Institutional Responses to Drought in a High HIV Prevalence Setting in Rural South Africa
Abstract
:1. Introduction
2. Material and Methods
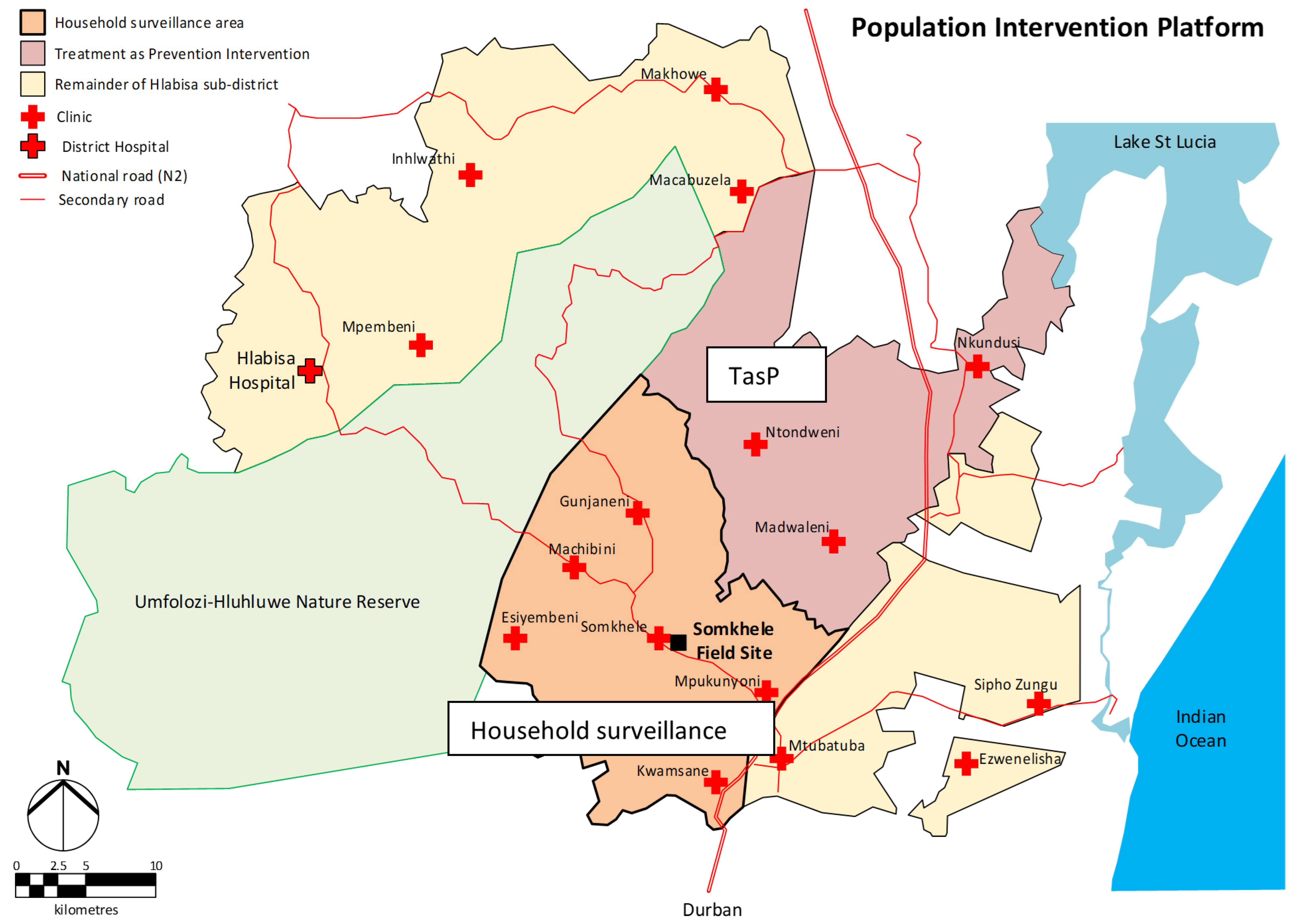
2.1. Study Setting
2.2. Data Collection and Analysis
3. Results
3.1. Experiences and Institutional Responses: The 2015 Drought in uMkhanyakude
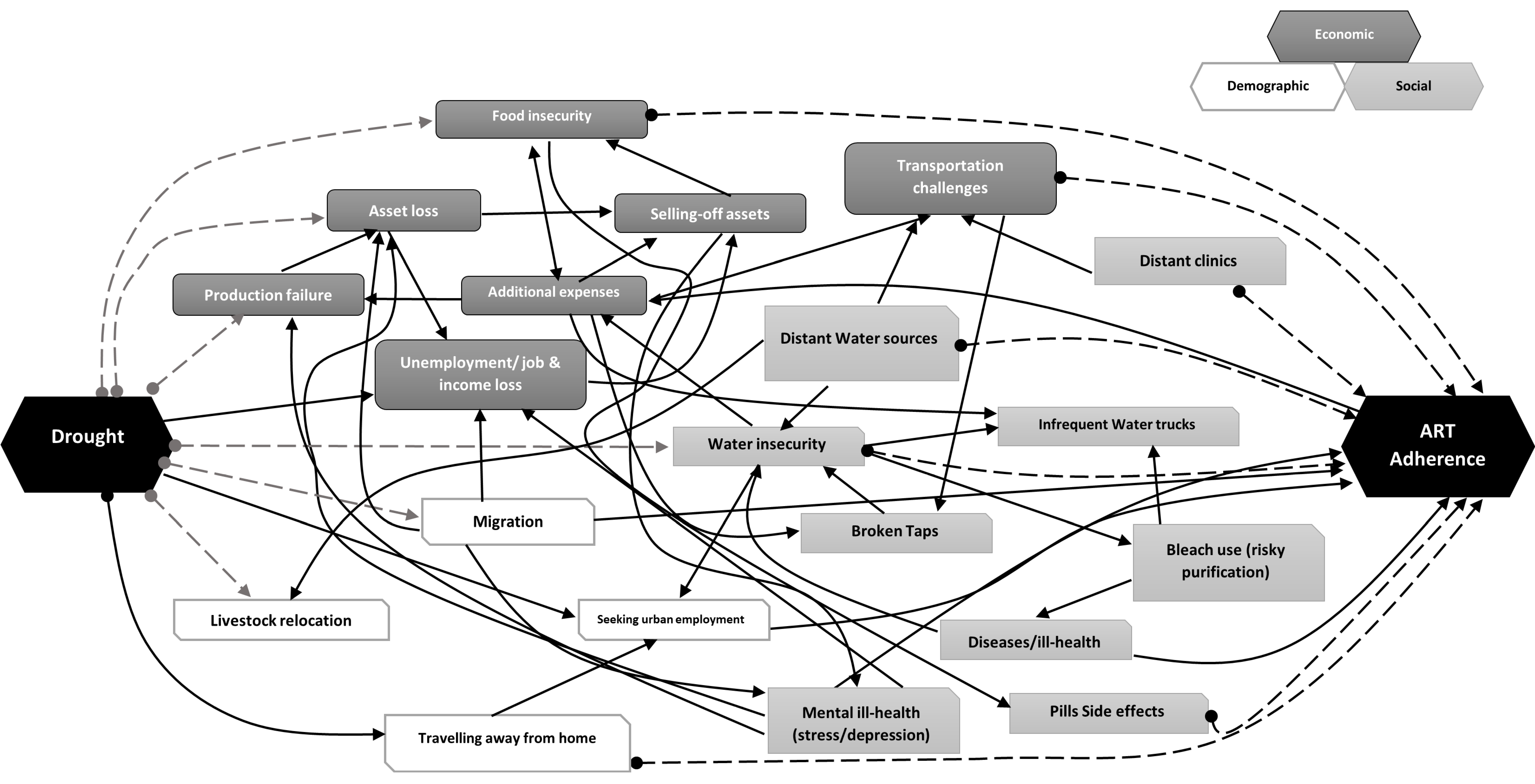
3.2. Drought’s Effects on Local Societies and PLHIV
3.3. Constraints on PLHIV’s Access to Treatment Care
3.4. Impacts on Government Institutions and Intervention Programmes
3.5. Government Interventions: Strategies and Drawbacks
“The information we took… was so useful such that we as the department now from an organizational perspective, we managed to see that there is a lack of dams for animals to drink because people are using water together with animals—they are competing with animals for drinking water. As you know, not everyone is able to go and buy drinking water like you and myself. So, that information assisted the department as well because after 2015 few dams were built, and few others were rehabilitated as well.” (GOVPART-IDI-041).
4. Discussion
Implications for PLHIV in uMkhanyakude
5. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- RSA (Republic of South Africa, Department of Agriculture). Drought Management Plan (DMP). Pretoria, South Africa. 2005. Available online: https://www.gov.za/sites/default/files/gcis_document/201409/2005dmp.pdf (accessed on 19 September 2021).
- RSA (Republic of South Africa). Disaster Management Act: Policy Framework for Disaster Risk Management in South Africa (Notice 654 of 2005). Pretoria, South Africa. 2005. Available online: https://www.gov.za/documents/disaster-management-act-policy-framework-disaster-risk-management-south-africa (accessed on 19 September 2021).
- Makaya, E.; Rohse, M.; Day, R.; Vogel, C.; Mehta, L.; McEwen, L.; Rangecroft, S.; Van Loon, A.F. Water governance challenges in rural South Africa: Exploring institutional coordination in drought management. Water Policy 2020, 22, 519–540. [Google Scholar] [CrossRef]
- Vogel, C.; Olivier, D. Re-imagining the potential of effective drought responses in South Africa. Reg. Environ. Chang. 2019, 19, 1561–1570. [Google Scholar] [CrossRef]
- Baudoin, M.A.; Vogel, C.; Nortje, K.; Naik, M. Living with drought in South Africa: Lessons learnt from the recent El Nino drought period. Int. J. Disaster Risk Reduct. 2017, 23, 128–137. [Google Scholar] [CrossRef]
- Wilhite, D.A.; Sivakumar, M.V.K.; Pulwarty, R. Managing drought risk in a changing climate: The role of national drought policy. Weather. Clim. Extrem. 2014, 3, 4–13. [Google Scholar] [CrossRef] [Green Version]
- IPCC. Summary for Policymakers. Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. 2021. In Press. Available online: https://www.ipcc.ch/report/sixth-assessment-report-working-group-i/ (accessed on 19 September 2021).
- Clover, J. Food Security in Sub-Saharan Africa. Afr. Secur. Rev. 2003, 12, 5–15. [Google Scholar] [CrossRef]
- Rouault, M.; Richard, Y. Intensity and spatial extension of drought in South Africa at different time scales. J. Water SA 2003, 29, 489–500. [Google Scholar] [CrossRef] [Green Version]
- Rouault, M.; Richard, Y. Intensity and spatial extent of droughts in southern Africa. Geophys. Res. Lett. 2005, 32, 1–4. [Google Scholar] [CrossRef]
- Stanke, C.; Kerac, M.; Prudhomme, C.; Medlock, J.; Murray, V. Health effects of drought: A systematic review of the evidence. PLoS Curr. 2013, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chersich, M.F.; Wright, C.Y.; Venter, F.; Rees, H.; Scorgie, F.; Erasmus, B. Impacts of Climate Change on Health and Wellbeing in South Africa. Int. J. Environ. Res. Public Health 2018, 15, 1884. [Google Scholar] [CrossRef] [Green Version]
- Peters, D.H. The application of systems thinking in health: Why use systems thinking? Health Res. Policy Syst. 2014, 12, 51. [Google Scholar] [CrossRef] [Green Version]
- Berry, H.L.; Waite, T.D.; Dear, K.B.G.; Capon, A.G.; Murray, V. The case for systems thinking about climate change and mental health. Nat. Clim. Chang. 2018, 8, 282–290. [Google Scholar] [CrossRef]
- Vins, H.; Bell, J.; Saha, S.; Hess, J.J. The Mental Health Outcomes of Drought: A Systematic Review and Causal Process Diagram. Int. J. Environ. Res. Public Health 2015, 12, 13251–13275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burke, M.; Gong, E.; Jones, K. Income Shocks and HIV in Africa. Econ. J. 2015, 125, 1157–1189. [Google Scholar] [CrossRef]
- Low, A.J.; Frederix, K.; McCracken, S.; Manyau, S.; Gummerson, E.; Radin, E.; Davia, S.; Longwe, H.; Ahmed, N.; Parekh, B.; et al. Association between severe drought and HIV prevention and care behaviors in Lesotho: A population-based survey 2016–2017. PLoS Med. 2019, 16, e1002727. [Google Scholar] [CrossRef] [Green Version]
- UNAIDS. The Gap Report, 2014; UN Joint Programme on HIV/AIDS: Geneva, Switzerland, 2014. Available online: https://www.unaids.org/en/resources/documents/2014/20140716_UNAIDS_gap_report (accessed on 19 September 2021).
- Iwuji, C.; McGrath, N.; Calmy, A.; Dabis, F.; Pillay, D.; Newell, M.L.; Baisley, K.; Porter, K. Universal test and treat is not associated with sub-optimal antiretroviral therapy adherence in rural South Africa: The ANRS 12249 TasP trial. J. Int. AIDS Soc. 2018, 21, e25112. [Google Scholar] [CrossRef] [PubMed]
- Vandormael, A.; Akullian, A.; Siedner, M.; de Oliveira, T.; Bärnighausen, T.; Tanser, F. Declines in HIV incidence among men and women in a South African population-based cohort. Nat. Commun. 2019, 10, 5482. [Google Scholar] [CrossRef] [Green Version]
- Chersich, M.F.; Wright, C.Y. Climate change adaptation in South Africa: A case study on the role of the health sector. Glob. Health 2019, 15, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muhwava, W.; Hosegood, V.; Nyirenda, M.; Newell, C.; Herbst, K.; Newell, M. Levels and determinants of population migration in rural KwaZulu-Natal, South Africa. Afr. Popul. Stud. 2010, 24, 259–280. [Google Scholar]
- Massyn, N.; Day, C.; Ndlovu, N.; Padayachee, T. District Health Barometer 2019/2020; Health Systems Trust: Durban, South Africa, 2020. [Google Scholar]
- Elliott, F.; Escott, B. Biodiversity Sector Plan—uMkhanyakude District Municipality; Ezemvelo KZN Wildlife: KwaZulu-Natal, South Africa, 2014. [Google Scholar]
- Morgenthal, T.L.; Kellner, K.; van Rensburg, L.; Newby, T.S.; van der Merwe, J.P.A. Vegetation and habitat types of the Umkhanyakude Node. S. Afr. J. Bot. 2006, 72, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Nachega, J.B.; Marconi, V.C.; van Zyl, G.U.; Gardner, E.M.; Preiser, W.; Hong, S.Y.; Mills, E.J.; Gross, R. HIV treatment adherence, drug resistance, virologic failure: Evolving concepts. Infect. Disord. Drug Targets 2011, 11, 167–174. [Google Scholar] [CrossRef] [Green Version]
- Orievulu, K.S.; Ayeb-Karlsson, S.; Ngema, S.U.; Baisley, K.; Tanser, F.; Ngwenya, N.; Seeley, J.; Hanekom, W.; Herbst, K.; Kniveton, D.; et al. Exploring linkages between drought and HIV treatment adherence in Africa: A Systematic Review. medRxiv 2020. [Google Scholar] [CrossRef]
- Masa, R.; Chowa, G.; Nyirenda, V. Barriers and facilitators of antiretroviral therapy adherence in rural Eastern province, Zambia: The role of household economic status. AJAR-Afr. J. Aids Res. 2017, 16, 91–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kheswa, J.G. Exploring the factors and effects of non-adherence to antiretroviral treatment by people living with HIV/AIDS. Indo-Pac. J. Phenomenol. 2017, 17, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Adeniyi, O.V.; Ajayi, A.I.; Ter Goon, D.; Owolabi, E.O.; Eboh, A.; Lambert, J. Factors affecting adherence to antiretroviral therapy among pregnant women in the Eastern Cape, South Africa. BMC Infect. Dis. 2018, 18, 175. [Google Scholar] [CrossRef] [Green Version]
- Haberer, J.E.; Bwana, B.M.; Orrell, C.; Asiimwe, S.; Amanyire, G.; Musinguzi, N.; Siedner, M.J.; Matthews, L.T.; Tsai, A.C.; Katz, I.T.; et al. ART adherence and viral suppression are high among most non-pregnant individuals with early-stage, asymptomatic HIV infection: An observational study from Uganda and South Africa. J. Int. Aids Soc. 2019, 22, e25232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hodgson, I.; Plummer, M.L.; Konopka, S.N.; Colvin, C.J.; Jonas, E.; Albertini, J.; Amzel, A.; Fogg, K.P. A systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum women. PLoS ONE 2014, 9, e111421. [Google Scholar] [CrossRef] [Green Version]
- Hayward, G.; Ayeb-Karlsson, S. ‘Seeing with Empty Eyes’: A systems approach to understand climate change and mental health in Bangladesh. Clim. Chang. 2021, 165, 29. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orievulu, K.S.; Iwuji, C.C. Institutional Responses to Drought in a High HIV Prevalence Setting in Rural South Africa. Int. J. Environ. Res. Public Health 2022, 19, 434. https://doi.org/10.3390/ijerph19010434
Orievulu KS, Iwuji CC. Institutional Responses to Drought in a High HIV Prevalence Setting in Rural South Africa. International Journal of Environmental Research and Public Health. 2022; 19(1):434. https://doi.org/10.3390/ijerph19010434
Chicago/Turabian StyleOrievulu, Kingsley S., and Collins C. Iwuji. 2022. "Institutional Responses to Drought in a High HIV Prevalence Setting in Rural South Africa" International Journal of Environmental Research and Public Health 19, no. 1: 434. https://doi.org/10.3390/ijerph19010434
APA StyleOrievulu, K. S., & Iwuji, C. C. (2022). Institutional Responses to Drought in a High HIV Prevalence Setting in Rural South Africa. International Journal of Environmental Research and Public Health, 19(1), 434. https://doi.org/10.3390/ijerph19010434






