Religiously Conditioned Health Behaviors within Selected Religious Traditions
Abstract
1. Introduction
2. Materials and Methods
2.1. The Aim of the Study
2.2. Study Organization and Course
2.3. The Study Group
2.4. Methods, Techniques and Research Tools
- verify whether the declared level of religious commitment among Catholics is a factor differentiating their health behaviors.
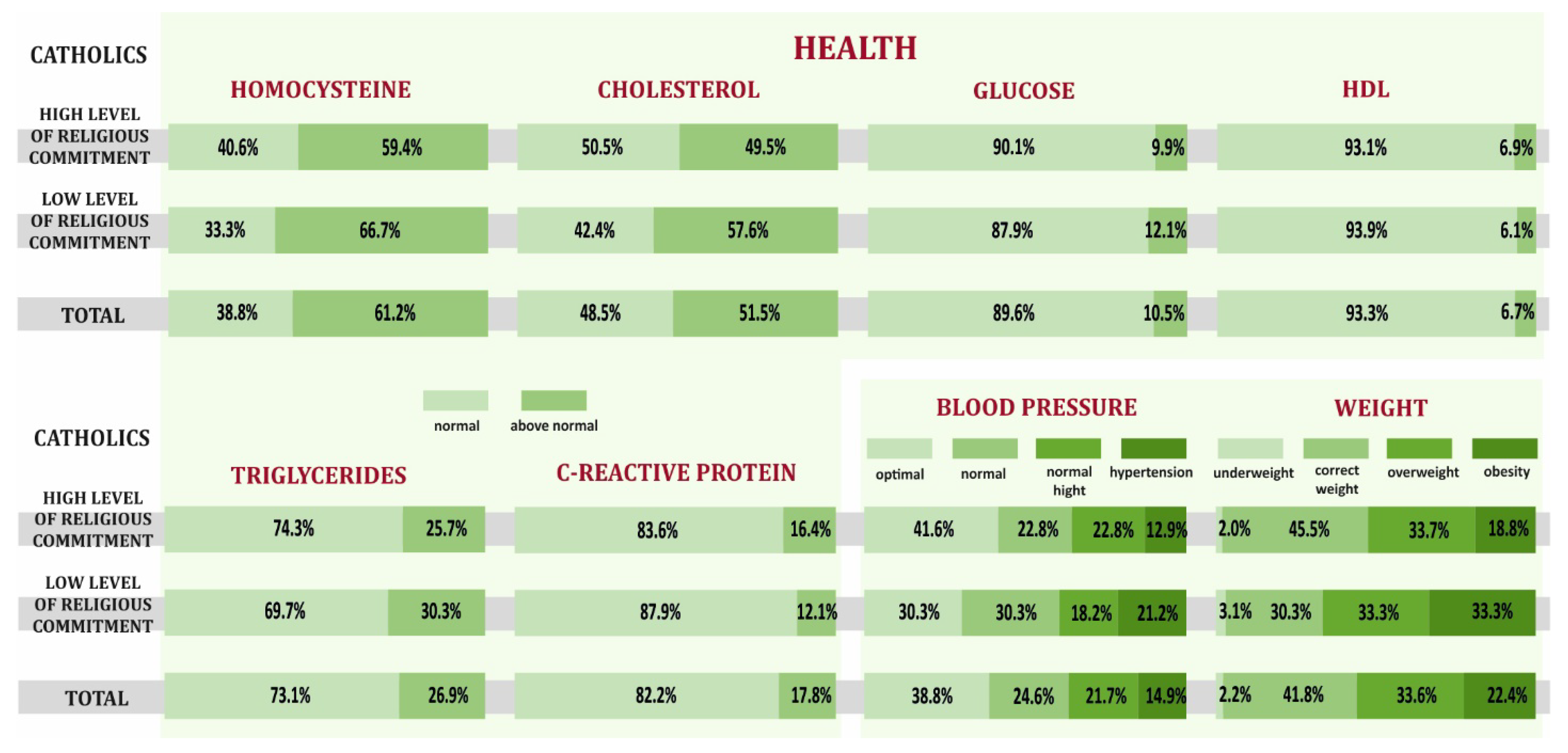
- verify whether the overall health (determined by selected parameters) of Catholics differs depending on the level of religious commitment declared by them.
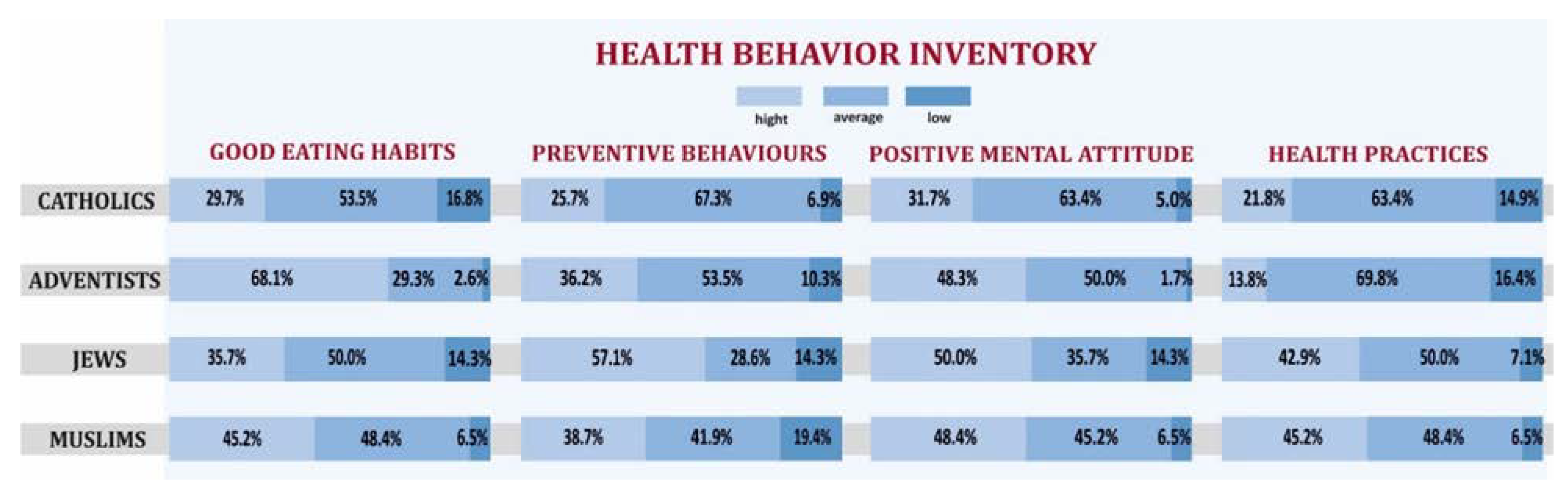
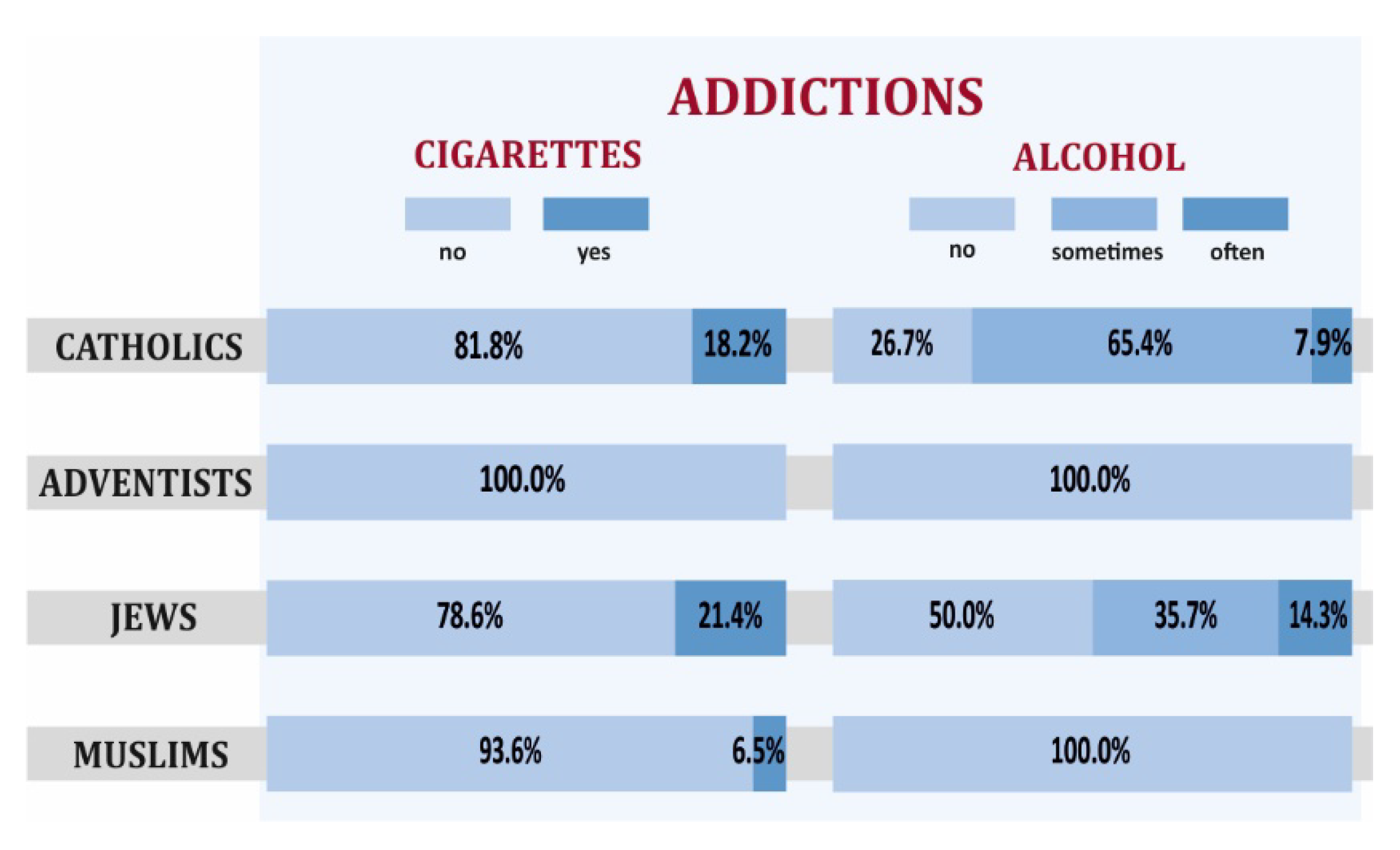
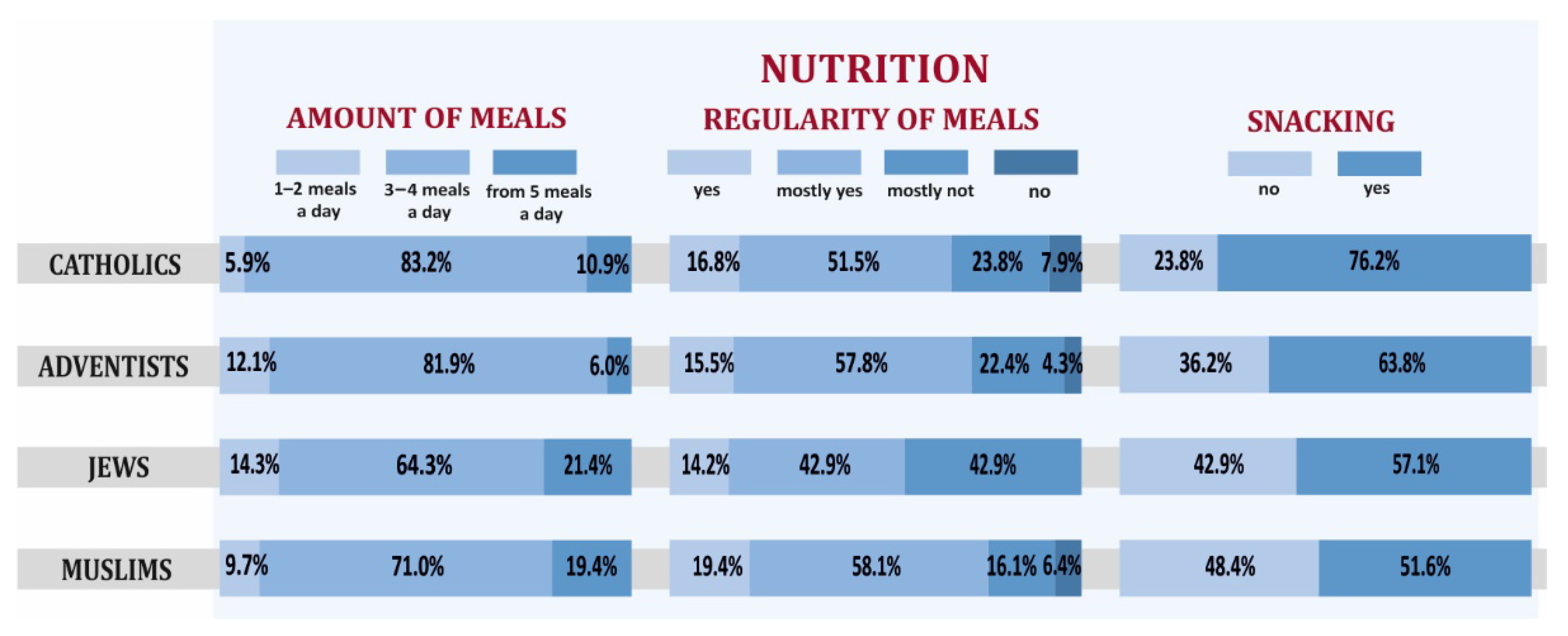
- determine whether there is a differentiation among the religious groups in terms of health behaviors.
- determine whether the indicated differences in health behaviors of people of particular faiths are reflected in their overall health (determined by selected parameters).
2.5. Ethical Considerations
3. Results
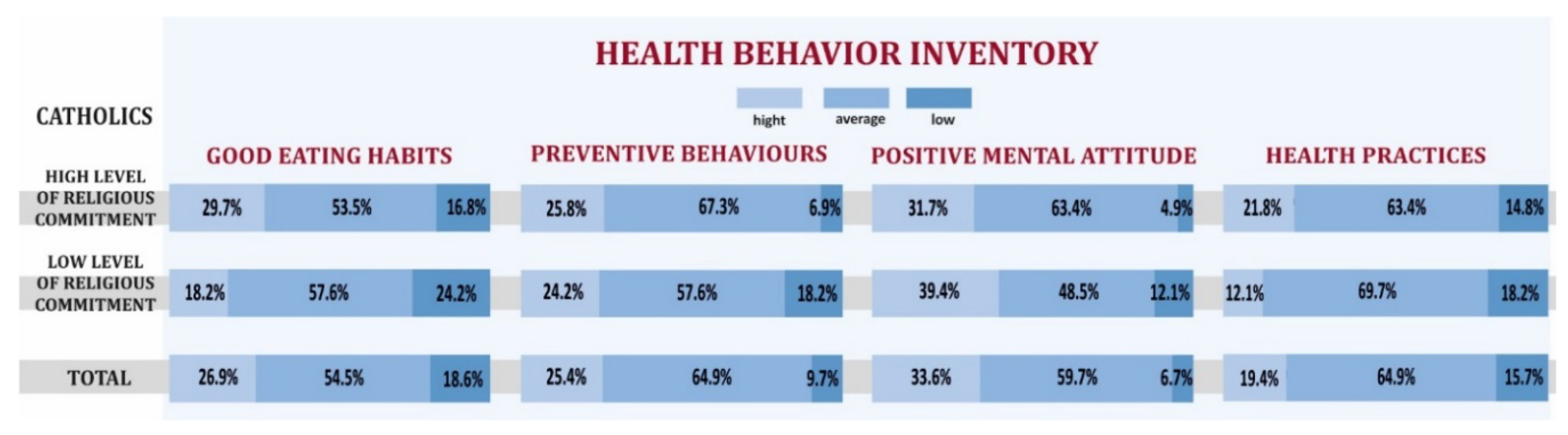
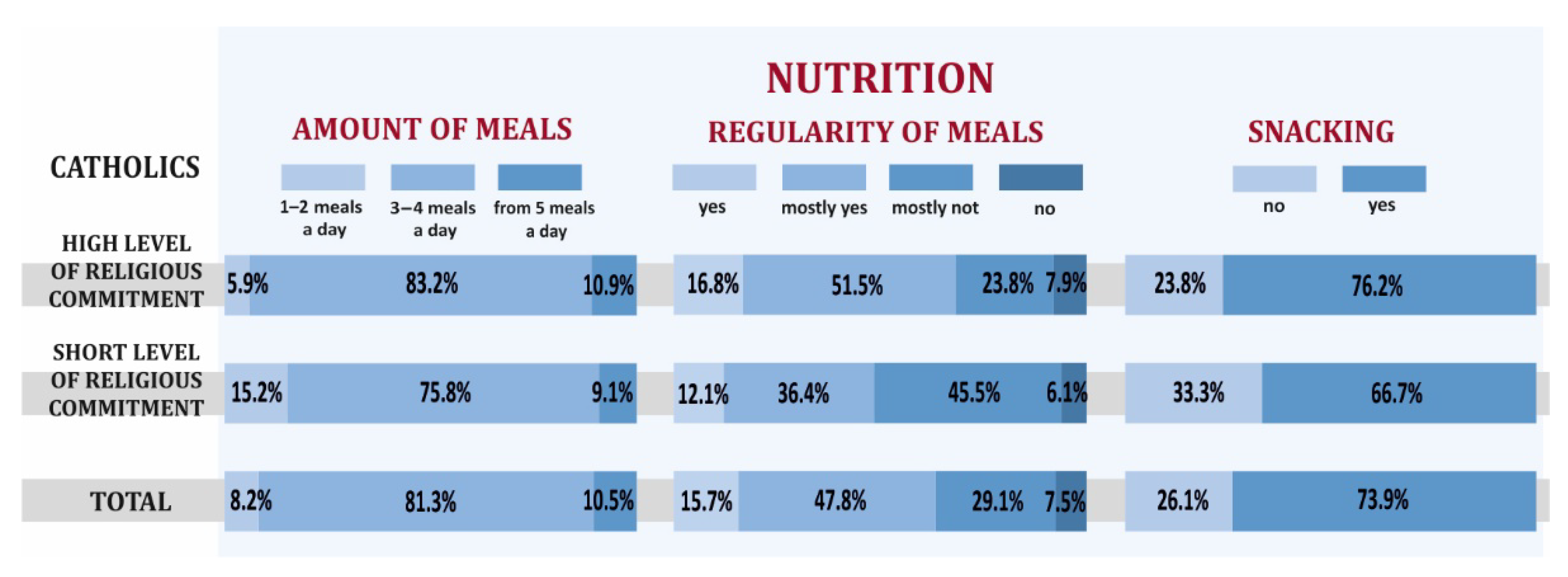
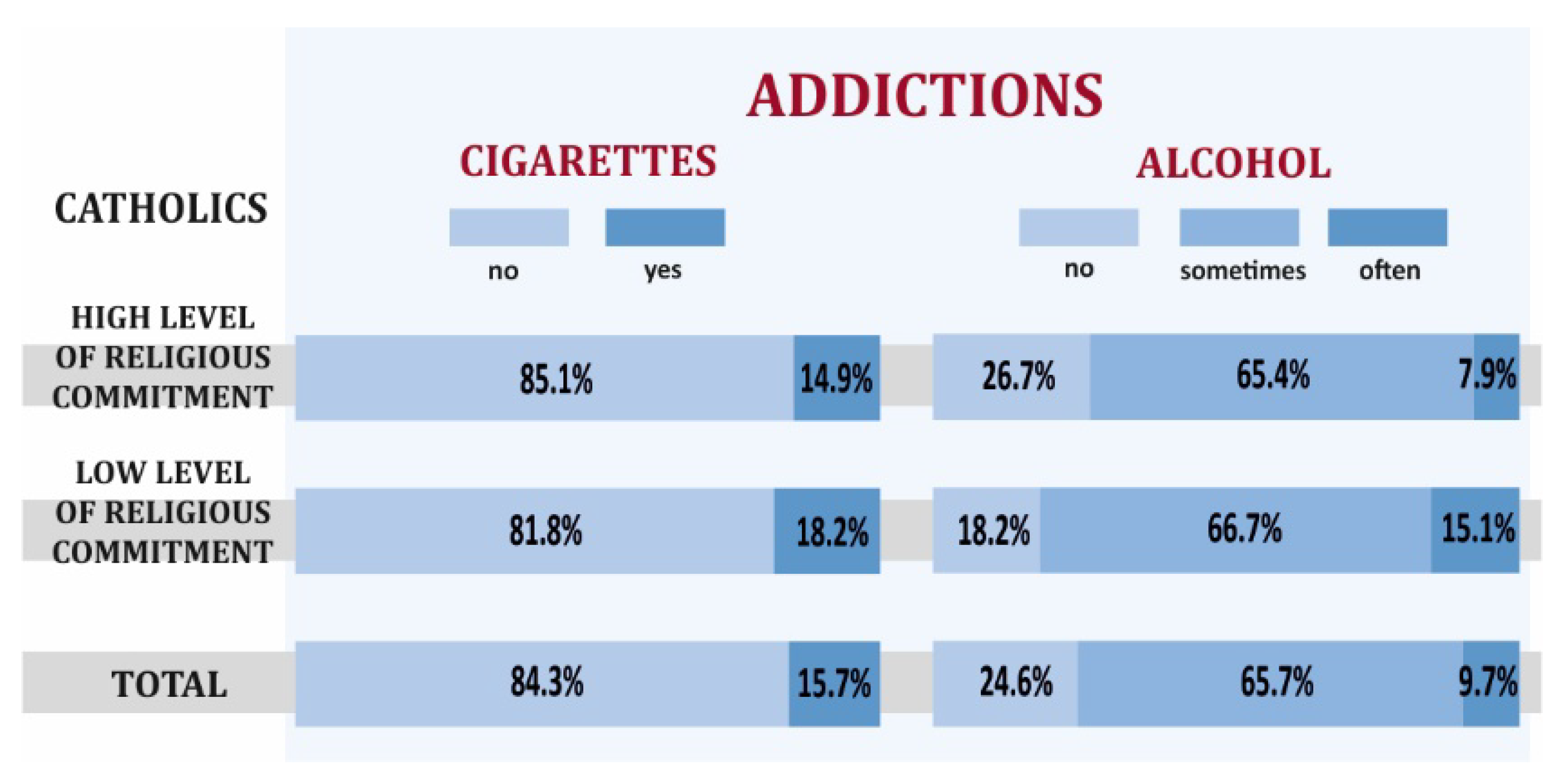
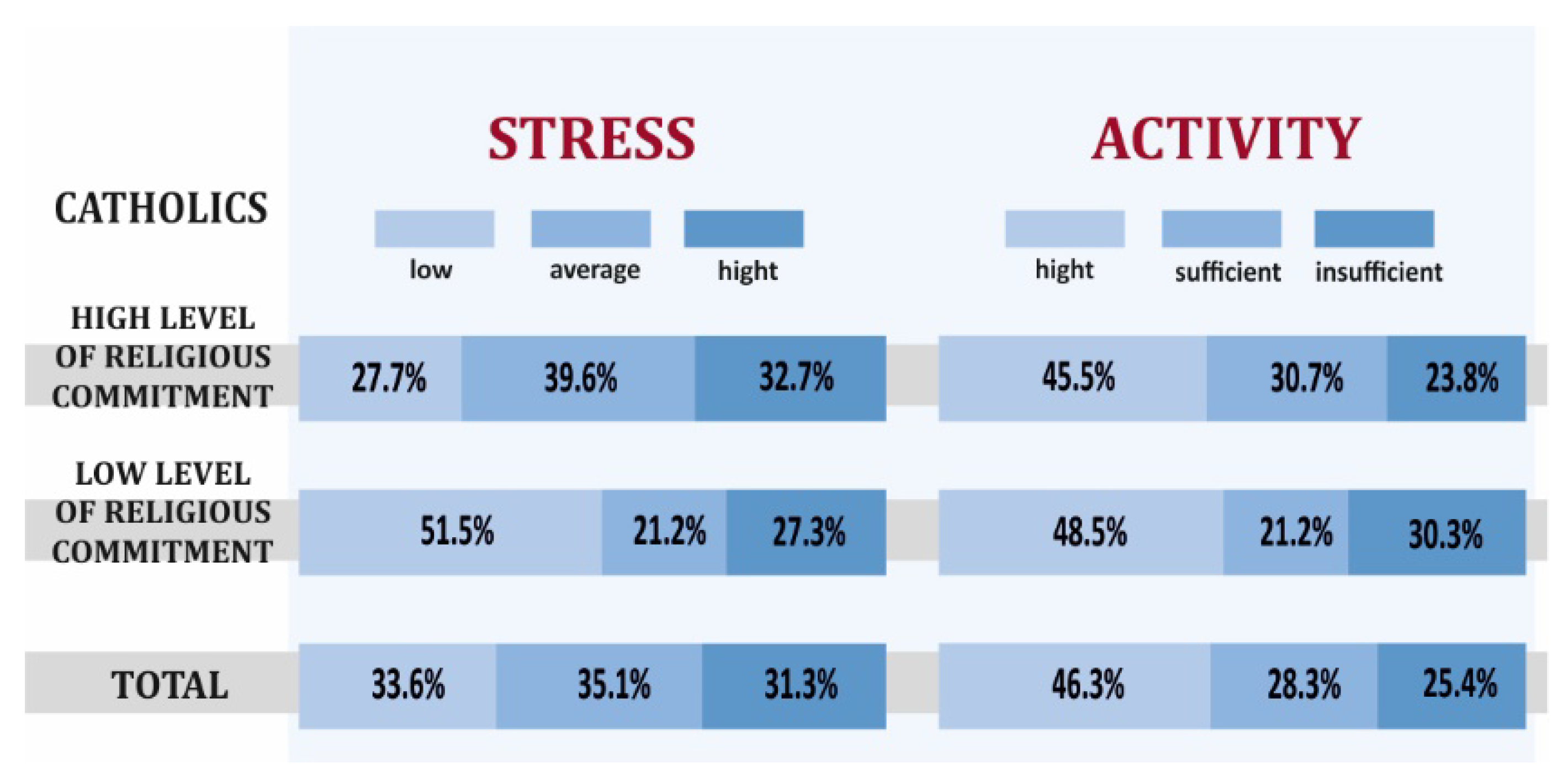
3.1. Health Behaviors and Overall Health of Catholics with High and Low Levels of Religious Commitment
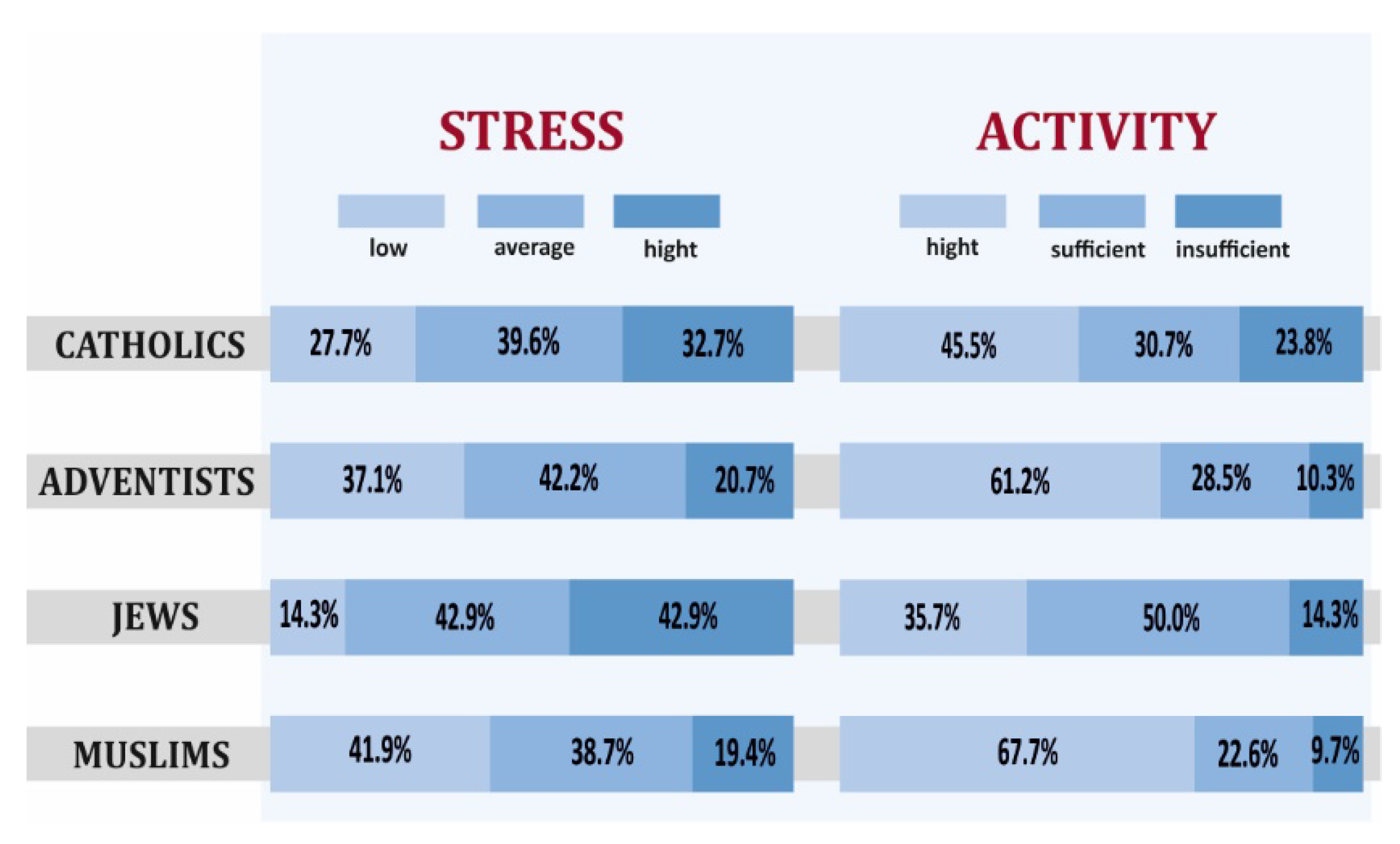
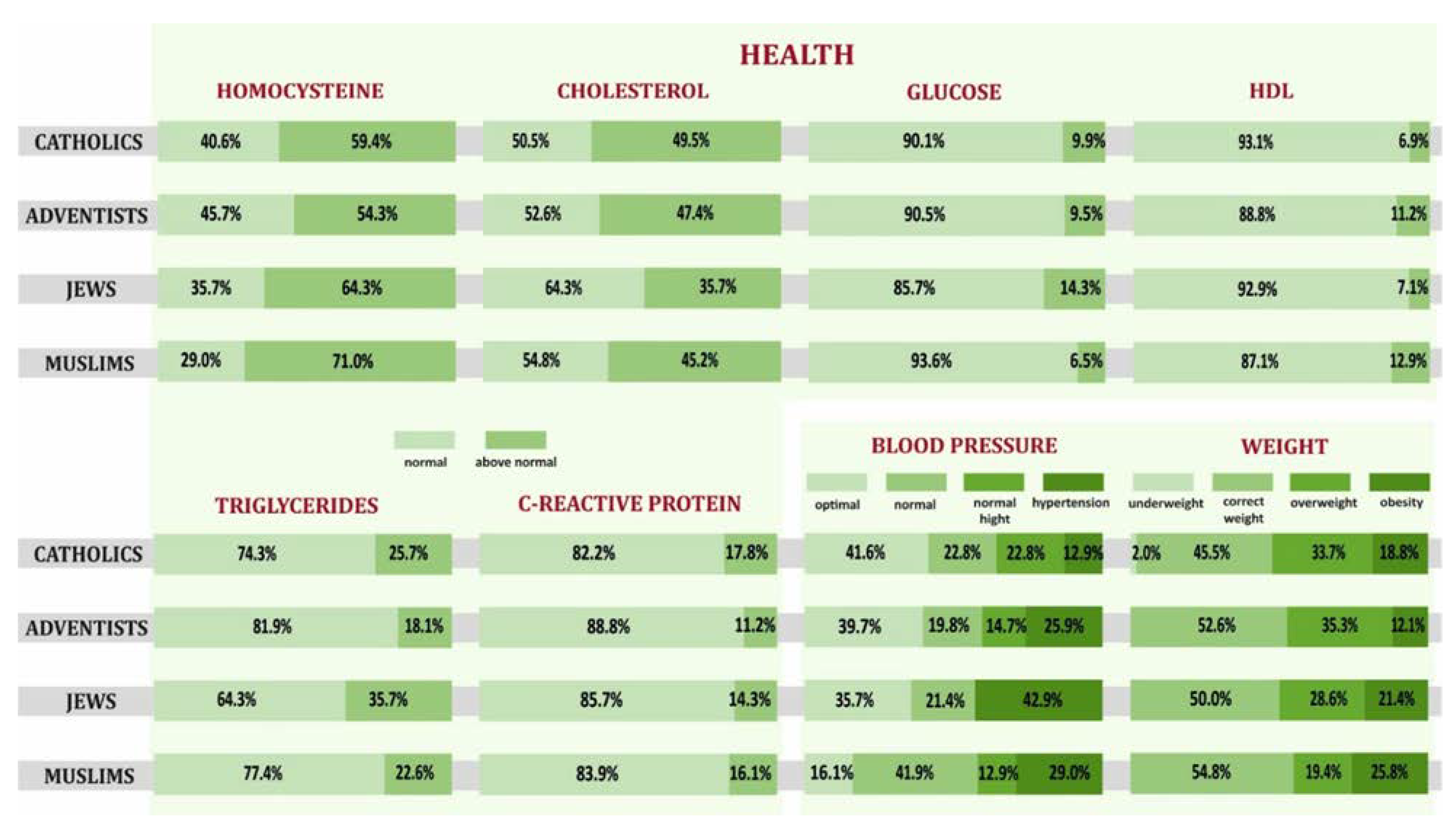
3.2. Health Behaviors and Overall Health of Representatives of Selected Religious Groups with a High Level of Religious Commitment
4. Discussion
5. Conclusions
- Only 75% of surveyed Catholics declared high religious commitment only, meanwhile for the surveyed SDA, Muslims, and Jews it was 100%.
- Catholics with a high level of religious commitment declared more positive health behaviors and presented better overall health compared to Catholics with a low level of religiousness, but also higher levels of stress, worse mental attitude, and less physical activity.
- Selected elements of lifestyle, overall health through the prism of the results of biochemical and anthropometric tests, blood pressure of Jews and Muslims differed from the recommendations of a healthy lifestyle. Still, they differed the most for Catholics and the least for SDAs.
- The results suggest that public health professionals and nurses should develop culturally specific educational interventions for the prevention cardiovascular disease, especially among Catholics, concerning a healthy lifestyle, including a change in diet, physical activity, stress reduction, and elimination of addictions.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Godlewska, D.; Gebreselassie, J. Religia a zdrowie i choroba. Język. Religia Tożsamość 2018, 1, 223–236. [Google Scholar]
- Tworuschka, M.; Tworuschka, U. Religie Świata; Wydawnictwo Bellona: Warsaw, Poland, 2010. [Google Scholar]
- Libiszowska-Żółtkowska, M. Religia w trosce o zdrowie. Wybrane zagadnienia z pogranicza socjologii medycyny i socjologii religii. In Szkice z Socjologii Medycyny; Libuszowska-Żółtkowska, M., Ogryzko-Wiewiórowska, M., Piątkowski, W., Eds.; Wydawnictwo UMCS: Lublin, Poland, 1998; pp. 39–61. [Google Scholar]
- Pawlikowski, J.; Marczewski, K. Religia a zdrowie–czy religia może sprzyjać trosce o zdrowie? Część 1—Wartość zdrowia w wielkich religiach świata. Kardiologia po Dyplomie 2008, 7, 96–98. [Google Scholar]
- Pawlikowski, J.; Sak, J.; Marczewski, K. Religia a zdrowie–czy religia może sprzyjać trosce o zdrowie? Część 2—Religijność a zdrowie. Kardiologia po Dyplomie 2009, 8, 87–94. [Google Scholar]
- Magdoń, M.; Skrzypek, M.; Klocek, M. Religijność a zdrowie. Sztuka Leczenia 1996, 3, 61–68. [Google Scholar]
- Marcus, Z.J.; McCullough, M.E. Does religion make people more self-controlled? A review of research from the lab and life. Curr. Opin. Psychol. 2021, 40, 167–170. [Google Scholar] [CrossRef] [PubMed]
- McCullough, M.E.; Willoughby, B.L.B. Religion, self-regulation, and self-control: Associations, explanations, and implications. Psychol. Bull. 2009, 135, 69–93. [Google Scholar] [CrossRef] [PubMed]
- Seybold, K.S.; Hill, P.C. The Role of Religion and Spirituality in Mental and Physical Health. Curr. Dir. Psychol. Sci. 2001, 10, 21–24. [Google Scholar] [CrossRef]
- Mueller, P.S.; Plevak, D.J.; Rummans, T.A. Religious Involvement, Spirituality, and Medicine: Implications for Clinical Practice. Mayo Clin. Proc. 2001, 76, 1225–1235. [Google Scholar] [CrossRef]
- Miller, D.; Chen, E.; Cole, S.W. Health Psychology: Developing Biologically Plausible Models Linking the Social World and Physical Health. Annu. Rev. Psychol. 2009, 60, 501–524. [Google Scholar] [CrossRef]
- Jędrychowski, W.; Tobiasz-Adamczyk, B.; Olma, A.; Gradziliewicz, P. Survival Rates Among Seventh-day Adventists Compared with the general population of Poland. Scand. J. Soc. Med. 1985, 13, 49–52. [Google Scholar] [CrossRef]
- Polak, J.; Grabowski, D. Wstępna charakterystyka psychometryczna polskiej wersji kwestionariusza Religious Commitment Inventory-10 (RCI-10-PL) Everetta Worthingtona i współpracowników. Rocz. Psychol. Ann. Psychol. 2017, 20, 91–212. [Google Scholar] [CrossRef][Green Version]
- Żołnierz, J.; Sak, J. Współczesne badania nad wpływem religijności na zdrowie człowieka. J. Educ. Health Sport. 2017, 7, 100–112. [Google Scholar]
- Shor, E.; Roelfs, D.J. The longevity effects of religious and nonreligious participation: A meta-analysis and meta-regression. J. Sci. Study Relig. 2013, 52, 120–145. [Google Scholar] [CrossRef]
- Phillips, R.L.; Kuzma, J.W.; Beeson, W.L.; Lotz, T. Influence of selection versus lifestyle on risk of fatal cancer and cardiovascular diseasae among Seventh-day Adventists. Am. J. Epidemiol. 1980, 112, 296–314. [Google Scholar] [CrossRef] [PubMed]
- Appel, L.J.; Miller, E.R.; Ha Jee, S.; Stolzenberg-Solomon, R.; Lin, P.H.; Erlinger, T.; Nadeau, M.R.; Selhub, J. Effect of dietary patterns on serum homocysteine. Results of a randomized, controlled feeding study. Circulation 2000, 102, 852–857. [Google Scholar] [CrossRef] [PubMed]
- Heuch, I.; Jacobsen, B.K.; Kraser, G.E. A cohort study found that earlier and longer Seventh-day Adventist church membership was associated with reduced male mortality. J. Clin. Epidemiol. 2005, 58, 83–91. [Google Scholar] [CrossRef]
- Orlich, M.J.; Singh, P.N.; Sabate, J.; Jaceldo-Siegl, K.; Fan, J.; Knutsen, S.; Beeson, W.L.; Fraser, G.E. Vegetarian Dietary Patterns and Mortality in Adventist Health Study 2. JAMA Intern. Med. 2013, 173, 1230–1238. [Google Scholar] [CrossRef] [PubMed]
- Kwokm, C.S.; Umar, S.; Myint, P.K.; Mamas, M.A.; Loke, Y.K. Vegetarian diet, Seventh Day Adventists and risk of cardiovascular mortality: A systematic review and meta-analysis. Int. J. Cardiol. 2014, 176, 680–686. [Google Scholar] [CrossRef] [PubMed]
- Williams, I.M.G. Mindfulness and Psychological Process. Am. Psychol. Assoc. 2010, 10, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Vaillant, G.E. Positive Emotions, Spirituality and the Practice of psychiatry. J. Ment. Health Spiritual. Mind. 2008, 6, 48–62. [Google Scholar] [CrossRef] [PubMed]
- Rippentrop, A.E. A Review of the Role and Religion and Spirituality in Chronic Pain Populations. Rehabil. Psychol. 2005, 50, 278–284. [Google Scholar] [CrossRef]
- Gorsuch, R.L.; Butler, M.C. Initial drug abuse: A review of predisposing social psychological factors. Psychol. Bull. 1976, 83, 120–137. [Google Scholar] [CrossRef]
- Gartner, J.; Larson, D.B.; Allen, G.D. Religious commitment and mental health: A review of the empirical literature. J. Psychol. Theol. 1991, 19, 6–25. [Google Scholar] [CrossRef]
- Idler, E.L.; Kasl, S.V. Religion among disabled and nondisabled persons, II: Attendance at religious services as a predictor of the course of disability. J. Gerontol. Ser. B 1997, 52, 306–316. [Google Scholar] [CrossRef] [PubMed]
- Matthews, D.A.; McCullough, M.E.; Larson, D.B. Religious commitment and health status: A review of the research and implications for family medicine. Arch. Fam. Med. 1988, 7, 118–124. [Google Scholar] [CrossRef]
- Bell, C.N.; Bowie, J.V.; Thorpe, R.J. The interrelationship between hypertension and blood pressure, attendance at religious services, and race/ethnicity. J. Relig. Health 2012, 51, 310–322. [Google Scholar] [CrossRef]
- Feinstein, M.; Liu, K.; Ning, H.; Fitchett, G.; Lloyd-Jones, D.M. Burden of cardiovascular risk factors, subclinical atherosclerosis, and incident cardiovascular events across dimensions of religiosity: The multi-ethnic study of atherosclerosis. Circulation 2010, 121, 659–666. [Google Scholar] [CrossRef]
- Katechizm Kościoła Katolickiego; Kongregacja Nauki Wiary, Pallotinum: Poznań, Poland, 1994.
- Papieska Rada ds. Duszpasterstwa Służby Zdrowia. Karta Pracowników Służby Zdrowia. In W trosce o życie. Wybrane Dokumenty Stolicy Apostolskiej; Szczygieł, K., Ed.; Biblos: Tarnów, Poland, 1998; pp. 549–627. [Google Scholar]
- Tobiasz-Adamczyk, B. Wybrane Elementy Socjologii Zdrowia i Choroby; Wydawnictwo UJ: Kraków, Poland, 2000. [Google Scholar]
- Majda, A.; Zalewska-Puchała, J.; Ogórek-Tęcza, B. Pielęgniarstwo Transkulturowe. Podręcznik dla Studiów Medycznych; Wydawnictwo Lekarskie PZWL: Warszawa, Poland, 2010. [Google Scholar]
- Klöcker, M.; Tworuschka, M.; Tworuschka, U. Etyka Wielkich Religii. Mały Słownik; Verbinum: Warszawa, Poland, 2002. [Google Scholar]
- Co Adwentyści Sądzą o Chrześcijaństwie. Available online: https://www.adventist.org/beliefs/fundamental-beliefs/living/christian-behavior/ (accessed on 8 March 2021).
- Bratosin, M. Mediatization of Beliefs: The Adventism from “Morning Star” to the Public Sphere. Religions 2020, 11, 483. Available online: https://www.mdpi.com/2077-1444/11/10/483/htm (accessed on 27 December 2021). [CrossRef]
- Tudor, M.A.; Benea, A.F.; Bratosin, S. COVID-19 Pandemic Lockdown and Religious Mediatization of Social Sustainability. A Case Study of Romania. Int. J. Environ. Res. Public Health 2021, 18, 2287. Available online: https://www.mdpi.com/1660-4601/18/5/2287/htm (accessed on 27 December 2021). [CrossRef]
- Modrzejewski, W.; Musiał, W.J. Stare i nowe czynniki ryzyka sercowo-naczyniowego–jak zahamować epidemię miażdżycy?. Część, I. Klasyczne czynniki ryzyka. Forum Zaburzeń Metabolicznych 2010, 2, 106–114. [Google Scholar]
- Gąsiorowska, D.; Korzeniowska, K.; Jabłecka, A. Homocysteina. Farmacja Współczesna 2008, 1, 169–175. [Google Scholar]
- Sjöström, M.; Ainsworth, B.; Bauman, A.; Bull, F.; Craig, C.; Sallis, J. International Physical Activity Questionnaire (IPAQ). Available online: http://www.ipaq.ki.se/ipaq.htm (accessed on 7 April 2020).
- Juczyński, Z. Measurement Tools in the Promotion and Health Psychology; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2001. [Google Scholar]
- Juczyński, Z.; Ogińska-Bulik, N. Tools for Measuring Stress and Coping with Stress; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2012. [Google Scholar]
- Majda, A.; Zalewska-Puchała, J.; Bodys-Cupak, I.; Kamińska, A.; Kurowska, A.; Suder, M. Comparison of Lifestyle of Catholics and Seventh-Day Adventists and the Relationship with Homocysteine as Risk Factor for Cardiovascular Diseases, a Cross-Sectional Study in Polish Males and Females. Int. J. Environ. Res. Public Health 2021, 18, 309. [Google Scholar] [CrossRef]
- Jóźwiak, J.; Podgórski, J. Statystyka od Podstaw, 7th ed.; PWE: Warszawa, Poland, 2012. [Google Scholar]
- Zagożdżon, P. Związek między religią a zdrowiem w badaniach epidemiologicznych. Polski Merkuriusz Lekarski 2012, XXXII, 349–353. [Google Scholar]
- Levav, I.; Kohn, R.; Golding, J.M.; Weissman, M.M. Vulnerability of Jews to affective disorders. Am. J. Psychiatry 1997, 154, 941–947. [Google Scholar] [PubMed]
- Berkel, J.; De Waard, F. Mortality Pattern and Life Expectancy of Seventh-day Adventist in the Netherlands. Int. J. Epidemiol. 1983, 12, 455–459. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, S.; Weinblatt, C.W.; Sager, R.V. Incidence of coronary heart disease in a population insured for medical care (HIP); myocardial infarction, angina pectoris, and possible myocardial infarction. Am. J. Public Health Nations Health 1969, 59 (Suppl. 6), 1–101. [Google Scholar] [CrossRef]
- Jacobsen, B.K.; Knutsen, S.F.; Oda, K.; Fraser, G.E. Parity and total, ischemic heart disease and stroke mortality. The Adventist Health Study, 1976–1988. Eur. J. Epidemiol. 2011, 26, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Nematy, M.; Alinezhad-Namaghi, M.; Rashed, M.M.; Mozhdehifard, M.; Sajjadi, S.S.; Akhlaghi, S.; Saberym, M.; Mohajeri, S.A.; Shalaey, N.; Moohebati, M.; et al. Effects of Ramadan fasting on cardiovascular risk factors: A prospective observational study. Nutr. J. 2012, 11, 69–70. [Google Scholar] [CrossRef]
- Yousefi, B.; Faghfoori, Z.; Samadi, N.; Karami, H.; Ahmadi, Y.; Badalzadeh, R.; Shafiei-Irannejad, V.; Majidinia, M.; Ghavini, M.; Jabbarpour, M. The effects of Ramadan fasting on endothelial function in patients with cardiovascular diseases. Eur. J. Clin. Nutr. 2014, 68, 83335–83339. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, M.M.; Modeste, N.N.; Marshak, H.H.; Wilson, C. Religious involvement and health-related behaviors among Black Seventh-day Adventists in Canada. Health Promot. Pract. 2015, 6, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Chamsi-Pasha, M.; Chamsi-Pasha, H. The cardiac patient in Ramadan. Avicenna J. Med. 2016, 6, 33–38. [Google Scholar] [PubMed]
- Plakht, Y.; Gilutz, H.; Shiyovich, A. Ethnical disparities in temporal trends of acute myocardial infarction (AMI) throughout a decade in Israel. Soroka acute myocardial infarction (SAMI-II) project. Intern. J. Cardiol. 2016, 214, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Janiszewska, J.; Lichodziejewska-Niemierko, M. Znaczenie religijności w życiu chorego. Polski Merkuriusz Lekarski 2006, XXI, 197–200. [Google Scholar]
| Variables | Muslims | Jews | Catholics | SDA | |||||
|---|---|---|---|---|---|---|---|---|---|
| N-31 | % | N-14 | % | N-134 | % | N-118 | % | ||
| Level of religious commitment | High | 31 | 100 | 14 | 100 | 101 | 75.4 | 118 | 100 |
| Low | 0 | 0 | 0 | 0 | 33 | 24.6 | 0 | 0 | |
| Sex | Female | 18 | 58.1 | 10 | 71.4 | 87.0 | 64.9 | 75.0 | 63.6 |
| Male | 13 | 41.9 | 4 | 28.6 | 47.0 | 35.1 | 43.0 | 36.4 | |
| Place of residence | Village | 4 | 12.9 | 0 | 0.0 | 29.0 | 21.6 | 39.0 | 33.1 |
| City | 27 | 87.1 | 14 | 100.0 | 105.0 | 78.4 | 79.0 | 66.9 | |
| Education | Primary/Elementary | 1 | 3.0 | 1 | 7.0 | 7.0 | 5.2 | 6.0 | 5.1 |
| Vocational | 6 | 19.4 | 0 | 0,0 | 18.0 | 13.4 | 32.0 | 27.1 | |
| Secondary | 4 | 12.9 | 2 | 14.0 | 33.0 | 24.6 | 41.0 | 34.7 | |
| Higher | 20 | 64.5 | 11 | 78.6 | 79.0 | 56.8 | 39.0 | 33.1 | |
| Professional activity | Physical work | 4 | 12.9 | 1 | 7.0 | 17.0 | 12.7 | 39.0 | 33.1 |
| Intellectual work | 16 | 51.6 | 7 | 50.0 | 90.0 | 67.2 | 43.0 | 36.4 | |
| Unemployed | 11 | 35.5 | 6 | 42.6 | 27.0 | 20.1 | 36,0 | 30.5 | |
| Source of income | Professionally active | 19 | 61.3 | 7 | 50.0 | 94.0 | 70.2 | 75.0 | 63.6 |
| Disablement pension | 0 | 0.0 | 1 | 7.0 | 6.0 | 4.5 | 7.0 | 5.9 | |
| Retirement pension | 9 | 29.0 | 5 | 35.7 | 30.0 | 22.4 | 32.0 | 27.1 | |
| Benefits | 0 | 0.0 | 0 | 0.0 | 4.0 | 2.9 | 4.0 | 23.4 | |
| Range | M (SD) | Range | M (SD) | Range | M (SD) | Range | M (SD) | ||
| Age | 21–84 | 52.0 (17.5) | 22–82 | 53.9 (23.1) | 20–96 | 47.7 (16.0) | 24–94 | 53 (15.8) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Majda, A.; Bodys-Cupak, I.; Kamińska, A.; Suder, M.; Gródek-Szostak, Z. Religiously Conditioned Health Behaviors within Selected Religious Traditions. Int. J. Environ. Res. Public Health 2022, 19, 454. https://doi.org/10.3390/ijerph19010454
Majda A, Bodys-Cupak I, Kamińska A, Suder M, Gródek-Szostak Z. Religiously Conditioned Health Behaviors within Selected Religious Traditions. International Journal of Environmental Research and Public Health. 2022; 19(1):454. https://doi.org/10.3390/ijerph19010454
Chicago/Turabian StyleMajda, Anna, Iwona Bodys-Cupak, Alicja Kamińska, Marcin Suder, and Zofia Gródek-Szostak. 2022. "Religiously Conditioned Health Behaviors within Selected Religious Traditions" International Journal of Environmental Research and Public Health 19, no. 1: 454. https://doi.org/10.3390/ijerph19010454
APA StyleMajda, A., Bodys-Cupak, I., Kamińska, A., Suder, M., & Gródek-Szostak, Z. (2022). Religiously Conditioned Health Behaviors within Selected Religious Traditions. International Journal of Environmental Research and Public Health, 19(1), 454. https://doi.org/10.3390/ijerph19010454







