Emergency Medical Services Calls Analysis for Trend Prediction during Epidemic Outbreaks: Interrupted Time Series Analysis on 2020–2021 COVID-19 Epidemic in Lazio, Italy
Abstract
:1. Introduction
1.1. Background and Rationale
1.1.1. Health Emergency Systems in Italy and ARES 118 in the Lazio Region
1.1.2. COVID-19 Outbreak in the Lazio Region during Years 2020–2021
1.1.3. COVID-19 Outbreaks and EMS Calls
1.2. Objectives
2. Methods
2.1. Study Design
2.2. Setting and Population
2.3. Variables and Data Sources
- Daily COVID-19 incidence;
- Daily COVID-19 admissions;
- Daily COVID-19 admissions in Intensive Care Units (ICU);
- Daily deaths among COVID-19 patients;
- Daily toll-free calls to EMS.
2.4. Statistical Analysis
2.4.1. Epidemic Trend
2.4.2. Trend of EMS Calls
2.4.3. Regression Analysis
2.4.4. Ex-Post Data Correction
2.4.5. Validation
2.4.6. Post Hoc Analysis: Forecasting Power
- (A)
- It must have current value as starting value for estimation (imput);
- (B)
- It must be a function of current fluctuation;
- (C)
- The two variables must be linked by the proposed regression model.
- (D)
- Its output would be the expected value of after 7 days,.
2.5. Privacy, Ethical Committee Approval and Informed Consent
3. Results
3.1. Participants
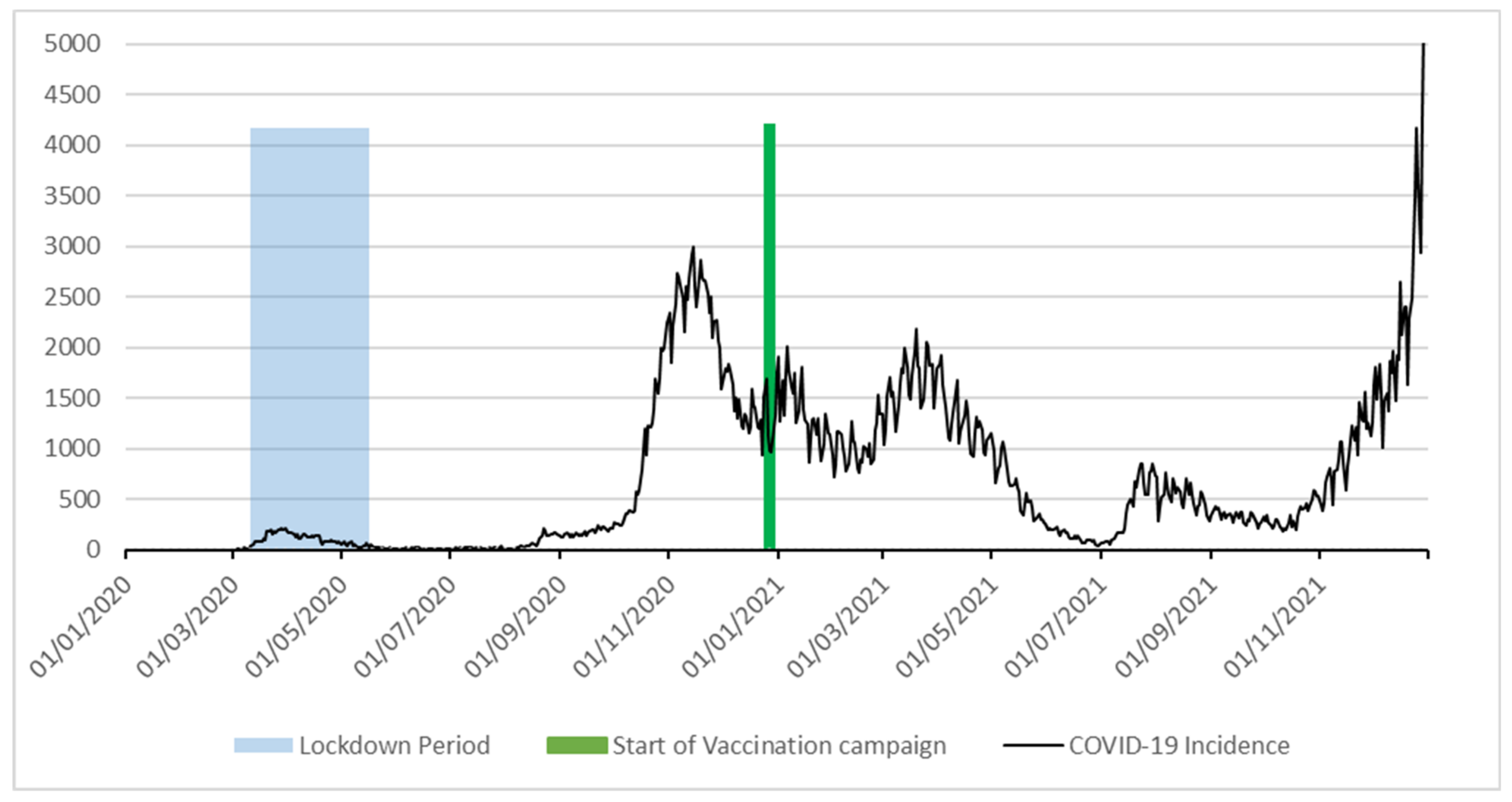
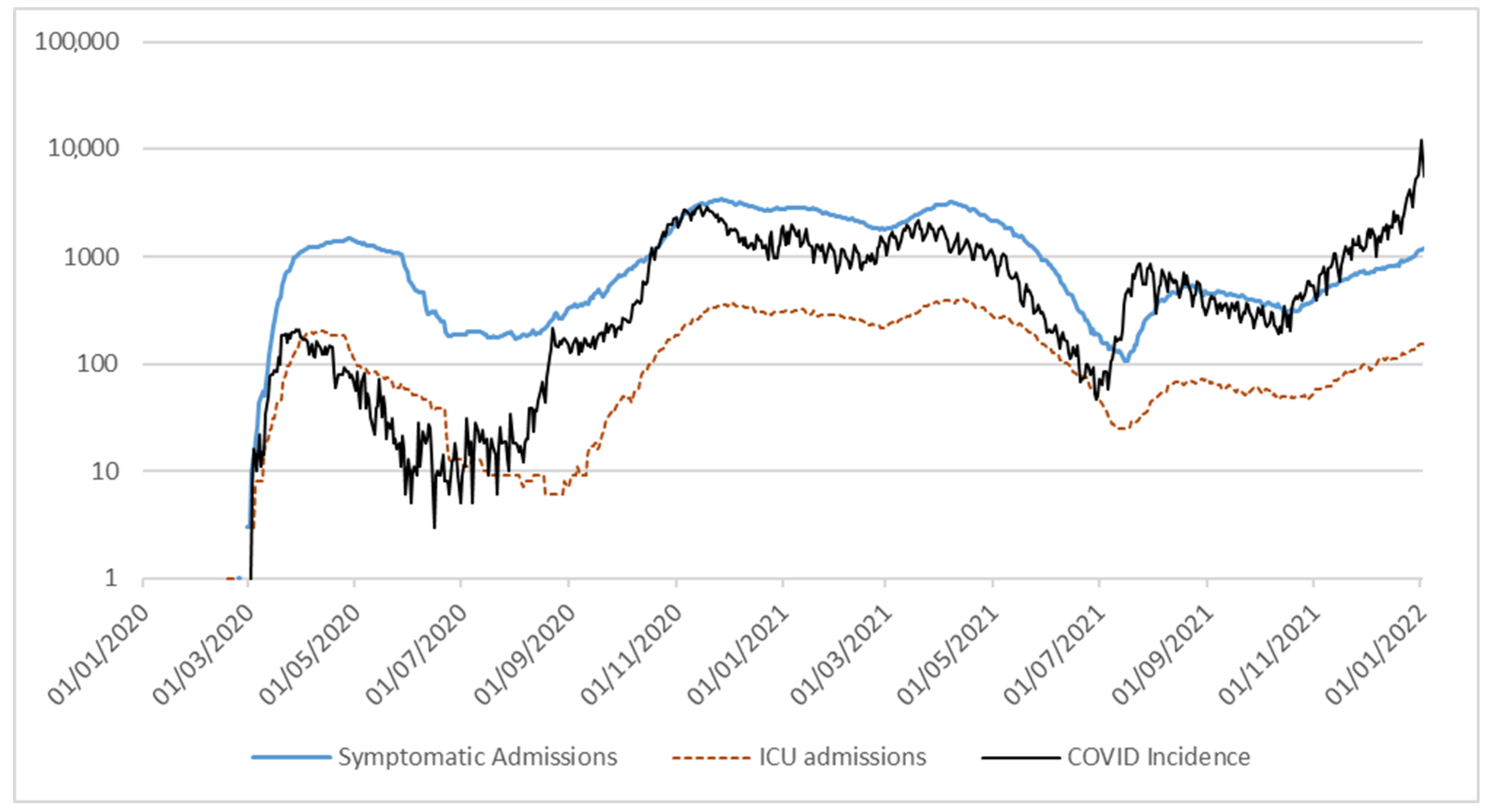
3.2. Epidemic Trend
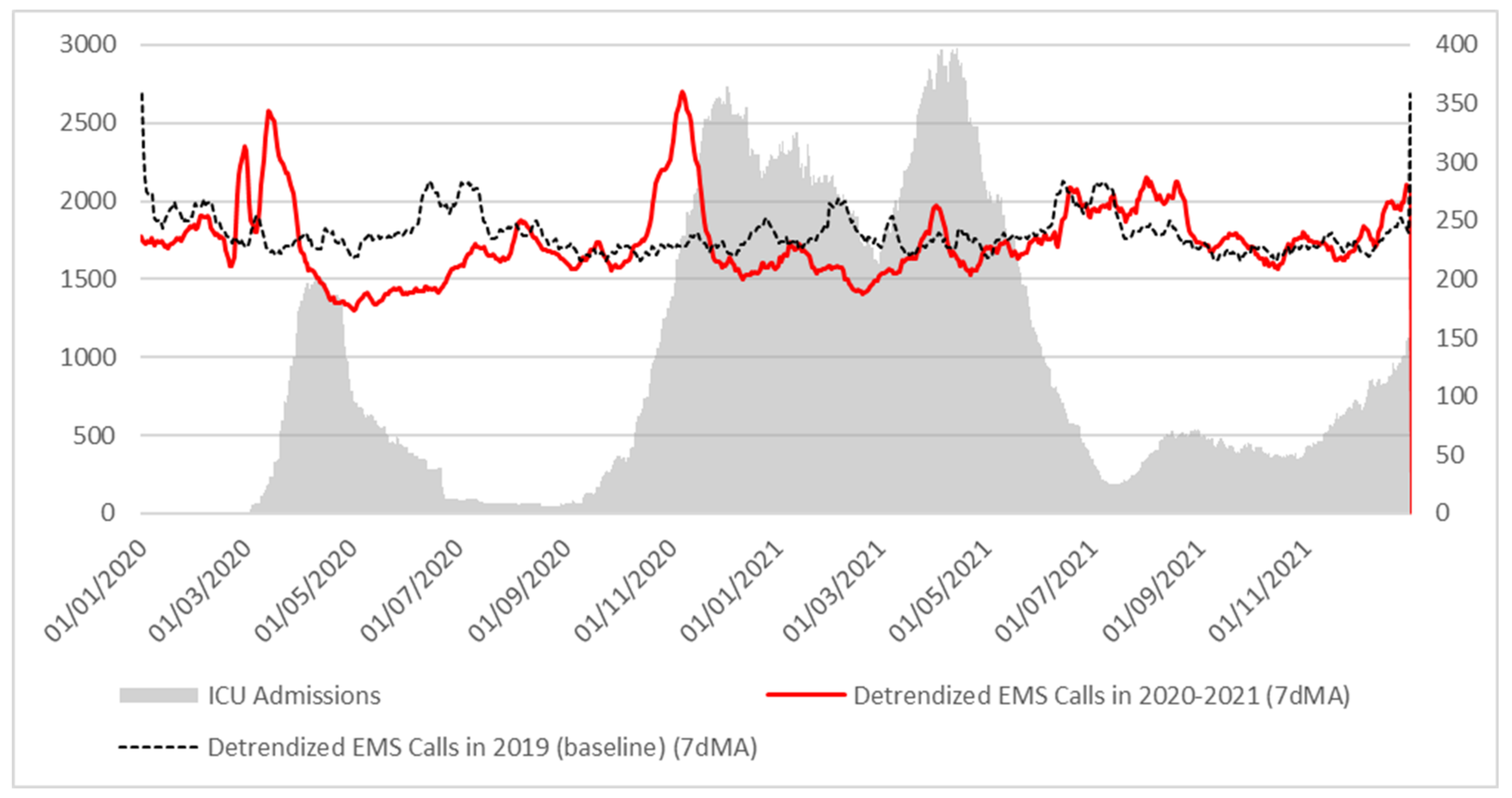
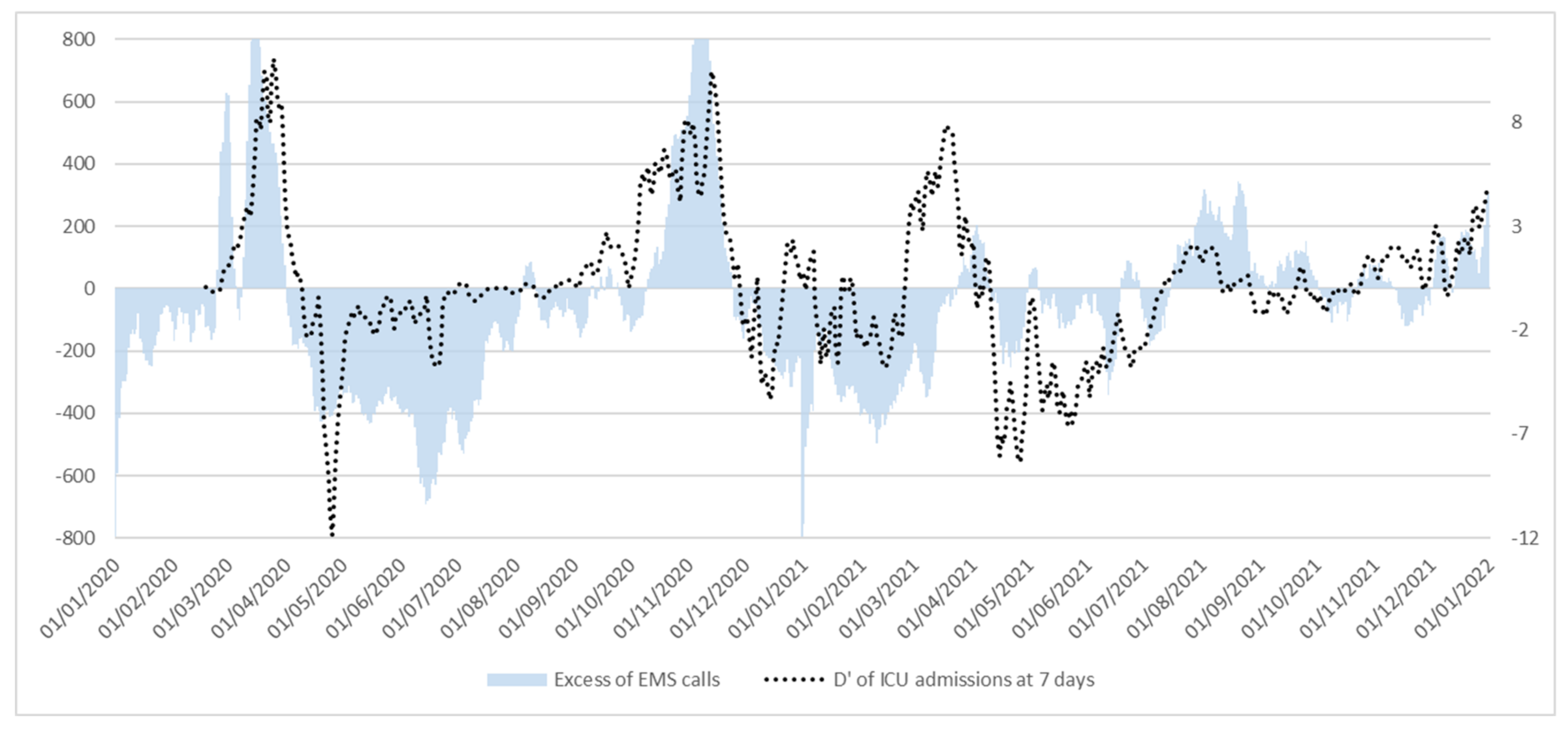
3.3. Trend of EMS Calls
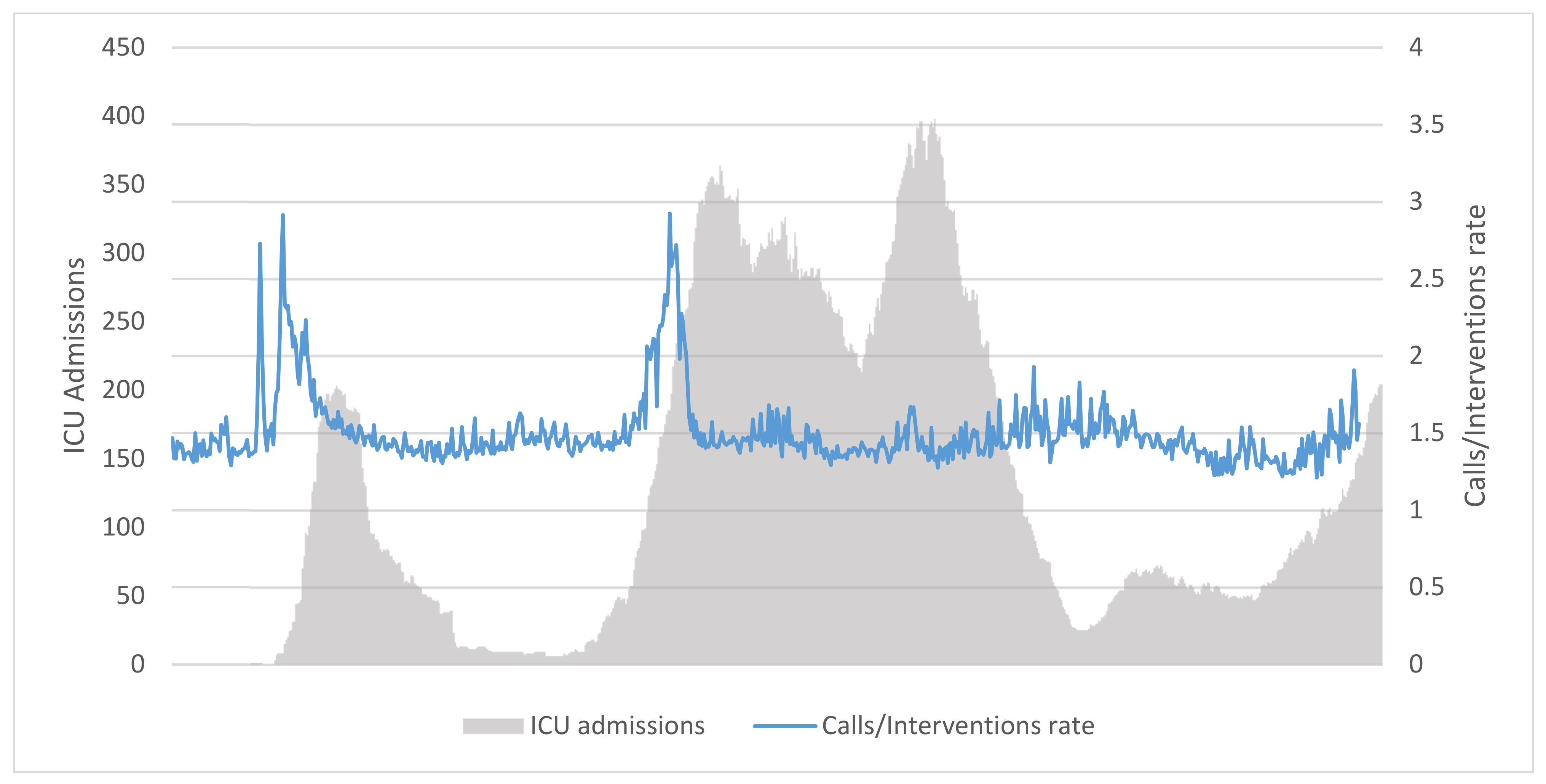
3.4. Regression Analysis
3.5. Validation
3.6. Forecasting Power
4. Discussion
4.1. Key Results
4.2. Limitations
- It has been partaken during a time when the COVID-19 pandemic was the major epidemic outbreak on the population. Lag time on ICU admissions depends on the epidemic characteristics of the virus itself: a pathogen with different epidemiological characteristics (such as serial interval, virulence, and infection rate) may yield to different results in terms of lag from EMS calls excess and actual increase in hospitalization. This of course does not affect the validity of current results or methodology, since the main purpose of current work was to investigate if EMS calls trend analysis is a viable tool in infectious diseases control, and if it can be a valid predictor in the right conditions.
- This study used only 2019 as a reference year for baseline drawing. Ideally, data from several “baseline” years should be used (for instance, European Mortality Monitoring EuroMOMO uses data from the previous 5 years in order to estimate excess mortality) in order to have a better baseline modelling [35]. Unfortunately, this limitation could not be overcome due to lack of an adequate data warehouse for ARES activity before 2019.
5. Conclusions
5.1. Interpretation
- Presence of a proportion of false-negatives;
- Limitation on the number of available tests, especially during the “first wave” phase, with a hard upper threshold on daily positive cases that could be identified;
- Late adoption of quick testing strategy as a viable case definition;
- Variability in symptoms onset and swab positivization, leading to disease underreporting.
5.2. Generalizability
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Decreto Del Presidente Della Repubblica. Atto Di Indirizzo E Coordinamento Alle Regioni Per La Determinazione Dei Livelli Di Assistenza Sanitaria Di Emergenza. 1992. Available online: https://www.gazzettaufficiale.it/eli/id/1997/02/20/097A1165/sg (accessed on 27 March 2022).
- Dominijanni, S.; Foniciello, M.; Tatangelo, P.; Angeloni, V.; Londrino, F.; Daniele, N.D.; Grandaliano, G.; Morosetti, M.; Palumbo, R. Chronic kidney disease and SARS-CoV-2 outbreak: Lazio region organizational model. Clin. Kidney J. 2020, 13, 480–481. [Google Scholar] [CrossRef] [PubMed]
- ISTAT. Statistiche Demografiche ISTAT. DemoISTAT. 2021. Available online: http://demo.istat.it/bilmens/index.php?anno=2020&lingua=ita (accessed on 27 March 2022).
- SANDUIR. 112 in Italy. Shaping Europe’s Digital Future—European Commission. 2013. Available online: https://ec.europa.eu/digital-single-market/en/112-italy (accessed on 27 March 2022).
- Perlini, S.; Canevari, F.; Cortesi, S.; Sgromo, V.; Brancaglione, A.; Contri, E.; Pettenazza, P.; Salinaro, F.; Speciale, F.; Sechi, G.; et al. Emergency Department and Out-of-Hospital Emergency System (112—AREU 118) integrated response to Coronavirus Disease 2019 in a Northern Italy centre. Intern. Emerg. Med. 2020, 15, 825–833. [Google Scholar] [CrossRef] [PubMed]
- Ientile, D.; Cardinale, M.; Cataldi, S. Emergency Medical Service Information System: The ARES 118 experience. Ann. Ig. 2017, 29, 504–514. [Google Scholar] [CrossRef] [PubMed]
- Montomoli, E.; Apolone, G.; Manenti, A.; Boeri, M.; Suatoni, P.; Sabia, F.; Marchianò, A.; Bollati, V.; Pastorino, U.; Sozzi, G. Timeline of SARS-CoV-2 Spread in Italy: Results from an Independent Serological Retesting. Viruses 2021, 14, 61. [Google Scholar] [CrossRef] [PubMed]
- Pietrantonio, F.; Rosiello, F.; Alessi, E.; Pascucci, M.; Rainone, M.; Cipriano, E.; Di Berardino, A.; Vinci, A.; Ruggeri, M.; Ricci, S. Burden of COVID-19 on Italian Internal Medicine Wards: Delphi, SWOT, and Performance Analysis after Two Pandemic Waves in the Local Health Authority “Roma 6” Hospital Structures. Int. J. Environ. Res. Public Health 2021, 18, 5999. [Google Scholar] [CrossRef]
- Piane, M.; Bianco, L.; Mancini, R.; Fornelli, P.; Gabriele, A.; Medici, F.; Battista, C.; Greco, S.; Croce, G.; Franceschetti, L.; et al. Impact of the COVID-19 Pandemic on Clinical Pathways for Non-SARS-CoV-2 Related Diseases in the Lazio Region, Italy. Int. J. Environ. Res. Public Health 2022, 19, 635. [Google Scholar] [CrossRef] [PubMed]
- Licata, F.; Oliverio, A.; Di Gennaro, G.; Nobile, C.G.A.; Bianco, A. Insight on Knowledge, Risk Perception and Practices to Prevent the Spread of COVID-19: A Cross-Sectional Study among Italian University Students. Appl. Sci. 2021, 11, 9031. [Google Scholar] [CrossRef]
- COVID-19—Situazione in Italia. Available online: https://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?id=5351&area=nuovoCoronavirus&menu=vuoto (accessed on 27 March 2022).
- COVID-19 ITALIA—Desktop. Available online: https://opendatadpc.maps.arcgis.com/apps/dashboards/b0c68bce2cce478eaac82fe38d4138b1 (accessed on 27 March 2022).
- Xie, Y.; Kulpanowski, D.; Ong, J.; Nikolova, E.; Tran, N.M. Predicting COVID-19 EMS Incidents from Daily Hospitalization Trends. Int. J. Clin. Pract. 2021, 75, e14920. [Google Scholar] [CrossRef]
- Laukkanen, L.; Lahtinen, S.; Liisanantti, J.; Kaakinen, T.; Ehrola, A.; Raatiniemi, L. Early impact of the COVID-19 pandemic and social restrictions on ambulance missions. Eur. J. Public Health 2021, 31, 1090–1095. [Google Scholar] [CrossRef]
- Jaffe, E.; Sonkin, R.; Alpert, E.A.; Zerath, E. Responses of a Pre-hospital Emergency Medical Service during Military Conflict Versus COVID-19: A Retrospective Comparative Cohort Study. Mil. Med. 2021, usab437. [Google Scholar] [CrossRef]
- Geyman, J. COVID-19 Has Revealed America’s Broken Health Care System: What Can We Learn? Int. J. Health Serv. 2021, 51, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, M.C.; Fox, M.A. Early Warnings: The Lessons of COVID-19 for Public Health Climate Preparedness. Int. J. Health Serv. 2020, 50, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Javed, S.; Chattu, V.K. Strengthening the COVID-19 pandemic response, global leadership, and international cooperation through global health diplomacy. Health Promot. Perspect. 2020, 10, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Griffin, K.M.; Karas, M.G.; Ivascu, N.S.; Lief, L. Hospital Preparedness for COVID-19: A Practical Guide from a Critical Care Perspective. Am. J. Respir. Crit. Care Med. 2020, 201, 1337–1344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, L.H.; Lerner, E.B.; Larmon, B.; LeGassick, T.; Taigman, M. Are EMS call volume predictions based on demand pattern analysis accurate? Prehosp. Emerg. Care 2007, 11, 199–203. [Google Scholar] [CrossRef]
- Jandoc, R.; Burden, A.M.; Mamdani, M.; Lévesque, L.E.; Cadarette, S.M. Interrupted time series analysis in drug utilization research is increasing: Systematic review and recommendations. J. Clin. Epidemiol. 2015, 68, 950–956. [Google Scholar] [CrossRef] [Green Version]
- Benchimol, E.I.; Smeeth, L.; Guttmann, A.; Harron, K.; Moher, D.; Petersen, I.; Sørensen, H.T.; von Elm, E.; Langan, S.M. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med. 2015, 12, e1001885. [Google Scholar] [CrossRef]
- Prado, R.; West, M. Time Series Modelling, Inference and Forecasting; Chapman and Hall/CRC: London, UK, 2010; ISBN 978-1420093360. [Google Scholar]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation Coefficients: Appropriate Use and Interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef]
- Slope Formula (Equation for Slope)|Algebra (Article). Khan Academy. Available online: https://www.khanacademy.org/math/cc-eighth-grade-math/cc-8th-linear-equations-functions/8th-slope/a/slope-formula (accessed on 27 March 2022).
- Hyndman, R.J.; Athanasopoulos, G. 3.4 Classical decomposition. In Forecasting: Principles and Practice, 3rd ed.; OTexts: Melbourne, Australia, 2018. [Google Scholar]
- Yan, X. Linear Regression Analysis: Theory and Computing; World Scientific: Singapore, 2009. [Google Scholar]
- Draper, N.R.; Smith, H. Applied Regression Analysis; Wiley: Hoboken, NJ, USA, 1998. [Google Scholar]
- Rodríguez, J.D.; Pérez, A.; Lozano, J.A. Sensitivity Analysis of k-Fold Cross Validation in Prediction Error Estimation. IEEE Trans. Pattern Anal. Mach. Intell. 2009, 32, 569–575. [Google Scholar] [CrossRef]
- Garante per la Protezione dei Dati Personali. Autorizzazione Generale Al Trattamento Dei Dati Personali Effettuato Per Scopi Di Ricerca Scientifica. G U. n. 303 del 29 dicembre 2016. Available online: https://www.gazzettaufficiale.it/eli/gu/2016/12/29/303/sg/pdf (accessed on 27 March 2022).
- Adam, D. A guide to R—The pandemic’s misunderstood metric. Nature 2020, 583, 346–348. [Google Scholar] [CrossRef]
- Gentili, S.; Gialloreti, L.E.; Riccardi, F.; Scarcella, P.; Liotta, G. Predictors of Emergency Room Access and Not Urgent Emergency Room Access by the Frail Older Adults. Front. Public Health 2021, 9, 721634. [Google Scholar] [CrossRef] [PubMed]
- Amore, S.; Puppo, E.; Melara, J.; Terracciano, E.; Gentili, S.; Liotta, G. Impact of COVID-19 on older adults and role of long-term care facilities during early stages of epidemic in Italy. Sci. Rep. 2021, 11, 12530. [Google Scholar] [CrossRef] [PubMed]
- Palombi, L.; Liotta, G.; Orlando, S.; Emberti Gialloreti, L.; Marazzi, M.C. Does the Coronavirus (COVID-19) Pandemic Call for a New Model of Older People Care? Front. Public Health 2020, 8, 311. [Google Scholar] [CrossRef] [PubMed]
- EuroMOMO. EUROMOMO Methods. Available online: https://euromomo.eu/dev-404-page/ (accessed on 27 March 2022).
- Sharif, N.; Alzahrani, K.J.; Ahmed, S.N.; Dey, S.K. Efficacy, Immunogenicity and Safety of COVID-19 Vaccines: A Systematic Review and Meta-Analysis. Front. Immunol. 2021, 12, 714170. [Google Scholar] [CrossRef]
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.-S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S.; et al. Health systems resilience in managing the COVID-19 pandemic: Lessons from 28 countries. Nat. Med. 2021, 27, 964–980. [Google Scholar] [CrossRef]
- Doumas, M.; Imprialos, K.P.; Patoulias, D.; Katsimardou, A.; Stavropoulos, K. COVID-19: The Waterloo of governments, healthcare systems, and large health organizations. Eur. J. Intern. Med. 2020, 77, 153–155. [Google Scholar] [CrossRef]
- Casigliani, V.; De Nard, F.; De Vita, E.; Arzilli, G.; Grosso, F.M.; Quattrone, F.; Tavoschi, L.; Lopalco, P. Too much information, too little evidence: Is waste in research fuelling the COVID-19 infodemic? BMJ 2020, 370, m2672. [Google Scholar] [CrossRef]
- Gesualdo, F.; D’Ambrosio, A.; Agricola, E.; Russo, L.; Campagna, I.; Ferretti, B.; Pandolfi, E.; Cristoforetti, M.; Tozzi, A.E.; Rizzo, C. How do Twitter users react to TV broadcasts dedicated to vaccines in Italy? Eur. J. Public Health 2020, 30, 481–486. [Google Scholar] [CrossRef] [Green Version]
- Olivieri, A.; Palù, G.; Sebastiani, G. COVID-19 cumulative incidence, intensive care, and mortality in Italian regions compared to selected European countries. Int. J. Infect. Dis. 2021, 102, 363–368. [Google Scholar] [CrossRef]
- Pires, C. What Is the State-of-the-Art in Clinical Trials on Vaccine Hesitancy 2015–2020? Vaccines 2021, 9, 348. [Google Scholar] [CrossRef]
- Bianco, A.; Della Polla, G.; Angelillo, S.; Pelullo, C.P.; Licata, F.; Angelillo, I.F. Parental COVID-19 vaccine hesitancy: A cross-sectional survey in Italy. Expert Rev. Vaccines 2022, 21, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Psaroudakis, I.; Quattrone, F.; Tavoschi, L.; De Vita, E.; Cervia, S.; Biancheri, R.; Lopalco, P.L. Engaging adolescents in developing health education interventions: A multidisciplinary pilot project. Eur. J. Public Health 2020, 30, 712–714. [Google Scholar] [CrossRef] [PubMed]
- Filippini, T.; Zagnoli, F.; Bosi, M.; Giannone, M.E.; Marchesi, C.; Vinceti, M. An assessment of case-fatality and infection-fatality rates of first and second COVID-19 waves in Italy. Acta Biomed. 2021, 92, e2021420. [Google Scholar]
- Babyak, M.A. What You See May Not Be What You Get: A Brief, Nontechnical Introduction to Overfitting in Regression-Type Models. Psychosom. Med. 2004, 66, 411–421. [Google Scholar]
- Castro, L.A.; Shelley, C.D.; Osthus, D.; Michaud, I.; Mitchell, J.; Manore, C.A.; Del Valle, S.Y. How New Mexico Leveraged a COVID-19 Case Forecasting Model to Preemptively Address the Health Care Needs of the State: Quantitative Analysis. JMIR Public Health Surveill. 2021, 7, e27888. [Google Scholar] [CrossRef]
- Rivieccio, B.A.; Micheletti, A.; Maffeo, M.; Zignani, M.; Comunian, A.; Nicolussi, F.; Salini, S.; Manzi, G.; Auxilia, F.; Giudici, M.; et al. COVID-19, learning from the past: A wavelet and cross-correlation analysis of the epidemic dynamics looking to emergency calls and Twitter trends in Italian Lombardy region. PLoS ONE 2021, 16, e0247854. [Google Scholar] [CrossRef] [PubMed]
- Ryan-Ibarra, S.; Nishimura, H.; Gallington, K.; Grinnell, S.; Bekemeier, B. Time to Modernize: Local Public Health Transitions to Population-Level Interventions. J. Public Health Manag. Pract. 2021, 27, 464–472. [Google Scholar] [CrossRef]

| Symptomatic Admissions | ICU Admissions | Total Admissions | COVID Incidence (14 Days Prior) | Daily Deaths | |
|---|---|---|---|---|---|
| Symptomatic Admissions | 1 | ||||
| ICU admissions | 0.968823 | 1 | |||
| Total admissions | 0.999663 | 0.974927 | 1 | ||
| COVID Incidence (14 days prior) | 0.841558 | 0.837922 | 0.843642 | 1 | |
| Daily deaths | 0.863062 | 0.835356 | 0.862688 | 0.760818 | 1 |
| 1st Derivative of ICU Admissions at | Adjusted R2 | F-Statistic p-Value |
|---|---|---|
| 0 days | 0.247 | 2.2259 × 10−43 |
| 5 days | 0.3191 | 4.6315 × 10−58 |
| 6 days | 0.326 | 1.5130 × 10−59 |
| 7 days | 0.328 | 5.6168 × 10−60 |
| 8 days | 0.3278 | 6.156 × 10−60 |
| 9 days | 0.3257 | 1.8340 × 10−59 |
| 10 days | 0.3191 | 4.7653 × 10−58 |
| 11 days | 0.3095 | 5.099 × 10−56 |
| 12 days | 0.296 | 3.3879 × 10−53 |
| 13 days | 0.2799 | 6.9579 × 10−50 |
| 14 days | 0.2627 | 1.8906 × 10−46 |
| Observations Set | R2 Values |
|---|---|
| Fold 1 | 0.24717 |
| Fold 2 | 0.244523 |
| Fold 3 | 0.481349 |
| Fold 4 | 0.32992 |
| Mean | 0.32574 |
| Global R2 estimate | 0.321919 |
| Difference | −0.00382 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vinci, A.; Pasquarella, A.; Corradi, M.P.; Chatzichristou, P.; D’Agostino, G.; Iannazzo, S.; Trani, N.; Parafati, M.A.; Palombi, L.; Ientile, D.A. Emergency Medical Services Calls Analysis for Trend Prediction during Epidemic Outbreaks: Interrupted Time Series Analysis on 2020–2021 COVID-19 Epidemic in Lazio, Italy. Int. J. Environ. Res. Public Health 2022, 19, 5951. https://doi.org/10.3390/ijerph19105951
Vinci A, Pasquarella A, Corradi MP, Chatzichristou P, D’Agostino G, Iannazzo S, Trani N, Parafati MA, Palombi L, Ientile DA. Emergency Medical Services Calls Analysis for Trend Prediction during Epidemic Outbreaks: Interrupted Time Series Analysis on 2020–2021 COVID-19 Epidemic in Lazio, Italy. International Journal of Environmental Research and Public Health. 2022; 19(10):5951. https://doi.org/10.3390/ijerph19105951
Chicago/Turabian StyleVinci, Antonio, Amina Pasquarella, Maria Paola Corradi, Pelagia Chatzichristou, Gianluca D’Agostino, Stefania Iannazzo, Nicoletta Trani, Maria Annunziata Parafati, Leonardo Palombi, and Domenico Antonio Ientile. 2022. "Emergency Medical Services Calls Analysis for Trend Prediction during Epidemic Outbreaks: Interrupted Time Series Analysis on 2020–2021 COVID-19 Epidemic in Lazio, Italy" International Journal of Environmental Research and Public Health 19, no. 10: 5951. https://doi.org/10.3390/ijerph19105951
APA StyleVinci, A., Pasquarella, A., Corradi, M. P., Chatzichristou, P., D’Agostino, G., Iannazzo, S., Trani, N., Parafati, M. A., Palombi, L., & Ientile, D. A. (2022). Emergency Medical Services Calls Analysis for Trend Prediction during Epidemic Outbreaks: Interrupted Time Series Analysis on 2020–2021 COVID-19 Epidemic in Lazio, Italy. International Journal of Environmental Research and Public Health, 19(10), 5951. https://doi.org/10.3390/ijerph19105951







