Near-Peer Teaching in Human Anatomy from a Tutors’ Perspective: An Eighteen-Year-Old Experience at the University of Bologna
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Survey Design
2.3. Quantitative Analysis
2.4. Qualitative Analysis
3. Results
3.1. Participation
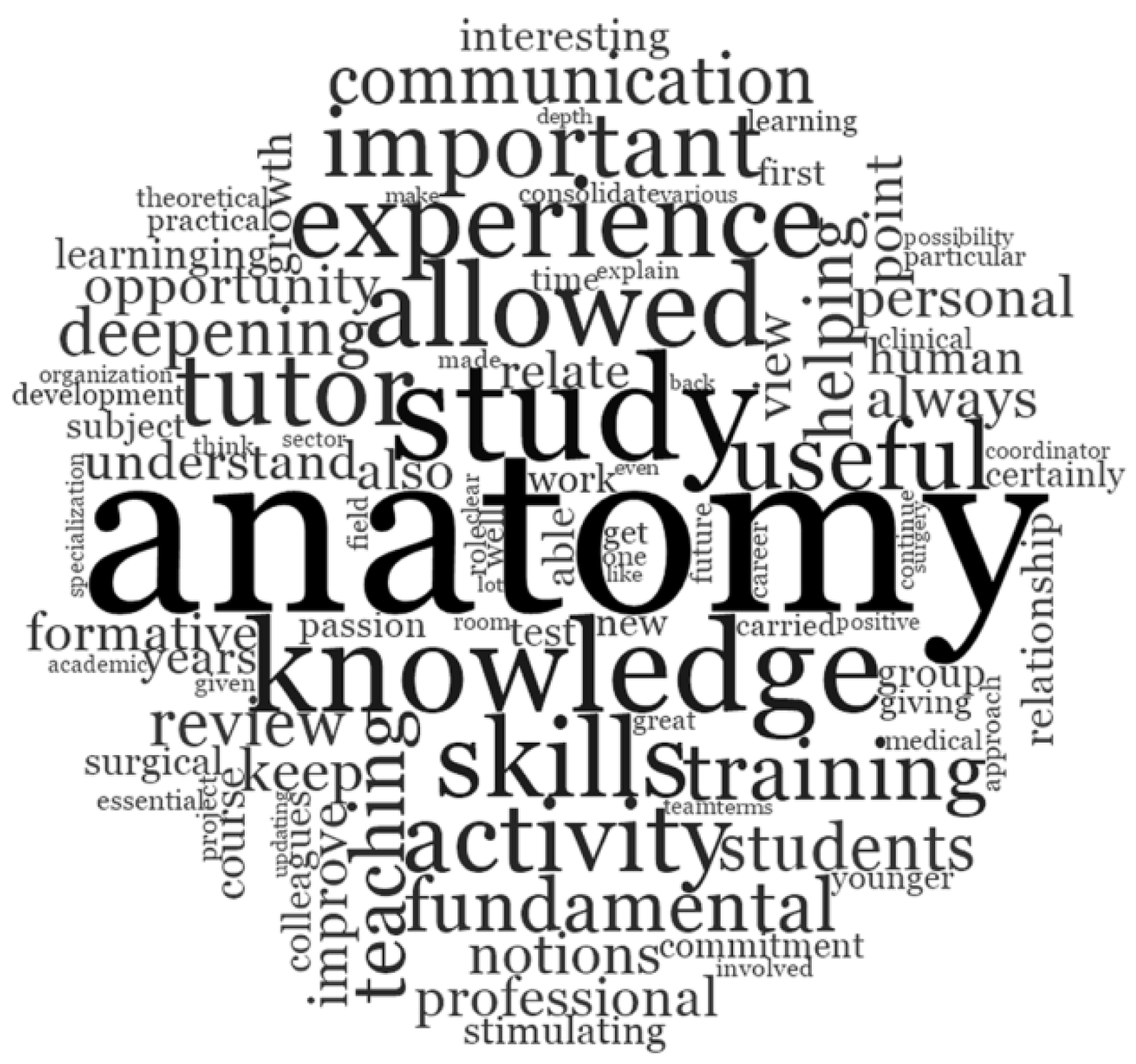
3.2. Evaluation of Quantitative Data and Open-Ended Queries
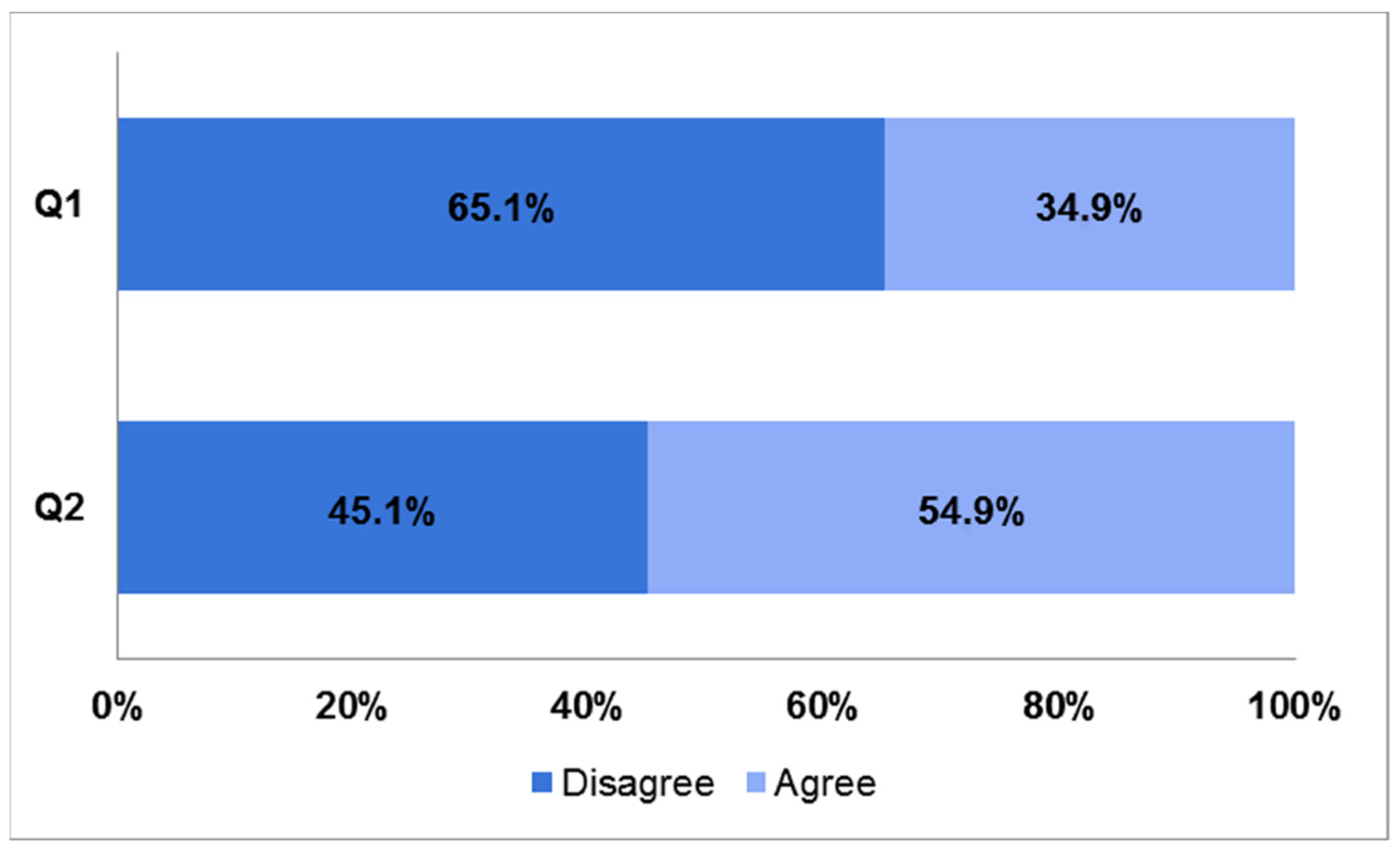
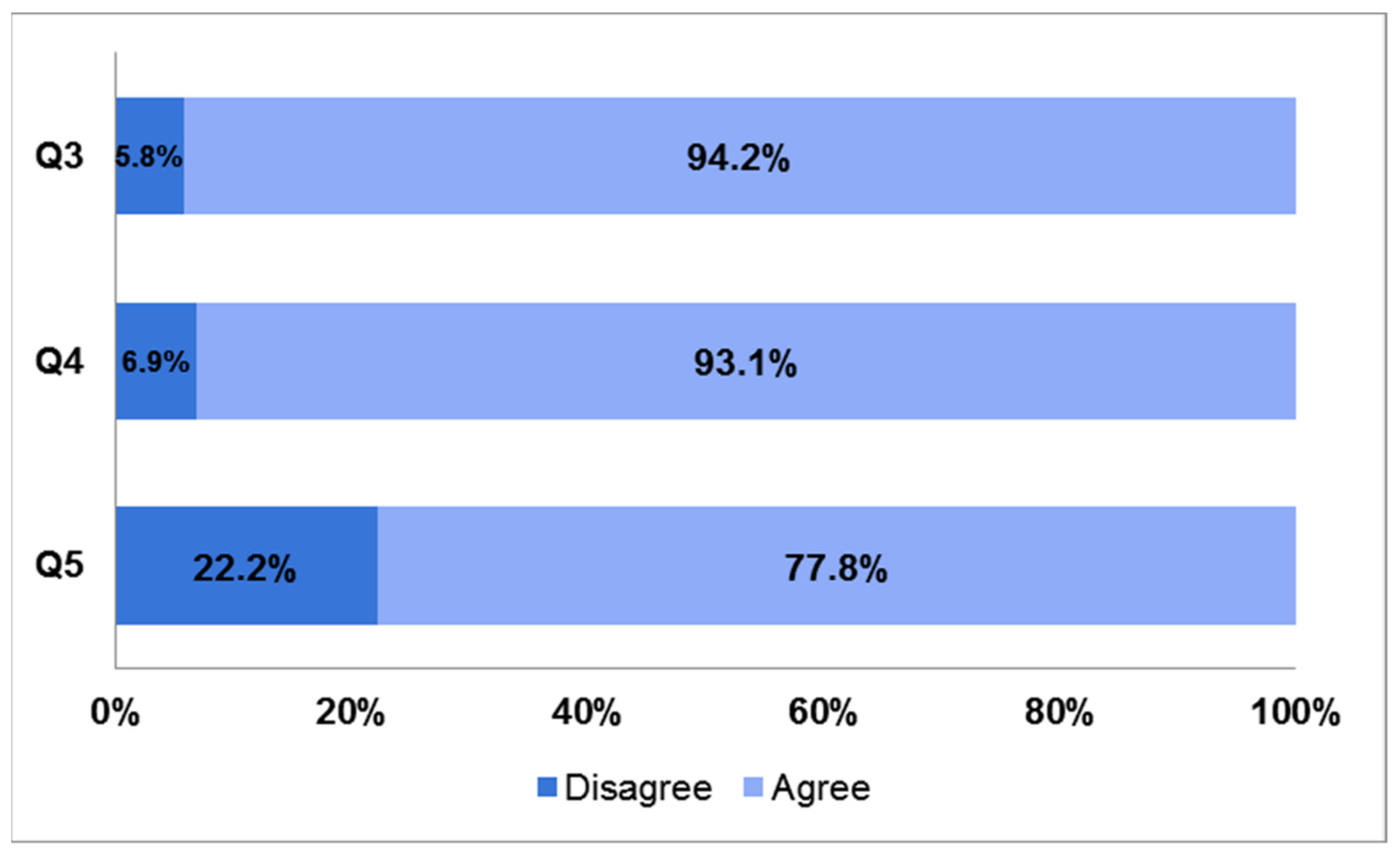
3.2.1. Impact on Education, Academic Achievement, and Career
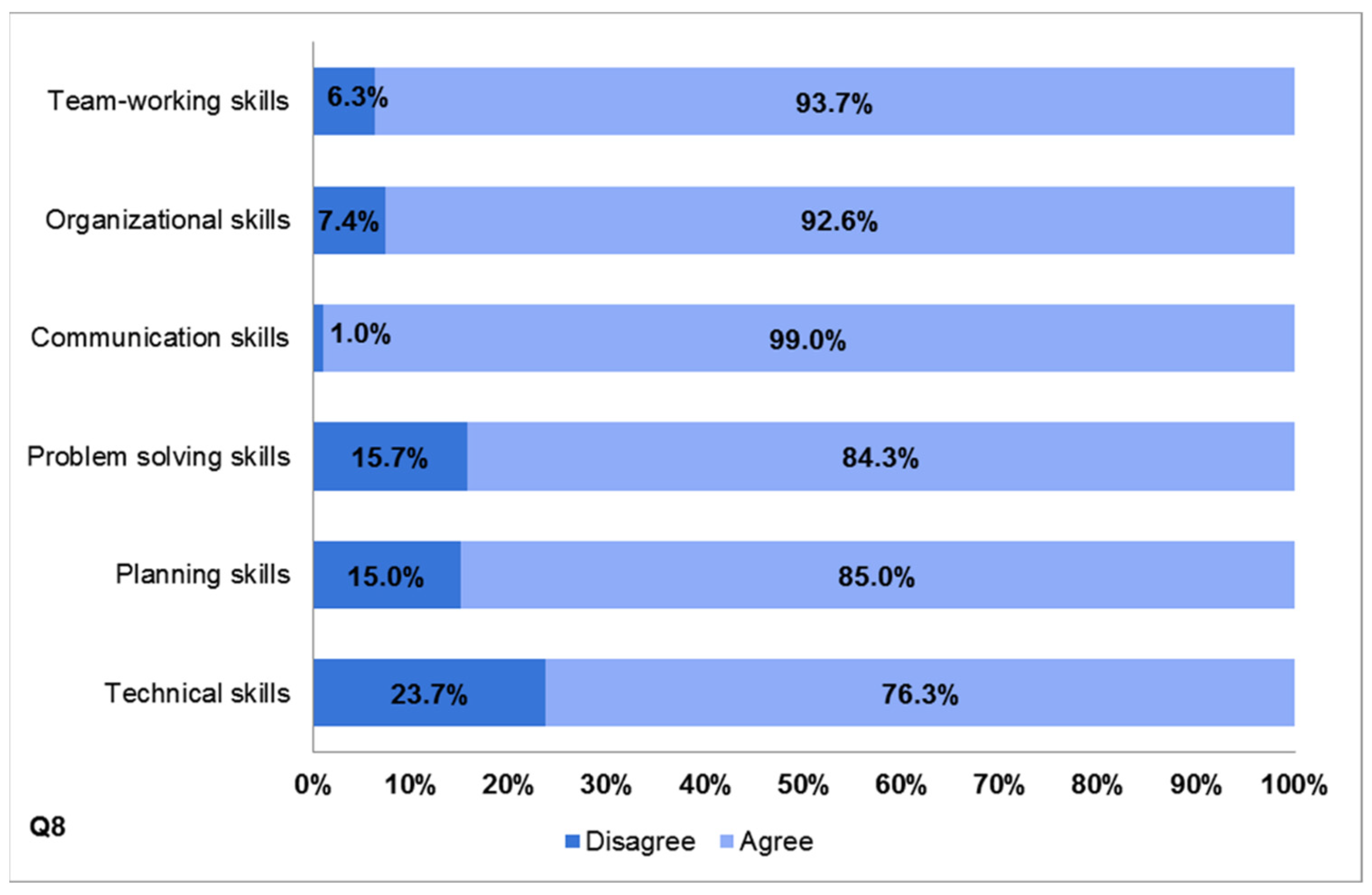
3.2.2. Improvement of Professional and Personal Skills
3.2.3. Impact of Cadaver Dissection on Learning and Professional Development
4. Discussion
4.1. Impact on Education, Academic Achievement, and Career
4.2. Improvement of Professional and Personal Skills
4.3. Impact of Cadaver Dissection on Learning and Professional Development
4.4. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| MEDICAL AREA | SURGICAL AREA | CLINICAL SERVICES AREA |
|---|---|---|
Class of GENERAL AND SPECIALISTIC CLINICAL MEDICINE
| Class of GENERAL AND SPECIALIST SURGERY
| Class of DIAGNOSTIC AND LABORATORY MEDICINE
|

Appendix B. Participants’ Demographics
References
- Orsini, E.; Quaranta, M.; Ratti, S.; Mariani, G.A.; Mongiorgi, S.; Billi, A.M.; Manzoli, L. The whole body donation program at the university of Bologna: A report based on the experience of one of the oldest university in Western world. Ann. Anat. 2021, 234, 151660. [Google Scholar] [CrossRef] [PubMed]
- Ocel, J.J.; Palmer, B.A.; Wittich, C.M.; Carmichael, S.W.; Pawlina, W. Outcomes of the gross and developmental anatomy teaching assistant experience. Clin. Anat. 2003, 16, 526–530. [Google Scholar] [CrossRef] [PubMed]
- Ross, M.T.; Cameron, H.S. Peer assisted learning: A planning and implementation framework: AMEE Guide no. 30. Med. Teach. 2007, 29, 527–545. [Google Scholar] [CrossRef] [PubMed]
- Soriano, R.P.; Blatt, B.; Coplit, L.; CichoskiKelly, E.; Kosowicz, L.; Newman, L.; Pasquale, S.J.; Pretorius, R.; Rosen, J.M.; Saks, N.S.; et al. Teaching medical students how to teach: A national survey of students-as-teachers programs in U.S. medical schools. Acad. Med. 2010, 85, 1725–1731. [Google Scholar] [CrossRef]
- Bugaj, T.J.; Blohm, M.; Schmid, C.; Koehl, N.; Huber, J.; Huhn, D.; Herzog, W.; Krautter, M.; Nikendei, C. Peer-assisted learning (PAL): Skills lab tutors’ experiences and motivation. BMC Med. Educ. 2019, 19, 353. [Google Scholar] [CrossRef] [PubMed]
- Biggs, J. Enhancing teaching through constructive alignment. High Educ. 1996, 32, 347–364. [Google Scholar] [CrossRef]
- Egan, T.; Jaye, C. Communities of clinical practice: The social organization of clinical learning. Health 2009, 13, 107–125. [Google Scholar] [CrossRef]
- Mann, K.V. Theoretical perspectives in medical education: Past experience and future possibilities. Med. Educ. 2011, 45, 60–68. [Google Scholar] [CrossRef]
- Knowles, M.S.; Holton, E.F.; Swanson, R.A. The Adult Learner: The Definitive Classic in Adult Education and Human Resource Development, 6th ed.; Elsevier: Burlington, MA, USA, 2005; p. 378. [Google Scholar]
- Topping, K.J. Trends in Peer Learning. Educ. Psychol. 2007, 25, 15. [Google Scholar] [CrossRef]
- Ten Cate, O.; Durning, S. Dimensions and psychology of peer teaching in medical education. Med. Teach. 2007, 29, 546–552. [Google Scholar] [CrossRef]
- Lockspeiser, T.M.; O’Sullivan, P.; Teherani, A.; Muller, J. Understanding the experience of being taught by peers: The value of social and cognitive congruence. Adv. Health Sci. Educ. 2008, 13, 361–372. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, H.G.; Moust, J.H. What makes a tutor effective? A structural-equations modeling approach to learning in problem-based curricula. Acad. Med. 1995, 70, 708–714. [Google Scholar] [CrossRef] [PubMed]
- De Caro, R.; Macchi, V.; Porzionato, A. Promotion of body donation and use of cadavers in anatomical education at the University of Padova. Anat. Sci. Educ. 2009, 2, 91–92. [Google Scholar] [CrossRef] [PubMed]
- Macchi, V.; Porzionato, A.; Stecco, C.; Parenti, A.; De Caro, R. Clinical neuroanatomy module 5 years’ experience at the School of Medicine of Padova. Surg. Radiol. Anat. 2007, 29, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Ten Cate, O.; Durning, S. Peer teaching in medical education: Twelve reasons to move from theory to practice. Med. Teach. 2007, 29, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Duran, C.E.; Bahena, E.N.; Rodriguez Mde, L.; Baca, G.J.; Uresti, A.S.; Elizondo-Omana, R.E.; Lopez, S.G. Near-peer teaching in an anatomy course with a low faculty-to-student ratio. Anat. Sci. Educ. 2012, 5, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Field, M.; Burke, J.M.; McAllister, D.; Lloyd, D.M. Peer-assisted learning: A novel approach to clinical skills learning for medical students. Med. Educ. 2007, 41, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, I.A.G.; Fung, I.Y.Y. Small-group composition and peer effects. Int. J. Educ. Res. 2002, 37, 23. [Google Scholar] [CrossRef]
- Engels, D.; Haupt, C.; Kugelmann, D.; Dethleffsen, K. The peer teachers’ perception of intrinsic motivation and rewards. Adv. Physiol. Educ. 2021, 45, 758–768. [Google Scholar] [CrossRef]
- Loda, T.; Erschens, R.; Loenneker, H.; Keifenheim, K.E.; Nikendei, C.; Junne, F.; Zipfel, S.; Herrmann-Werner, A. Cognitive and social congruence in peer-assisted learning—A scoping review. PLoS ONE 2019, 14, e0222224. [Google Scholar] [CrossRef]
- Loda, T.; Erschens, R.; Nikendei, C.; Zipfel, S.; Herrmann-Werner, A. Qualitative analysis of cognitive and social congruence in peer-assisted learning—The perspectives of medical students, student tutors and lecturers. Med. Educ. Online 2020, 25, 1801306. [Google Scholar] [CrossRef]
- Topping, K.J.; Ehly, S. Peer-Assisted Learning, 1st ed.; Routledge: New York, NY, USA, 1998; p. 392. [Google Scholar]
- Yew, E.H.J.; Yong, J.J.Y. Student perceptions of facilitators’ social congruence, use of expertise and cognitive congruence in problem-based learning. Instr. Sci. 2014, 42, 795–815. [Google Scholar] [CrossRef]
- Armstrong, D.; Hicks, B.H.; Higgins, P.M.; Weinman, J.A. Teaching communication skills to pre-clinical medical students: A general practice based approach. Med. Educ. 1979, 13, 82–85. [Google Scholar] [CrossRef] [PubMed]
- Erie, A.J.; Starkman, S.J.; Pawlina, W.; Lachman, N. Developing Medical Students as Teachers: An Anatomy-Based Student-As-Teacher Program with Emphasis on Core Teaching Competencies. Anat. Sci. Educ. 2013, 6, 385–392. [Google Scholar] [CrossRef]
- Hall, S.; Harrison, C.H.; Stephens, J.; Andrade, M.G.; Seaby, E.G.; Parton, W.; McElligott, S.; Myers, M.A.; Elmansouri, A.; Ahn, M.; et al. The benefits of being a near-peer teacher. Clin. Teach. 2018, 15, 403–407. [Google Scholar] [CrossRef]
- Maguire, P.; Pitceathly, C. Key communication skills and how to acquire them. BMJ 2002, 325, 697–700. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; McGregor, D. Peer teacher training for health professional students: A systematic review of formal programs. BMC Med. Educ. 2018, 18, 263. [Google Scholar] [CrossRef]
- Burgess, A.; McGregor, D.; Mellis, C. Medical students as peer tutors: A systematic review. BMC Med. Educ. 2014, 14, 115. [Google Scholar] [CrossRef]
- Evans, D.J.; Cuffe, T. Near-peer teaching in anatomy: An approach for deeper learning. Anat. Sci. Educ. 2009, 2, 227–233. [Google Scholar] [CrossRef]
- Shiozawa, T.; Hirt, B.; Celebi, N.; Baur, F.; Weyrich, P.; Lammerding-Koppel, M. Development and implementation of a technical and didactical training program for student tutors in the dissection course. Ann. Anat. 2010, 192, 355–360. [Google Scholar] [CrossRef]
- Reyes-Hernandez, C.G.; Carmona Pulido, J.M.; De la Garza Chapa, R.I.; Serna Vazquez, R.P.; Alcala Briones, R.D.; Plasencia Banda, P.M.; Villarreal Silva, E.E.; Jacobo Baca, G.; de la Garza Castro, O.; Elizondo Omana, R.E.; et al. Near-peer teaching strategy in a large human anatomy course: Perceptions of near-peer instructors. Anat. Sci. Educ. 2015, 8, 189–193. [Google Scholar] [CrossRef]
- Dandavino, M.; Snell, L.; Wiseman, J. Why medical students should learn how to teach. Med. Teach. 2007, 29, 558–565. [Google Scholar] [CrossRef]
- Learning Together to Work Together for Health: Report of a WHO Study Group on Multiprofessional Education of Health Personnel: The Team Approach; World Health Organ Tech Rep Ser 769; World Health Organization: Geneva, Switzerland, 1988; pp. 1–72.
- Jackson, T.A.; Evans, D.J. Can medical students teach? A near-peer-led teaching program for year 1 students. Adv. Physiol. Educ. 2012, 36, 192–196. [Google Scholar] [CrossRef] [PubMed]
- Peets, A.D.; Coderre, S.; Wright, B.; Jenkins, D.; Burak, K.; Leskosky, S.; McLaughlin, K. Involvement in teaching improves learning in medical students: A randomized cross-over study. BMC Med. Educ. 2009, 9, 55. [Google Scholar] [CrossRef]
- Sobral, D.T. Cross-year peer tutoring experience in a medical school: Conditions and outcomes for student tutors. Med. Educ. 2002, 36, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Frey, J.H.; Whitman, N.A. Peer Teaching: To Teach Is to Learn Twice; Association for the Study of Higher Education; ERIC Clearinghouse on Higher Education: Washington, DC, USA, 1988; p. 103. [Google Scholar]
- Beard, J.H.; O’Sullivan, P.; Palmer, B.J.; Qiu, M.; Kim, E.H. Peer assisted learning in surgical skills laboratory training: A pilot study. Med. Teach. 2012, 34, 957–959. [Google Scholar] [CrossRef] [PubMed]
- Loke, A.J.; Chow, F.L. Learning partnership—The experience of peer tutoring among nursing students: A qualitative study. Int. J. Nurs. Stud. 2007, 44, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Secomb, J. A systematic review of peer teaching and learning in clinical education. J. Clin. Nurs. 2008, 17, 703–716. [Google Scholar] [CrossRef]
- Best, G.; Hajzler, D.; Ivanov, T.; Limon, J. Peer Mentoring as a Strategy to Improve Paramedic Students’ Clinical Skills. J. Peer Learn. 2008, 1, 13. [Google Scholar]
- Buckley, S.; Zamora, J. Effects of participation in a cross year peer tutoring programme in clinical examination skills on volunteer tutors’ skills and attitudes towards teachers and teaching. BMC Med. Educ. 2007, 7, 20. [Google Scholar] [CrossRef]
- Blanchard, D.S. Peer-teaching: An important skill for all medical students and doctors? Perspect. Med. Educ. 2015, 4, 6–7. [Google Scholar] [CrossRef][Green Version]
- Parr, J.M.; Townsend, M.A.R. Environments, processes, and mechanisms in peer learning. Int. J. Educ. Res. 2002, 37, 20. [Google Scholar] [CrossRef]
- Cornwall, J.; Stringer, M.D. The wider importance of cadavers: Educational and research diversity from a body bequest program. Anat. Sci. Educ. 2009, 2, 234–237. [Google Scholar] [CrossRef]
- Ellis, H. Teaching in the dissecting room. Clin. Anat. 2001, 14, 149–151. [Google Scholar] [CrossRef]
- Guo, K.; Luo, T.; Zhou, L.H.; Xu, D.; Zhong, G.; Wang, H.; Xu, J.; Chu, G. Cultivation of humanistic values in medical education through anatomy pedagogy and gratitude ceremony for body donors. BMC Med. Educ. 2020, 20, 440. [Google Scholar] [CrossRef]
- Korf, H.W.; Wicht, H.; Snipes, R.L.; Timmermans, J.P.; Paulsen, F.; Rune, G.; Baumgart-Vogt, E. The dissection course-necessary and indispensable for teaching anatomy to medical students. Ann. Anat. 2008, 190, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Orsbon, C.P.; Kaiser, R.S.; Ross, C.F. Physician opinions about an anatomy core curriculum: A case for medical imaging and vertical integration. Anat. Sci. Educ. 2014, 7, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Bohl, M.; Bosch, P.; Hildebrandt, S. Medical students’ perceptions of the body donor as a “first patient” or “teacher”: A pilot study. Anat. Sci. Educ. 2011, 4, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.C.; Hsu, J.; Fan, V.Y. “Silent virtuous teachers”: Anatomical dissection in Taiwan. BMJ 2009, 339, b5001. [Google Scholar] [CrossRef] [PubMed]

| Questions and Statements | SD | D | A | SA | |
|---|---|---|---|---|---|
| Impact on Education, Academic Achievement and Career | |||||
| Q1 | I had a clear career path plan when I entered medical school | 26.1% | 39.0% | 24.1% | 10.8% |
| Q2 | My career path plan has been affected by near-peer tutoring experience | 12.7% | 32.4% | 37.7% | 17.2% |
| Q3 | Attending/graduating at University of Bologna medical school has brought an added value to my education | 0.7% | 5.1% | 35.2% | 59.0% |
| Q4 | In the case of positive response to the previous question, it was my experience as a neer-peer tutor that mainly affected it | 0.4% | 6.5% | 45.6% | 47.5% |
| Q5 | I noticed differences in attitudes and preparation among colleagues who were not enrolled as near-peer tutors | 3.0% | 19.2% | 47.7% | 30.1% |
| Q6 | As a tutee, prior to being enrolled as tutor, I appreciated/enjoyed the near-peer teaching model in human anatomy education | 0.7% | 0.7% | 15.2% | 83.4% |
| Q7 | I would recommend near-peer tutoring experience as a beneficial tool in preclinical education pathway to early years medical students | 0.0% | 0.7% | 12.3% | 87.0% |
| A | What were the strengths of this neer-peer tutoring model? | Open-ended question | |||
| Improvement of professional and personal skills | |||||
| Q8 | Near-peer tutoring experience helped me to develop the following skills:
| ||||
| 1.1% | 5.2% | 36.2% | 57.5% | ||
| 0.7% | 6.7% | 41.8% | 50.8% | ||
| 0.0% | 1.0% | 14.3% | 84.7% | ||
| 1.7% | 14.0% | 44.2% | 40.1% | ||
| 2.1% | 12.9% | 47.4% | 37.6% | ||
| 3.2% | 20.5% | 30.0% | 46.3% | ||
| Q9 | The opportunity to constantly revise anatomy helped me to improve my academic performance | 0.7% | 6.3% | 43.9% | 49.1% |
| Q10 | Near-peer tutoring experience helped me to increase my self-confidence | 0.7% | 8.4% | 41.5% | 49.4% |
| Q11 | Near-peer tutoring experience helped me to develop a proactive approach to the degree course | 0.0% | 9.8% | 37.1% | 53.1% |
| B | Describe the role near-peer tutoring experience plays/played in your professional career. | Open-ended question | |||
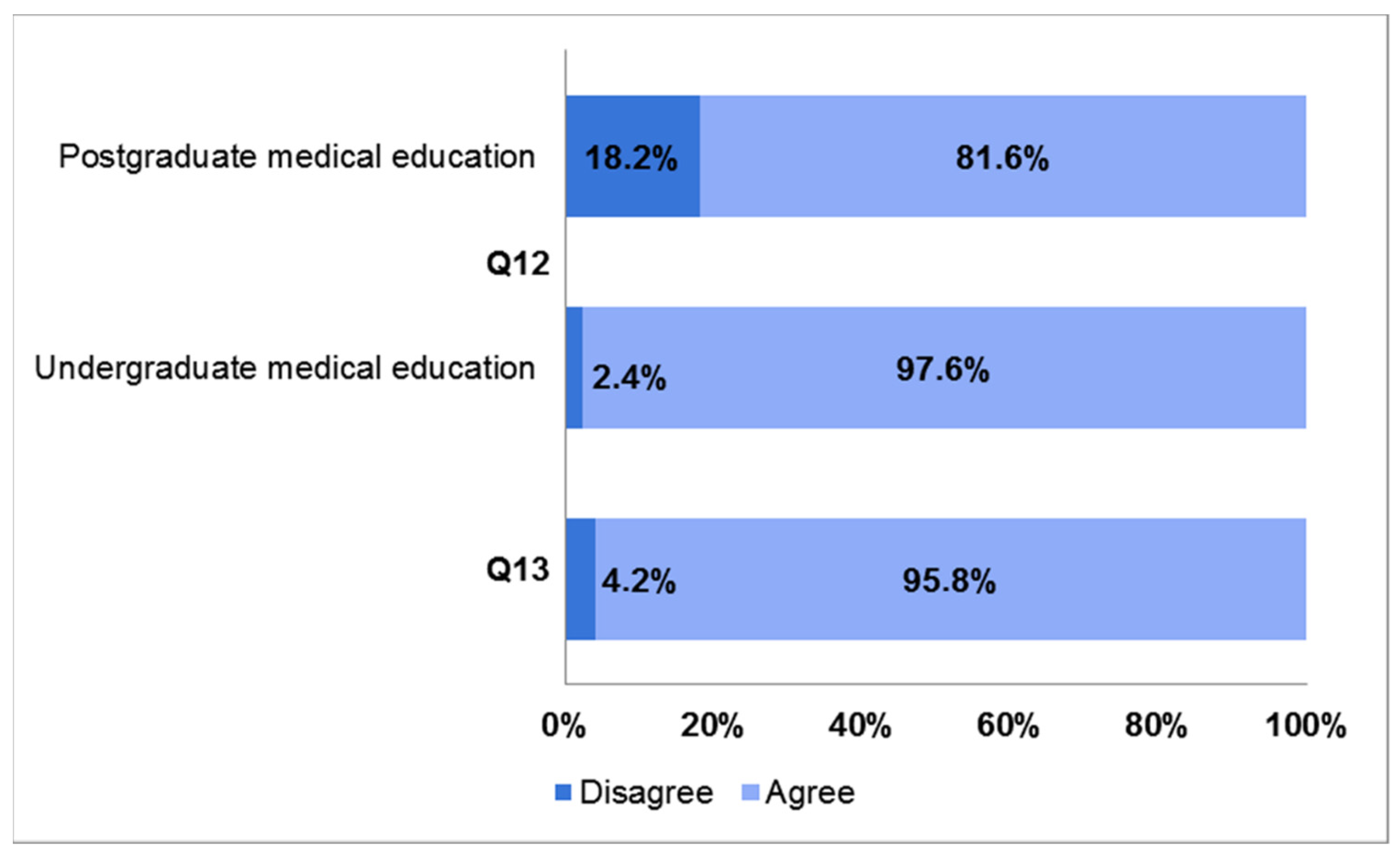
| Impact of cadaver dissection on learning and professional development | |||||
| Q12 | Cadaver dissection is an invaluable and necessary learning tool in:
| ||||
| 0.0% | 2.4% | 20.8% | 76.8% | ||
| 2.2% | 16.0% | 35.4% | 46.2% | ||
| Q13 | Cadaver dissection is a powerful tool in positively shaping professional and ethical values like compassion, empathy and respect toward patients | 0.6% | 3.6% | 30.9% | 64.9% |
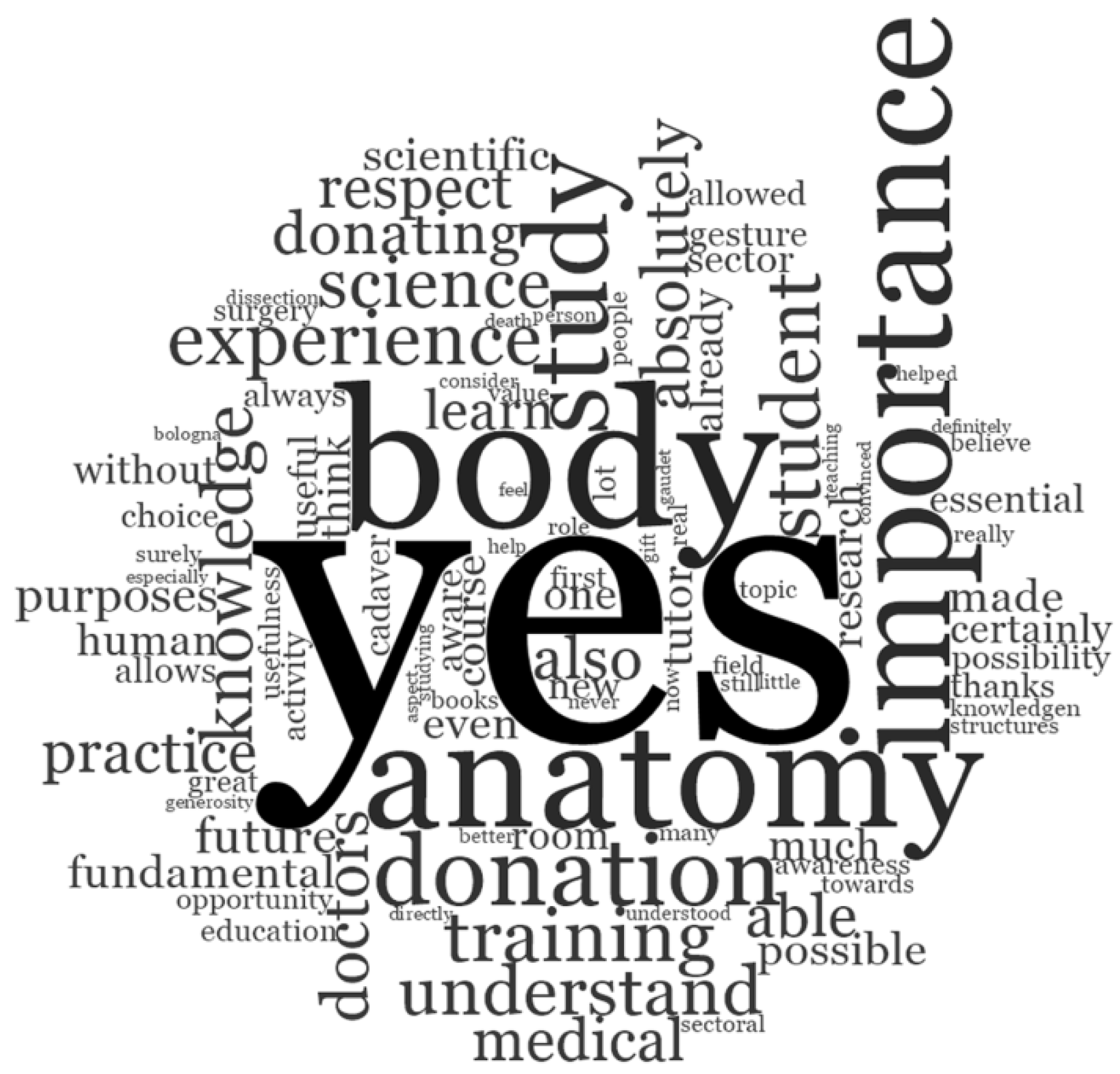
| C | Did near-peer tutoring experience positively influence your perception towards body donation for medical education and scientific purposes? | Open-ended question | |||
| Themes | Subthemes | Example Comments |
|---|---|---|
| Impact on education, academic achievement, and career | Education | The hands-on experience has allowed a better memorization of what has been studied in books. |
| Academic achievement | Seeing colleagues only a few years older able to master such a complex subject in such a clear and confident way helped me to deal with it in a different way when preparing for the exam and contributed to the considerable interest in the subject that I still study today. | |
| Career | I consider my experience as anatomy tutor as a fundamental part of my professional career. I have not only been able to follow several students during their second year of studies, but I have also been able to have a concrete example of interdisciplinary collaboration and functionality, fundamental in my work. | |
| Improvement of professional and personal skills | Practical skills | It prepares for what the hospital reality is and promotes the development of clinical thinking and technical skills. It makes you extremely prepared and allows you to interact during internships. |
| Attitude | It allowed to understand the importance of anatomical-clinical correlations and to develop teaching and communication skills; the organization of teaching activities contributed to the development of organizational skills. | |
| Knowledge | It has certainly consolidated my knowledge, giving me an overview of the topographical anatomy otherwise difficult to acquire with the theoretical study only, which helps me a lot in my current clinical work, especially in the interpretation of diagnostic images. It also allowed me to get in touch with the world of research and conferences at an early stage. | |
| Impact of cadaver dissection on learning and professional development | Awareness of body donation | Before my experience as a student in the dissecting room, I did not even know that there was the possibility of studying anatomy on cadaver in Italy. |
| Effectiveness of body donation | Yes. Studying anatomy on cadaver and not only in atlases is essential to fully and deeply understand it. Donating one’s body for such purposes is a way to promote the education of future doctors and therefore the quality of public health. | |
| Ethical value of body donation | Yes. Body donation is a gesture of great generosity and unconditional trust in medical science which contributes to the advancement of medical education and biomedical research. Treating donors and our future patients with the highest level of respect, care and dedication will be our concrete forms of gratefulness. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orsini, E.; Quaranta, M.; Mariani, G.A.; Mongiorgi, S.; Cocco, L.; Billi, A.M.; Manzoli, L.; Ratti, S. Near-Peer Teaching in Human Anatomy from a Tutors’ Perspective: An Eighteen-Year-Old Experience at the University of Bologna. Int. J. Environ. Res. Public Health 2022, 19, 398. https://doi.org/10.3390/ijerph19010398
Orsini E, Quaranta M, Mariani GA, Mongiorgi S, Cocco L, Billi AM, Manzoli L, Ratti S. Near-Peer Teaching in Human Anatomy from a Tutors’ Perspective: An Eighteen-Year-Old Experience at the University of Bologna. International Journal of Environmental Research and Public Health. 2022; 19(1):398. https://doi.org/10.3390/ijerph19010398
Chicago/Turabian StyleOrsini, Ester, Marilisa Quaranta, Giulia Adalgisa Mariani, Sara Mongiorgi, Lucio Cocco, Anna Maria Billi, Lucia Manzoli, and Stefano Ratti. 2022. "Near-Peer Teaching in Human Anatomy from a Tutors’ Perspective: An Eighteen-Year-Old Experience at the University of Bologna" International Journal of Environmental Research and Public Health 19, no. 1: 398. https://doi.org/10.3390/ijerph19010398
APA StyleOrsini, E., Quaranta, M., Mariani, G. A., Mongiorgi, S., Cocco, L., Billi, A. M., Manzoli, L., & Ratti, S. (2022). Near-Peer Teaching in Human Anatomy from a Tutors’ Perspective: An Eighteen-Year-Old Experience at the University of Bologna. International Journal of Environmental Research and Public Health, 19(1), 398. https://doi.org/10.3390/ijerph19010398







