The Association between Parenting Confidence and Later Child Mental Health in the Area Affected by the Fukushima Nuclear Disaster: The Fukushima Health Management Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
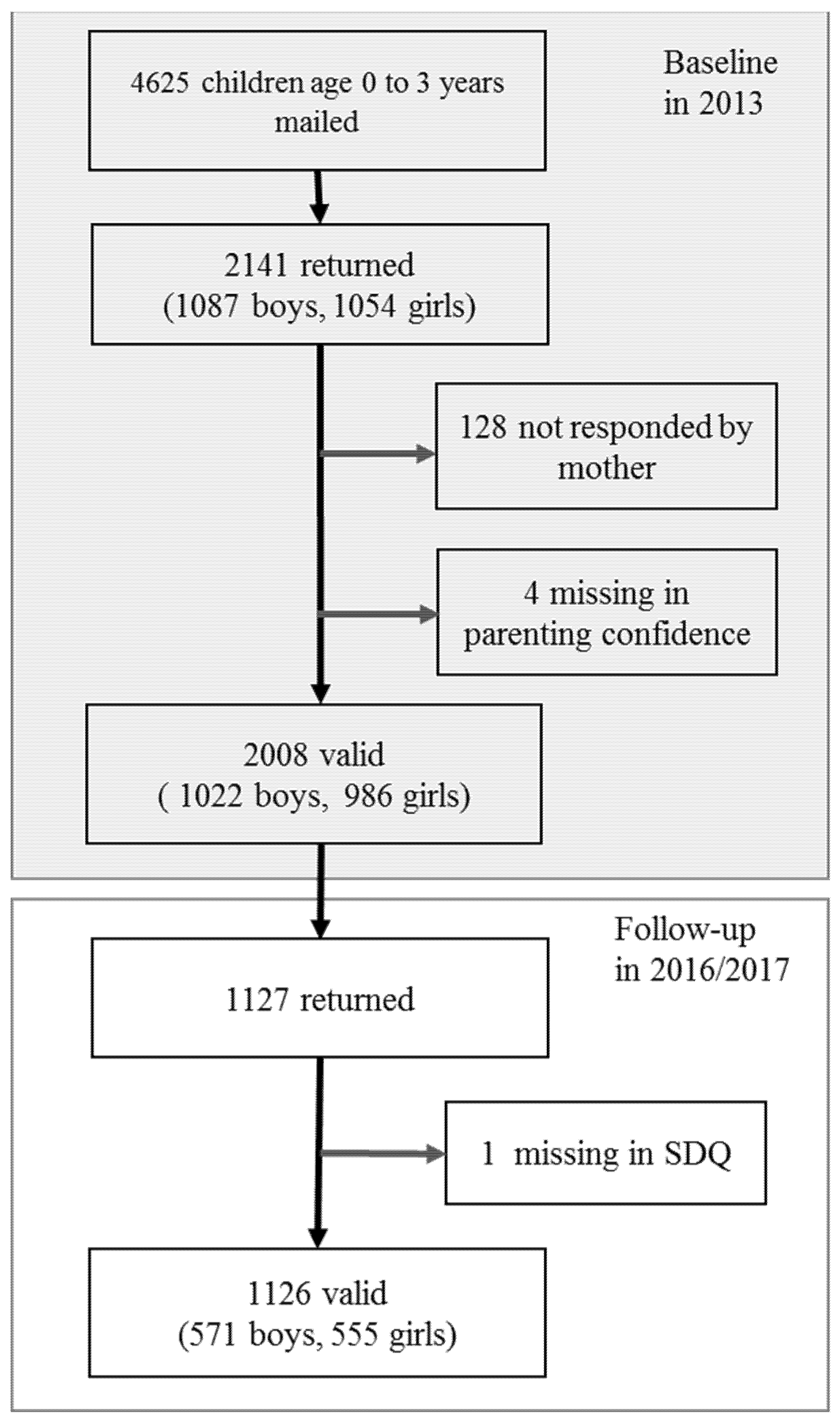
2.2. Participants
2.3. Measures
2.3.1. Baseline Assessment
2.3.2. Follow-Up Assessment
2.4. Ethics
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McDermott, B.M.; Cobham, V.E. Family Functioning in the Aftermath of a Natural Disaster. BMC Psychiatry 2012, 12, 55. [Google Scholar] [CrossRef] [PubMed]
- McFarlane, A.C. Family Functioning and Overprotection Following a Natural Disaster: The Longitudinal Effects of Post-Traumatic Morbidity. Aust. N. Z. J. Psychiatry 1987, 21, 210–218. [Google Scholar] [CrossRef]
- Roussos, A.; Goenjian, A.K.; Steinberg, A.M.; Sotiropoulou, C.; Kakaki, M.; Kabakos, C.; Karagianni, S.; Manouras, V. Posttraumatic Stress and Depressive Reactions among Children and Adolescents after the 1999 Earthquake in Ano Liosia, Greece. Am. J. Psychiatry 2005, 162, 530–537. [Google Scholar] [CrossRef]
- Cobham, V.E.; McDermott, B. Perceived Parenting Change and Child Posttraumatic Stress Following a Natural Disaster. J. Child Adolesc. Psychopharmacol. 2014, 24, 18–23. [Google Scholar] [CrossRef]
- Cohen, J.A.; Berliner, L.; Mannarino, A.P. Treating Traumatized Children: A Research Review and Synthesis. Trauma Violence Abus. 2000, 1, 29–46. [Google Scholar] [CrossRef]
- Trickey, D.; Siddaway, A.P.; Meiser-Stedman, R.; Serpell, L.; Field, A.P. A Meta-Analysis of Risk Factors for Post-Traumatic Stress Disorder in Children and Adolescents. Clin. Psychol. Rev. 2012, 32, 122–138. [Google Scholar] [CrossRef]
- Wickrama, K.A.; Kaspar, V. Family Context of Mental Health Risk in Tsunami-Exposed Adolescents: Findings from a Pilot Study in Sri Lanka. Soc. Sci. Med. 2007, 64, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Fukushima Prefecture. Survey of Intentions of Evacuees of Fukushima Prefecture [Fukushimaken Hinansha Iko Chosa]. Available online: http://www.pref.fukushima.lg.jp/site/portal/ps-hinansha-ikouchousa.html (accessed on 30 March 2021).
- Yabe, H.; Suzuki, Y.; Mashiko, H.; Nakayama, Y.; Hisata, M.; Niwa, S.-I.; Yasumura, S.; Yamashita, S.; Kamiya, K.; Abe, M. Psychological Distress after the Great East Japan Earthquake and Fukushima Daiichi Nuclear Power Plant Accident: Results of a Mental Health and Lifestyle Survey through the Fukushima Health Management Survey in FY2011 and FY2012. Fukushima J. Med. Sci. 2014, 60, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Inui, Y. The Uneasy Living Realitites on Evacuee-Families with Children—A Study on the Victims in Ibaraki Prefecture by the Great East Japan EArthquake-. J. Hum. Living Environ. 2015, 22, 93–102. [Google Scholar]
- Yamane, S. Problems of the Evacuees Resulting from the Fukushima Nuclear Accident. Fac. Lit. Soc. Sci. Yamagata Univ. Annu. Res. Rep. 2013, 10, 37–51. [Google Scholar]
- Igarashi, S.; Nishizawa, Y.; Noto, Y.; Kitajima, M.; Ogura, N.; Sasatake, H.; Hosokawa, Y. Mothers’ Anxieties Concerning Radiation, Child Raising and Quality of Life: A Study of Evacuees of the Fukushima Daiichi Nuclear Disaster. J. Radiol. Nurs. Soc. Jpn. 2017, 5, 3–11. [Google Scholar]
- Yoshioka-Maeda, K.; Kuroda, M. Literature Review on Fukushima Nuclear Plant Accident and Evacuation: Focusing on the Literature Published During 2011~2014. J. Jpn. Acad. Commun. Health Nursin 2015, 18, 69–78. [Google Scholar]
- Mizuki, R.; Kobayashi, T.; Maeda, M. Disruption of Child Environments and Its Psychological Consequences after the Fukushima Disaster: A Narrative Review Based on the Ecological Systems Model. Curr. Psychiatry Rep. 2021, 23, 49. [Google Scholar] [CrossRef] [PubMed]
- Mashiko, H.; Yabe, H.; Maeda, M.; Itagaki, S.; Kunii, Y.; Shiga, T.; Miura, I.; Suzuki, Y.; Yasumura, S.; Iwasa, H.; et al. Mental Health Status of Children after the Great East Japan Earthquake and Fukushima Daiichi Nuclear Power Plant Accident. Asia Pac. J. Public Health 2017, 29 (Suppl. 2), 131S–138S. [Google Scholar] [CrossRef]
- Badr, L.K. Further Psychometric Testing and Use of the Maternal Confidence Questionnaire. Issues Comp. Pediatr. Nurs. 2005, 28, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Badr, L.K. Quantitative and Qualitative Predictors of Development for Low-birth Weight Infants of Latino Background. Appl. Nurs. R. 2001, 14, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Loo, K.K.; Zhu, H.; Yin, Q.; Luo, H.; Min, L.; Tyler, R. Maternal Confidence in China: Association with Infant Neurobehaviors But Not Sociodemographic Variables. J. Pediatr. Psychol. 2006, 31, 452–459. [Google Scholar] [CrossRef]
- Morawska, A.; Winter, L.; Sanders, M. Parenting Knowledge and Its Role in the Prediction of Dysfunctional Parenting and Disruptive Child Behaviour. Child. Care. Health. Dev. 2009, 35, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Zahr, L.K. The Relationship between Maternal Confidence and Mother–Infant Behaviors in Premature Infants. Res. Nurs. Health. 1991, 14, 279–286. [Google Scholar] [CrossRef]
- Goto, A.; Nguyen, Q.V.; Van Nguyen, T.T.; Pham, N.M.; Chung, T.M.T.; Trinh, H.P.; Yabe, J.; Sasaki, H.; Yasumura, S. Associations of Psychosocial Factors with Maternal Confidence among Japanese and Vietnamese Mothers. J. Child Fam. Stud. 2010, 19, 118–127. [Google Scholar] [CrossRef]
- Morawska, A.; Sanders, M.R. Concurrent Predictors of Dysfunctional Parenting and Maternal Confidence: Implications for Parenting Interventions. Child Care Health Dev. 2007, 33, 757–767. [Google Scholar] [CrossRef]
- Miki, T.; Fujiwara, T.; Yagi, J.; Homma, H.; Mashiko, H.; Nagao, K.; Okuyama, M. Impact of Parenting Style on Clinically Significant Behavioral Problems among Children Aged 4–11 Years Old after Disaster: A Follow-Up Study of the Great East Japan Earthquake. Front. Psychiatry 2019, 10, 45. [Google Scholar] [CrossRef]
- Mulraney, M.; Giallo, R.; Efron, D.; Brown, S.; Nicholson, J.M.; Sciberras, E. Maternal Postnatal Mental Health and Offspring Symptoms of ADHD at 8–9 Years: Pathways via Parenting Behavior. Eur. Child Adolesc. Psychiatry 2019, 28, 923–932. [Google Scholar] [CrossRef]
- Knox, M.; Burkhart, K.; Khuder, S.A. Parental Hostility and Depression as Predictors of Young Children’s Aggression and Conduct Problems. J. Aggress. Maltreat. Trauma 2011, 20, 800–811. [Google Scholar] [CrossRef]
- Gewirtz, A.H.; DeGarmo, D.S.; Plowman, E.J.; August, G.; Realmuto, G. Parenting, Parental Mental Health, and Child Functioning in Families Residing in Supportive Housing. Am. J. Orthopsychiatry 2009, 79, 336–347. [Google Scholar] [CrossRef]
- Jones, T.L.; Prinz, R.J. Potential Roles of Parental Self-Efficacy in Parent and Child Adjustment: A Review. Clin. Psychol. Rev. 2005, 25, 341–363. [Google Scholar] [CrossRef] [PubMed]
- Cutrona, C.E.; Troutman, B.R. Social Support, Infant Temperament, and Parenting Self-Efficacy: A Mediational Model of Postpartum Depression. Child Dev. 1986, 57, 1507–1518. [Google Scholar] [CrossRef] [PubMed]
- Goto, A.; Bromet, E.J.; Ota, M.; Ohtsuru, A.; Yasumura, S.; Fujimori, K. The Fukushima Nuclear Accident Affected Mothers’ Depression but Not Maternal Confidence. Asia Pac. J. Public Health. 2017, 29 (Suppl. 2), 139S–150S. [Google Scholar] [CrossRef]
- Oyserman, D.; Bybee, D.; Mowbray, C.; Hart-Johnson, T. When Mothers Have Serious Mental Health Problems: Parenting as a Proximal Mediator. J. Adolesc. 2005, 28, 443–463. [Google Scholar] [CrossRef] [PubMed]
- Nishihara, M.; Nakamura, Y.; Fuchimukai, T.; Ohnishi, M. Factors Associated with Social Support in Child-rearing among Mothers in Post-Disaster Communities. Environ. Health Prev. Med. 2018, 23, 58. [Google Scholar] [CrossRef] [PubMed]
- Takaya, Y.; Yamamoto, A.; Kobayashi, Y.; Nakaoka, A.; Katuda, H.; Nakagomi, S.; Osaki, F.; Katada, N. The Effect of Hanshin-Awaji Earthquake on the Physical and Psychological Health Status of Maternal-Child and Their on Environment. J. Jpn. Acad. Nurs. Sci. 1998, 18, 40–50. [Google Scholar] [CrossRef]
- Goto, A.; Reich, M.R.; Suzuki, Y.; Tsutomi, H.; Watanabe, E.; Yasumura, S. Parenting in Fukushima City in the Post-disaster Period: Short-term Strategies and Long-term Perspectives. Disasters 2014, 38 (Suppl. 2), S179–S189. [Google Scholar] [CrossRef]
- Goto, A.; Rudd, R.E.; Bromet, E.J.; Suzuki, Y.; Yoshida, K.; Suzuki, Y.; Halstead, D.D.; Reich, M.R. Maternal Confidence of Fukushima Mothers Before and After the Nuclear Power Plant Disaster in Northeast Japan: Analyses of Municipal Health Records. J. Commun. Healthc. 2014, 7, 106–116. [Google Scholar] [CrossRef]
- Bromet, E.J.; Guey, L.T.; Taormina, D.P.; Carlson, G.A.; Havenaar, J.M.; Kotov, R.; Gluzman, S.F. Growing Up in the Shadow of Chornobyl: Adolescents’ Risk Perceptions and Mental Health. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 393–402. [Google Scholar] [CrossRef]
- Yasumura, S.; Hosoya, M.; Yamashita, S.; Kamiya, K.; Abe, M.; Akashi, M.; Kodama, K.; Ozasa, K. Fukushima Health Management Survey Group. Study Protocol for the Fukushima Health Management Survey. J. Epidemiol. 2012, 22, 375–383. [Google Scholar] [CrossRef]
- World Health Organization. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; WHO: Geneva, Switzerland, 2006; Available online: https://www.who.int/publications/i/item/924154693X (accessed on 26 October 2021).
- Goodman, R. The Strengths and Difficulties Questionnaire: A Research Note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Matsuishi, T.; Nagano, M.; Araki, Y.; Tanaka, Y.; Iwasaki, M.; Yamashita, Y.; Nagamitsu, S.; Iizuka, C.; Ohya, T.; Shibuya, K.; et al. Scale Properties of the Japanese Version of the Strengths and Difficulties Questionnaire (SDQ): A Study of Infant and School Children in Community Samples. Brain Dev. 2008, 30, 410–415. [Google Scholar] [CrossRef]
- Moriwaki, A.; Kamio, Y. Normative Data and Psychometric Properties of the Strengths and Difficulties Questionnaire among Japanese School-aged Children. Child Adolesc. Psychiatry Ment. Health 2014, 8, 1–12. [Google Scholar] [CrossRef]
- Doi, Y.; Ishihara, K.; Uchiyama, M. Reliability of the Strengths and Difficulties Questionnaire in Japanese Preschool Children Aged 4–6 years. J. Epidemiol. 2014, 24, 514–518. [Google Scholar] [CrossRef]
- Bridgett, D.J.; Gartstein, M.A.; Putnam, S.P.; McKay, T.; Iddins, E.; Robertson, C.; Ramsay, K.; Rittmueller, A. Maternal and Contextual Influences and the Effect of Temperament Development during Infancy on Parenting in Toddlerhood. Infant Behav. Dev. 2009, 32, 103–116. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Fine, M.A. Modeling Parenting Stress Trajectories among Low-Income Young Mothers across the Child’s Second and Third Years: Factors Accounting for Stability and Change. J. Fam. Psychol. 2007, 21, 584–594. [Google Scholar] [CrossRef]
- Crnic, K.A.; Booth, C.L. Mothers’ and Fathers’ Perceptions of Daily Hassles of Parenting across Early Childhood. J. Marriage Fam. 1991, 53, 1042–1050. [Google Scholar] [CrossRef]
- Coleman, P.K.; Karraker, K.H. Maternal Self-Efficacy Beliefs, Competence in Parenting, and Toddlers’ Behavior and Developmental Status. Infant Ment. Health J. 2003, 24, 126–148. [Google Scholar] [CrossRef]
- Izzo, C.; Weiss, L.; Shanahan, T.; Rodriguez-Brown, F. Parental Self-Efficacy and Social Support as Predictors of Parenting Practices and Children’s Socioemotional Adjustment in Mexican Immigrant Families. J. Prev. Interv. Commun. 2000, 20, 197–213. [Google Scholar] [CrossRef]
- Goto, A.; Bromet, E.J.; Fujimori, K. Pregnancy and Birth Survey Group of Fukushima Health Management Survey. Immediate Effects of the Fukushima Nuclear Power Plant Disaster on Depressive Symptoms among Mothers with Infants: A Prefectural-Wide Cross-Sectional Study from the Fukushima Health Management Survey. BMC Psychiatry. 2015, 15, 59. [Google Scholar] [CrossRef]
- Bromet, E.J. Mental Health of Residents near the Three Mile Island Reactor: A Comparative Study of Selected Groups. J. Prev. Psychiatry 1982, 1, 225–276. [Google Scholar]
- Ministry of Education, Culture, Sports, Science, and Technology. Report on the School Basic Survey; Ministry of Education, Culture, Sports, Science, and Technology: Tokyo, Japan, 2017.
- Oikawa, Y.; Momoi, M.; Maeda, M. Practicing Telephone Support for a Caregivers with a Child: The Fukushima Health Management Survey. J. Health Psychol. Res. 2020, 32, 151–158. [Google Scholar]
- Ministry of Education, Culture, Sports, Science and Technology. Results of Investigation Regarding Bullying against the Students Who Evacuated from Fukushima Prefecture Due to Fukushima Dai-Ichi Nuclear Power Plant Accident [Genshiryoku Hatsudensho Jiko Touniyori Fukushimaken kara Hinanshiteiru Jidou Seito ni Taisuru Ijimeno Joukyoutouno Kakunin ni Kakaru Foro-Appu Kekkani Tsuite]. Available online: https://www.mext.go.jp/a_menu/shotou/seitoshidou/1405633.htm (accessed on 26 October 2021).
- Maeda, M.; Harigane, M.; Horikoshi, N.; Takebayashi, Y.; Sato, H.; Takahashi, A.; Kamiya, K. Long-Term, Community-Based Approach for Affected People Having Mental Health and Lifstye Issues after 2011 Fukushima Disaster: Mental Health and Lifestyle Survey. J. Epidemiol. accepted.
- Hiromoto, Y. Vacillation and Voluntary Evacuation in the Wake of the Fukushima Nuclear Accident. Shakaigaku Hyoron JSR 2016, 67, 267–284. [Google Scholar] [CrossRef][Green Version]
- Sato, A. Structure of the Issues Surrounding the Nuclear Accident Evacuees: What Has Been Seen While Supporting Town Meetings. Shakaigaku Hyoron JSR 2013, 64, 439–459. [Google Scholar] [CrossRef][Green Version]
- Yoshioka-Maeda, K.; Togari, T. Experiences of Male Workers Whose Wife and Children Evacuated Voluntarily after Fukushima Nuclear Disaster. J. Jpn. Acad. Nurs. Sci. 2019, 39, 38–44. [Google Scholar] [CrossRef]
- Yaman, A.; Mesman, J.; van Ijzendoorn, M.H.; Bakermans-Kranenburg, M.J. Perceived Family Stress, Parenting Efficacy, and Child Externalizing Behaviors in Second-Generation Immigrant Mothers. Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Tokunaga, A.; Iwanaga, R.; Yamanishi, Y.; Higashionna, T.; Tanaka, K.; Nakane, H.; Tanaka, G. Relationship between Parenting Stress and Children’s Behavioral Characteristics in Japan. Pediatr. Int. 2019, 61, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Gilkerson, L.; Burkhardt, T.; Katch, L.E.; Hans, S.L. Increasing Parenting Self-Efficacy: The Fussy Baby Network(®) Intervention. Infant Ment. Health J. 2020, 41, 232–245. [Google Scholar] [CrossRef] [PubMed]
- Sanders, M.R.; Kirby, J.N.; Tellegen, C.L.; Day, J.J. The Triple P-Positive Parenting Program: A Systematic Review and Meta-Analysis of a Multi-Level System of Parenting Support. Clin. Psychol. Rev. 2014, 34, 337–357. [Google Scholar] [CrossRef] [PubMed]
- Scaramella, L.V.; Sohr-Preston, S.L.; Callahan, K.L.; Mirabile, S.P. A Test of the Family Stress Model on Toddler-Aged Children’s Adjustment among Hurricane Katrina Impacted and Nonimpacted Low-Income Families. J. Clin. Child Adolesc. Psychol. 2008, 37, 530–541. [Google Scholar] [CrossRef] [PubMed]
- Fukushima Medical University. Report of the Fukushima Health Management Survey 2011–2020; Fukushima Medical University: Fukushima, Japan, 2021. [Google Scholar]
- Fukasawa, M.; Kawakami, N.; Umeda, M.; Akiyama, T.; Horikoshi, N.; Yasumura, S.; Yabe, H.; Suzuki, Y.; Bromet, E.J. Distrust in government and its relationship with mental health after the Fukushima nuclear power plant accident. Int. J. Soc. Psychiatry 2020. [Google Scholar] [CrossRef]
| SDQ < 16 (n = 1019) | SDQ ≥ 16 (n = 107) | p | Cramer’s v/ Cohen’s d | ||||
|---|---|---|---|---|---|---|---|
| n/Mean | %/SD | n/Mean | %/SD | ||||
| Parenting confidence | Confident | 443 | 43.5 | 28 | 26.2 | <0.001 | 0.128 |
| Not sure | 428 | 42.0 | 49 | 45.8 | |||
| Not confident | 148 | 14.5 | 30 | 28.0 | |||
| Age, years | Mean | 2.0 | 0.86 | 1.9 | 0.82 | 0.167 | 0.141 |
| 0 | 24 | 2.4 | 3 | 2.8 | 0.239 | 0.061 | |
| 1 | 306 | 30.0 | 34 | 31.8 | |||
| 2 | 336 | 33.0 | 43 | 40.2 | |||
| 3 | 353 | 34.6 | 27 | 25.2 | |||
| Sex | Girl | 525 | 51.5 | 46 | 43.0 | 0.093 | 0.050 |
| Boy | 494 | 48.5 | 61 | 57.0 | |||
| Stunting | No | 988 | 97.0 | 99 | 92.5 | 0.026 † | 0.011 |
| Yes | 31 | 3.0 | 8 | 7.5 | |||
| Current health conditions | Very good or good | 697 | 69.1 | 58 | 54.2 | 0.007 † | 0.094 |
| Fair | 295 | 29.2 | 46 | 43.0 | |||
| Poor or very poor | 17 | 1.7 | 3 | 2.8 | |||
| Sleep duration, hours | Mean | 10.0 | 0.83 | 9.8 | 0.88 | 0.025 | 0.229 |
| Hospitalization history | No | 776 | 76.3 | 72 | 67.3 | 0.039 | 0.061 |
| Yes | 241 | 23.7 | 35 | 32.7 | |||
| Evacuation location | Inside of Fukushima | 659 | 64.7 | 65 | 60.7 | 0.420 | 0.024 |
| Out of Fukushima | 360 | 35.3 | 42 | 39.3 | |||
| Reluctance to attend school | No | 880 | 86.8 | 73 | 68.2 | <0.001 | 0.153 |
| Yes | 134 | 13.2 | 34 | 31.8 | |||
| SDQ Total Difficulties (n = 1110) | Reluctance to Attend School (n = 1105) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age and Sex-Adjusted | Multiple * | Age and Sex-Adjusted | Multiple * | ||||||||||
| OR | CI Lower | CI Upper | OR | CI Lower | CI Upper | OR | CI Lower | CI Upper | OR | CI Lower | CI Upper | ||
| Confidence in parenting | |||||||||||||
| Yes | ref. | ref. | ref. | ||||||||||
| Not sure | 1.81 | 1.11 | 2.93 | 1.65 | 1.01 | 2.70 | 1.50 | 1.02 | 2.19 | 1.45 | 0.99 | 2.14 | |
| No | 3.24 | 1.87 | 5.62 | 2.75 | 1.56 | 4.84 | 2.24 | 1.42 | 3.54 | 1.99 | 1.24 | 3.20 | |
| Age | 0.83 | 0.657 | 1.048 | 0.78 | 0.61 | 0.99 | 0.68 | 0.56 | 0.83 | 0.66 | 0.54 | 0.80 | |
| Sex | 1.383 | 0.921 | 2.077 | 1.33 | 0.88 | 2.02 | 1.12 | 0.80 | 1.56 | 1.14 | 0.81 | 1.61 | |
| Stunting | 1.34 | 0.50 | 3.61 | 1.70 | 0.78 | 3.69 | |||||||
| Current health condition | 1.51 | 1.04 | 2.19 | 1.47 | 1.07 | 2.02 | |||||||
| Sleep duration | 0.75 | 0.59 | 0.97 | 1.07 | 0.87 | 1.31 | |||||||
| Hospitalization history | 1.32 | 0.84 | 2.08 | 1.16 | 0.79 | 1.71 | |||||||
| Evacuation out of Fukushima | 1.21 | 0.78 | 1.87 | 1.36 | 0.95 | 1.93 | |||||||
| Emotional Symptoms | Conduct Problems | Hyperactivity/Inattention | Peer Relationship Problems | Prosocial Behavior | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | CI Lower | CI Upper | OR | CI Lower | CI Upper | OR | CI Lower | CI Upper | OR | CI Lower | CI Upper | OR | CI Lower | CI Upper | |
| Parenting confidence | |||||||||||||||
| Confident | ref. | ref. | ref. | ref. | ref. | ||||||||||
| Not sure | 2.58 | 1.52 | 4.39 | 1.38 | 0.74 | 2.56 | 0.97 | 0.61 | 1.55 | 2.23 | 1.11 | 4.48 | 0.94 | 0.65 | 1.36 |
| Not confident | 2.53 | 1.33 | 4.82 | 4.50 | 2.39 | 8.48 | 1.91 | 1.11 | 3.28 | 3.26 | 1.48 | 7.17 | 1.45 | 0.91 | 2.30 |
| Age | 1.03 | 0.80 | 1.33 | 0.66 | 0.50 | 0.88 | 0.74 | 0.59 | 0.94 | 0.85 | 0.62 | 1.16 | 0.75 | 0.62 | 0.91 |
| Sex | 0.91 | 0.59 | 1.40 | 1.09 | 0.66 | 1.78 | 1.49 | 0.99 | 2.26 | 1.46 | 0.83 | 2.56 | 2.24 | 1.58 | 3.16 |
| Stunting | 1.45 | 0.54 | 3.87 | 0.76 | 0.17 | 3.30 | 1.69 | 0.68 | 4.21 | 1.66 | 0.48 | 5.75 | 1.38 | 0.59 | 3.22 |
| Current health condition | 1.29 | 0.87 | 1.93 | 1.03 | 0.65 | 1.64 | 0.94 | 0.63 | 1.41 | 1.47 | 0.90 | 2.39 | 1.24 | 0.91 | 1.71 |
| Sleep duration, hours | 1.01 | 0.78 | 1.32 | 1.03 | 0.77 | 1.38 | 0.82 | 0.64 | 1.05 | 0.91 | 0.66 | 1.27 | 0.92 | 0.75 | 1.13 |
| Hospitalization history | 0.92 | 0.55 | 1.53 | 1.30 | 0.75 | 2.25 | 1.35 | 0.86 | 2.12 | 1.25 | 0.69 | 2.29 | 0.90 | 0.61 | 1.33 |
| Evacuation location | 1.66 | 1.07 | 2.58 | 0.92 | 0.55 | 1.56 | 0.80 | 0.51 | 1.25 | 1.24 | 0.70 | 2.20 | 0.88 | 0.62 | 1.26 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mizuki, R.; Maeda, M.; Kobayashi, T.; Horikoshi, N.; Harigane, M.; Itagaki, S.; Nakano, H.; Ohira, T.; Yabe, H.; Yasumura, S.; et al. The Association between Parenting Confidence and Later Child Mental Health in the Area Affected by the Fukushima Nuclear Disaster: The Fukushima Health Management Survey. Int. J. Environ. Res. Public Health 2022, 19, 476. https://doi.org/10.3390/ijerph19010476
Mizuki R, Maeda M, Kobayashi T, Horikoshi N, Harigane M, Itagaki S, Nakano H, Ohira T, Yabe H, Yasumura S, et al. The Association between Parenting Confidence and Later Child Mental Health in the Area Affected by the Fukushima Nuclear Disaster: The Fukushima Health Management Survey. International Journal of Environmental Research and Public Health. 2022; 19(1):476. https://doi.org/10.3390/ijerph19010476
Chicago/Turabian StyleMizuki, Rie, Masaharu Maeda, Tomoyuki Kobayashi, Naoko Horikoshi, Mayumi Harigane, Shuntaro Itagaki, Hironori Nakano, Tetsuya Ohira, Hirooki Yabe, Seiji Yasumura, and et al. 2022. "The Association between Parenting Confidence and Later Child Mental Health in the Area Affected by the Fukushima Nuclear Disaster: The Fukushima Health Management Survey" International Journal of Environmental Research and Public Health 19, no. 1: 476. https://doi.org/10.3390/ijerph19010476
APA StyleMizuki, R., Maeda, M., Kobayashi, T., Horikoshi, N., Harigane, M., Itagaki, S., Nakano, H., Ohira, T., Yabe, H., Yasumura, S., & Kamiya, K. (2022). The Association between Parenting Confidence and Later Child Mental Health in the Area Affected by the Fukushima Nuclear Disaster: The Fukushima Health Management Survey. International Journal of Environmental Research and Public Health, 19(1), 476. https://doi.org/10.3390/ijerph19010476






