asghari Jafarabadi, M.; Zoroufchi Benis, K.; Hajaghazadeh, M. Correlation of ambient particulate matters (PM10, PM2.5) with respiratory hospital admissions: A case-crossover study in Urmia, Iran. Hum. Ecol. Risk Assess. Int. J. 2021, 27, 2184–2201. [Google Scholar] [CrossRef]
- Denton, M.; Prus, S.; Walters, V. Gender differences in health: A Canadian study of the psychosocial, structural and behavioural determinants of health. Soc. Sci. Med. 2004, 58, 2585–2600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- PACI. The Public Authority for Civil Information; Government of Kuwait: Kuwait City, Kuwait, 2019.
- Achilleos, S.; Al-Ozairi, E.; Alahmad, B.; Garshick, E.; Neophytou, A.M.; Bouhamra, W.; Yassin, M.F.; Koutrakis, P. Acute effects of air pollution on mortality: A 17-year analysis in Kuwait. Environ. Int. 2019, 126, 476–483. [Google Scholar] [CrossRef]
- Zhang, Y.; Ding, Z.; Xiang, Q.; Wang, W.; Huang, L.; Mao, F. Short-term effects of ambient PM1 and PM2.5 air pollution on hospital admission for respiratory diseases: Case-crossover evidence from Shenzhen, China. Int. J. Hyg. Environ. Health 2019, 224, 113418. [Google Scholar] [CrossRef] [PubMed]
- Delfino, R.J.; Staimer, N.; Tjoa, T.; Gillen, D.; Kleinman, M.T.; Sioutas, C.; Cooper, D. Personal and Ambient Air Pollution Exposures and Lung Function Decrements in Children with Asthma. Environ. Health Perspect. 2008, 116, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Hanley, Q.S.; Koenig, J.Q.; Larson, T.V.; Anderson, T.L.; Van Belle, G.; Rebolledo, V.; Covert, D.S.; Pierson, W.E. Response of Young Asthmatic Patients to Inhaled Sulfuric Acid. Am. Rev. Respir. Dis. 1992, 145, 326–331. [Google Scholar] [CrossRef]
- Jung, K.H.; Torrone, D.; Lovinsky-Desir, S.; Perzanowski, M.; Bautista, J.; Jezioro, J.R.; Hoepner, L.; Ross, J.; Perera, F.P.; Chillrud, S.N.; et al. Short-term exposure to PM2.5 and vanadium and changes in asthma gene DNA methylation and lung function decrements among urban children. Respir. Res. 2017, 18, 63. [Google Scholar] [CrossRef] [Green Version]
- Koenig, J.; Larson, T.; Hanley, Q.; Rebolledo, V.; Dumler, K.; Checkoway, H.; Wang, S.; Lin, D.; Pierson, W. Pulmonary Function Changes in Children Associated with Fine Particulate Matter. Environ. Res. 1993, 63, 26–38. [Google Scholar] [CrossRef]
- Karakatsani, A.; Analitis, A.; Perifanou, D.; Ayres, J.G.; Harrison, R.M.; Kotronarou, A.; Kavouras, I.; Pekkanen, J.; Hämeri, K.; Kos, G.P.; et al. Particulate matter air pollution and respiratory symptoms in individuals having either asthma or chronic obstructive pulmonary disease: A European multicentre panel study. Environ. Health 2012, 11, 75. [Google Scholar] [CrossRef] [Green Version]
- Williams, A.M.; Phaneuf, D.J.; Barrett, M.A.; Su, J.G. Short-term impact of PM2.5 on contemporaneous asthma medication use: Behavior and the value of pollution reductions. Proc. Natl. Acad. Sci. USA 2018, 116, 5246–5253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, J.; Zhong, T.; Zhu, Y.; Ge, D.; Lin, X.; Li, Q. Effects of particulate matter (PM) on childhood asthma exacerbation and control in Xiamen, China. BMC Pediatr. 2019, 19, 194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baldacci, S.; Maio, S.; Cerrai, S.; Sarno, G.; Baïz, N.; Simoni, M.; Annesi-Maesano, I.; Viegi, G. Allergy and asthma: Effects of the exposure to particulate matter and biological allergens. Respir. Med. 2015, 109, 1089–1104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heinrich, J.; Hoelscher, B.; Wjst, M.; Ritz, B.; Cyrys, J.; Wichmann, H. Respiratory diseases and allergies in two polluted areas in East Germany. Environ. Health Perspect. 1999, 107, 53–62. [Google Scholar] [CrossRef]
- Gavett, S.H.; Koren, H.S. The Role of Particulate Matter in Exacerbation of Atopic Asthma. Int. Arch. Allergy Immunol. 2001, 124, 109–112. [Google Scholar] [CrossRef]
- Seaton, A.; Godden, D.; MacNee, W.; Donaldson, K. Particulate air pollution and acute health effects. Lancet 1995, 345, 176–178. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).