Prevalence of SARS-CoV-2 Infection in a Sample of Health Workers in Two Health Departments of the Valencian Community in Spain
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Variables
2.3.1. Active SARS-CoV-2 Infection
2.3.2. Epidemiological Variables
2.4. Procedure
2.5. Ethical Considerations
2.6. Statistical Analysis
3. Results
3.1. Prevalence of SARS-CoV-2 Infection in the Target Sample
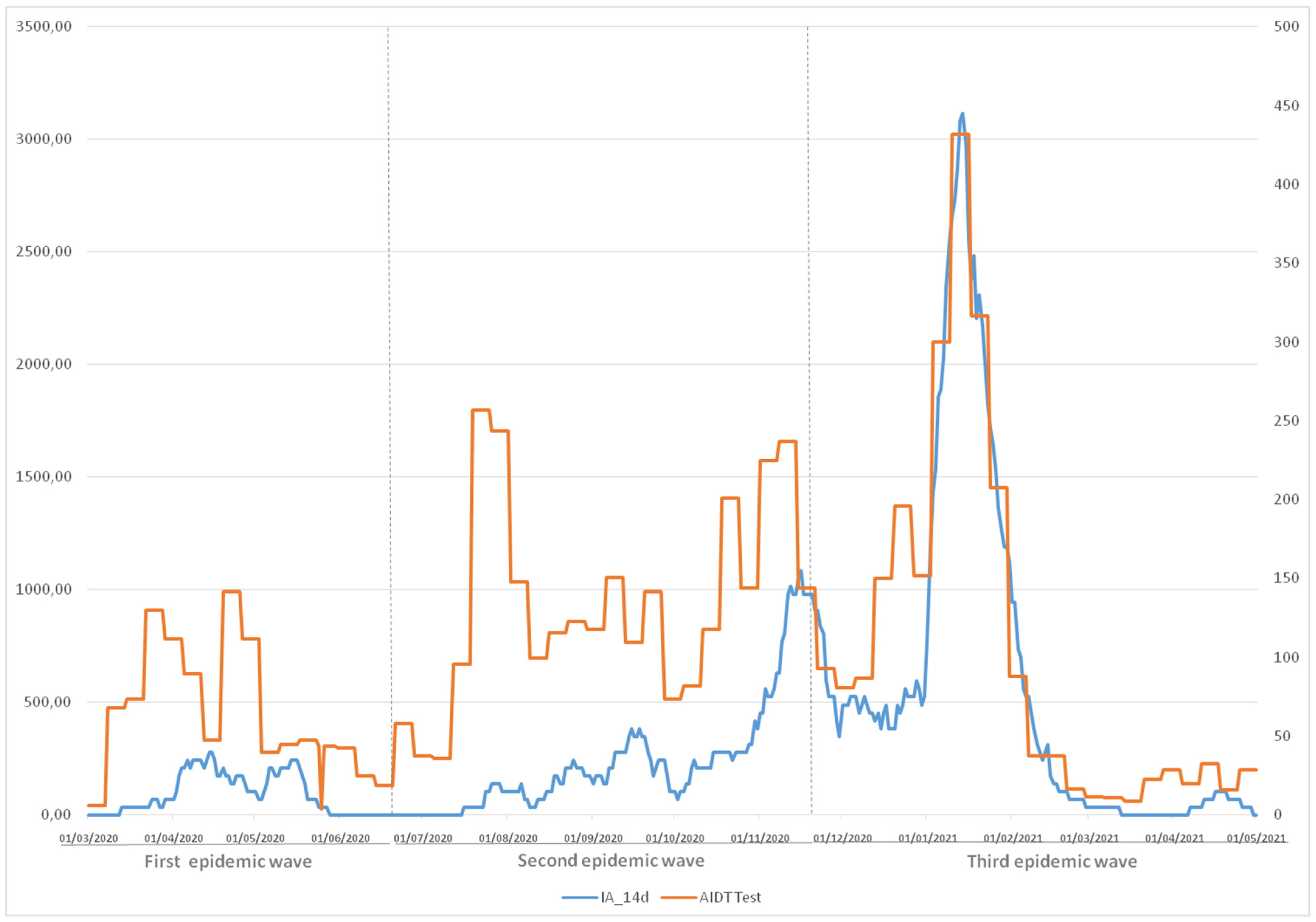
3.2. AIDT vs. SARS-CoV-2 in the Target Sample
3.3. Confirmed Cases of SARS-CoV-2 Infection in the Target Sample
3.4. Distribution of Confirmed Cases of SARS-CoV-2 Infection in the Target Sample in Chronological Periods
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centro de Coordinación de Alertas y Emergencias Sanitarias. Valoración de la Declaración del Brote de Nuevo Coranavirus 2019 (n-CoV) una Emergencia de Salud Pública de Importancia Internacional (ESPII). Dirección General de Salud Pública, Calidad e Innovación. MSSI, 31 January 2020. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Valoracion_declaracion_emergencia_OMS_2019_nCoV.pdf (accessed on 15 January 2021).
- Moreno-Borraz, L.A.; Gimenez-López, M.; Carrera-Lasfuentes, P.; González-Pérez, E.; Ortíz-Domingo, C.; Bonafonte-Marteles, J.L.; Vicente-Gaspar, C.; Amorós de la Nieta, F.; Sastre-Heres, A.; García-Forcada, A.L.; et al. Prevalencia de infección por coronavirus SARS-CoV-2 en pacientes y profesionales de un hospital de media y larga estancia en España. Rev. Esp. Geriotr. Gerontol. 2020, 56, 75–80. [Google Scholar] [CrossRef]
- Meintrup, D.; Nowak-Machen, M.; Borgmann, S. Nine months of COVID-19 Pandemic in Europe: A Comparative Time Series Analysis of Cases and Fatalities in 35 Countries. Int. J. Environ. Res. Public Health 2021, 18, 6680. [Google Scholar] [CrossRef]
- Gras-Valentí, P.; Chico-Sánchez, P.; Algado-Selles, N.; Gimeno-Gascón, M.A.; Mora-Muriel, J.G.; Jimenez-Sepulveda, N.J.; Gómez-Sotero, I.L.; Montiel-Higuero, I.; Sánchez-Paya, J.; Rodríguez-Díaz, J.C.; et al. Estudio de sero-epidemiología de la infección por SARS-CoV-2 en profesionales sanitarios de un departamento sanitario. Enferm. Infecc. Microbiol. Clin. 2020, 39, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Nioi, M.; Napoli, P.E.; Lobina, J.; Fossarello, M.; d’Aloja, E. COVID-19 and Italian healthcare workers from the initial sacrifice to the mRNA vaccine: Pandemic chrono-history, epidemiological data, ethical dilemmas, and future challenges. Front. Public Health 2021, 8, 591900. [Google Scholar] [CrossRef] [PubMed]
- Napoli, P.E.; Nioi, M.; Fossarello, M. The “quarantine dry eye”: The lockdown for coronavirus disease 2019 and its implications for ocular surface health. Risk Manag. Healthc. Policy 2021, 14, 1629–1636. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhou, M.; Liu, F. Reason for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J. Hosp. Infect. 2020, 105, 100–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al Maskari, Z.; Al Blushi, A.; Khamis, F.; Al Tai, A.; Al Salmi, I.; Al Harthi, H.; Al Saadi, M.; Al Mughairy, A.; Gutierrez, R.; Al Blushi, Z. Characteristics of healthcare workers infected with COVID-19: A cross-sectional observational study. Int. J. Infect. Dis. 2021, 102, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Arenas, M.D.; Villar, J.; González, C.; Cao, H.; Collado, S.; Barbosa, F.; Crespo, M.; Horcajada, J.P.; Pascual, J. Protección de los profesionales sanitarios en nefrología ante la pandemia por COVID-19. Nefrología 2020, 40, 395–402. [Google Scholar] [CrossRef]
- Cioffi, A.; Rinaldi, R. COVID-19 and medical liability: A delicate balance. Med.-Leg. J. 2020, 88, 187–188. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Infection Prevention and Control for COVID-19 in Healthcare Settings—Sixth Update. 9 February 2021; ECDC: Stockholm, Sweden, 2020; Available online: https://www.ecdc.europa.eu/sites/default/files/documents/Infection-prevention-and-control-in-healthcare-settings-COVID-19_6th_update_9_Feb_2021.pdf (accessed on 15 June 2021).
- Dacosta-Urbieta, A.; Rivero-Calle, I.; Pardo-Seco, J.; Redondo-Collazo, L.; Salas, A.; Gómez-Rial, J.; Martinon-Torres, F. Seroprevalence of SARS-CoV-2 Among Pediatric Healthcare Workers in Spain. Front. Pediatr. 2020, 8, 547. [Google Scholar] [CrossRef]
- Actualización de la Situación del Centro Europeo para la Prevención y el Control de Enfermedades COVID-19 en Todo el Mundo. Available online: https://www.ecdc.europa.eu/en (accessed on 12 January 2021).
- Trullàs, J.C.; Vilardell, I.; Blasco, M.; Heredia, J. COVID-19 in health workers from the Olot Regional Hospital (Girona). Rev. Clin. Esp. 2020, 220, 529–531. [Google Scholar] [CrossRef]
- Ministerio de Sanidad. Informe Sobre la Situación de COVID-19 en Personal Sanitario en España a 21 de Mayo de 2020. Equipo COVID-19. RENAVE. CNE. CNM (ISCIII). 2020. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/COVID-19%20en%20Espa%C3%B1a.%20Situaci%C3%B3n%20en%20Sanitarios%20a%2021%20de%20mayo%20de%202020.pdf (accessed on 16 June 2021).
- Pruc, M.; Golik, D.; Szarpk Adam ISmereka, J. COVID-19 in healthcare workers. Am. J. Emerg. Med. 2021, 39, 236. [Google Scholar] [CrossRef] [PubMed]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Seroprevalence of SARS-CoV-2 antibodies and associated factors in healthcare workers: A systematic review and meta-analysis. J. Hosp. Infect. 2021, 108, 120–134. [Google Scholar] [CrossRef]
- Keeley, A.J.; Evans, C.; Colton, H.; Ankcorn, M.; Cope, A.; Bennett, T.; Giri, P.; de Silva, T.I.; Raza, M. Roll-out of SARS-CoV-2 testing for healthcare workers at a large NHS Foundation Trust in the United Kingdom, March 2020. Eurosurveillance 2020, 25, 2000433. [Google Scholar] [CrossRef] [PubMed]
- Wee, L.E.; Sim, X.Y.J.; Conceicao, E.P.; Aung, M.K.; Goh, J.Q.; Yeo, D.W.T.; Gan, W.H.; Chua, Y.Y.; Wijaya, L.; Tan, T.T.; et al. Containment of COVID-19 cases among healthcare workers: The role of surveillance, early detection, and outbreak management. Infect. Control Hosp. Epidemiol. 2020, 41, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Folgueira, M.D.; Muñoz-Ruiperez, C.; Alonso-López, M.A.; Delgado, R. SARS-CoV-2 infection in Health Care Workers in a large public hospital in Madrid, Spain, during March 2020. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Basteiro, A.L.; Moncunill, G.; Tortajada, M.; Vidal, M.; Guinovart, C.; Jiménez, A.; Santano, R.; Sanz, S.; Méndez, S.; Llupià, A.; et al. Seroprevalence of antibodies against SARS-CoV-2 among health care workers in a large Spanish reference hospital. Nat. Commun. 2020, 11, 3500. [Google Scholar] [CrossRef]
- Reusken, C.B.; Buiting, A.; Bleeker-Rovers, C.; Diederen, B.; Hooiveld, M.; Friesema, I.; Koopmans, M.; Kortbeek, T.; Lutgens, S.P.; Meijer, A.; et al. Rapid assessment of regional SARS-CoV-2 community transmission through a convenience sample of healthcare workers, the Netherlands, march 2020. Eurosurveillance 2020, 25, 2000334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suarez-Gracía, I.; Martínez de Aramayona-López, M.J.; Sáez-Vicente, A.; Lobo-Abascal, P. SARS-CoV-s infection among healthcare workers in a hospital in Madrid, Spain. J. Hosp. Infect. 2020, 106, 357–363. [Google Scholar] [CrossRef] [PubMed]
- García-Sierra, R.M.; Badia-Perich, E.; Manresa-Dominguez, J.M.; Moreno-Millán, N.; Sabaté-Cintas, V.; Romero-Martínez, M.; Moreno-Gabriel, E.; Pera, G.; Seda-Gambau, G.; Montellá-Jorana, N.; et al. Estudio descriptivo de los trabajadores de servicios sanitarios de una dirección de Atención Primaria confinados por COVID-19. Rev. Esp. Salud Pública 2020, 94, e1–e11. [Google Scholar]
- Ministerio de Sanidad. Estrategia de Detección Precoz, Vigilancia y Control de COVID-19. 2021. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/COVID19_Estrategia_vigilancia_y_control_e_indicadores.pdf (accessed on 16 August 2021).
- Napolitano, F.; Di Giuseppe, G.; Montemurro, M.V.; Molinari, A.M.; Donnarumma, G.; Arnese, A.; Pavia, M.; Angelillo, I.F. Seroprevalence of SARS-CoV-2 Antibodies in adults and healthcare workers in southern Italy. Int. J. Environ. Res. Public Health 2021, 18, 4761. [Google Scholar] [CrossRef] [PubMed]
- Stringhini, S.; Wisniak, A.; Piumatti, G.; Azman, A.S.; Lauer, S.A.; Baysson, H.; De Ridder, D.; Petrovic, D.; Schrempft, S.; Marcus, K.; et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): A population-based study. Lancet 2020, 396, 313–319. [Google Scholar] [CrossRef]
- Stubblefield, W.B.; Talbot, H.K.; Feldstein, L.R.; Tenforde, M.W.; Rasheed, M.A.; Mills, L.; Lester, S.N.; Freeman, B.; Thornbug, N.; Jones, I.D.; et al. Seroprevalence of SARS-CoV-2 Among Frontline Healthcare Personnel During the First Month of Caring for Patients With COVID-19—Nashville, Tennessee. Clin. Infect. Dis. 2021, 72, 1645–1648. [Google Scholar] [CrossRef] [PubMed]
- Mansour, M.; Leven, E.; Muellers, K.; Stone, K.; Rao-Mendu, D.; Wajnberg, A. Prevalence of SARS-CoV-2 Antibodies Among Healthcare Workers at a Tertiary Academic Hospital in New York City. J. Gen. Intern. Med. 2020, 35, 2485–2486. [Google Scholar] [CrossRef]
- Hunter, E.; Price, D.A.; Murphy, E.; van der Loeff, I.S.; Baker, K.F.; Lendrem, D.; Lendrem, C.; Schmid, M.L.; Pareja-Cebrian, L.; Welch, A.; et al. First experience of COVID-19 screening of health-care workers in England. Lancet 2020, 395, e77–e78. [Google Scholar] [CrossRef]
- Grant, J.J.; Wilmore, S.M.; McCann, N.S.; Donnelly, O.; Lai, R.W.; Kinsella, M.J.; Rochford, H.; Patel, T.; Kelsey, M.C.; Andrews, J.A. Seroprevalence of SARS-CoV-2 antibodies in healthcare workers at a London NHS Trust. Infec. Control Hosp. Epidemiol. 2021, 42, 212–214. [Google Scholar] [CrossRef]
- Alserehi, H.A.; Alqunaibet, A.M.; Al-Tawfiq, J.A.; Alharbi, N.K.; Alshukairi, A.N.; Alanazi, K.H.; Bin-Saleh, G.M.; Alshehri, A.M.; Almasoud, A.; Hashem, A.M.; et al. Seroprevalence of SARS-CoV-2 (COVID-19) among healthcare workers in Saudi Arabia: Comparing case and control hospitals. Diag. Microbiol. Infect. Dis. 2021, 99, 115273. [Google Scholar] [CrossRef]
- Galán, I.; Velasco, M.; Casas, M.L.; Goyanes, M.J.; Rodríguez-Caravaca, G.; Losa, J.E.; Noguera, C.; Castilla, V. SARS-CoV-2 Seroprevalence Among All Workers in a Teaching Hospital in Spain: Unmasking The Risk. medRxiv 2020. [Google Scholar] [CrossRef]
- Garralda-Fernandez, J.; Molero-Vilches, I.; Bermejo-Rodríguez, A.; Cano-Torres, I.; Colino-Romay, E.I.; García-Arata, I.; Jaqueti-Aroca, J.; Lillo-Rodríguez, R.; López-Lacomba, D.; Mazón-Cuadrado, L.; et al. Impact of SARS-CoV-2 pandemic among health care workers in a secondary teaching hospital in Spain. PLoS ONE 2021, 16, e0245001. [Google Scholar] [CrossRef]
- Conti, P.; Younes, A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: Clinical response to viral infection. J. Biol. Regul. Homeost. Agents 2020, 34, 339–343. [Google Scholar] [CrossRef]
- Elgendy, I.; Pepine, C.J. Why are women better protected from COVID-19: Clues for men? Sex and COVID-19. Int. J. Cardiol. 2020, 315, 105–106. [Google Scholar] [CrossRef] [PubMed]
- Lahner, E.; Dilaghi, E.; Prestigiacomo, C.; Alessio, G.; Marcellini, L.; Simmaco, M.; Santino, L.; Battista-Orsi, G.; Anibaldi, P.; Marcolongo, A.; et al. Prevalence of SARS-Cov-2 infection in Healht Workers (HWs) and diagnostic test performance: The experience of a Teaching Hospital in Central Italy. Int. J. Environ. Res. Public Health 2020, 17, 4417. [Google Scholar] [CrossRef]
- Lai, X.; Wang, M.; Qin, C.; Tan, L.; Ran, L.; Chen, D.; Zhang, H.; Shang, K.; Xia, C.; Wang, S.; et al. Coronavirus Disease 2019 (COVID-2019) Infection Among Health Care Workers and Implications for Prevention Measures in a Tertiary Hospital in Wuhan, China. JAMA Netw. Open 2020, 3, e209666. [Google Scholar] [CrossRef] [PubMed]
- Rudberg, A.S.; Havervall, S.; Månberg, A.; Jernbom Falk, A.; Aguilera, K.; Ng, H.; Gabrielsson, L.; Salomonsson, A.C.; Hanke, L.; Murrell, B.; et al. SARS-CoV-2 exposure, symptoms and seroprevalence in healthcare workers in Sweden. Nat. Commun. 2020, 11, 5064. [Google Scholar] [CrossRef]
- Ministerio de Sanidad. Situación de COVID-19 en España a 11 de Agosto de 2021. Equipo COVID-19. RENAVE. CNE. CNM (ISCIII). 2020. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/INFORMES%20COVID-19%202021/Informe%20n%C2%BA%2091%20Situaci%C3%B3n%20de%20COVID-19%20en%20Espa%C3%B1a%20a%2011%20de%20agosto%20de%202021.pdf (accessed on 9 August 2021).
- García-Montero, C.; Fraile-Martínez, O.; Bravo, C.; Torres-Carranza, D.; Sanchez-Trujillo, L.; Gómez-Lahoz, A.M.; Guijarro, L.G.; García-Honduvilla, N.; Asúnsolo, A.; Bujan, J.; et al. An Updated Review of SARS-CoV-2 Vaccines and the Importance of Effective Vaccination Programs in Pandemic Times. Vaccines 2021, 9, 433. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad. Estrategia de Vacunación Frente a COVID-19 en España a 18 de Diciembre de 2020. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/covid19/docs/COVID-19_Actualizacion1_EstrategiaVacunacion.pdf (accessed on 15 December 2021).
- Gallè, F.; Sabella, E.A.; Roma, P.; De Giglio, O.; Caggiano, G.; Tafuri, S.; Da Molin, G.; Ferracuti, S.; Montagna, M.T.; Liguori, G.; et al. Knowledge and Acceptance of COVID-19 Vaccination among Undergraduate Students from Central and Southern Italy. Vaccines 2021, 9, 638. [Google Scholar] [CrossRef]
| n = 2858 | % | |
|---|---|---|
| Age, Mean (SD) Minimum-maximum | 38.99 ± 9.34 18–69 | |
| Sex | ||
| Male | 860 | 30.1 |
| Female | 1988 | 69.9 |
| Age group | ||
| 18–34 | 1000 | 35.0 |
| 35–49 | 1451 | 50.8 |
| >50 | 407 | 14.3 |
| COVID-19 exposure service | ||
| No risk | 1324 | 46.3 |
| Risk | 1534 | 53.7 |
| Emergency | 294 | 19.2 |
| Intensive care | 197 | 12.8 |
| Internal | 307 | 20.0 |
| Medicine primary care | 736 | 48.0 |
| Professional category | ||
| Doctors | 739 | 25.9 |
| Nurses | 970 | 33.9 |
| Other health personnel | 642 | 22.5 |
| Non-health staff | 507 | 17.7 |
| Department | ||
| Specialized | 2122 | 74.2 |
| Primary | 736 | 25.8 |
| AIDT * | ||
| Request | 1582 | 55.4 |
| No request | 1276 | 44.6 |
| AIDT result * | ||
| Positive | 277 | 9.7 |
| Temporal distribution result | ||
| March–June 2020 | 21 | 0.7 |
| July–December 2020 | 126 | 4.4 |
| January–April 2021 | 139 | 4.8 |
| Evaluated (n) 1582/2858 | % 55.4 | ORc 95% CI | ORa 95% CI | p * Value | |
|---|---|---|---|---|---|
| Sex | |||||
| Male (n = 860) | 453 | 52.7 | Reference | Reference | 0.059 |
| Female (n = 1988) | 1129 | 56.8 | 1.16 [0.99–1.37] | 1.15 [0.97–1.36] | |
| Age group | 0.389 | ||||
| 18–34 (n = 1000) | 563 | 56.3 | 1.21 [0.95–1.54] | 1.17 [0.93–1.47] | |
| 35–49 (n = 1451) | 806 | 55.5 | 1.18 [0.94–1.47] | 1.13 [0.93–1.14] | |
| >50 (n = 407) | 213 | 52.3 | Reference | Reference | |
| COVID-19 exposure service | 0.001 | ||||
| No risk (n = 1324) | 685 | 51.7 | Reference | Reference | |
| Risk (n = 1534) | 897 | 58.5 | 1.27 [0.99–1.65] | 1.13 [1.05–1.21] | |
| Emergency (n = 294) | 170 | 57.8 | 1.30 [1.01–1.69] | 1.28 [0.99–1.65] | 0.001 |
| Intensive medicine (n = 197) | 93 | 47.2 | 0.83 [0.61–1.12] | 0.81 [0.59–1.09] | |
| Internal medicine (n = 307) | 185 | 60.3 | 1.41 [1.09–1.82] | 1.38 [1.07–1.79] | |
| Primary care (n = 736) | 449 | 61.0 | 1.46 [1.21–1.76] | 1.45 [1.21–1.75] | |
| Professional category | |||||
| Doctors (n = 739) | 419 | 56.7 | 1.24 [0.98–1.55] | 1.25 [0.99–1.57] | 0.088 |
| Nurses (n = 970) | 557 | 57.4 | 1.32 [1.06–1.64] | 1.29 [1.04–1.60] | |
| Other health personnel (n = 642) | 347 | 54.0 | 1.19 [0.94–1.52] | 1.12 [0.89–1.52] | |
| Non-health personnel (n = 507) | 259 | 51.1 | Reference | Reference | |
| Department | |||||
| Specialized (n = 2122) | 1133 | 53.4 | Reference | Reference | 0.001 |
| Primary (n = 736) | 449 | 61.0 | 1.36 [1.15–1.62] | 1.48 [1.23–1.79] |
| Positive Cases (n) 277/2858 | % 9.7 | ORc 95% CI | ORa 95% CI | p * Value | |
|---|---|---|---|---|---|
| Sex | 0.269 | ||||
| Male (n = 860) | 84 | 9.8 | Reference | Reference | |
| Female (n = 1988) | 193 | 9.7 | 0.90 [0.68–1.20] | 0.89 [0.67–1.18] | |
| Age group | |||||
| 18–34 (n = 1000) | 126 | 12.6 | 1.98 [1.26–3.11] | 1.94 [1.22–3.07] | 0.001 |
| 35–49 (n = 1451) | 124 | 8.5 | 1.25 [0.80–1.95] | 1.22 [0.77–1.91] | |
| >50 (n = 407) | 27 | 6.6 | Reference | Reference | |
| COVID-19 exposure service | 0.010 | ||||
| No risk (n = 1324) | 102 | 7.7 | Reference | Reference | |
| Risk (n = 1534) | 175 | 11.4 | 1.38 [1.06–1.81] | 1.23 [1.02–1.79] | |
| Emergency (n = 294) | 41 | 13.9 | 1.81 [1.20–2.73] | 1.78 [1.11–2.70] | 0.001 |
| Intensive medicine (n = 197) | 21 | 10.7 | 1.66 [0.98–2.83] | 1.52 [0.82–2.41] | |
| Internal medicine (n = 307) | 50 | 16.3 | 2.11 [1.43–3.11] | 1.82 [1.22–2.70] | |
| Primary care (n = 736) | 63 | 8.6 | 0.93 [0.66–1.31] | 0.85 [0.58–1.23] | |
| Professional category | 0.001 | ||||
| Doctors (n = 739) | 50 | 6.8 | 0.76 [0.48–1.20] | 0.77 [0.48–1.22] | |
| Nurses (n = 970) | 117 | 12.1 | 1.50 [1.00–2.23] | 1.34 [0.88–2.03] | |
| Other health personnel (n = 642) | 71 | 11.1 | 1.45 [0.94–2.22] | 1.32 [0.83–2.08] | |
| Non-health personnel (n = 507) | 39 | 7.7 | Reference | Reference | |
| Department | 0.021 | ||||
| Specialized (n = 2122) | 214 | 10.1 | Reference | Reference | |
| Primary (n = 736) | 63 | 8.6 | 0.70 [0.51–095] | 0.69 [0.51–0.94] |
| March–June 2020 | July–December 2020 | January–April 2021 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Positive n = 21/2858 | % (0.7) | p * Value | Positive n = 126/2858 | % (4.4) | p * Value | Positive n = 139/2858 | % (4.8) | p * Value | |
| Sex | 0.172 | ||||||||
| Male (n = 860) | 7 | 0.8 | 0.672 | 32 | 3.7 | 0.665 | 49 | 5.7 | |
| Female (n = 1988) | 14 | 0.7 | 94 | 4.7 | 90 | 4.5 | |||
| Age group | 0.296 | ||||||||
| 18–34 (n = 1000) | 10 | 1.0 | 0.016 | 64 | 6.4 | 0.005 | 57 | 5.7 | |
| 35–49 (n = 1451) | 8 | 0.6 | 50 | 3.4 | 69 | 4.8 | |||
| >50 (n = 407) | 3 | 0.7 | 12 | 2.9 | 13 | 3.2 | |||
| COVID-19 exposure service | 0.921 | ||||||||
| No risk (n = 1324) | 9 | 0.7 | 0.978 | 35 | 2.6 | 0.001 | 59 | 4.5 | |
| Risk (n = 1534) | 12 | 0.8 | 91 | 5.9 | 80 | 5.2 | |||
| Emergency (n = 294) | 5 | 1.7 | 0.675 | 20 | 6.8 | 0.001 | 19 | 6.5 | 0.110 |
| Intensive medicine (n = 197) | - | - | 8 | 4.1 | 13 | 6.6 | |||
| Internal medicine (n = 307) | 1 | 0.3 | 30 | 9.8 | 22 | 7.2 | |||
| Primary care (n = 736) | 6 | 0.8 | 33 | 4.5 | 26 | 3.5 | |||
| Professional category | 0.096 | ||||||||
| Doctors (n = 739) | 5 | 0.7 | 0.078 | 25 | 3.4 | 0.001 | 22 | 3.0 | |
| Nurses (n = 970) | 9 | 0.9 | 55 | 5.7 | 58 | 6.0 | |||
| Other health personnel (n = 642) | 3 | 0.5 | 37 | 5.8 | 32 | 5.0 | |||
| Non-health personnel (n = 507) | 4 | 0.8 | 9 | 1.8 | 27 | 5.3 | |||
| Department | 0.029 | ||||||||
| Specialized (n = 2122) | 15 | 0.7 | 0.990 | 93 | 4.4 | 0.001 | 113 | 5.3 | |
| Primary (n = 736) | 6 | 0.8 | 33 | 4.5 | 26 | 3.5 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez de Limia Ramírez, K.; Ruiz-Robledillo, N.; Duro-Torrijos, J.L.; García-Román, V.; Albaladejo-Blázquez, N.; Ferrer-Cascales, R. Prevalence of SARS-CoV-2 Infection in a Sample of Health Workers in Two Health Departments of the Valencian Community in Spain. Int. J. Environ. Res. Public Health 2022, 19, 66. https://doi.org/10.3390/ijerph19010066
Rodríguez de Limia Ramírez K, Ruiz-Robledillo N, Duro-Torrijos JL, García-Román V, Albaladejo-Blázquez N, Ferrer-Cascales R. Prevalence of SARS-CoV-2 Infection in a Sample of Health Workers in Two Health Departments of the Valencian Community in Spain. International Journal of Environmental Research and Public Health. 2022; 19(1):66. https://doi.org/10.3390/ijerph19010066
Chicago/Turabian StyleRodríguez de Limia Ramírez, Kenan, Nicolás Ruiz-Robledillo, José Luis Duro-Torrijos, Vicente García-Román, Natalia Albaladejo-Blázquez, and Rosario Ferrer-Cascales. 2022. "Prevalence of SARS-CoV-2 Infection in a Sample of Health Workers in Two Health Departments of the Valencian Community in Spain" International Journal of Environmental Research and Public Health 19, no. 1: 66. https://doi.org/10.3390/ijerph19010066
APA StyleRodríguez de Limia Ramírez, K., Ruiz-Robledillo, N., Duro-Torrijos, J. L., García-Román, V., Albaladejo-Blázquez, N., & Ferrer-Cascales, R. (2022). Prevalence of SARS-CoV-2 Infection in a Sample of Health Workers in Two Health Departments of the Valencian Community in Spain. International Journal of Environmental Research and Public Health, 19(1), 66. https://doi.org/10.3390/ijerph19010066







