Evaluation of the Effect of Supervised Group Exercise on Self-Reported Sleep Quality in Pregnant Women with or at High Risk of Depression: A Secondary Analysis of a Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
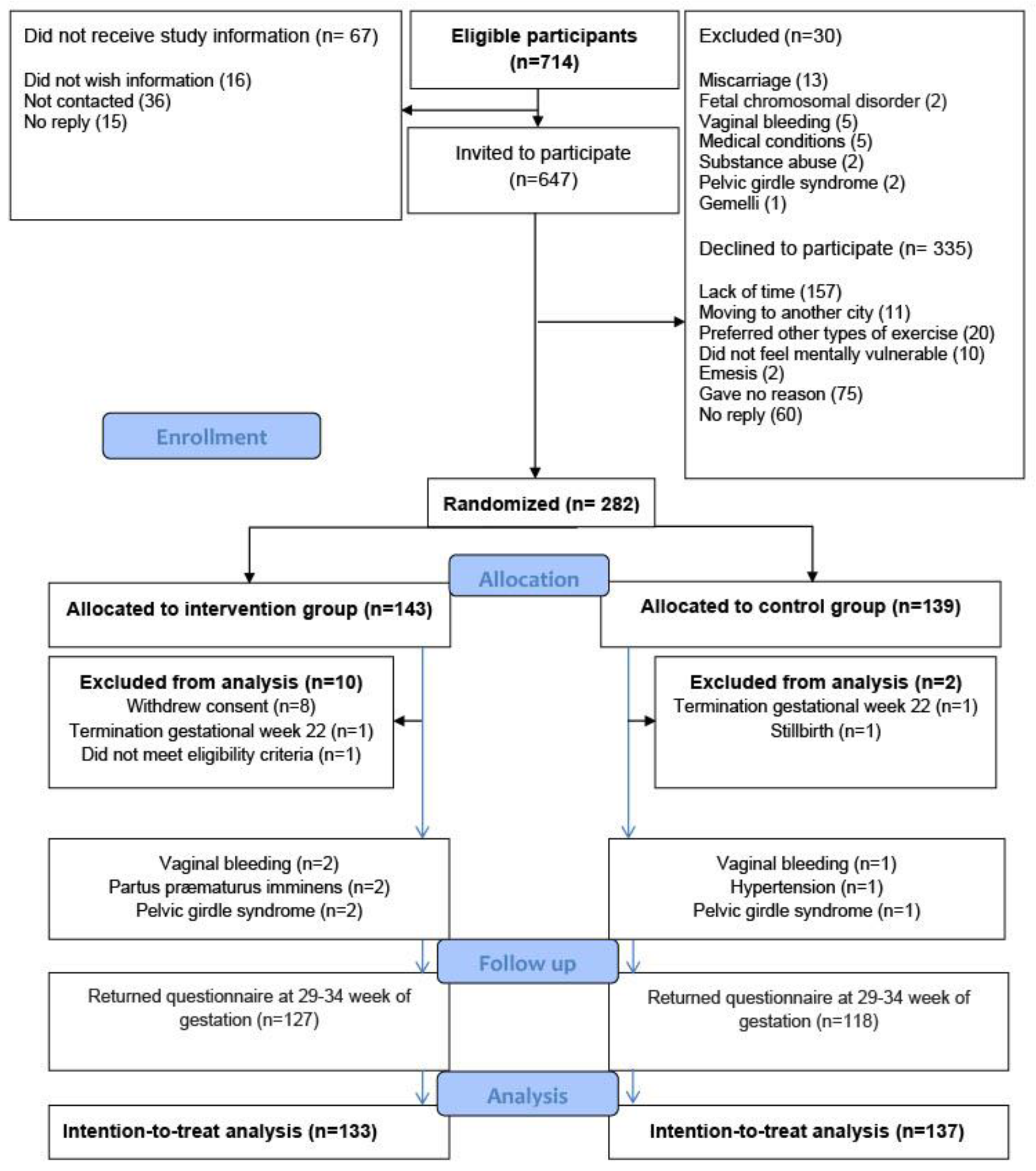
2.1. Study Design
2.2. Intervention Group
2.3. Control Group
2.4. Outcomes
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Response Rate, Adherence to Intervention, and Amount of Weekly Exercise
3.3. Intention-to-Treat Analysis
3.4. Per Protocol Analysis
3.5. Association between Subjective Sleep Quality and Psychological Well-Being in the Total Study Population
4. Discussion
4.1. Strengths and Limitations
4.1.1. Strengths
4.1.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chattu, V.K.; Manzar, M.D.; Kumary, S.; Burman, D.; Spence, D.W.; Pandi-Perumal, S.R. The Global Problem of Insufficient Sleep and Its Serious Public Health Implications. Healthcare 2018, 7, 1. [Google Scholar] [CrossRef] [Green Version]
- Lehrer, S.; Green, S.; Ramanathan, L.; Rosenzweig, K.E. Insufficient sleep associated with increased breast cancer mortality. Sleep Med. 2013, 14, 469. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; Miller, M.A. Sleep and Cardio-Metabolic Disease. Curr. Cardiol. Rep. 2017, 19, 110. [Google Scholar] [CrossRef] [Green Version]
- Grandner, M.A.; Seixas, A.; Shetty, S.; Shenoy, S. Sleep Duration and Diabetes Risk: Population Trends and Potential Mechanisms. Curr. Diabetes Rep. 2016, 16, 106. [Google Scholar] [CrossRef] [Green Version]
- Soehner, A.M.; Kaplan, K.A.; Harvey, A.G. Prevalence and clinical correlates of co-occurring insomnia and hypersomnia symptoms in depression. J. Affect. Disord. 2014, 167, 93–97. [Google Scholar] [CrossRef] [Green Version]
- Zhai, L.; Zhang, H.; Zhang, D. Sleep Duration and Depression among Adults: A Meta-Analysis of Prospective Studies. Depress. Anxiety 2015, 32, 664–670. [Google Scholar] [CrossRef]
- Khazaie, H.; Zakiei, A.; McCall, W.V.; Noori, K.; Rostampour, M.; Bahmani, D.S.; Brand, S. Relationship between Sleep Problems and Self-Injury: A Systematic Review. Behav. Sleep Med. 2020, 19, 689–704. [Google Scholar] [CrossRef]
- Roth, T.; Coulouvrat, C.; Hajak, G.; Lakoma, M.D.; Sampson, N.A.; Shahly, V.; Shillington, A.; Stephenson, J.J.; Walsh, J.K.; Kessler, R.C. Prevalence and Perceived Health Associated with Insomnia Based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition Criteria: Results from the America Insomnia Survey. Biol. Psychiatry 2011, 69, 592–600. [Google Scholar] [CrossRef]
- Sedov, I.D.; Cameron, E.E.; Madigan, S.; Tomfohr-Madsen, L.M. Sleep quality during pregnancy: A meta-analysis. Sleep Med. Rev. 2017, 38, 168–176. [Google Scholar] [CrossRef]
- Bourjeily, G. Sleep disorders in pregnancy. Obstet. Med. 2009, 2, 100–106. [Google Scholar] [CrossRef]
- Sharma, S.K.; Nehra, A.; Sinha, S.; Soneja, M.; Sunesh, K.; Sreenivas, V.; Vedita, D. Sleep disorders in pregnancy and their association with pregnancy outcomes: A prospective observational study. Sleep Breath 2015, 20, 87–93. [Google Scholar] [CrossRef]
- Naghi, I.; Keypour, F.; Ahari, S.B.; Tavalai, S.A.; Khak, M. Sleep disturbance in late pregnancy and type and duration of labour. J. Obstet. Gynaecol. 2011, 31, 489–491. [Google Scholar] [CrossRef]
- González-Mesa, E.; Cuenca-Marín, C.; Suarez-Arana, M.; Tripiana-Serrano, B.; Ibrahim-Díez, N.; Gonzalez-Cazorla, A.; Blasco-Alonso, M. Poor sleep quality is associated with perinatal depression. A systematic review of last decade scientific literature and meta-analysis. JPME 2019, 47, 689–703. [Google Scholar] [CrossRef]
- Okun, M.L.; Mancuso, R.A.; Hobel, C.J.; Schetter, C.D.; Coussons-Read, M. Poor sleep quality increases symptoms of depression and anxiety in postpartum women. J. Behav. Med. 2018, 41, 703–710. [Google Scholar] [CrossRef]
- Sedov, I.D.; Goodman, S.H.; Tomfohr-Madsen, L.M. Insomnia Treatment Preferences During Pregnancy. J. Obstet. Gynecol. Neonatal Nurs. 2017, 46, e95–e104. [Google Scholar] [CrossRef]
- Miller, M.A.; Mehta, N.; Clark-Bilodeau, C.; Bourjeily, G. Sleep Pharmacotherapy for Common Sleep Disorders in Pregnancy and Lactation. Chest 2019, 157, 184–197. [Google Scholar] [CrossRef] [Green Version]
- Kelley, G.A.; Kelley, K.S. Exercise and sleep: A systematic review of previous meta-analyses. J. Evid.-Based Med. 2017, 10, 26–36. [Google Scholar] [CrossRef]
- Kovacevic, A.; Mavros, Y.; Heisz, J.J.; Singh, M.A.F. The effect of resistance exercise on sleep: A systematic review of randomized controlled trials. Sleep Med. Rev. 2018, 39, 52–68. [Google Scholar] [CrossRef]
- Lederman, O.; Ward, P.B.; Firth, J.; Maloney, C.; Carney, R.; Vancampfort, D.; Stubbs, B.; Kalucy, M.; Rosenbaum, S. Does exercise improve sleep quality in individuals with mental illness? A systematic review and meta-analysis. J. Psychiatr. Res. 2018, 109, 96–106. [Google Scholar] [CrossRef] [Green Version]
- Kryger, M.H.; Roth, T.; Dement, W.C. Principles and Practice of Sleep Medicine; Elsevier/Saunders: Philadelphia, PA, USA, 2005. [Google Scholar]
- Herring, M.P.; Monroe, D.C.; Gordon, B.R.; Hallgren, M.; Campbell, M.J. Acute Exercise Effects among Young Adults with Analogue Generalized Anxiety Disorder. Med. Sci. Sports Exerc. 2019, 51, 962–969. [Google Scholar] [CrossRef]
- Broberg, L.; Ersbøll, A.S.; Backhausen, M.G.; Damm, P.; Tabor, A.; Hegaard, H.K. Compliance with national recommendations for exercise during early pregnancy in a Danish cohort. BMC Pregnancy Childbirth 2015, 15, 317. [Google Scholar] [CrossRef] [Green Version]
- Wagnild, J.M.; Pollard, T. “Sit Yourself Down”: Women’s Experiences of Negotiating Physical Activity During Pregnancy. Qual. Health Res. 2020, 30, 1072–1082. [Google Scholar] [CrossRef]
- Yang, S.-Y.; Lan, S.-J.; Yen, Y.-Y.; Hsieh, Y.-P.; Kung, P.-T.; Lan, S.-H. Effects of Exercise on Sleep Quality in Pregnant Women: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Asian Nurs. Res. 2020, 14, 1–10. [Google Scholar] [CrossRef]
- Field, T.; Diego, M.; Delgado, J.; Medina, L. Tai chi/yoga reduces prenatal depression, anxiety and sleep disturbances. Complement. Ther. Clin. Pract. 2012, 19, 6–10. [Google Scholar] [CrossRef] [Green Version]
- Broberg, L.; Backhausen, M.; Damm, P.; Bech, P.; Tabor, A.; Hegaard, H.K. Effect of supervised exercise in groups on psychological well-being among pregnant women at risk of depression (the EWE Study): Study protocol for a randomized controlled trial. Trials 2017, 18, 210. [Google Scholar] [CrossRef] [Green Version]
- Broberg, L.; Tabor, A.; Rosthøj, S.; Backhausen, M.; Frokjaer, V.G.; Damm, P.; Hegaard, H.K. Effect of supervised group exercise on psychological well-being among pregnant women with or at high risk of depression (the EWE Study): A randomized controlled trial. Acta Obstet. Gynecol. Scand. 2020, 100, 129–138. [Google Scholar] [CrossRef]
- American Psychiatric Association (Ed.) Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- The Danish Health and medicines Authority. Recommendations for Prenatal Care; Copenhagen Second Edition; The Danish Health and Medicines Authority: Copenhagen, Denmark, 2013. [Google Scholar]
- Borg, G. Borg’s Perceived Exertion and Pain Scales; Human Kinetics: Champaign, IL, USA, 1998; Volume 1998. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Qiu-Yue, Z.; Gelaye, B.; Zhong, Q.-Y.; Enquobahrie, D.A.; Frederick, I.O.; Williams, M.A. Construct validity and factor structure of the Pittsburgh Sleep Quality Index among pregnant women in a Pacific-Northwest cohort. Sleep Breath 2016, 20, 293–301. [Google Scholar] [CrossRef] [Green Version]
- Løppenthin, K.; Esbensen, B.A.; Jennum, P.; Østergaard, M.; Tolver, A.; Thomsen, T.; Midtgaard, J. Sleep quality and correlates of poor sleep in patients with rheumatoid arthritis. Clin. Rheumatol. 2015, 34, 2029–2039. [Google Scholar] [CrossRef]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- Van Buuren, S. Flexible Imputation of Missing Data, 2nd ed.; CRC Press, Chapman & Hall: Boca Raton, FL, USA, 2018. [Google Scholar]
- Guideline on Adjustment for Baseline Covariates in Clinical Trials. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-adjustment-baseline-covariates-clinical-trials_en.pdf (accessed on 26 February 2015).
- Liu, G.F.; Lu, K.; Mogg, R.; Mallick, M.; Mehrotra, D.V. Should baseline be a covariate or dependent variable in analyses of change from baseline in clinical trials? Stat. Med. 2009, 28, 2509–2530. [Google Scholar] [CrossRef]
- Wang, C.; Paik, M.C. A Weighting Approach for GEE Analysis with Missing Data. Commun. Stat.-Theory Methods 2011, 40, 2397–2411. [Google Scholar] [CrossRef]
- Cepeda, M.S.; Stang, P.; Blacketer, C.; Kent, J.M.; Wittenberg, G.M. Clinical Relevance of Sleep Duration: Results from a Cross-Sectional Analysis Using NHANES. J. Clin. Sleep Med. 2016, 12, 813–819. [Google Scholar] [CrossRef] [Green Version]
- Kredlow, M.A.; Capozzoli, M.C.; Hearon, B.A.; Calkins, A.W.; Otto, M.W. The effects of physical activity on sleep: A meta-analytic review. J. Behav. Med. 2015, 38, 427–449. [Google Scholar] [CrossRef]
- Baron, K.G.; Reid, K.J.; Zee, P.C. Exercise to Improve Sleep in Insomnia: Exploration of the Bidirectional Effects. J. Clin. Sleep Med. 2013, 9, 819–824. [Google Scholar] [CrossRef]
- Boutron, I.; Altman, D.G.; Moher, D.; Schulz, K.F.; Ravaud, P.; for the CONSORT NPT Group. CONSORT Statement for Randomized Trials of Nonpharmacologic Treatments: A 2017 Update and a CONSORT Extension for Nonpharmacologic Trial Abstracts. Ann. Intern. Med. 2017, 167, 40–47. [Google Scholar] [CrossRef]
- Christian, L.M.; Carroll, J.E.; Porter, K.; Hall, M.H. Sleep quality across pregnancy and postpartum: Effects of parity and race. Sleep Health 2019, 5, 327–334. [Google Scholar] [CrossRef]
- Vuori, I.; Urponen, H.; Hasan, J.; Partinen, M. Epidemiology of exercise effects on sleep. Acta Physiol. Scand. Suppl. 1988, 574, 3–7. [Google Scholar]
- Kamysheva, E.; Skouteris, H.; Wertheim, E.H.; Paxton, S.J.; Milgrom, J. A prospective investigation of the relationships among sleep quality, physical symptoms, and depressive symptoms during pregnancy. J. Affect. Disord. 2010, 123, 317–320. [Google Scholar] [CrossRef]
- Calcagni, S.C.; Bei, B.; Milgrom, J.; Trinder, J. The Relationship between Sleep and Mood in First-Time and Experienced Mothers. Behav. Sleep Med. 2012, 10, 167–179. [Google Scholar] [CrossRef]
- Coble, P.A.; Reynolds, C.F.; Kupfer, D.J.; Houck, P.R.; Day, N.L.; Giles, D.E. Childbearing in women with and without a history of affective disorder. II. Electroencephalographic sleep. Compr. Psychiatry 1994, 35, 215–224. [Google Scholar] [CrossRef]
- Park, E.M.; Meltzer-Brody, S.; Stickgold, R. Poor sleep maintenance and subjective sleep quality are associated with postpartum maternal depression symptom severity. Arch. Women’s Ment. Health 2013, 16, 539–547. [Google Scholar] [CrossRef] [Green Version]
- Okun, M.L.; Kiewra, K.; Luther, J.F.; Wisniewski, S.; Wisner, K. Sleep disturbances in depressed and nondepressed pregnant women. Depress. Anxiety 2011, 28, 676–685. [Google Scholar] [CrossRef] [Green Version]
- Dennis, C.-L.; Ross, L. Relationships Among Infant Sleep Patterns, Maternal Fatigue, and Development of Depressive Symptomatology. Birth 2005, 32, 187–193. [Google Scholar] [CrossRef]
- Bell, M.L.; Fiero, M.; Horton, N.J.; Hsu, C.-H. Handling missing data in RCTs; a review of the top medical journals. BMC Med. Res. Methodol. 2014, 14, 118. [Google Scholar] [CrossRef] [Green Version]
- Stremler, R.; McMurray, J.; Brennenstuhl, S. Self-Reported Sleep Quality and Actigraphic Measures of Sleep in New Mothers and the Relationship to Postpartum Depressive Symptoms. Behav. Sleep Med. 2019, 18, 396–405. [Google Scholar] [CrossRef]
- Muggli, E.; Curd, H.; Nagle, C.; Forster, D.; Halliday, J. Engaging pregnant women in observational research: A qualitative exploratory study. BMC Pregnancy Childbirth 2018, 18, 334. [Google Scholar] [CrossRef]
- McCambridge, J.; Kypri, K.; Elbourne, D. In randomization we trust? There are overlooked problems in experimenting with people in behavioral intervention trials. J. Clin. Epidemiol. 2013, 67, 247–253. [Google Scholar] [CrossRef] [Green Version]

| Characteristics | Intervention Group n = 143 | Control Group n = 139 | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Maternal age, years | 31.9 | 3.8 | 31.7 | 3.9 |
| Body mass index, kg/m2 | 22.8 | 3.4 | 22.7 | 3.6 |
| Sleep quality, PSQI | 6.16 | 2.8 | 6.37 | 3.1 |
| Psychological well-being, WHO-5 | 54.4 | 14.8 | 56.0 | 16.4 |
| n | Percentage | N | Percentage | |
| WHO-5 ≤ 50 | 55 | 38.7 | 42 | 30.7 |
| WHO-5 > 50 | 87 | 61.3 | 95 | 69.3 |
| Nulliparous | 107 | 74.8 | 100 | 71.9 |
| Living with partner | 137 | 95.8 | 132 | 95.0 |
| Educational level | ||||
| Advanced degree | 72 | 50.3 | 74 | 53.2 |
| 3–4 years higher education | 47 | 32.9 | 40 | 28.8 |
| 1–2 years higher education | 9 | 6.3 | 5 | 3.6 |
| Skilled worker | 4 | 2.8 | 8 | 5.8 |
| Compulsory education | 11 | 7.7 | 10 | 7.2 |
| Occupation | ||||
| Employed | 96 | 67.1 | 88 | 63.3 |
| Unemployed | 19 | 13.3 | 16 | 11.5 |
| Student | 24 | 16.8 | 29 | 20.9 |
| Other † | 4 | 2.8 | 6 | 4.3 |
| Smoking before pregnancy | 26 | 18.2 | 21 | 15.1 |
| Smoking in early pregnancy | 2 | 1.4 | 0 | 0 |
| Physical activity ≥ 3.5 h a week before pregnancy * | 115 | 80.4 | 105 | 75.5 |
| Chronic disorders ** | 26 | 18 | 19 | 14 |
| History of depression and anxiety | ||||
| Depression within the last 10 years | 44 | 31 | 39 | 28 |
| Anxiety within the last 10 years | 38 | 26 | 42 | 30 |
| Comorbid depression and anxiety within the last 10 years | 61 | 43 | 58 | 42 |
| Antidepressants three months prior to conception and/or during pregnancy | 30 | 21 | 32 | 23 |
| Sleep Parameters | Baseline | Post-Intervention | Eight Weeks pp | |||||
|---|---|---|---|---|---|---|---|---|
| 17–22 wg | 29–34 wg | |||||||
| IG | CG | IG | CG | p | IG | CG | p | |
| Global score, mean (CI) | 6.16 (5.66–6.66) | 6.37 (5.87–6.87) | 6.56 (6.05–7.07) | 7.00 (6.47–7.53) | 0.2 | 7.69 (7.14–8.25) | 7.61 (6.99–8.22) | 0.80 |
| Global score > 5, % (n) | 57.1 (76) | 58.8 (80) | 56.8 (71) | 64.1 (75) | 0.24 | 78.6 (77) | 78.3 (65) | 0.97 |
| Component 1 Subjective sleep quality, mean (CI) | 1.38 (1.02–1.26) | 1.21 (1.09–1.33) | 1.2 (1.08–1.34) | 1.34 (1.21–1.47) | 0.2 | 1.43 (1.29–1.58) | 1.38 (1.21–1.47) | 0.50 |
| Subjective sleep quality, very or fairly bad, % (n) | 30.8 (41) | 31.6 (43) | 30.4 (38) | 41.9 (49) | 0.06 | 36.7 (36) | 41.0 (34) | 0.50 |
| mean (CI) | mean (CI) | mean (CI) | mean (CI) | mean (CI) | mean (CI) | |||
| Component 2 Sleep latency | 1.02 (0.87–1.17) | 1.13 (0.98–1.28) | 0.85 (0.69–1.02) | 1.02 (0.86–1.19) | 0.28 | 0.48 (0.33–0.63) | 0.63 (0.47–0.78) | 0.25 |
| Component 3 Sleep duration | 0.64 (0.50–0.77) | 0.65 (0.52–0.78) | 0.77 (0.63–0.92) | 0.95 (0.80–1.10) | 0.06 | 1.58 (1.42–1.75) | 1.54 (1.37–1.72) | 0.73 |
| Component 4 Habitual sleep efficiency | 0.66 (0.51–0.82) | 0.76 (0.61–0.91) | 0.91 (0.73–1.09) | 1.09 (0.90–1.27) | 0.26 | 2.0 (1.81–2.21) | 1.70 (1.49–1.92) | 0.04 |
| Component 5 Sleep disturbances | 1.51 (1.42–1.61) | 1.49 (1.40–1.59) | 1.62 (1.52–1.72) | 1.64 (1.54–1.74) | 0.68 | 1.14 (1.03–1.25) | 1.20 (1.09–1.32) | 0.38 |
| Component 6 Use of sleeping medication | 0.01 (−0.03–0.04) | 0.06 (−0.03–0.12) | 0.12 (0.04–0.19) | 0.04 (−0.04–0.12) | 0.14 | 0.12 (0.02–0.22) | 0.10 (−0.01–0.21) | 0.69 |
| Component 7 Daytime dysfunction | 1.18 (1.06–1.30) | 1.07 (0.96–1.18) | 1.07 (0.95–1.18) | 0.95 (0.83–1.06) | 0.29 | 0.91 (0.78–1.05) | 1.05 (0.91–1.20) | 0.07 |
| WHO ≤ 50 | WHO > 50 | p Value | WHO ≤ 50 | WHO > 50 | p Value | |||
|---|---|---|---|---|---|---|---|---|
| Baseline | 75.2 (65.3–83) | 47.3 (39.9–54.8) | <0.0001 | 7.82 (7.26–8.38) | 5.42 (5.02–5.82) | <0.0001 | ||
| 29–34 wg | PSQI > 5 | 70.3 (59.1–79.4) | 55.6 (47.9–63) | 0.03 | PSQI | 7.72 (7.02–8.41) | 6.30 (5.82–6.78) | <0.0001 |
| % (CI) | global score | |||||||
| mean (CI) | ||||||||
| 8 wk pp | 83.7 (71.6–91.3) | 75.8 (67.5–82.6) | 0.24 | 8.25 (7.51–9.00) | 7.41 (6.90–7.91) | <0.0001 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Broberg, L.; Damm, P.; Frokjaer, V.G.; Rosthøj, S.; de Wolff, M.G.; Høgh, S.; Tabor, A.; Hegaard, H.K. Evaluation of the Effect of Supervised Group Exercise on Self-Reported Sleep Quality in Pregnant Women with or at High Risk of Depression: A Secondary Analysis of a Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 5954. https://doi.org/10.3390/ijerph19105954
Broberg L, Damm P, Frokjaer VG, Rosthøj S, de Wolff MG, Høgh S, Tabor A, Hegaard HK. Evaluation of the Effect of Supervised Group Exercise on Self-Reported Sleep Quality in Pregnant Women with or at High Risk of Depression: A Secondary Analysis of a Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(10):5954. https://doi.org/10.3390/ijerph19105954
Chicago/Turabian StyleBroberg, Lotte, Peter Damm, Vibe G. Frokjaer, Susanne Rosthøj, Mie Gaarskjaer de Wolff, Stinne Høgh, Ann Tabor, and Hanne Kristine Hegaard. 2022. "Evaluation of the Effect of Supervised Group Exercise on Self-Reported Sleep Quality in Pregnant Women with or at High Risk of Depression: A Secondary Analysis of a Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 10: 5954. https://doi.org/10.3390/ijerph19105954
APA StyleBroberg, L., Damm, P., Frokjaer, V. G., Rosthøj, S., de Wolff, M. G., Høgh, S., Tabor, A., & Hegaard, H. K. (2022). Evaluation of the Effect of Supervised Group Exercise on Self-Reported Sleep Quality in Pregnant Women with or at High Risk of Depression: A Secondary Analysis of a Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(10), 5954. https://doi.org/10.3390/ijerph19105954







