Demographic and Clinical Factors Associated with Reactivity of Anti-SARS-CoV-2 Antibodies in Serbian Convalescent Plasma Donors
Abstract
:1. Introduction
2. Donors and Methods
2.1. Study Design
2.2. General Criteria for Study Enrollment
Serological and Molecular Detection of SARS-CoV-2 Infection
2.3. Laboratory Screening of CCP Donor Candidates
2.3.1. Hematological and Biochemical Parameter Screening
2.3.2. Screening for Markers of Transfusion-Transmitted Pathogens
2.3.3. ABO Typing
2.3.4. Quantification of IgG Reactive against SARS-CoV-2
2.4. COVID-19 Severity Assessment in CCP Donor Candidates
2.5. Parameters of Interest in CCP Donor Candidates
2.6. Statistical Analysis
3. Results
3.1. Majority of Enrolled Donor Candidates Had Anti-SARS-CoV-2 Abs above Acceptance Threshold
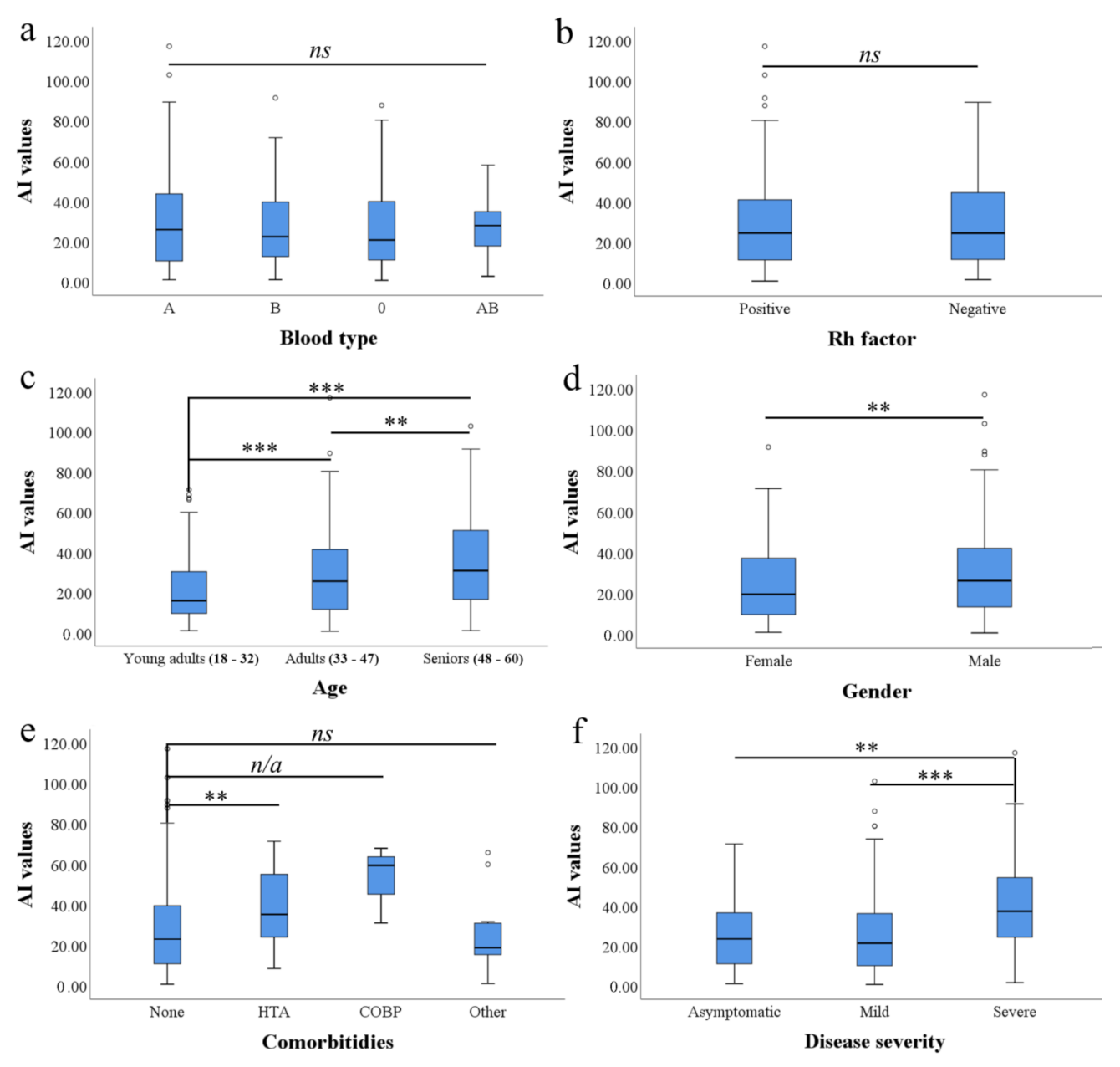
3.2. ABO Blood Type and RhD Factor Are Not Linked with Reactivity of Anti-SARS-CoV-2 Abs
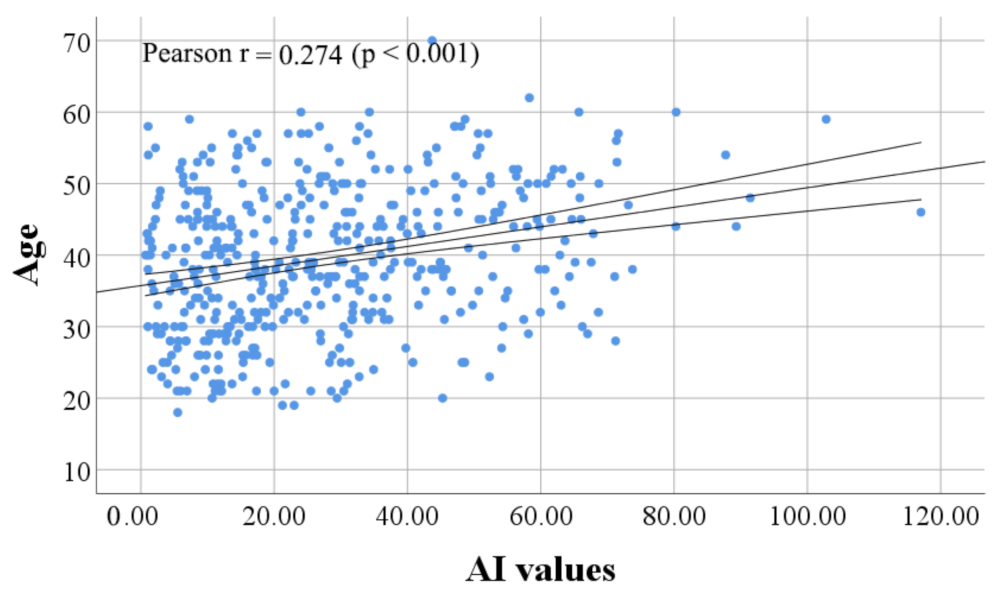
3.3. Age Was Associated with Reactivity of Anti-SARS-CoV-2 IgG in CCP Donor Candidates
3.4. Men Show Higher Anti-SARS-CoV-2 IgG Reactivity Than Women
3.5. Comorbidities and Anti-SARS-CoV-2 IgG Reactivity
3.6. Severity of COVID-19 Is Linked with Age and Anti-SARS-CoV-2 IgG Reactivity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Bio-Med. Atenei Parm. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Bogdanović, M.; Skadrić, I.; Atanasijević, T.; Stojković, O.; Popović, V.; Savić, S.; Mihailović, Z.; Radnić, B.; Aćimović, T.; Damjanjuk, I.; et al. Case Report: Post-Mortem Histopathological and Molecular Analyses of the Very First Documented COVID-19-Related Death in Europe. Front. Med. 2021, 8, 90. [Google Scholar] [CrossRef] [PubMed]
- Maier, H.E.; Kuan, G.; Saborio, S.; Carrillo, F.A.B.; Plazaola, M.; Barilla, C.; Sanchez, N.; Lopez, R.; Smith, M.; Kubale, J.; et al. Clinical Spectrum of Severe Acute Respiratory Syndrome Coronavirus 2 Infection and Protection From Symptomatic Reinfection. Clin. Infect. Dis. 2021. In press. [Google Scholar] [CrossRef]
- Baj, J.; Karakuła-Juchnowicz, H.; Teresiński, G.; Buszewicz, G.; Ciesielka, M.; Sitarz, E.; Forma, A.; Karakuła, K.; Flieger, W.; Portincasa, P.; et al. COVID-19: Specific and Non-Specific Clinical Manifestations and Symptoms: The Current State of Knowledge. J. Clin. Med. 2020, 9, 1753. [Google Scholar] [CrossRef]
- Long, B.; Brady, W.J.; Koyfman, A.; Gottlieb, M. Cardiovascular Complications in COVID-19. Am. J. Emerg. Med. 2020, 38, 1504–1507. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, I.; Rathore, F.A. Neurological Manifestations and Complications of COVID-19: A Literature Review. J. Clin. Neurosci. 2020, 77, 8–12. [Google Scholar] [CrossRef]
- Casadevall, A.; Pirofski, L. The Convalescent Sera Option for Containing COVID-19. J. Clin. Investig. 2020, 130, 1545–1548. [Google Scholar] [CrossRef] [Green Version]
- Bloch, E.M.; Shoham, S.; Casadevall, A.; Sachais, B.S.; Shaz, B.; Winters, J.L.; van Buskirk, C.; Grossman, B.J.; Joyner, M.; Henderson, J.P.; et al. Deployment of Convalescent Plasma for the Prevention and Treatment of COVID-19. J. Clin. Investig. 2020, 130, 2757–2765. [Google Scholar] [CrossRef] [Green Version]
- Kloypan, C.; Saesong, M.; Sangsuemoon, J.; Chantharit, P.; Mongkhon, P. CONVALESCENT Plasma for COVID-19: A Meta-Analysis of Clinical Trials and Real-World Evidence. Eur. J. Clin. Investig. 2021, 51, e13663. [Google Scholar] [CrossRef]
- Fodor, E.; Müller, V.; Iványi, Z.; Berki, T.; Olga, K.P.; Ambrus, M.; Sárkány, Á.; Skázel, Á.; Madár, Á.; Kardos, D.; et al. Early Transfusion of Convalescent Plasma Improves the Clinical Outcome in Severe SARS-CoV2 Infection. Infect. Dis. Ther. 2021, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Gharbharan, A.; Jordans, C.C.E.; GeurtsvanKessel, C.; den Hollander, J.G.; Karim, F.; Mollema, F.P.N.; Stalenhoef, J.E.; Dofferhoff, A.; Ludwig, I.; Koster, A.; et al. Convalescent Plasma for COVID-19. A Randomized Clinical Trial. Nat. Commun. 2021, 120, 3189. [Google Scholar] [CrossRef]
- Li, L.; Zhang, W.; Hu, Y.; Tong, X.; Zheng, S.; Yang, J.; Kong, Y.; Ren, L.; Wei, Q.; Mei, H.; et al. Effect of Convalescent Plasma Therapy on Time to Clinical Improvement in Patients With Severe and Life-Threatening COVID-19: A Randomized Clinical Trial. JAMA 2020, 324, 460–470. [Google Scholar] [CrossRef]
- Bégin, P.; Callum, J.; Jamula, E.; Cook, R.; Heddle, N.M.; Tinmouth, A.; Zeller, M.P.; Beaudoin-Bussières, G.; Amorim, L.; Bazin, R.; et al. Convalescent Plasma for Hospitalized Patients with COVID-19: An Open-Label, Randomized Controlled Trial. Nat. Med. 2021, 27, 1–13. [Google Scholar] [CrossRef]
- Briggs, N.; Gormally, M.V.; Li, F.; Browning, S.L.; Treggiari, M.M.; Morrison, A.; Laurent-Rolle, M.; Deng, Y.; Hendrickson, J.E.; Tormey, C.A.; et al. Early but Not Late Convalescent Plasma Is Associated with Better Survival in Moderate-to-Severe COVID-19. PLoS ONE 2021, 16, e0254453. [Google Scholar] [CrossRef] [PubMed]
- Vassallo, R.R.; Dumont, L.J.; Bravo, M.D.; Hazegh, K.; Kamel, H. Progression and Predictors of SARS-CoV-2 Antibody Seroreactivity In US Blood Donors. Transfus. Med. Rev. 2021, 35, 8–15. [Google Scholar] [CrossRef]
- Bainbridge, E.D.; Hsue, P.Y.; Esensten, J.H.; Lynch, K.L.; Hendrickson, C.M.; Doernberg, S.B.; Fung, M.; Chin-Hong, P.; Di Germanio, C.; Norris, P.J.; et al. Characteristics of High-Titer Convalescent Plasma and Antibody Dynamics After Administration in Patients With Severe Coronavirus Disease 2019. Open Forum Infect. Dis. 2021, 8, ofab385. [Google Scholar] [CrossRef] [PubMed]
- Bloch, E.M.; Patel, E.U.; Marshall, C.; Littlefield, K.; Goel, R.; Grossman, B.J.; Winters, J.L.; Shrestha, R.; Burgess, I.; Laeyendecker, O.; et al. ABO Blood Group and SARS-CoV-2 Antibody Response in a Convalescent Donor Population. Vox Sang. 2021, 116, 766–773. [Google Scholar] [CrossRef]
- De Bonetti, T.C.S.; Latini, F.R.M.; Invitti, A.L.; Fonseca, M.C.M.; Scorza, F.A.; Saldanha, M.G.; Bellucco, F.T.; Bacarov, N.B.S.; Soane, M.M.; Girão, M.J.B.C.; et al. Antibody Indexes in COVID-19 Convalescent Plasma Donors: Unanswered Questions. Clinics 2021, 76, e2818. [Google Scholar] [CrossRef]
- Klein, S.L.; Pekosz, A.; Park, H.-S.; Ursin, R.L.; Shapiro, J.R.; Benner, S.E.; Littlefield, K.; Kumar, S.; Naik, H.M.; Betenbaugh, M.J.; et al. Sex, Age, and Hospitalization Drive Antibody Responses in a COVID-19 Convalescent Plasma Donor Population. J. Clin. Investig. 2020, 130, 6141–6150. [Google Scholar] [CrossRef]
- Mehew, J.; Johnson, R.; Roberts, D.; Harvala, H. Convalescent Plasma for COVID-19: Male Gender, Older Age and Hospitalisation Associated with High Neutralising Antibody Levels, England, 22 April to 12 May 2020. Eurosurveillance 2020, 25, 2001754. [Google Scholar] [CrossRef]
- Körper, S.; Jahrsdörfer, B.; Corman, V.M.; Pilch, J.; Wuchter, P.; Blasczyk, R.; Müller, R.; Tonn, T.; Bakchoul, T.; Schäfer, R.; et al. Donors for SARS-CoV-2 Convalescent Plasma for a Controlled Clinical Trial: Donor Characteristics, Content and Time Course of SARS-CoV-2 Neutralizing Antibodies. Transfus. Med. Hemotherapy 2021, 48, 137–147. [Google Scholar] [CrossRef]
- Márquez-González, H.; López-Martínez, B.; Parra-Ortega, I.; de la Rosa-Zamboni, D.; Salazar-García, M.; Olivar-López, V.; Klünder-Klünder, M. Analysis of the Behaviour of Immunoglobulin G Antibodies in Children and Adults Convalescing From Severe Acute Respiratory Syndrome-Coronavirus-2 Infection. Front. Pediatr. 2021, 9, 671831. [Google Scholar] [CrossRef]
- Doniraj Plazmu—#COVID-19. Available online: https://donirajplazmu.gov.rs/ (accessed on 5 December 2021).
- Ristić, M.; Nikolić, N.; Čabarkapa, V.; Turkulov, V.; Petrović, V. Validation of the STANDARD Q COVID-19 Antigen Test in Vojvodina, Serbia. PLoS ONE 2021, 16, e0247606. [Google Scholar] [CrossRef] [PubMed]
- Vircell, S.L. (Ed.) COVID-19 ELISA IgG Assay Cat. No G1032; Parque Tecnológico de la Salud: Granada, Spain, 2020. [Google Scholar]
- COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health: Bethesda, MD, USA.
- WHO Clinical Management of COVID-19 Patients: Living Guidance. Available online: https://app.magicapp.org/#/guideline/j1WBYn/rec/EalkPn (accessed on 10 October 2021).
- McBride, R.; van Zyl, M.; Fielding, B.C. The Coronavirus Nucleocapsid Is a Multifunctional Protein. Viruses 2014, 6, 2991–3018. [Google Scholar] [CrossRef] [Green Version]
- Ibarrondo, F.J.; Fulcher, J.A.; Goodman-Meza, D.; Elliott, J.; Hofmann, C.; Hausner, M.A.; Ferbas, K.G.; Tobin, N.H.; Aldrovandi, G.M.; Yang, O.O. Rapid Decay of Anti-SARS-CoV-2 Antibodies in Persons with Mild Covid-19. N. Engl. J. Med. 2020, 383, 1085–1087. [Google Scholar] [CrossRef]
- Choudhary, H.R.; Parai, D.; Dash, G.C.; Peter, A.; Sahoo, S.K.; Pattnaik, M.; Rout, U.K.; Nanda, R.R.; Pati, S.; Bhattacharya, D. IgG Antibody Response against Nucleocapsid and Spike Protein Post-SARS-CoV-2 Infection. Infection 2021, 49, 1045–1048. [Google Scholar] [CrossRef] [PubMed]
- Altawalah, H. Antibody Responses to Natural SARS-CoV-2 Infection or after COVID-19 Vaccination. Vaccines 2021, 9, 910. [Google Scholar] [CrossRef] [PubMed]
- Hanssen, D.A.T.; Slaats, M.; Mulder, M.; Savelkoul, P.H.M.; van Loo, I.H.M. Evaluation of 18 Commercial Serological Assays for the Detection of Antibodies against SARS-CoV-2 in Paired Serum Samples. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 1695–1703. [Google Scholar] [CrossRef]
- Szabó, Z.; Szabó, T.; Bodó, K.; Kemenesi, G.; Földes, F.; Kristóf, K.; Barabás, E.; Vásárhelyi, B.; Prohászka, Z.; Fodor, E.; et al. Comparison of Virus Neutralization Activity and Results of 10 Different Anti-SARS-CoV-2 Serological Tests in COVID-19 Recovered Plasma Donors. Pract. Lab. Med. 2021, 25, e00222. [Google Scholar] [CrossRef]
- Abegaz, S.B. Human ABO Blood Groups and Their Associations with Different Diseases. BioMed Res. Int. 2021, 2021, 6629060. [Google Scholar] [CrossRef]
- Ewald, D.R.; Sumner, S.C.J. Blood Type Biochemistry and Human Disease. Wiley Interdiscip. Rev. Syst. Biol. Med. 2016, 8, 517–535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooling, L. Blood Groups in Infection and Host Susceptibility. Clin. Microbiol. Rev. 2015, 28, 801–870. [Google Scholar] [CrossRef] [Green Version]
- Guillon, P.; Clément, M.; Sébille, V.; Rivain, J.-G.; Chou, C.-F.; Ruvoën-Clouet, N.; Le Pendu, J. Inhibition of the Interaction between the SARS-CoV Spike Protein and Its Cellular Receptor by Anti-Histo-Blood Group Antibodies. Glycobiology 2008, 18, 1085–1093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, J.; Yang, Y.; Huang, H.; Li, D.; Gu, D.; Lu, X.; Zhang, Z.; Liu, L.; Liu, T.; Liu, Y.; et al. Relationship Between the ABO Blood Group and the Coronavirus Disease 2019 (COVID-19) Susceptibility. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2021, 73, 328–331. [Google Scholar] [CrossRef]
- Muñiz-Diaz, E.; Llopis, J.; Parra, R.; Roig, I.; Ferrer, G.; Grifols, J.; Millán, A.; Ene, G.; Ramiro, L.; Maglio, L.; et al. Relationship between the ABO Blood Group and COVID-19 Susceptibility, Severity and Mortality in Two Cohorts of Patients. Blood Transfus. Trasfus. Sangue 2021, 19, 54–63. [Google Scholar] [CrossRef]
- Goel, R.; Bloch, E.M.; Pirenne, F.; Al-Riyami, A.Z.; Crowe, E.; Dau, L.; Land, K.; Townsend, M.; Jecko, T.; Rahimi-Levene, N.; et al. ABO Blood Group and COVID-19: A Review on Behalf of the ISBT COVID-19 Working Group. Vox Sang. 2021, 116, 849–861. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Tong, X.; Chen, H.; He, R.; Lv, Q.; Yang, R.; Zhao, L.; Wang, J.; Xu, H.; Liu, C.; et al. Characteristics and Serological Patterns of COVID-19 Convalescent Plasma Donors: Optimal Donors and Timing of Donation. Transfusion (Paris) 2020, 60, 1765–1772. [Google Scholar] [CrossRef]
- Anstee, D.J. The Relationship between Blood Groups and Disease. Blood 2010, 115, 4635–4643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flegr, J. Influence of Latent Toxoplasma Infection on Human Personality, Physiology and Morphology: Pros and Cons of the Toxoplasma-Human Model in Studying the Manipulation Hypothesis. J. Exp. Biol. 2013, 216, 127–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ray, J.G.; Schull, M.J.; Vermeulen, M.J.; Park, A.L. Association between ABO and Rh Blood Groups and SARS-CoV-2 Infection or Severe COVID-19 Illness. Ann. Intern. Med. 2020, 174, 308–315. [Google Scholar] [CrossRef]
- Zietz, M.; Zucker, J.; Tatonetti, N.P. Associations between Blood Type and COVID-19 Infection, Intubation, and Death. Nat. Commun. 2020, 11, 5761. [Google Scholar] [CrossRef] [PubMed]
- Boudin, L.; Janvier, F.; Bylicki, O.; Dutasta, F. ABO Blood Groups Are Not Associated with Risk of Acquiring the SARS-CoV-2 Infection in Young Adults. Haematologica 2020, 105, 2841–2843. [Google Scholar] [CrossRef] [PubMed]
- Leaf, R.K.; Al-Samkari, H.; Brenner, S.K.; Gupta, S.; Leaf, D.E. ABO Phenotype and Death in Critically Ill Patients with COVID-19. Br. J. Haematol. 2020, 190, e204–e208. [Google Scholar] [CrossRef]
- Kim, Y.; Latz, C.A.; DeCarlo, C.S.; Lee, S.; Png, C.Y.M.; Kibrik, P.; Sung, E.; Alabi, O.; Dua, A. Relationship between Blood Type and Outcomes Following COVID-19 Infection. Semin. Vasc. Surg. 2021, 34, 125–131. [Google Scholar] [CrossRef]
- Hayes, C.; Rubenstein, W.; Gibb, D.; Klapper, E.; Tanaka, J.; Pepkowitz, S. Blood Group O Convalescent Plasma Donations Have Significantly Lower Levels of SARS-CoV-2 IgG Antibodies Compared to Blood Group A Donations. Transfusion 2021, 61, 2245–2249. [Google Scholar] [CrossRef]
- Madariaga, M.L.L.; Guthmiller, J.J.; Schrantz, S.; Jansen, M.O.; Christensen, C.; Kumar, M.; Prochaska, M.; Wool, G.; Durkin-Celauro, A.; Oh, W.H.; et al. Clinical Predictors of Donor Antibody Titre and Correlation with Recipient Antibody Response in a COVID-19 Convalescent Plasma Clinical Trial. J. Intern. Med. 2021, 289, 559–573. [Google Scholar] [CrossRef]
- Schmidt, J.; Berghaus, S.; Blessing, F.; Wenzel, F.; Herbeck, H.; Blessing, J.; Schierack, P.; Rödiger, S.; Roggenbuck, D. Serological and Viral Genetic Features of Patients with COVID-19 in a Selected German Patient Cohort—Correlation with Disease Characteristics. GeroScience 2021, 43, 2249–2264. [Google Scholar] [CrossRef]
- Gniadek, T.J.; Thiede, J.M.; Matchett, W.E.; Gress, A.R.; Pape, K.A.; Fiege, J.K.; Jenkins, M.K.; Menachery, V.D.; Langlois, R.A.; Bold, T.D. SARS-CoV-2 Neutralization and Serology Testing of COVID-19 Convalescent Plasma from Donors with Nonsevere Disease. Transfusion 2021, 61, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Jungbauer, C.; Weseslindtner, L.; Weidner, L.; Gänsdorfer, S.; Farcet, M.R.; Gschaider-Reichhart, E.; Kreil, T.R. Characterization of 100 Sequential SARS-CoV-2 Convalescent Plasma Donations. Transfusion 2021, 61, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Terpos, E.; Politou, M.; Sergentanis, T.N.; Mentis, A.; Rosati, M.; Stellas, D.; Bear, J.; Hu, X.; Felber, B.K.; Pappa, V.; et al. Anti–SARS-CoV-2 Antibody Responses in Convalescent Plasma Donors Are Increased in Hospitalized Patients; Subanalyses of a Phase 2 Clinical Study. Microorganisms 2020, 8, 1885. [Google Scholar] [CrossRef] [PubMed]
- Bandopadhyay, P.; D’Rozario, R.; Lahiri, A.; Sarif, J.; Ray, Y.; Paul, S.R.; Roy, R.; Maiti, R.; Chaudhuri, K.; Bagchi, S.; et al. Nature and Dimensions of Systemic Hyperinflammation and Its Attenuation by Convalescent Plasma in Severe COVID-19. J. Infect. Dis. 2021, 224, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Bartleson, J.M.; Radenkovic, D.; Covarrubias, A.J.; Furman, D.; Winer, D.A.; Verdin, E. SARS-CoV-2, COVID-19 and the Aging Immune System. Nat. Aging 2021, 1, 769–782. [Google Scholar] [CrossRef]
- Cancro, M.P. Age-Associated B Cells. Annu. Rev. Immunol. 2020, 38, 315–340. [Google Scholar] [CrossRef] [Green Version]
- Frasca, D. Senescent B Cells in Aging and Age-Related Diseases: Their Role in the Regulation of Antibody Responses. Exp. Gerontol. 2018, 107, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Woodruff, M.C.; Ramonell, R.P.; Nguyen, D.C.; Cashman, K.S.; Saini, A.S.; Haddad, N.S.; Ley, A.M.; Kyu, S.; Howell, J.C.; Ozturk, T.; et al. Extrafollicular B Cell Responses Correlate with Neutralizing Antibodies and Morbidity in COVID-19. Nat. Immunol. 2020, 21, 1506–1516. [Google Scholar] [CrossRef] [PubMed]
- Kunze, K.L.; Johnson, P.W.; van Helmond, N.; Senefeld, J.W.; Petersen, M.M.; Klassen, S.A.; Wiggins, C.C.; Klompas, A.M.; Bruno, K.A.; Mills, J.R.; et al. Mortality in Individuals Treated with COVID-19 Convalescent Plasma Varies with the Geographic Provenance of Donors. Nat. Commun. 2021, 12, 4864. [Google Scholar] [CrossRef] [PubMed]
- Korakas, E.; Ikonomidis, I.; Kousathana, F.; Balampanis, K.; Kountouri, A.; Raptis, A.; Palaiodimou, L.; Kokkinos, A.; Lambadiari, V. Obesity and COVID-19: Immune and Metabolic Derangement as a Possible Link to Adverse Clinical Outcomes. Am. J. Physiol. Endocrinol. Metab. 2020, 319, E105–E109. [Google Scholar] [CrossRef]
- Gonzalez-Quintela, A.; Alende, R.; Gude, F.; Campos, J.; Rey, J.; Meijide, L.M.; Fernandez-Merino, C.; Vidal, C. Serum Levels of Immunoglobulins (IgG, IgA, IgM) in a General Adult Population and Their Relationship with Alcohol Consumption, Smoking and Common Metabolic Abnormalities. Clin. Exp. Immunol. 2008, 151, 42–50. [Google Scholar] [CrossRef]
- Riou, M.; Marcot, C.; Canuet, M.; Renaud-Picard, B.; Chatron, E.; Porzio, M.; Dégot, T.; Hirschi, S.; Metz-Favre, C.; Kassegne, L.; et al. Clinical Characteristics of and Outcomes for Patients with COVID-19 and Comorbid Lung Diseases Primarily Hospitalized in a Conventional Pulmonology Unit: A Retrospective Study. Respir. Med. Res. 2021, 79, 100801. [Google Scholar] [CrossRef]
- Peng, M.; He, J.; Xue, Y.; Yang, X.; Liu, S.; Gong, Z. The Role of Hypertension on the Severity of COVID-19: A Review. J. Cardiovasc. Pharmacol. 2021, 78, e648–e655. [Google Scholar] [CrossRef]
- Ortona, E.; Pierdominici, M.; Rider, V. Editorial: Sex Hormones and Gender Differences in Immune Responses. Front. Immunol. 2019, 10, 1076. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giagulli, V.A.; Guastamacchia, E.; Magrone, T.; Jirillo, E.; Lisco, G.; De Pergola, G.; Triggiani, V. Worse Progression of COVID-19 in Men: Is Testosterone a Key Factor? Andrology 2021, 9, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Ciarambino, T.; Para, O.; Giordano, M. Immune System and COVID-19 by Sex Differences and Age. Womens Health 2021, 17, 17455065211022262. [Google Scholar] [CrossRef] [PubMed]
- Andreano, E.; Piccini, G.; Licastro, D.; Casalino, L.; Johnson, N.V.; Paciello, I.; Dal Monego, S.; Pantano, E.; Manganaro, N.; Manenti, A.; et al. SARS-CoV-2 Escape from a Highly Neutralizing COVID-19 Convalescent Plasma. Proc. Natl. Acad. Sci. USA 2021, 118, e2103154118. [Google Scholar] [CrossRef] [PubMed]
- Yaqinuddin, A.; Shafqat, A.; Kashir, J.; Alkattan, K. Effect of SARS-CoV-2 Mutations on the Efficacy of Antibody Therapy and Response to Vaccines. Vaccines 2021, 9, 914. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grujić, J.; Bujandrić, N.; Budakov-Obradović, Z.; Dolinaj, V.; Bogdan, D.; Savić, N.; Cabezas-Cruz, A.; Mijatović, D.; Simin, V.; Anđelić, N.; et al. Demographic and Clinical Factors Associated with Reactivity of Anti-SARS-CoV-2 Antibodies in Serbian Convalescent Plasma Donors. Int. J. Environ. Res. Public Health 2022, 19, 42. https://doi.org/10.3390/ijerph19010042
Grujić J, Bujandrić N, Budakov-Obradović Z, Dolinaj V, Bogdan D, Savić N, Cabezas-Cruz A, Mijatović D, Simin V, Anđelić N, et al. Demographic and Clinical Factors Associated with Reactivity of Anti-SARS-CoV-2 Antibodies in Serbian Convalescent Plasma Donors. International Journal of Environmental Research and Public Health. 2022; 19(1):42. https://doi.org/10.3390/ijerph19010042
Chicago/Turabian StyleGrujić, Jasmina, Nevenka Bujandrić, Zorana Budakov-Obradović, Vladimir Dolinaj, Damir Bogdan, Nebojša Savić, Alejandro Cabezas-Cruz, Dragana Mijatović, Verica Simin, Nikola Anđelić, and et al. 2022. "Demographic and Clinical Factors Associated with Reactivity of Anti-SARS-CoV-2 Antibodies in Serbian Convalescent Plasma Donors" International Journal of Environmental Research and Public Health 19, no. 1: 42. https://doi.org/10.3390/ijerph19010042
APA StyleGrujić, J., Bujandrić, N., Budakov-Obradović, Z., Dolinaj, V., Bogdan, D., Savić, N., Cabezas-Cruz, A., Mijatović, D., Simin, V., Anđelić, N., & Banović, P. (2022). Demographic and Clinical Factors Associated with Reactivity of Anti-SARS-CoV-2 Antibodies in Serbian Convalescent Plasma Donors. International Journal of Environmental Research and Public Health, 19(1), 42. https://doi.org/10.3390/ijerph19010042







