Psychological Wellbeing, Worry, and Resilience-Based Coping during COVID-19 in Relation to Sleep Quality
Abstract
:1. Introduction
1.1. Main Effect Model: Psychological Wellbeing
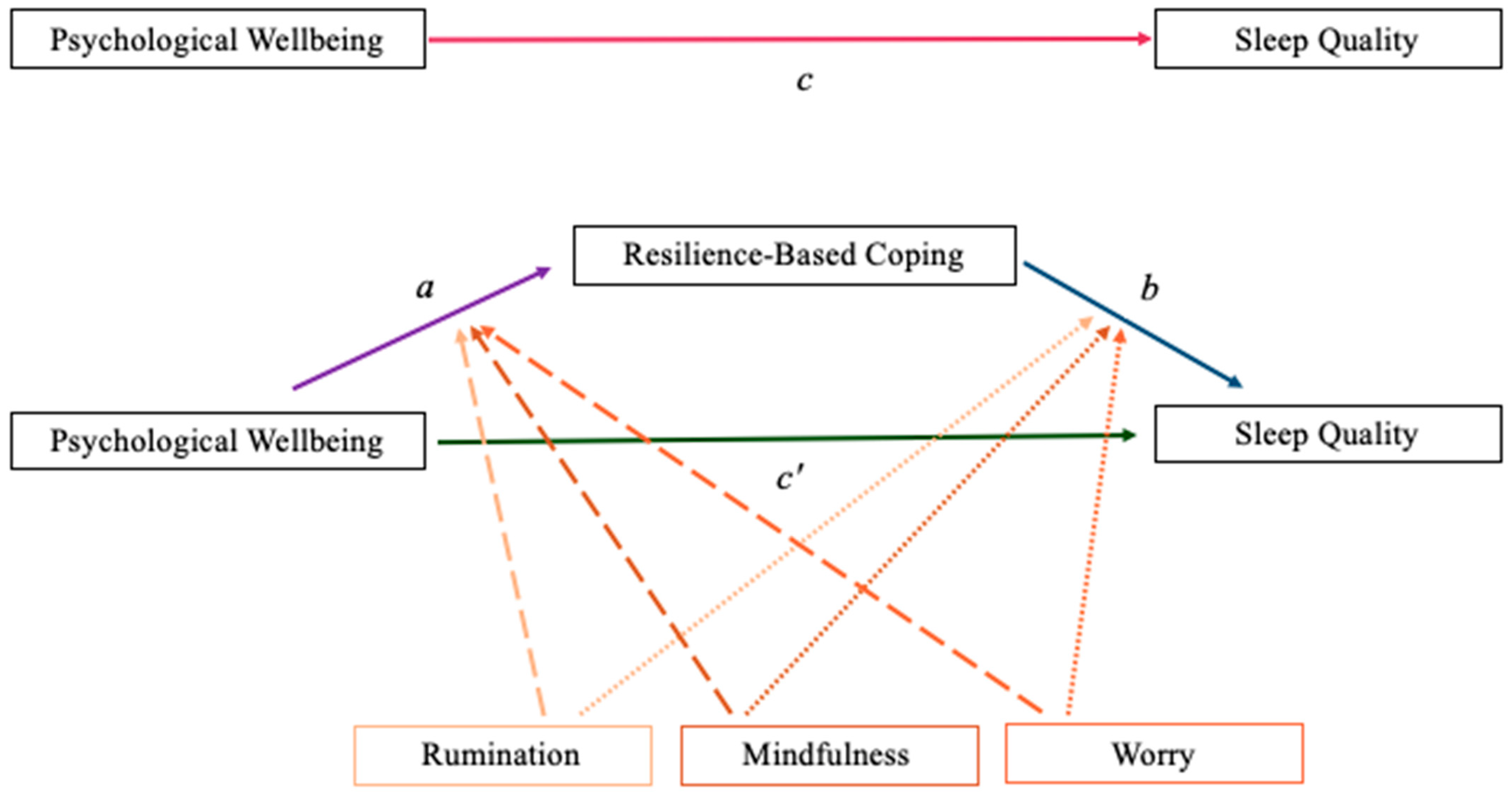
1.2. Mediation Model: Resilience-Based Coping
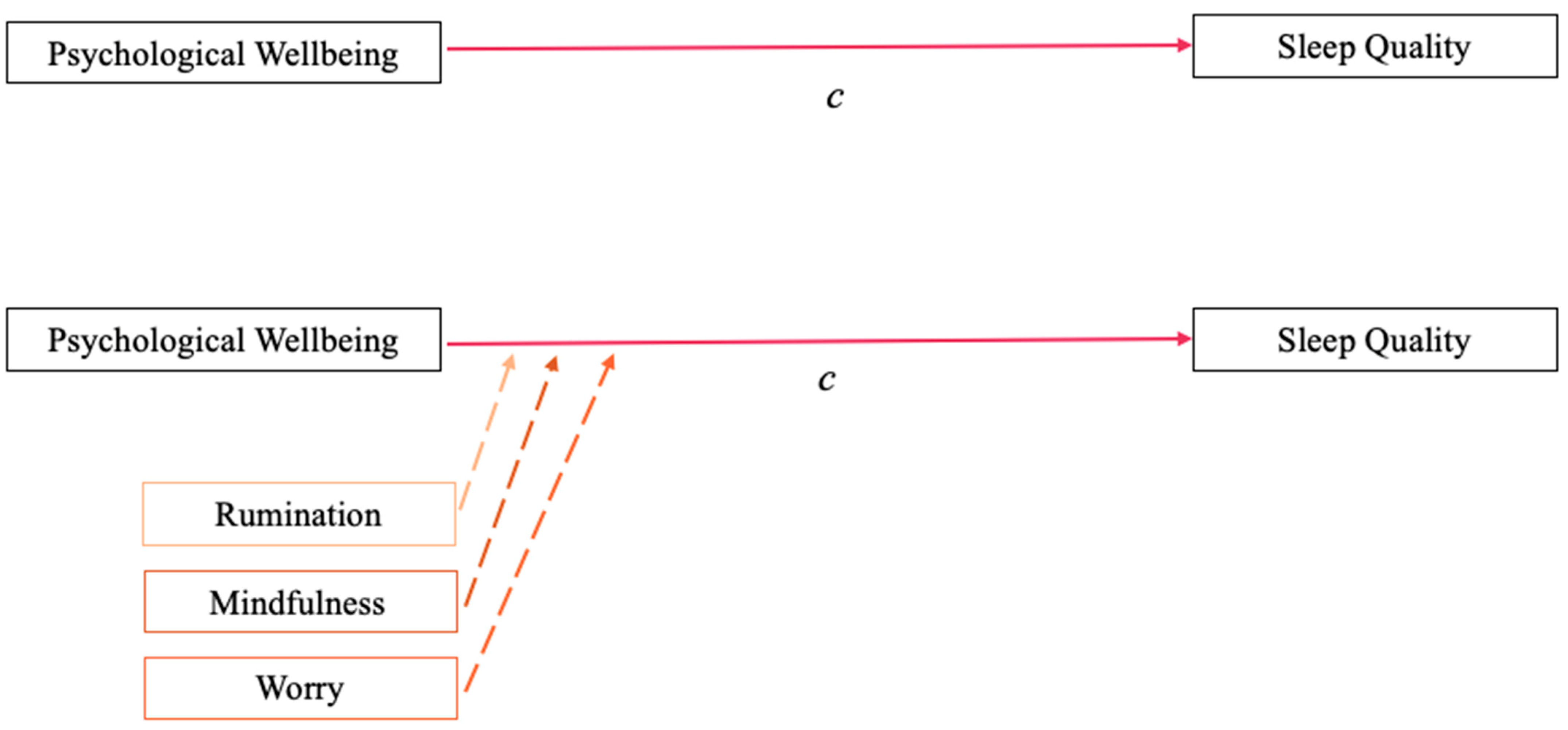
1.3. Moderation Model: Cognitive Approaches
2. Materials and Methods
2.1. Procedures and Participants
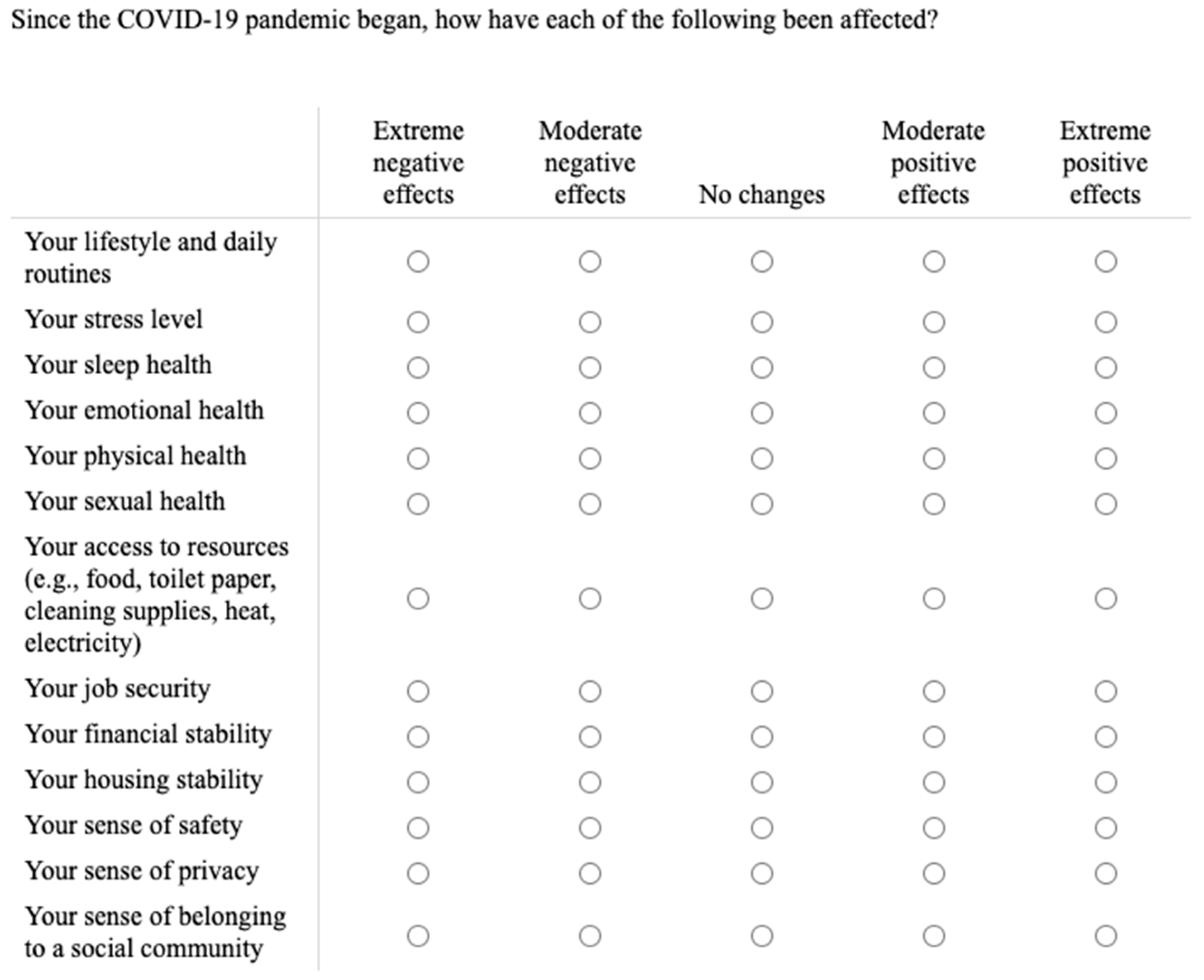
2.2. Measures
2.3. Data Analysis
3. Results
3.1. Main Effect Model Analysis and Mediation Model Analysis
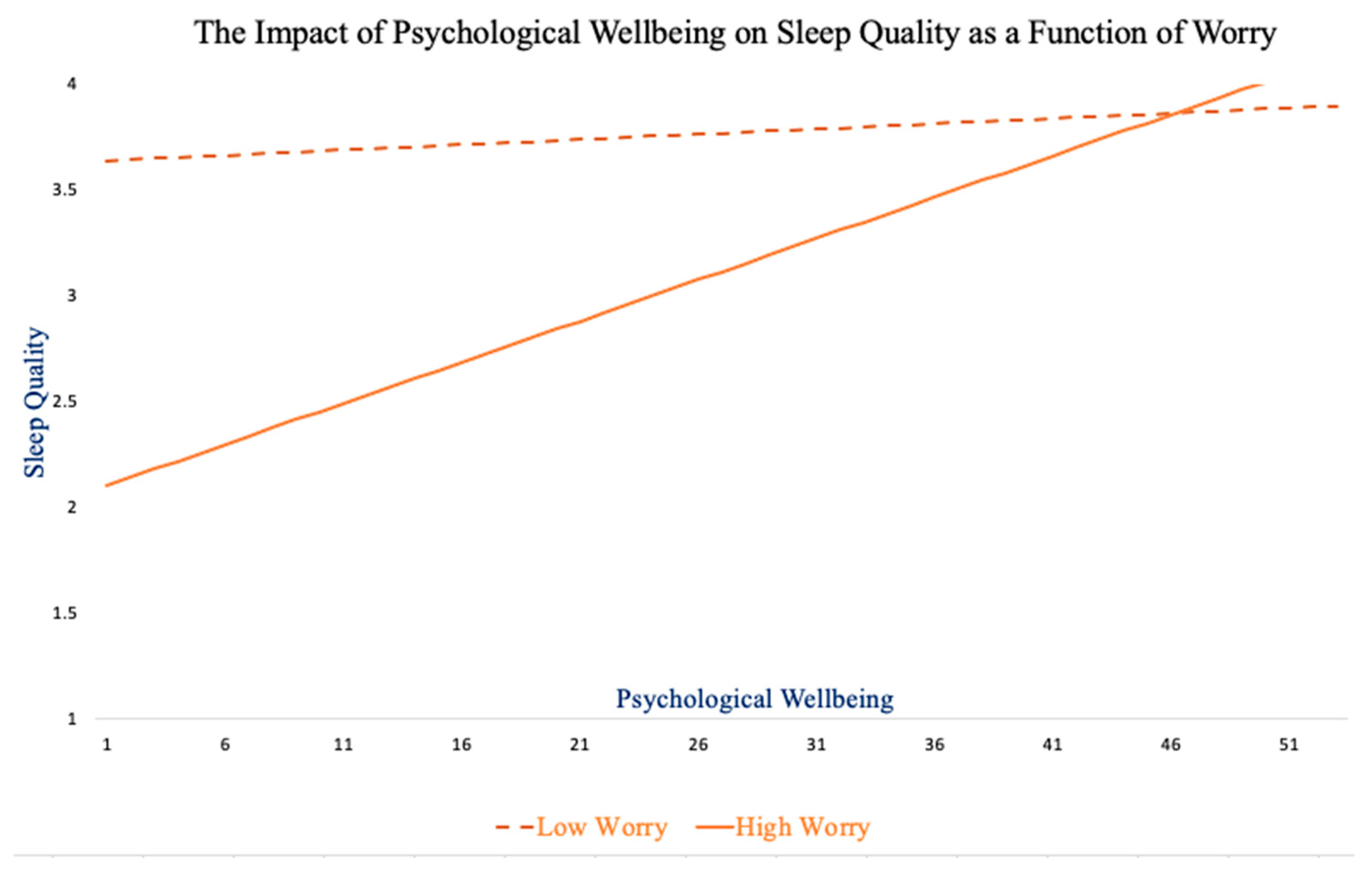
3.2. Analyses of Cognitive Approach Moderating the Impact of Psychological Wellbeing on SQ
3.3. Moderated Mediation Model Analyses
4. Discussion
4.1. Main Effect Model and Mediation Model
4.2. Moderation Model
4.3. Future Directions and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sleep Quality and Quality of Life in Adults with Type 2 Diabetes-Faith S. Luyster, Jacqueline Dunbar-Jacob. 2011. Available online: https://journals.sagepub.com/doi/abs/10.1177/0145721711400663 (accessed on 27 October 2021).
- Shao, M.-F.; Chou, Y.-C.; Yeh, M.-Y.; Tzeng, W.-C. Sleep Quality and Quality of Life in Female Shift-Working Nurses. J. Adv. Nurs. 2010, 66, 1565–1572. [Google Scholar] [CrossRef]
- Tel, H. Sleep Quality and Quality of Life among the Elderly People. Neurol. Psychiatry Brain Res. 2013, 19, 48–52. [Google Scholar] [CrossRef]
- Zeitlhofer, J.; Schmeiser-Rieder, A.; Tribl, G.; Rosenberger, A.; Bolitschek, J.; Kapfhammer, G.; Saletu, B.; Katschnig, H.; Holzinger, B.; Popovic, R.; et al. Sleep and Quality of Life in the Austrian Population. Acta Neurol. Scand. 2000, 102, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Grover, S.; Basu, A.; Krishnan, V.; Tripathi, A.; Subramanyam, A.; Nischal, A.; Hussain, A.; Mehra, A.; Ambekar, A.; et al. Changes in Sleep Pattern and Sleep Quality during COVID-19 Lockdown. Indian J. Psychiatry 2020, 62, 370–378. [Google Scholar] [CrossRef]
- Gargiulo, A.T.; Peterson, L.M.; Grafe, L.A. Stress, Coping, Resilience, and Sleep during the COVID-19 Pandemic: A Representative Survey Study of US Adults. Brain Behav. 2021, 11, e2384. [Google Scholar] [CrossRef]
- Kocevska, D.; Blanken, T.F.; Van Someren, E.J.W.; Rösler, L. Sleep Quality during the COVID-19 Pandemic: Not One Size Fits All. Sleep Med. 2020, 76, 86–88. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L. Pandemic Fatigue And Clinical Nurses’ Mental Health, Sleep Quality And Job Contentment During The COVID-19 Pandemic: The Mediating Role Of Resilience. J. Nurs. Manag. 2021, 29, 1992–2001. [Google Scholar] [CrossRef]
- Jahrami, H.; BaHammam, A.S.; Bragazzi, N.L.; Saif, Z.; Faris, M.; Vitiello, M.V. Sleep Problems during the COVID-19 Pandemic by Population: A Systematic Review and Meta-Analysis. J. Clin. Sleep Med. 2021, 17, 299–313. [Google Scholar] [CrossRef] [PubMed]
- Werner, A.; Kater, M.-J.; Schlarb, A.A.; Lohaus, A. Sleep and Stress in Times of the COVID-19 Pandemic: The Role of Personal Resources. Appl. Psychol. Health Well-Being 2021, 13, 935–951. [Google Scholar] [CrossRef] [PubMed]
- Zacher, H.; Rudolph, C.W. Individual Differences and Changes in Subjective Wellbeing during the Early Stages of the COVID-19 Pandemic. Am. Psychol. 2021, 76, 50. [Google Scholar] [CrossRef]
- Li, Y.; Gu, S.; Wang, Z.; Li, H.; Xu, X.; Zhu, H.; Deng, S.; Ma, X.; Feng, G.; Wang, F.; et al. Relationship Between Stressful Life Events and Sleep Quality: Rumination as a Mediator and Resilience as a Moderator. Front. Psychiatry 2019, 10, 348. [Google Scholar] [CrossRef] [Green Version]
- Casagrande, M.; Forte, G.; Tambelli, R.; Favieri, F. The Coronavirus Pandemic: A Possible Model of the Direct and Indirect Impact of the Pandemic on Sleep Quality in Italians. Nat. Sci. Sleep 2021, 13, 191–199. [Google Scholar] [CrossRef]
- Appleton, S.L.; Melaku, Y.A.; Reynolds, A.C.; Gill, T.K.; de Batlle, J.; Adams, R.J. Multidimensional Sleep Health Is Associated with Mental Well-Being in Australian Adults. J. Sleep Res. 2021, e13477. [Google Scholar] [CrossRef]
- Giuntella, O.; Hyde, K.; Saccardo, S.; Sadoff, S. Lifestyle and Mental Health Disruptions during COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2016632118. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Lin, Y.; Hu, Z.; Alias, H.; Wong, L.P. Practice of New Normal Lifestyles, Economic and Social Disruption, and Level of Happiness Among General Public in China in the Post-COVID-19 Era. Risk Manag. Healthc. Policy 2021, 14, 3383–3393. [Google Scholar] [CrossRef]
- Alfonsi, V.; Gorgoni, M.; Scarpelli, S.; Zivi, P.; Sdoia, S.; Mari, E.; Fraschetti, A.; Ferlazzo, F.; Giannini, A.M.; De Gennaro, L. COVID-19 Lockdown and Poor Sleep Quality: Not the Whole Story. J. Sleep Res. 2021, 30, e13368. [Google Scholar] [CrossRef] [PubMed]
- Vemprala, N.; Bhatt, P.; Valecha, R.; Rao, H.R. Emotions During the COVID-19 Crisis: A Health Versus Economy Analysis of Public Responses. Am. Behav. Sci. 2021, 65, 1972–1989. [Google Scholar] [CrossRef]
- Carter, S.J.; Baranauskas, M.N.; Fly, A.D. Considerations for Obesity, Vitamin D, and Physical Activity Amid the COVID-19 Pandemic. Obesity 2020, 28, 1176–1177. [Google Scholar] [CrossRef] [PubMed]
- Jacob, L.; Smith, L.; Butler, L.; Barnett, Y.; Grabovac, I.; McDermott, D.; Armstrong, N.; Yakkundi, A.; Tully, M.A. Challenges in the Practice of Sexual Medicine in the Time of COVID-19 in the United Kingdom. J. Sex. Med. 2020, 17, 1229–1236. [Google Scholar] [CrossRef]
- Sarkis, J. Supply Chain Sustainability: Learning from the COVID-19 Pandemic. Int. J. Oper. Prod. Manag. 2020, 41, 63–73. [Google Scholar] [CrossRef]
- Zurayk, R. Pandemic and Food Security: A View from the Global South. J. Agric. Food Syst. Community Dev. 2020, 9, 17–21. [Google Scholar] [CrossRef]
- Leung, J.; Chung, J.Y.C.; Tisdale, C.; Chiu, V.; Lim, C.C.W.; Chan, G. Anxiety and Panic Buying Behaviour during COVID-19 Pandemic—A Qualitative Analysis of Toilet Paper Hoarding Contents on Twitter. Int. J. Environ. Res. Public Health 2021, 18, 1127. [Google Scholar] [CrossRef]
- Chakraborti, R.; Roberts, G. Learning to Hoard: The Effects of Preexisting and Surprise Price-Gouging Regulation During the COVID-19 Pandemic. J. Consum. Policy 2021, 44, 507–529. [Google Scholar] [CrossRef] [PubMed]
- Ambrose, A.; Baker, W.; Sherriff, G.; Chambers, J. Cold Comfort: Covid-19, Lockdown and the Coping Strategies of Fuel Poor Households. Energy Rep. 2021, 7, 5589–5596. [Google Scholar] [CrossRef]
- Karpman, M.; Zuckerman, S.; Gonzalez, D.; Kenney, G.M. The COVID-19 Pandemic Is Straining Families’ Abilities to Afford Basic Needs: Low-Income and Hispanic Families the Hardest Hit. Available online: https://www.urban.org/sites/default/files/publication/102124/the-covid-19-pandemic-is-straining-families-abilities-to-afford-basic-needs_5.pdf (accessed on 18 December 2021).
- Pacheco, T.; Coulombe, S.; Khalil, C.; Meunier, S.; Doucerain, M.; Auger, É.; Cox, E. Job Security and the Promotion of Workers’ Wellbeing in the Midst of the COVID-19 Pandemic: A Study with Canadian Workers One to Two Weeks after the Initiation of Social Distancing Measures. Int. J. Wellbeing 2020, 10, 58–76. [Google Scholar] [CrossRef]
- Folayan, M.O.; Ibigbami, O.; El Tantawi, M.; Brown, B.; Aly, N.M.; Ezechi, O.; Abeldaño, G.F.; Ara, E.; Ayanore, M.A.; Ellakany, P.; et al. Factors Associated with Financial Security, Food Security and Quality of Daily Lives of Residents in Nigeria during the First Wave of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 7925. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.; Grigsby-Toussaint, D. Housing Stability and the Residential Context of the COVID-19 Pandemic. Cities Health 2020, 1–3. [Google Scholar] [CrossRef]
- Bradbury-Jones, C.; Isham, L. The Pandemic Paradox: The Consequences of COVID-19 on Domestic Violence. J. Clin. Nurs. 2020. [Google Scholar] [CrossRef] [Green Version]
- Zhang, B.; Kreps, S.; McMurry, N.; McCain, R.M. Americans’ Perceptions of Privacy and Surveillance in the COVID-19 Pandemic. PLoS ONE 2020, 15, e0242652. [Google Scholar] [CrossRef] [PubMed]
- Saiz, J.; González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Abad, A.; Salazar, M.; Muñoz, M. The Role of the Sense of Belonging During the Alarm Situation and Return to the New Normality of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Psychol. Stud. 2021, 66, 326–336. [Google Scholar] [CrossRef] [PubMed]
- Matthews, K.A.; Hall, M.H.; Cousins, J.; Lee, L. Getting a Good Night’s Sleep in Adolescence: Do Strategies for Coping with Stress Matter? Behav. Sleep Med. 2016, 14, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Faircloth, A.L. Resilience as a Mediator of the Relationship Between Negative Life Events and Psychological Well-Being. Ph.D. Thesis, Georgia Southern University, Statesboro, GA, USA, 2017. [Google Scholar]
- Xie, Y.; Kong, Y.; Yang, J.; Chen, F. Perfectionism, Worry, Rumination, and Distress: A Meta-Analysis of the Evidence for the Perfectionism Cognition Theory. Personal. Individ. Differ. 2019, 139, 301–312. [Google Scholar] [CrossRef]
- Manigault, A.W.; Zoccola, P.M. Rumination. In The Wiley Encyclopedia of Health Psychology; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2020; pp. 557–567. [Google Scholar] [CrossRef]
- Müller, D.; Sabine, S.; Vocks, S.; Schneider, S.; Teismann, T. Predictive Importance of Antenatal Depressive Rumination and Worrying for Maternal–Foetal Attachment and Maternal Well-Being. Cogn. Ther. Res. 2016, 40, 565–576. [Google Scholar] [CrossRef]
- Baer, R.; Lykins, E.; Peters, J. Mindfulness and Self-Compassion as Predictors of Psychological Wellbeing in Long-Term Meditators and Nonmeditators. J. Posit. Psychol. 2012, 7, 230–238. [Google Scholar] [CrossRef]
- Davis, T.J.; Morris, M.; Drake, M.M. The Moderation Effect of Mindfulness on the Relationship between Adult Attachment and Wellbeing. Personal. Individ. Differ. 2016, 96, 115–121. [Google Scholar] [CrossRef]
- Auer, E.M.; Behrend, T.S.; Collmus, A.B.; Landers, R.N.; Miles, A.F. Pay for Performance, Satisfaction and Retention in Longitudinal Crowdsourced Research. PLoS ONE 2021, 16, e0245460. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Badahdah, A.M.; Khamis, F.; Al, M.N. Sleep Quality among Health Care Workers during the COVID-19 Pandemic. J. Clin. Sleep Med. 2020, 16, 1635. [Google Scholar] [CrossRef]
- Carney, C.E.; Buysse, D.J.; Ancoli-Israel, S.; Edinger, J.D.; Krystal, A.D.; Lichstein, K.L.; Morin, C.M. The Consensus Sleep Diary: Standardizing Prospective Sleep Self-Monitoring. Sleep 2012, 35, 287–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tousignant, O.H.; Taylor, N.D.; Suvak, M.K.; Fireman, G.D. Effects of Rumination and Worry on Sleep. Behav. Ther. 2019, 50, 558–570. [Google Scholar] [CrossRef]
- Online Survey Software | Qualtrics Survey Solutions. Available online: https://suffolk.co1.qualtrics.com/jfe/preview/SV_e8S47khxxP4c7LD/BL_b1pgMkWQmSm4uPj?Q_SurveyVersionID= (accessed on 18 December 2021).
- Dupuy, H. The Psychological General Well-Being (PGWB) Index. In Assessment of Quality of Life in Clinical Trials of Cardiovascular Therapies; Elsevier: Amsterdam, The Netherlands, 1984; pp. 170–183. [Google Scholar]
- Grossi, E.; Groth, N.; Mosconi, P.; Cerutti, R.; Pace, F.; Compare, A.; Apolone, G. Development and Validation of the Short Version of the Psychological General Well-Being Index (PGWB-S). Health Qual Life Outcomes 2006, 4, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Sinclair, V.; Wallston, K.; Sinclair, V.G.; Wallston, K.A. The Development and Psychometric Evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Fung, S. Validity of the Brief Resilience Scale and Brief Resilient Coping Scale in a Chinese Sample. Int. J. Environ. Res. Public Health 2020, 17, 1265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nolen-Hoeksema, S. Responses to Depression and Their Effects on the Duration of Depressive Episodes. J. Abnorm. Psychol. 1991, 100, 569–582. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksema, S.; Wisco, B.E.; Lyubomirsky, S. Rethinking Rumination. Perspect. Psychol. Sci. 2008, 3, 400–424. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Strauss, C.; Crane, C.; Barnhofer, T.; Karl, A.; Cavanagh, K.; Kuyken, W. Examining the Factor Structure of the 39-Item and 15-Item Versions of the Five Facet Mindfulness Questionnaire Before and After Mindfulness-Based Cognitive Therapy for People With Recurrent Depression. Psychol. Assess. 2016, 28, 791–802. [Google Scholar] [CrossRef] [Green Version]
- Christopher, M.S.; Neuser, N.J.; Michael, P.G.; Baitmangalkar, A. Exploring the Psychometric Properties of the Five Facet Mindfulness Questionnaire. Mindfulness 2012, 3, 124–131. [Google Scholar] [CrossRef]
- Carpenter, J.K.; Conroy, K.; Gomez, A.F.; Curren, L.C.; Hofmann, S.G. The Relationship Between Trait Mindfulness and Affective Symptoms: A Meta-Analysis of the Five Facet Mindfulness Questionnaire (FFMQ). Clin. Psychol. Rev. 2019, 74, 101785. [Google Scholar] [CrossRef] [PubMed]
- Meyer, T.J.; Miller, M.L.; Metzger, R.L.; Borkovec, T.D. Development and Validation of the Penn State Worry Questionnaire. Behav. Res. Ther. 1990, 28, 487–495. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical Power Analyses Using G*Power 3.1: Tests for Correlation and Regression Analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baron, R.M.; Kenny, D.A. The Moderator–Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations. J. Personal. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Monte Carlo Method for Mediation. Available online: http://www.quantpsy.org/medmc/medmc.htm (accessed on 30 October 2021).
- Du, C.; Zan, M.C.H.; Cho, M.J.; Fenton, J.I.; Hsiao, P.Y.; Hsiao, R.; Keaver, L.; Lai, C.-C.; Lee, H.; Ludy, M.-J.; et al. Increased Resilience Weakens the Relationship between Perceived Stress and Anxiety on Sleep Quality: A Moderated Mediation Analysis of Higher Education Students from 7 Countries. Clocks Sleep 2020, 2, 334–353. [Google Scholar] [CrossRef]
- Pinto, J.; van Zeller, M.; Amorim, P.; Pimentel, A.; Dantas, P.; Eusébio, E.; Neves, A.; Pipa, J.; Santa Clara, E.; Santiago, T.; et al. Sleep Quality in Times of Covid-19 Pandemic. Sleep Med. 2020, 74, 81–85. [Google Scholar] [CrossRef]
- Lin, Y.N.; Liu, Z.R.; Li, S.Q.; Li, C.X.; Zhang, L.; Li, N.; Sun, X.W.; Li, H.P.; Zhou, J.P.; Li, Q.Y. Burden of Sleep Disturbance During COVID-19 Pandemic: A Systematic Review. Nat. Sci. Sleep 2021, 13, 933–966. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.M. Sleep and Wellbeing, Now and in the Future. Int. J. Environ. Res. Public Health 2020, 17, 2883. [Google Scholar] [CrossRef] [PubMed]
- Saalwirth, C.; Leipold, B. Well-Being and Sleep in Stressful Times of the COVID-19 Pandemic: Relations to Worrying and Different Coping Strategies. Stress Health 2021, 37, 973–985. [Google Scholar] [CrossRef]
- Koch, T.; Liedl, A.; Takano, K.; Ehring, T. Daily Worry in Trauma-Exposed Afghan Refugees: Relationship with Affect and Sleep in a Study Using Ecological Momentary Assessment. Cogn. Ther. Res. 2020, 44, 645–658. [Google Scholar] [CrossRef]
- Wright, L.; Steptoe, A.; Fancourt, D. Are Adversities and Worries during the COVID-19 Pandemic Related to Sleep Quality? Longitudinal Analyses of 46,000 UK Adults. PLoS ONE 2021, 16, e0248919. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.S.; Jamal-Orozco, N.; Hallion, L.S. Dissociable Associations of Facets of Mindfulness with Worry, Rumination, and Transdiagnostic Perseverative Thought. Mindfulness 2021, 1–12. [Google Scholar] [CrossRef]
- Hyun, S.; Hahm, H.C.; Wong, G.T.F.; Zhang, E.; Liu, C.H. Psychological Correlates of Poor Sleep Quality among U.S. Young Adults during the COVID-19 Pandemic. Sleep Med. 2021, 78, 51–56. [Google Scholar] [CrossRef]
- Marini, C.M.; Wilson, S.J.; Nah, S.; Martire, L.M.; Sliwinski, M.J. Rumination and Sleep Quality Among Older Adults: Examining the Role of Social Support. J. Gerontol. Ser. B 2021, 76, 1948–1959. [Google Scholar] [CrossRef] [PubMed]
- Roberts, L.R.; Solomon, S.; Renati, S.J.; Montgomery, S. Exploring Mental Health during the Initial COVID-19 Lockdown in Mumbai: Serendipity for Some Women. Int. J. Environ. Res. Public Health 2021, 18, 12542. [Google Scholar] [CrossRef] [PubMed]
- Beckwé, M.; Deroost, N.; Koster, E.H.W.; De Lissnyder, E.; De Raedt, R. Worrying and Rumination Are Both Associated with Reduced Cognitive Control. Psychol. Res. 2014, 78, 651–660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Q.-Q.; Zhou, Z.-K.; Yang, X.-J.; Kong, F.-C.; Sun, X.-J.; Fan, C.-Y. Mindfulness and Sleep Quality in Adolescents: Analysis of Rumination as a Mediator and Self-Control as a Moderator. Personal. Individ. Differ. 2018, 122, 171–176. [Google Scholar] [CrossRef]
- Cloonan, S.A.; Taylor, E.C.; Persich, M.R.; Dailey, N.S.; Killgore, W.D.S. Sleep and Resilience during the COVID-19 Pandemic; IntechOpen: London, UK, 2021. [Google Scholar] [CrossRef]

| Demographic Characteristic | n | % |
|---|---|---|
| Gender | ||
| Female | 76 | 49.7 |
| Male | 76 | 49.7 |
| Non-binary | 1 | 0.6 |
| Race | ||
| White | 125 | 81.7% |
| Asian | 9 | 5.9% |
| Black | 6 | 3.9% |
| Multiracial | 13 | 8.5% |
| Unstandardized Coefficient | Standardized Coefficient | |||
|---|---|---|---|---|
| Effect | B | Beta | t | p |
| c-path: Wellbeing → Sleep quality | 0.02 | 0.221 | 2.77 | 0.006 |
| a-path: Wellbeing → Resilience-based coping | 0.11 | 0.27 | 3.47 | <0.001 |
| b-path: Resilience-based coping → Sleep quality | 0.07 | 0.31 | 4.02 | <0.001 |
| c’-path: Wellbeing → Resilience-based coping → Sleep quality | 0.02 | 0.17 | 2.19 | 0.030 |
| Size of Effect | 95% CI | |||
|---|---|---|---|---|
| R2 | LL | UL | p | |
| Step 1 - Rumination Model | ||||
| Constant | 2.696 | 2.948 | <0.001 | |
| Step 2 - Rumination Interaction | ||||
| RUM*EBAC | 1.8% | 0.000 | 0.002 | 0.104 |
| Step 1 – Mindfulness Model | ||||
| Constant | 2.710 | 2.962 | <0.001 | |
| Step 2 – Mindfulness Interaction | ||||
| MNDFL*EBAC | 0.4% | -0.003 | 0.001 | 0.426 |
| Step 1 – Worry Model | ||||
| Constant | 2.742 | 2.998 | <0.001 | |
| Step 2 – Worry Interaction | ||||
| WOR*EBAC | 3.2% | 0.000 | 0.002 | 0.028 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tousignant, O.H.; Hopkins, S.W.; Stark, A.M.; Fireman, G.D. Psychological Wellbeing, Worry, and Resilience-Based Coping during COVID-19 in Relation to Sleep Quality. Int. J. Environ. Res. Public Health 2022, 19, 50. https://doi.org/10.3390/ijerph19010050
Tousignant OH, Hopkins SW, Stark AM, Fireman GD. Psychological Wellbeing, Worry, and Resilience-Based Coping during COVID-19 in Relation to Sleep Quality. International Journal of Environmental Research and Public Health. 2022; 19(1):50. https://doi.org/10.3390/ijerph19010050
Chicago/Turabian StyleTousignant, Olivia H., Sarah W. Hopkins, Abigail M. Stark, and Gary D. Fireman. 2022. "Psychological Wellbeing, Worry, and Resilience-Based Coping during COVID-19 in Relation to Sleep Quality" International Journal of Environmental Research and Public Health 19, no. 1: 50. https://doi.org/10.3390/ijerph19010050
APA StyleTousignant, O. H., Hopkins, S. W., Stark, A. M., & Fireman, G. D. (2022). Psychological Wellbeing, Worry, and Resilience-Based Coping during COVID-19 in Relation to Sleep Quality. International Journal of Environmental Research and Public Health, 19(1), 50. https://doi.org/10.3390/ijerph19010050






