Weight Status Change in Chinese American Children over a Ten-Year Period: Retrospective Study of a Primary Care Pediatric Population
Abstract
1. Introduction
2. Materials and Methods
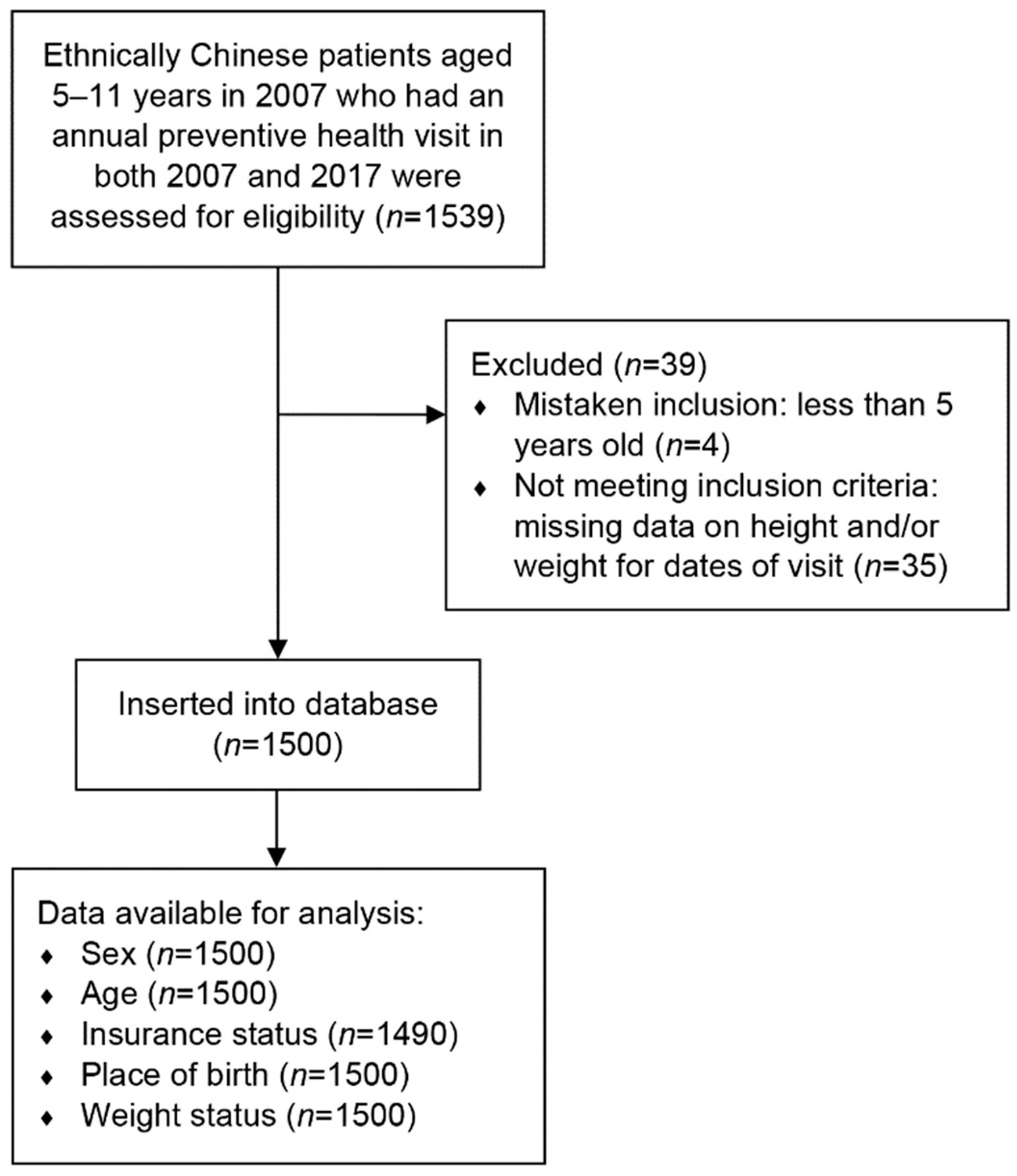
2.1. Study Design and Participants
2.2. Ethical Considerations
2.3. Measures
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fryar, C.D.; Carroll, M.D.; Afful, J. Prevalence of Overweight, Obesity, and Severe Obesity among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 through 2017–2018. Available online: https://www.cdc.gov/nchs/data/hestat/obesity-child-17-18/obesity-child.htm (accessed on 20 March 2021).
- Ogden, C.L.; Fryar, C.D.; Martin, C.B.; Freedman, D.S.; Carroll, M.D.; Gu, Q.; Hales, C.M. Trends in obesity prevalence by race and Hispanic origin—1999–2000 to 2017–2018. JAMA 2020, 324, 1208–1210. [Google Scholar] [CrossRef] [PubMed]
- Park, M.H.; Falconer, C.; Viner, R.M.; Kinra, S. The impact of childhood obesity on morbidity and mortality in adulthood: A systematic review. Obes. Rev. 2012, 13, 985–1000. [Google Scholar] [CrossRef] [PubMed]
- Reilly, J.J.; Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. 2011, 35, 891–898. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.S.; Mulder, C.; Twisk, J.W.; van Mechelen, W.; Chinapaw, M.J. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes. Rev. 2008, 9, 474–488. [Google Scholar] [CrossRef]
- Starc, G.; Strel, J. Tracking excess weight and obesity from childhood to young adulthood: A 12-year prospective cohort study in Slovenia. Public Health Nutr. 2011, 14, 49–55. [Google Scholar] [CrossRef]
- Johannsson, E.; Arngrimsson, S.A.; Thorsdottir, I.; Sveinsson, T. Tracking of overweight from early childhood to adolescence in cohorts born 1988 and 1994: Overweight in a high birth weight population. Int. J. Obes. 2006, 30, 1265–1271. [Google Scholar] [CrossRef]
- Evensen, E.; Wilsgaard, T.; Furberg, A.S.; Skeie, G. Tracking of overweight and obesity from early childhood to adolescence in a population-based cohort—The Tromso Study, Fit Futures. BMC Pediatr. 2016, 16, 64. [Google Scholar] [CrossRef]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef]
- Freedman, D.S.; Khan, L.K.; Serdula, M.K.; Dietz, W.H.; Srinivasan, S.R.; Berenson, G.S. Racial differences in the tracking of childhood BMI to adulthood. Obes. Res. 2005, 13, 928–935. [Google Scholar] [CrossRef]
- Schuster, M.A.; Elliott, M.N.; Bogart, L.M.; Klein, D.J.; Feng, J.Y.; Wallander, J.L.; Cuccaro, P.; Tortolero, S.R. Changes in obesity between fifth and tenth grades: A longitudinal study in three metropolitan areas. Pediatrics 2014, 134, 1051–1058. [Google Scholar] [CrossRef]
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics 2018, 141, e20173459. [Google Scholar] [CrossRef] [PubMed]
- Deurenberg, P.; Deurenberg-Yap, M.; Guricci, S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes. Rev. 2002, 3, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Wen, C.P.; David Cheng, T.Y.; Tsai, S.P.; Chan, H.T.; Hsu, H.L.; Hsu, C.C.; Eriksen, M.P. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. 2009, 12, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Hsu, W.C.; Araneta, M.R.G.; Kanaya, A.M.; Chiang, J.L.; Fujimoto, W. BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care 2015, 38, 150. [Google Scholar] [CrossRef]
- Jih, J.; Mukherjea, A.; Vittinghoff, E.; Nguyen, T.T.; Tsoh, J.Y.; Fukuoka, Y.; Bender, M.S.; Tseng, W.; Kanaya, A.M. Using appropriate body mass index cut points for overweight and obesity among Asian Americans. Prev. Med. 2014, 65, 1–6. [Google Scholar] [CrossRef]
- Zheng, W.; McLerran, D.F.; Rolland, B.; Zhang, X.; Inoue, M.; Matsuo, K.; He, J.; Gupta, P.C.; Ramadas, K.; Tsugane, S.; et al. Association between body-mass index and risk of death in more than 1 million Asians. N. Engl. J. Med. 2011, 364, 719–729. [Google Scholar] [CrossRef]
- Yi, S.S.; Kwon, S.C.; Wyatt, L.; Islam, N.; Trinh-Shevrin, C. Weighing in on the hidden Asian American obesity epidemic. Prev. Med. 2015, 73, 6–9. [Google Scholar] [CrossRef]
- Ogden, C.L.; Fryar, C.D.; Hales, C.M.; Carroll, M.D.; Aoki, Y.; Freedman, D.S. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013–2016. JAMA 2018, 319, 2410–2418. [Google Scholar] [CrossRef]
- Ogden, C.L.; Carroll, M.D.; Lawman, H.G.; Fryar, C.D.; Kruszon-Moran, D.; Kit, B.K.; Flegal, K.M. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 2016, 315, 2292–2299. [Google Scholar] [CrossRef]
- Asian & Pacific Islander American Health Forum. Obesity and Overweight among Asian American Children and Adolescents. Available online: https://www.apiahf.org/resource/obesity-and-overweight-among-asian-american-children-and-adolescents/ (accessed on 10 April 2021).
- Au, L.; Kwong, K.; Chou, J.C.; Tso, A.; Wong, M. Prevalence of overweight and obesity in Chinese American children in New York City. J. Immigr. Minor. Health 2009, 11, 337–341. [Google Scholar] [CrossRef]
- Au, L.; Lau, J.D.; Chao, E.; Tse, R.; Elbaar, L. Update on Chinese American childhood obesity prevalence in New York City. J. Immigr. Minor. Health 2018, 20, 1303–1307. [Google Scholar] [CrossRef] [PubMed]
- New York City Mayor’s Office for Economic Opportunity. The New York City Government Poverty Measure, 2005–2017: An Annual Report from the Office of the Mayor. Available online: https://www1.nyc.gov/assets/opportunity/pdf/19_poverty_measure_report.pdf (accessed on 20 April 2022).
- New York City Mayor’s Office for Economic Opportunity. An Economic Profile of Immigrants in New York City 2017: Results from NYC Opportunity’s Experimental Population Estimate. Available online: https://www1.nyc.gov/assets/opportunity/pdf/immigrant-poverty-report-2017.pdf (accessed on 20 April 2022).
- Sterling IRB. Overview of Services with Institutions. Available online: https://www.sterlingirb.com/services-overview/ (accessed on 20 April 2022).
- Kuczmarski, R.J.; Ogden, C.L.; Guo, S.S.; Grummer-Strawn, L.M.; Flegal, K.M.; Mei, Z.; Wei, R.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. 2000 CDC Growth Charts for the United States: Methods and Development; Vital and Health Statistics. Series 11; National Center for Health Statistics: Hyattsville, MD, USA, 2002; pp. 1–190.
- IBM. IBM SPSS Statistics. Available online: https://www.ibm.com/products/spss-statistics (accessed on 20 January 2020).
- Cunningham, S.A.; Kramer, M.R.; Narayan, K.M.V. Incidence of childhood obesity in the United States. N. Engl. J. Med. 2014, 370, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Dai, S.; Labarthe, D.R.; Grunbaum, J.A.; Harrist, R.B.; Mueller, W.H. Longitudinal analysis of changes in indices of obesity from age 8 years to age 18 years. Project HeartBeat! Am. J. Epidemiol. 2002, 156, 720–729. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Araújo, J.; Barros, H.; Severo, M.; Lopes, C.; Ramos, E. Longitudinal changes in adiposity during adolescence: A population-based cohort. BMJ Open 2014, 4, e004380. [Google Scholar] [CrossRef]
- Williamson, D.A.; Han, H.; Johnson, W.D.; Stewart, T.M.; Harsha, D.W. Longitudinal study of body weight changes in children: Who is gaining and who is losing weight. Obesity 2011, 19, 667–670. [Google Scholar] [CrossRef]
- Guo, S.S.; Wu, W.; Chumlea, W.C.; Roche, A.F. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am. J. Clin. Nutr. 2002, 76, 653–658. [Google Scholar] [CrossRef]
- Power, C.; Lake, J.K.; Cole, T.J. Body mass index and height from childhood to adulthood in the 1958 British born cohort. Am. J. Clin. Nutr. 1997, 66, 1094–1101. [Google Scholar] [CrossRef]
- Wang, Y.; Ge, K.; Popkin, B.M. Tracking of body mass index from childhood to adolescence: A 6-y follow-up study in China. Am. J. Clin. Nutr. 2000, 72, 1018–1024. [Google Scholar] [CrossRef]
- Geserick, M.; Vogel, M.; Gausche, R.; Lipek, T.; Spielau, U.; Keller, E.; Pfäffle, R.; Kiess, W.; Körner, A. Acceleration of BMI in early childhood and risk of sustained obesity. N. Engl. J. Med. 2018, 379, 1303–1312. [Google Scholar] [CrossRef]
- Baur, L.A.; Garnett, S.P. Early childhood—A critical period for obesity prevention. Nat. Rev. Endocrinol. 2019, 15, 5–6. [Google Scholar] [CrossRef]
- Lau, J.D.; Elbaar, L.; Chao, E.; Zhong, O.; Yu, C.R.; Tse, R.; Au, L. Measuring overweight and obesity in Chinese American children using US, international and ethnic-specific growth charts. Public Health Nutr. 2020, 23, 2663–2670. [Google Scholar] [CrossRef] [PubMed]
- Nakano, T.; Sei, M.; Ewis, A.A.; Munakata, H.; Onishi, C.; Nakahori, Y. Tracking overweight and obesity in Japanese children; a six years longitudinal study. J. Med. Investig. 2010, 57, 114–123. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef] [PubMed]
- De Onis, M.; Garza, C.; Onyango, A.W.; Borghi, E. Comparison of the WHO Child Growth Standards and the CDC 2000 Growth Charts. J. Nutr. 2007, 137, 144–148. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Zhou, N.; Cheah, C.S. Ecological risk model of childhood obesity in Chinese immigrant children. Appetite 2015, 90, 99–107. [Google Scholar] [CrossRef]
- Matloff, G.R.; Lee, A.C.; Tang, R.; Brugge, D. The obesity epidemic in Chinese American youth? A literature review and pilot study. AAPI Nexus 2008, 6, 31–42. [Google Scholar] [CrossRef]
- Cheah, C.S.; Van Hook, J. Chinese and Korean immigrants’ early life deprivation: An important factor for child feeding practices and children’s body weight in the United States. Soc. Sci. Med. 2012, 74, 744–752. [Google Scholar] [CrossRef][Green Version]
- Nobari, T.Z.; Wang, M.-C.; Chaparro, M.P.; Crespi, C.M.; Koleilat, M.; Whaley, S.E. Immigrant enclaves and obesity in preschool-aged children in Los Angeles County. Soc. Sci. Med. 2013, 92, 1–8. [Google Scholar] [CrossRef]
- Singh, G.K.; Yu, S.M.; Kogan, M.D. Health, chronic conditions, and behavioral risk disparities among U.S. immigrant children and adolescents. Public Health Rep. 2013, 128, 463–479. [Google Scholar] [CrossRef]
- Batchelder, A.; Matusitz, J. “Let’s Move” Campaign: Applying the Extended Parallel Process Model. Soc. Work Public Health 2014, 29, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Brennan, L.K.; Kemner, A.L.; Donaldson, K.; Brownson, R.C. Evaluating the implementation and impact of policy, practice, and environmental changes to prevent childhood obesity in 49 diverse communities. J. Public Health Manag. Pract. 2015, 21, S121–S134. [Google Scholar] [CrossRef] [PubMed]
- Kelly, P.M.; Davies, A.; Greig, A.J.M.; Lee, K.K. Obesity prevention in a city state: Lessons from New York City during the Bloomberg administration. Front. Public Health 2016, 4, 60. [Google Scholar] [CrossRef] [PubMed][Green Version]
- American Academy of Pediatrics. What Is Medical Home? Available online: https://medicalhomeinfo.aap.org/overview/Pages/Whatisthemedicalhome.aspx (accessed on 27 April 2022).
- Medical Home Initiatives for Children with Special Needs Project Advisory Committee. Policy Statement: Organizational Principles to Guide and Define the Child Health Care System and/or Improve the Health of All Children. Pediatrics 2004, 113, 1545–1547. [Google Scholar] [CrossRef]
- Cygan, H.; Reed, M.; Lui, K.; Mullen, M. The chronic care model to improve management of childhood obesity. Clin. Pediatr. 2018, 57, 727–732. [Google Scholar] [CrossRef]
- Von Korff, M.; Gruman, J.; Schaefer, J.; Curry, S.J.; Wagner, E.H. Collaborative management of chronic illness. Ann. Intern. Med. 1997, 127, 1097–1102. [Google Scholar] [CrossRef]
- Barlow, S.E. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007, 120, S164–S192. [Google Scholar] [CrossRef]
- Rhee, K.E.; Kessl, S.; Lindback, S.; Littman, M.; El-Kareh, R.E. Provider views on childhood obesity management in primary care settings: A mixed methods analysis. BMC Health Serv. Res. 2018, 18, 55. [Google Scholar] [CrossRef]
- Hurt, R.T.; Kulisek, C.; Buchanan, L.A.; McClave, S.A. The obesity epidemic: Challenges, health initiatives, and implications for gastroenterologists. Gastroenterol. Hepatol. 2010, 6, 780–792. [Google Scholar]
| Characteristic | n | % | US-Born | Foreign-Born | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Sex | ||||||
| Male | 769 | 51.3 | 663 | 51.8 | 106 | 48.2 |
| Female | 731 | 48.7 | 617 | 48.2 | 114 | 51.8 |
| Age in 2007 | ||||||
| 5–8 years | 1108 | 73.9 | 989 | 77.3 | 119 | 54.1 |
| 9–11 years | 392 | 26.1 | 291 | 22.7 | 101 | 45.9 |
| Insurance Status 1 | ||||||
| Public insurance/self-pay (no change in 2007 vs. 2017) | 1241 | 82.7 | 1045 | 82.3 | 196 | 89.1 |
| Private insurance (no change in 2007 vs. 2017) | 109 | 7.3 | 104 | 8.2 | 5 | 2.3 |
| Public insurance/self-pay in 2007 to Private insurance in 2017 | 102 | 6.8 | 83 | 6.5 | 19 | 8.6 |
| Private insurance in 2007 to public insurance/self-pay in 2017 | 38 | 2.5 | 38 | 3 | 0 | 0 |
| Place of Birth | ||||||
| US-Born | 1280 | 85.3 | - | - | - | - |
| Foreign-Born | 220 | 14.7 | - | - | - | - |
| Characteristic | 2007 | 2017 | ||
|---|---|---|---|---|
| n | % | n | % | |
| Entire Sample (n = 1500) | 449 | 29.9 | 279 | 18.6 |
| Sex | ||||
| Male (n = 769) | 295 | 38.4 | 187 | 24.3 |
| Female (n = 731) | 154 | 21.1 | 92 | 12.6 |
| Age | ||||
| 5–8 years (n = 1108) | 322 | 29.1 | 201 | 18.1 |
| 9–11 years (n = 392) | 127 | 32.4 | 78 | 19.9 |
| Place of Birth | ||||
| US-Born (n = 1280) | 395 | 30.9 | 243 | 19.0 |
| Foreign-Born (n = 220) | 54 | 24.5 | 36 | 16.4 |
| Overweight/Obese in 2007 | Overweight/Obese in 2017 | Total | |
|---|---|---|---|
| No | Yes | ||
| No | 977 | 74 | 1051 |
| Yes | 244 | 205 | 449 |
| Total | 1221 | 279 | 1500 |
| Characteristic | Weight Status in 2007 | ||
|---|---|---|---|
| Underweight/Normal Weight | Overweight/Obese | Adjusted OR 1 (95% CI), p < 0.001 | |
| Entire Sample (n = 1500) | 7.0% | 45.7% | 10.30 (7.60–13.96) |
| Place of Birth | |||
| US Born (n = 1280) | 7.8% | 44.1% | 8.64 (6.28–11.90) |
| Foreign Born (n = 220) | 3.0% | 57.4% | 40.57 (14.27–115.39) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, J.L.L.; Zhong, O.; Tse, R.; Lau, J.D.; Chao, E.; Au, L. Weight Status Change in Chinese American Children over a Ten-Year Period: Retrospective Study of a Primary Care Pediatric Population. Int. J. Environ. Res. Public Health 2022, 19, 5916. https://doi.org/10.3390/ijerph19105916
Lin JLL, Zhong O, Tse R, Lau JD, Chao E, Au L. Weight Status Change in Chinese American Children over a Ten-Year Period: Retrospective Study of a Primary Care Pediatric Population. International Journal of Environmental Research and Public Health. 2022; 19(10):5916. https://doi.org/10.3390/ijerph19105916
Chicago/Turabian StyleLin, Jia Lu Lilian, Olivia Zhong, Raymond Tse, Jennifer D. Lau, Eda Chao, and Loretta Au. 2022. "Weight Status Change in Chinese American Children over a Ten-Year Period: Retrospective Study of a Primary Care Pediatric Population" International Journal of Environmental Research and Public Health 19, no. 10: 5916. https://doi.org/10.3390/ijerph19105916
APA StyleLin, J. L. L., Zhong, O., Tse, R., Lau, J. D., Chao, E., & Au, L. (2022). Weight Status Change in Chinese American Children over a Ten-Year Period: Retrospective Study of a Primary Care Pediatric Population. International Journal of Environmental Research and Public Health, 19(10), 5916. https://doi.org/10.3390/ijerph19105916






